Abstract
Writing effective learning objectives is a necessary skill in academic medicine. Learning objectives are clearly written, specific statements of observable learner behavior or action that can be measured upon completion of an educational activity. They are the foundation for instructional alignment whereby the learning objectives, assessment tools, and instructional methods mutually support the desired learning outcome. This review article describes the essential components of a learning objective and provides practical tips on writing well-defined learning objectives.
Keywords: learning objectives, goals, Bloom's Taxonomy
Introduction
An anesthesiologist starts his grand rounds presentation on the topic of malignant hyperthermia (MH) with the following learning objectives:
Understand the pathophysiology of MH.
Review the clinical presentation of MH.
Discuss the treatment of MH.
Become familiar with caffeine-halothane contracture testing for MH.
This list informs the attendees about the topics covered during the presentation. However, do they know what is expected of them when they apply this content in their own clinical practice?
We have all seen learning “objectives” mentioned, such as the ones above, at the beginning of a presentation or workshop. But is what we see actually a learning objective? Learning objectives are often confused with learning goals; the example above is such a case in point. Learning goals are related to—but different from—learning objectives. A learning goal is a broad statement of an expected learning outcome of a course or curriculum. Learning goals provide a vision for the future and often summarize the intention or topic area of several related learning objectives. Learning objectives are drawn from the learning goals. They are guiding statements for each learning encounter, and they connect intention with reality within the learning experience as well as to the assessment planned. In keeping with the Roman philosopher Lucius Seneca, who said, “If a man knows not to which port he sails, no wind is favorable,” this review article describes the essential components of learning objectives and provides practical tips on writing well-defined learning objectives.
Defining “Learning Objective”
A learning objective is a description of what the learner must be able to do upon completion of an educational activity. A well-written learning objective outlines the knowledge, skills and/or attitude the learners will gain from the educational activity and does so in a measurable way.
An effective learning objective should include the following 5 elements: who, will do, how much or how well, of what, by when.1 The mnemonic SMART—Specific, Measurable, Attainable, Relevant, and Time-bound—can be used to describe the elements of a well-written learning objective.2 One example of a SMART objective for an airway conference is: “Upon completion of the difficult airway workshop, participants should be able to formulate an accurate algorithm for the management of an obese adult patient with inadequate face mask ventilation, according to the American Society of Anesthesiologists difficult airway algorithm.”
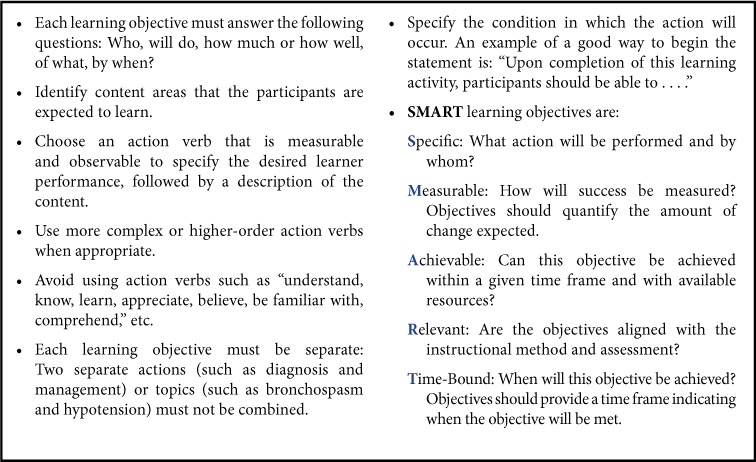
Practical tips for writing learning objectives are summarized in Table 1. Since the point of a learning objective is to describe the intended outcome for learning, begin the learning objective with: “Upon completion of this educational activity, learners should be able to . . . .” The next step is to identify the concepts the learners need to learn and how they will demonstrate their understanding. It is recommended that the instructor choose one action verb that is measurable and observable. Verbs such as understand, know, learn, appreciate, believe, be familiar with, comprehend, and so on, are not observable or measurable and should be avoided. Each learning objective must be separate; two actions (such as diagnosis and management) or topics (such as bronchospasm and hypotension) must not be combined. It is also important that the action verb identify the level and cognitive domain at which the learner is expected to perform. Bloom's Taxonomy connects the depth of learning with action verbs that may be used when writing learning objectives.
Table 1:
Practical tips for writing effective learning objectives.
Blooms' Taxonomy and Action Verbs
When writing learning objectives, educators leverage Bloom's Taxonomy3 (Table 2). Bloom's Taxonomy describes 6 levels of hierarchy in the cognitive domain: knowledge, comprehension, application, analysis, synthesis, and evaluation. This taxonomy was revised in 20014 (Figure 1). Each level of the hierarchy correlates to action verbs that educators use within learning objectives. To help anesthesia educators apply Bloom's Taxonomy more readily to their own learning, we will briefly review what each level of the hierarchy means to learning.
