Abstract
Background
Virtual reality (VR) training with motion-controlled console games can be incorporated into stroke rehabilitation programs. The use of a variety of gaming software can provide the patient with an opportunity to perform activities that are exciting, entertaining, and that may not be feasible in clinical environments. The aim of this preliminary randomized controlled study was to investigate the effects of game-based VR canoe paddling training, when combined with conventional physical rehabilitation programs, on postural balance and upper extremity function in 30 patients with subacute stroke.
Material/Methods
Thirty patients, who were within six months following the diagnosis of stroke, were randomly allocated to either the experimental group (n=15) or the control group (n=15). All participants participated in a conventional rehabilitation program. Also, the experimental group (n=15) performed the VR canoe paddling training for 30 minutes each day, three times per week, for five weeks. After five weeks, outcomes of changes in postural balance and upper extremity function were evaluated and compared between the two groups.
Results
At five weeks, postural balance and upper extremity function showed significant improvements in both patients groups when compared with the baseline measurements (p<0.05). However, postural balance and upper extremity function were significantly improved in the experimental group when compared with the control group (p<0.05).
Conclusions
Game-based VR canoe paddling training is an effective rehabilitation therapy that enhances postural balance and upper extremity function in patients with subacute stroke when combined with conventional physical rehabilitation programs.
MeSH Keywords: Postural Balance, Stroke, Upper Extremity, Virtual Reality Exposure Therapy
Background
The maintenance of the core or upper body control, is essential for maintaining posture and stability while changing positions, performing activities of daily living (ADL), and ambulating [1,2]. Patients who are undergoing physical rehabilitation following stroke, tend to deviate towards the affected side, as a result of postural instability, which induces both asymmetrical trunk movement and trunk muscle weakness. Upper body instability makes it difficult to maintain postural control when performing tasks and leads to functional disability [3]. The lack of postural stability also affects the balance of patients following stroke, increasing the risk of falls, and negatively impacting on patient independence and safety. For example, it has been reported that up to 73% of patients with stroke experience a fall within six months after leaving hospital [4]. Falls following a stroke can have severe consequences, including hip fractures and reduced physical activity due to fear of repeat falls [5]. Therefore, because these factors can have a negative impact on patient rehabilitation following stroke, the improvement of postural stability is an important goal of patient rehabilitation following stroke [6].
Sports that involve paddling with a single oar, such as canoeing and kayaking, are effective outdoor activities that improve postural stability and upper body stabilization [7]. Continuous body adjustment and compensation are required during the single-oar paddling motion to maintain balance during perturbations caused by the movement of the canoe or kayak and the paddle in the water [8]. Currently, canoe paddling training can be conducted using an ergometer to provide a training opportunity that is independent of outdoor conditions and to better control training progression [9]. A paddling ergometer has also been studied for rehabilitation training of patients with paraplegia and has been shown to be effective in improving postural control, balance, motor performance, and upper extremity strength [8,9].
Game-based virtual reality (VR) using gaming consoles is now used as a therapeutic approach for the rehabilitation of patients with stroke and provides an opportunity for patients to perform activities that are difficult in a clinical setting. Furthermore, VR programs are often designed to be more entertaining and enjoyable than traditional physical therapy tasks, thereby encouraging patients to participate in the rehabilitation program.
The use of VR equipment specifically designed for physical rehabilitation is not yet commonly available in clinical settings. Therefore, VR rehabilitation programs using a game-based, motion-controlled console that can be used in clinical settings and at low cost that can utilize a variety of gaming software are needed.
The aim of this preliminary randomized controlled study was to investigate the effects of game-based VR canoe paddling training, when combined with conventional physical rehabilitation programs, on postural balance and upper extremity function in 30 patients with subacute stroke.
Material and Methods
Patients studied
Initially, 31 study participants were recruited from an inpatient rehabilitation center in the Sahmyook University Hospital, Gyeonggi Province, South Korea. Participants were selected if they met the following criteria: subacute stroke within the prior six months; a Mini-Mental State Examination (MMSE) score ≥21; moderate (7–11) to good (12–16) scores on the trunk impairment scale (TIS) [10]; and the ability to to stand independently for at least 3 minutes without an assistive device.
The exclusion criteria for this study included a history of a psychiatric disorder, dementia, apraxia or hemi-neglect, epilepsy, the presence of a pacemaker, severe pain in the hemiplegic shoulder, ataxia, or any other cerebellar symptoms. Individuals who began the study, but participated in less than 80% of the intervention activities, were also excluded from the study.
All the participants in this study signed informed consents after receiving a detailed explanation of the study objectives and requirements. The study was approved by the Institutional Review Board (IRB) of Sahmyook University, Gyeonggi Province, South Korea.
Study design
This study was an assessor-blinded, randomized controlled study. To determine the sample size, the G*Power 3.19 statistical power analysis software program was used. The alpha level and the power were set as 0.05 and 0.8, respectively. According to a prior pilot test, the effective size was set at 0.94, and at least 15 subjects were required in each group. A total of 31 participants were initially enrolled in the trial and randomly assigned to the experimental group (n=16) or the control group (n=15) after undergoing a preliminary test. The randomization process was performed using Random Allocation software for parallel group randomized studies [11].
Both the experimental and control groups received a conventional rehabilitation program consisting of physical therapy and occupational therapy. All participants underwent physical therapy aimed at improving balance and lower limb strength to facilitate walking; occupational therapy was used to improve the performance of activities of daily living (ADL). Each type of therapy was performed for 30 minutes per session, twice daily, five days each week, for five weeks. The patients in the experimental group performed the game-based virtual reality (VR) canoe paddling training for 30 minutes per day, three days per week, for five weeks. The post-test evaluation was performed one day after the five-week intervention period. All assessment data were collected by two physical therapists, who were blinded to the treatment allocations (Figure 1).
Figure 1.
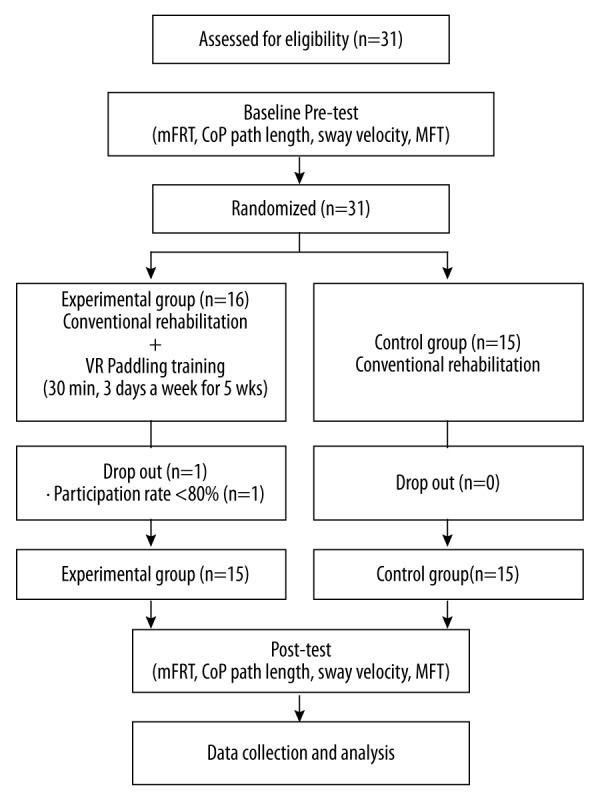
Flow diagram of the study design.
The canoe paddling game used for the VR training program in this study was the Nintendo Wii Sports Resort game (Nintendo®, Kyoto, Japan). To simulate the swaying from side to side that occurs in an actual canoe; the canoe-like apparatus was created by fixing a chair to a springboard (W: 45 cm×D: 150 cm×H: 20 cm) (Pedalo® Springboard, Germany). While seated on the springboard, the study participants performed a paddling movement with both hands grasping the motion controller that was inserted in a separate canoe paddle accessory (Nintendo®, Kyoto, Japan). Grip-assist gloves were provided for patients who found it difficult to grasp the motion controller.