Table 2:
Revised Bloom's Taxonomy of Learning Objectives
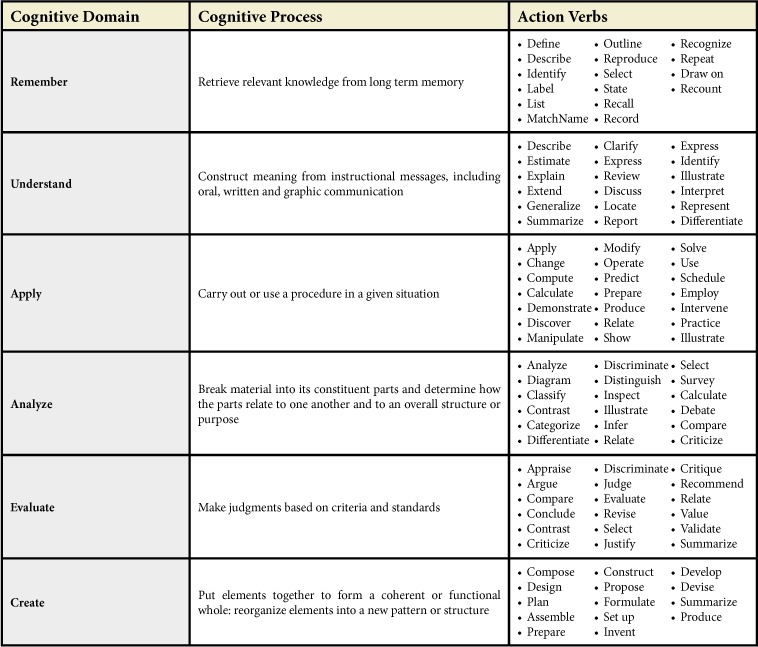
Figure 1:
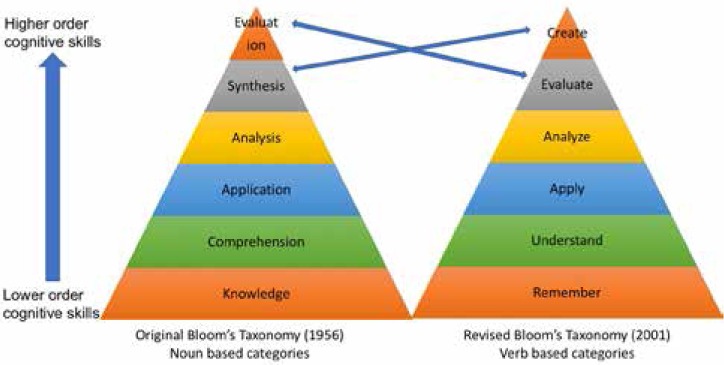
Original and revised versions of Bloom's Taxonomy (Reprinted with permission from Wilson LO. http://thesecondprinciple.com)
Knowledge “involves the recall of specifics and universals, the recall of methods and processes, or the recall of a pattern, structure, or setting.”3 This category appreciates and distinguishes factual knowledge, conceptual knowledge, procedural knowledge, and metacognitive knowledge as separate elements of “knowledge.” In anesthesia teaching, we frequently use the first 3 types. For example, we provide factual knowledge (eg, lecture to undergraduate medical learners), procedural knowledge (eg, teaching in simulation or during an operation), and conceptual knowledge (eg, case-based learning, principles of anesthesia). Metacognitive knowledge is often applicable when giving feedback to learners; for example, when helping learners understand their competency in communication with patients and families.
Comprehension “refers to a type of understanding or apprehension such that the individual knows what is being communicated and can make use of the material or idea being communicated without necessarily relating it to other material or seeing its fullest implications.”3 Application refers to the “use of abstractions in particular and concrete situations.”3 Analysis represents the “breakdown of a communication into its constituent elements or parts such that relative hierarchy of ideas is made clear and/or the relations between ideas expressed are made explicit.”3 Synthesis involves “putting together of elements and parts so as to form a whole,”3 and evaluation includes “judgments about the value of material and methods for given purposes.”3
All educators should make the important connection between the intended learning depth (eg, comprehension) and the action verbs that reflect that intended learning outcome within the learning objective. Action verbs guide the learner about the intended outcome; for example, “critically appraise the evidence related to rapid sequence induction for airway management in pregnant patients.”