The study participants operated the paddle in the direction of the virtual character displayed on an LED TV 42LN549C screen (LG Electronics, Korea) during the intervention sessions. Also, study participants were instructed to focus on trunk control to maintain their balance on top of the springboard, while canoe paddling. For safety reasons, the patients wore a safety belt on their waist during the training. The intervention consisted of three sessions. The first session was carried out in a ‘free practice’ mode for 5 minutes to allow patients to warm up and familiarize themselves with the program. The second session was performed in a ‘timed run’ mode in which each patient established a personal record of paddling distance during 15 minutes. The third session was performed in a ‘competition mode.’ during which the patient was motivated to improve their performance by competing with a caregiver or therapist for 10 minutes. Improvements in the personal records for paddling distance during the timed run mode were used as indicators of achievement by comparison with previous results (Figure 2).
Figure 2.
Game-based virtual reality (VR) canoe paddling training.
Outcome measurements
The modified functional reach test (mFRT) and postural sway test were used to assess the postural balance of the study participants. The mFRT assesses trunk stability in the forward and lateral direction by measuring the maximal distance an individual can reach forward beyond arm’s length at shoulder height while maintaining a fixed base of support in the sitting position. The distance was measured as the difference between the position of the acromion process of the scapula at the start and end of the action. The mFRT was repeated three times, and the average value was calculated. Previously published data have shown that the inter-observer reliability of the mFRT was good (r=0.97) [12].
To assess postural sway for each study participant, the Wii Balance Board (WBB) (Nintendo®, Kyoto, Japan) was used in a system that included the WBB, a laptop equipped with Bluetooth technology, and Balancia version 2.0 software (Minto Systems, Seoul, Korea) for signal acquisition. Balancia software was developed using C++ in LabVIEW, and data were exchanged between the laptop computer and the WBB using the built-in Bluetooth and Balancia software [13]. The system tracked the movement of the center of pressure (CoP) and calculated the path length (PL) and sway velocity (SV). The data were sampled at a frequency of 50 Hz and were filtered using a fourth-order active low-pass Butterworth filter with a cut-off frequency of 12 Hz. Study participants stood barefoot comfortably on the board, first with their eyes open, and then again with their eyes closed. The participants attempted to remain as still as possible for 30 seconds, and the average of three consecutive measurements was calculated. A 30-second break period was provided when changing between standing with the eyes open and the eyes closed.
The manual function test (MFT) was used to assess the upper extremity motor function in the study participants. The MFT consisted of four shoulder assessment items and four hand assessment items. Flexion, extension, abduction, and adduction were assessed for shoulder functions, and the ability to grasp, pick up, and pinch were assessed for hand functions. The total MFT score ranged from 0 (severely impaired) to 32 (full function). Previously published data have shown that the MFT on the affected side had a test-retest reliability of r=0.99 and an inter-observer reliability of r=0.99 [14].
Statistical analysis
Statistical analysis was performed using SPSS version 19.0 software (IBM, Chicago, IL, USA). The Shapiro-Wilk test was used to confirm the normal distribution of all outcome variables. The paired t-test was used to compare dependent variables within groups; independent t-test and Chi-squared test were used to compare dependent variables between the two groups. Statistical significance was <0.05 for p-values.
Results
One of the 16 study participants in the experimental group was excluded from the analysis because of a participation rate less of 80%. There were then 30 study participants in total, with 15 participants in each group, who completed the five weeks of intervention therapy and the associated assessments. There were no significant differences in the general characteristics between the two groups (Table 1), or dependent variables between the two groups (Tables 2, 3).
Table 1.
General characteristics of the participants (N=30).
| Experimental group (n=15) | Control group (n=15) | χ2/t(p) | |
|---|---|---|---|
| Gender (male/female) | 9/6 | 9/6 | 0.000 (1.000) |
| Age (years) | 61.80±6.80* | 61.33±8.44 | 0.167 (0.869) |
| Height (cm) | 161.60±7.91 | 161.93±8.17 | −0.113 (0.910) |
| Weight (kg) | 61.73±8.15 | 63.40±6.36 | −0.625 (0.537) |
| Stroke type (Infarction/hemorrhage) | 9/6 | 10/5 | 0.144 (0.705) |
| Affected side (left/right) | 9/6 | 10/5 | 0.144 (0.705) |
| Onset time (months) | 3.43±1.34 | 3.13±1.54 | 0.575 (0.570) |
| TIS (scores) | 12.93±1.62 | 13.13±1.36 | −0.366 (0.717) |
| MMSE-K (scores) | 23.73±2.12 | 24.20±2.24 | −0.586 (0.563) |
TIS – trunk impairment scale; MMSE-K – mini mental state examination-Korea version.
Mean ± standard deviation.
Table 2.
Comparison of postural balance within groups and between groups (N=30).
| Experimental group (n=15) | Control group (n=15) | t(p) | ||
|---|---|---|---|---|
| The changes of mFRT values | ||||
| Forward (cm) | Pre | 21.50±4.28* | 20.04±4.34 | 0.932 (0.359) |
| Post | 26.65±4.36 | 24.14±4.53 | ||
| Post-pre | 5.14±1.66 | 4.10±1.82 | 1.633 (0.114) | |
| t(p) | −12.031 (0.000) | −8.716 (0.000) | ||
| Unaffected side (cm) | Pre | 13.40±2.87 | 13.27±2.39 | 0.136 (0.893) |
| Post | 20.13±3.01 | 18.60±3.32 | ||
| Post-pre | 6.73±1.61 | 5.33±1.85 | 2.197 (0.036) | |
| t(p) | −16.140 (0.000) | −11.145 (0.000) | ||
| Affected side (cm) | Pre | 8.09±2.36 | 8.04±2.80 | 0.051 (0.959) |
| Post | 13.73±3.15 | 12.16±3.49 | ||
| Post-pre | 5.64±1.35 | 4.12±1.86 | 2.564 (0.016) | |
| t(p) | −16.212 (0.000) | −8.565 (0.000) | ||
| The changes of postural sway | ||||
| EO-CoP PL (cm) | Pre | 82.48±30.68 | 74.02±28.48 | 0.782 (0.441) |
| Post | 75.69±31.63 | 72.88±28.31 | ||
| Post-pre | −6.79±8.10 | −1.14±3.25 | 2.505 (0.022) | |
| t(p) | 3.247 (0.006) | 1.361 (0.195) | ||
| EO-SV (cm/s) | Pre | 2.78±1.05 | 2.58±0.96 | 0.533 (0.598) |
| Post | 2.42±0.94 | 2.50±0.96 | ||
| Post-pre | −0.36±0.23 | −0.08±0.14 | 3.846 (0.001) | |
| t(p) | 5.863 (0.000) | 2.311 (0.037) | ||
| EC-CoP PL (cm) | Pre | 99.88±38.62 | 87.17±36.04 | 0.932 (0.359) |
| Post | 92.97±38.10 | 84.25±32.99 | ||
| Post-pre | −6.91±3.41 | −2.92±6.49 | 2.109 (0.044) | |
| t(p) | 7.846 (0.000) | 1.739 (0.104) | ||
| EC-SV (cm/s) | Pre | 3.44±1.32 | 3.08±1.22 | 0.781 (0.441) |
| Post | 3.22±1.28 | 2.99±1.14 | ||
| Post-pre | −0.23±0.16 | −0.09±0.16 | 2.316 (0.028) | |
| t(p) | 5.421 (0.000) | 2.090 (0.055) | ||
mFRT – modified functional reach test; EO – eyes opened; EC – eyes closed; CoP – center of pressure; PL – path length; SV – sway velocity.
Mean ± standard deviation.
Table 3.
Comparison of upper limb motor function within groups and between groups (N=30).
| Experimental group (n=15) | Control group (n=15) | t(p) | ||
|---|---|---|---|---|
| The change of MFT scores | ||||
| Total (score) | Pre | 8.93±1.53* | 8.80±1.97 | 2.207 (0.838) |
| Post | 11.40±2.47 | 10.27±1.91 | ||
| Post-pre | 2.47±1.36 | 1.47±0.92 | 2.367 (0.025) | |
| t(p) | −7.046 (0.000) | −6.205 (0.000) | ||
| Upper limb (score) | Pre | 7.80±0.86* | 8.13±1.64 | −0.696 (0.494) |
| Post | 9.87±1.36 | 9.20±1.42 | ||
| Post-pre | 2.07±1.22 | 1.07±0.88 | 2.567 (0.016) | |
| t(p | −6.546 (0.000) | −4.675 (0.000) | ||
| Hand (score) | Pre | 1.07±0.80 | 0.67±0.72 | 1.437 (0.162) |
| Post | 1.53±0.92 | 1.07±0.70 | ||
| Post-pre | 0.47±0.64 | 0.40±0.51 | 0.316 (0.754) | |
| t(p | −2.824 (0.014) | −3.055 (0.009) |
MFT – manual function test.
Mean ± standard deviation.
Outcome measures of postural balance data for the experimental and control groups are shown in Table 2. The modified functional reach test (mFRT) for all directions showed significant improvement in both groups when compared with baseline values (p<0.05). However, the experimental group showed significantly more improvement than the control group (p<0.05). The center of pressure (CoP), path length (PL), and sway velocity (SV) associated with postural sway were significantly decreased in both the eye open and eyes closed condition when compared with baseline values in the experimental group (p<0.05). In the control group, only the SV when the participant’s eyes were open was significantly decreased compared with the baseline values (p<0.05); the experimental group showed a significantly greater reduction in the SV compared with the control group (p<0.05).
The changes in upper body extremity function, upper limb, and hand item scores of the manual function test (MFT) were significantly improved in both groups compared with baseline values (p<0.05). However, the experimental group showed significantly more improvement compared with control group (p<0.05) (Table 3).
Discussion
The aim of this preliminary randomized controlled study was to investigate the effects of game-based virtual reality (VR) canoe paddling training, when combined with conventional physical rehabilitation programs, on postural balance and upper extremity function in 30 patients with subacute stroke. The findings were that after five weeks, the experimental group who underwent additional VR training showed significantly greater improvement in trunk stability on the affected side and the unaffected side, postural sway, and upper extremity function.
The modified functional reach test (mFRT) results in the experimental group showed an average improvement of 19.32% in the forward direction, 33.43% in the direction of the unaffected side, and 41.01% in the direction of the affected side, relative to baseline measurements. These values were, respectively, 2.34%, 4.77%, and 7.19% greater than those in the control group. In this study, the mFRT results showed a greater improvement in measurements along the direction of the unaffected side and the affected side compared with the forward direction. Balance control, when moving forward and backward in the sitting position, can be assisted by the lower limbs, whereas balance control when moving medially and laterally depends only on trunk control [15]. Unlike previous VR balance training [16–20], the participants in this study focused on the use of their trunk muscles to maintain postural balance, while paddling on top of a swinging springboard. The effort to maintain postural balance seems to have contributed to increased postural stability through an interactive process during VR canoe paddling training.
Several previously published studies have reported improved balance and gait in patients following stroke with the use of the Wii Balance Board (WBB) while standing [16–20]. However, dynamic balance training involving weight transfer and visual feedback did not result in a significant improvement in standing postural sway in patients with stroke. In 2012, Cho et al. [17] showed that a VR balance training program that used WBB improved the dynamic balance when assessed by the Berg balance scale and the ‘timed up and go’ (TUG) test, but there was no effect on postural sway. According to these previous findings, the postural control skill learned through the dynamic balance training was not effective in maintaining the static balance [17]. However, Cuthbert et al. [22] reported that balance training that facilitates only one body position, such as weight shifting in the standing position, did not improve dynamic balance as much as static balance. Based on the findings of Cuthbert et al. [22], using the WBB as an additional method to informally assess or treat dynamic balance would not be as strongly recommended as it would be for improving static balance. Yu et al. [23] showed that when patients with stroke maintain a standing posture, movements are minimized and less effort is required maintain their center of gravity. These results indicated that the simultaneous improvements in both static and dynamic balance depended on particular training methods and suggested the need for interventions that could influence both static and dynamic balance [23]. Whether or not dynamic balance training is effective in improving static postural stability remains unresolved.
Unlike previous studies, this present study emphasized trunk control through game-based VR canoe paddling training in the sitting position. As a result, the experimental group showed a significantly greater improvement in postural sway when compared with the control group. Therefore, the findings of this study indicated that enhancing the ability to maintain postural control can improve not only postural stability but also postural sway, in patients with subacute stroke. Game-based VR paddling training in patients with subacute stroke showed a positive effect on upper extremity function.
In this study, the manual function test (MFT) was used to assess the changes in upper extremity function. The post-intervention MFT scores in the experimental group showed improvement of 27.65% compared with baseline values, which was 10.96% greater than the improvement observed in the control group. It is interesting that the variation in the upper limb item scores of the MFT was significantly greater (13.38%) in the experimental group when compared with the control group. The core muscles, which control the trunk, play an important role in trunk stability by connecting the lower limbs to the upper limbs [24]. The enhanced trunk stability acquired during the paddling exercises appeared to have influenced the improvement in the movement of the upper extremity. Also, it seems that the effort to use the proximal part of the upper extremity strongly contributed to increased upper extremity function during the paddling. In a previously published study by da Silva Cameirao et al. [25] they showed that game-based VR rehabilitation was effective in improving the upper extremity function and resulted in more rapid functional recovery when compared with a control group when applied during the early stages of stroke. Furthermore, Michaelsen et al. [26] reported that trunk restraint training for upper extremity function was not beneficial in mildly impaired patients with stroke.
In this study, the participants were patients with subacute stroke, which occurred <6 months previously, and with moderately severe MFT scores (range, 6–11). During the intervention process, there were some complaints from the study participants regarding shoulder pain due to increase in the use of the upper extremity, since the use of hemiparetic side was difficult. However, as the study participants adapted to the intervention and concentrated in the VR training, there was a reduction in pain and improvements in the participation of the hemiparetic upper limb. During the canoe paddling training, the trunk stability and stability of the proximal part of the upper extremity could be improved, which may have affected the progressive reduction in discomfort.
Standard rehabilitation for patients who have experienced stroke has the properties of being repetitive and task-oriented, leaving the patients, in many cases, with low levels of participation and motivations for training activities. As a countermeasure for this phenomenon, interventions that facilitate VR may become increasingly used and may be a method to increase patient motivation, participation, and compliance by patients. An immediate response regarding patient performance using visual feedback is provided to the patients, which allows more active participation and makes the experience more rewarding and entertaining. Although previously published VR-related studies report the use of VR gaming, there is also a study that has shown that the attention of the participants can be limited when trained with VR in an environment that is not reality-based [27]. Paddling training used in the intervention method of this study provided not only the physical simulation of actual canoeing but was also able to induce coordinated movements by controlling the trunk and upper limb simultaneously, while in the sitting position. The VR paddling gaming training was composed of a free practice mode, a timed run mode, and a competition mode, which motivated the participants to be more familiar with the program and to participate more actively. As a result, the experimental group, who participated in VR paddling training, had increased improvements in postural balance and upper extremity function when compared with the control group.
This study is the first to demonstrate improvement in postural balance and upper limb movement, while in a sitting position, resulting from the use of a motion-controlled VR video gaming to simulate an actual environment. However, the study had several limitations. First, we did not control the intensity of the conventional rehabilitation training that was provided to both groups. The physical therapy that patients underwent to improve balance and lower limb strength for improving gait may have affected the lower limb strength of the participants. Second, the control group did not receive placebo therapy for comparison with the experimental group. However, it has been previously suggested that placebo physical therapy is impossible to deliver [28]. Further studies that include a comparison of task-oriented training with VR training are therefore required. Third, we did not evaluate the long-term effects of VR training, and there remains a need for further studies that include long-term follow-up assessment. Finally, although the study design included the blinding of patient treatment allocation to the assessor, there remains a possibility that the assessor was aware of the patient groups. Therefore, to improve the understanding of the effects of VR training programs in patients with stroke, further studies that use more stringent controlled methods are required.
Conclusions
This preliminary randomized controlled clinical study is the first to assess the effects of game-based virtual reality (VR) canoe paddling training on postural balance and upper extremity function in patients with subacute stroke. The findings of this study indicate that the addition of game-based VR paddling training to standard post-stroke rehabilitation programs may be more effective than conventional rehabilitation alone for improving postural balance and upper extremity function. Game-based VR training, when offered in more realistic clinical circumstances, may result in meaningful therapeutic effects in patients with stroke.
Footnotes
Source of support: This research was supported by the Daejeon University Fund, 2016
References
- 1.Van Criekinge T, Saeys W, Hallemans A, et al. Effectiveness of additional trunk exercises on gait performance: Study protocol for a randomized controlled trial. Trials. 2017;18:249. doi: 10.1186/s13063-017-1989-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dogru Huzmeli E, Yildirim SA, Kilinc M. Effect of sensory training of the posterior thigh on trunk control and upper extremity functions in stroke patients. Neurol Sci. 2017;38:651–57. doi: 10.1007/s10072-017-2822-z. [DOI] [PubMed] [Google Scholar]
- 3.Portnoy S, Reif S, Mendelboim T, Rand D. Postural control of individuals with chronic stroke compared to healthy participants: TUG, FRT and center of pressure movement. Eur J Phys Rehabil Med. 2017 doi: 10.23736/S1973-9087.17.04522-1. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 4.Batchelor FA, Mackintosh SF, Said CM, Hill KD. Falls after stroke. Int J Stroke. 2012;7:482–90. doi: 10.1111/j.1747-4949.2012.00796.x. [DOI] [PubMed] [Google Scholar]
- 5.Andersson AG, Seiger A, Appelros P. Hip fractures in persons with stroke. Stroke Res Treat. 2013;2013:954279. doi: 10.1155/2013/954279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Haruyama K, Kawakami M, Otsuka T. Effect of core stability training on trunk function, standing balance, and mobility in stroke patients. Neurorehabil Neural Repair. 2017;31:240–49. doi: 10.1177/1545968316675431. [DOI] [PubMed] [Google Scholar]
- 7.Stambolieva K, Diafas V, Bachev V, Christova L, Gatev P. Postural stability of canoeing and kayaking young male athletes during quiet stance. Eur J Appl Physiol. 2012;112:1807–15. doi: 10.1007/s00421-011-2151-5. [DOI] [PubMed] [Google Scholar]
- 8.Grigorenko A, Bjerkefors A, Rosdahl H, Hultling C, et al. Sitting balance and effects of kayak training in paraplegics. J Rehabil Med. 2004;36:110–16. doi: 10.1080/16501970310020401. [DOI] [PubMed] [Google Scholar]
- 9.Bjerkefors A, Thorstensson A. Effects of kayak ergometer training on motor performance in paraplegics. Int J Sports Med. 2006;27:824–29. doi: 10.1055/s-2005-872970. [DOI] [PubMed] [Google Scholar]
- 10.Jijimol G, Fayaz RK, Vijesh PV. Correlation of trunk impairment with balance in patients with chronic stroke. NeuroRehabilitation. 2013;32:323–25. doi: 10.3233/NRE-130851. [DOI] [PubMed] [Google Scholar]
- 11.Saghaei M. Random allocation software for parallel group randomized trials. BMC Med Res Methodol. 2004;4:26. doi: 10.1186/1471-2288-4-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Katz-Leurer M, Fisher I, Neeb M, Schwartz I, Carmeli E. Reliability and validity of the modified functional reach test at the subacute stage post-stroke. Disabil Rehabil. 2009;31:243–48. doi: 10.1080/09638280801927830. [DOI] [PubMed] [Google Scholar]
- 13.Park DS, Lee G. Validity and reliability of balance assessment software using the Nintendo Wii balance board: usability and validation. J Neuroeng Rehabil. 2014;11:99. doi: 10.1186/1743-0003-11-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Miyamoto S, Kondo T, Suzukamo Y, Michimata A, Izumi S. Reliability and validity of the Manual Function Test in patients with stroke. Am J Phys Med Rehabil. 2009;88:247–55. doi: 10.1097/PHM.0b013e3181951133. [DOI] [PubMed] [Google Scholar]
- 15.Van Nes IJ, Nienhuis B, Latour H, Geurts AC. Posturographic assessment of sitting balance recovery in the subacute phase of stroke. Gait Posture. 2008;28:507–12. doi: 10.1016/j.gaitpost.2008.03.004. [DOI] [PubMed] [Google Scholar]
- 16.Bower KJ, Clark RA, Mcginley JL, Martin CL, Miller KJ. Clinical feasibility of the Nintendo Wii for balance training post-stroke: A phase II randomized controlled trial in an inpatient setting. Clin Rehabil. 2014;28:912–23. doi: 10.1177/0269215514527597. [DOI] [PubMed] [Google Scholar]
- 17.Cho KH, Lee KJ, Song CH. Virtual-reality balance training with a video-game system improves dynamic balance in chronic stroke patients. Tohoku J Exp Med. 2012;228:69–74. doi: 10.1620/tjem.228.69. [DOI] [PubMed] [Google Scholar]
- 18.Barcala L, Grecco LA, Colella F, Lucareli PR, et al. Visual biofeedback balance training using wii fit after stroke: a randomized controlled trial. J Phys Ther Sci. 2013;25:1027–32. doi: 10.1589/jpts.25.1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rajaratnam BS, Gui Kaien J, Lee Jialin K, et al. Does the inclusion of virtual reality games within conventional rehabilitation enhance balance retraining after a recent episode of stroke? Rehabil Res Pract. 2013;2013:649561. doi: 10.1155/2013/649561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Meldrum D, Glennon A, Herdman S, Murray D, Mcconn-Walsh R. Virtual reality rehabilitation of balance: Assessment of the usability of the Nintendo Wii((R)) Fit Plus. Disabil Rehabil Assist Technol. 2012;7:205–10. doi: 10.3109/17483107.2011.616922. [DOI] [PubMed] [Google Scholar]
- 21.Barclay-Goddard R, Stevenson T, Poluha W, et al. Force platform feedback for standing balance training after stroke. Cochrane Database Syst Rev. 2004;(4):CD004129. doi: 10.1002/14651858.CD004129.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cuthbert JP, Staniszewski K, Hays K, et al. Virtual reality-based therapy for the treatment of balance deficits in patients receiving inpatient rehabilitation for traumatic brain injury. Brain Inj. 2014;28:181–88. doi: 10.3109/02699052.2013.860475. [DOI] [PubMed] [Google Scholar]
- 23.Yu E, Abe M, Masani K, et al. Evaluation of postural control in quiet standing using center of mass acceleration: Comparison among the young, the elderly, and people with stroke. Arch Phys Med Rehabil. 2008;89:1133–39. doi: 10.1016/j.apmr.2007.10.047. [DOI] [PubMed] [Google Scholar]
- 24.Huxel Bliven KC, Anderson BE. Core stability training for injury prevention. Sports Health. 2013;5:514–22. doi: 10.1177/1941738113481200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Da Silva Cameirao M, Bermudez IBS, Duarte E, Verschure PF. Virtual reality based rehabilitation speeds up functional recovery of the upper extremities after stroke: A randomized controlled pilot study in the acute phase of stroke using the rehabilitation gaming system. Restor Neurol Neurosci. 2011;29:287–98. doi: 10.3233/RNN-2011-0599. [DOI] [PubMed] [Google Scholar]
- 26.Michaelsen SM, Dannenbaum R, Levin MF. Task-specific training with trunk restraint on arm recovery in stroke: Randomized control trial. Stroke. 2006;37:186–92. doi: 10.1161/01.STR.0000196940.20446.c9. [DOI] [PubMed] [Google Scholar]
- 27.Horlings CG, Carpenter MG, Kung UM, et al. Influence of virtual reality on postural stability during movements of quiet stance. Neurosci Lett. 2009;451:227–31. doi: 10.1016/j.neulet.2008.12.057. [DOI] [PubMed] [Google Scholar]
- 28.Stack E. Physiotherapy: The ultimate placebo. Physiother Res Int. 2006;11:127–28. doi: 10.1002/pri.342. [DOI] [PubMed] [Google Scholar]