Incorporating Bloom's Taxonomy and SMART for Effective Learning Objectives
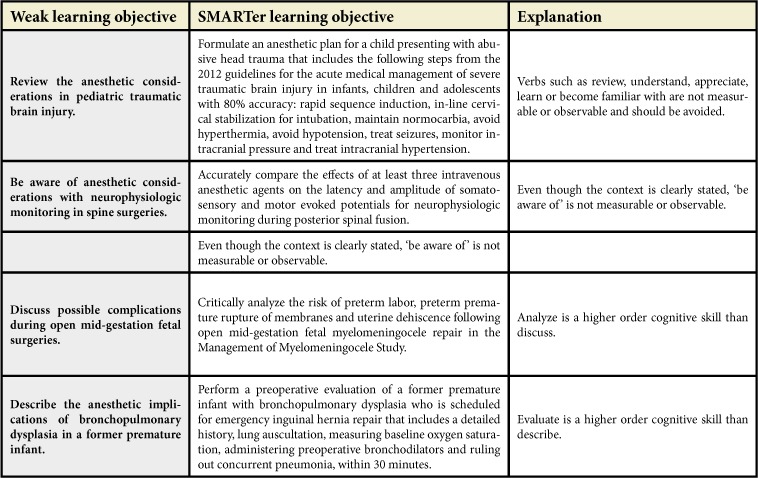
Both Bloom's Taxonomy and SMART are necessary for writing effective learning objectives that communicate the intention for the learner with the intended learning outcomes. Examples of weak learning objectives and suggestions for better wording, based on incorporating Bloom's Taxonomy and SMART, are listed in Table 3.
Table 3.
Examples of weak learning objectives and suggestions for SMARTer learning objectives. All of the learning objectives are written for an hour-long grand rounds presentation and begin with “Upon completion of the grand rounds presentation, participants should be able to:”
When faculty are leading sessions on writing SMART objectives, the authors often hear participants challenge that SMART objectives are longer and very detailed—consequently, will learners even follow them? The counterargument is that any objective worded too broadly, with no measurable standard that is attainable and repeatable for the learner in the given time frame, leads to confusion about “what to study” or “what performance is expected.” The value in writing SMART objectives includes helping educators focus and specify what they intend to teach, assess, and offer as feedback for the learner. This shapes the learning session's scope, the method of instruction, and the type and quality of the assessment.
Do Learning Objectives Add Value to Curriculum and Assessment?
For many, writing out the learning objectives appears to be an effort to its own end. However, learning objectives are the foundation for instructional alignment. Instructional alignment means that learning objectives, assessment tools, and instructional methods mutually support the same educational outcome.5 This is known as the Golden Triangle5 (Figure 2). Well-defined learning objectives outline the desired outcome for learners, which will help specify the instructional method. For example, if we want the learners to demonstrate correct intubation procedure in a normal adult 100% of the time, we need the instructional method to involve some sort of hands-on experience so that learners can demonstrate their skills. In contrast, if the teacher lectures about correct intubation without the opportunity for learners to complete hands-on skills, the learning activity is not aligned with the stated learning objective.
Figure 2:
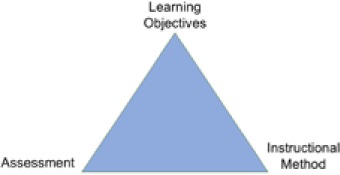
Instructional alignment of learning objectives, assessment and instructional methods.
Likewise, learning objectives guide the assessment method. Taking the above example: If the objective is for learners to be 100% successful in normal adult intubation, assessing their skill using a written exam would misalign the objective and assessment method. As educators, we would miss the accuracy of the skill! Instead, the assessment method needs hands-on performance.
Constructive alignment underscores what learning objectives contribute towards achieving the intended educational outcomes. Learning objectives also contribute to shaping expectations, preparing learners for the educational activity and the standard by which their performance will be measured; the objectives also define faculty and learner responsibilities towards achieving the intended learning outcomes. Learning objectives may also guide teaching, by defining and limiting content or activities.
Are SMART Learning Objectives a Required Component of Medical Education?
Learning objectives are a required component in the planning of all medical education curricula. At the undergraduate level, the Liaison Committee on Medical Education (LCME) requires that “the faculty of a medical school define its medical education program objectives in outcome-based terms that allow the assessment of medical student's progress in developing the competencies that the profession and the public expect of a physician.”6 At the graduate medical education level, one of the common program requirements from the Accreditation Council on Graduate Medical Education (ACGME) states that each program must distribute competency-based goals and objectives for each assignment at every educational level.7 Even for continuing medical education (CME), both the American Medical Association (AMA) and Accreditation Council for Continuing Medical Education (ACCME) require that a CME activity has learning objectives to qualify for category 1 credit.8 Consequently, writing effective learning objectives is a core skill that every academic anesthesiologist should master.
Conclusion
Writing effective learning objectives is a necessary skill in academic medicine. Well-defined learning objectives describe what the learner must be able to achieve upon completion of the educational activity. Bloom's Taxonomy and SMART are two tools that educators may leverage towards writing learning objectives that effectively relate the intended outcomes to the learners, simultaneously setting up the educators to successfully attain the learning outcomes within the time and resources provided. The successful academic anesthesiologist can align the instructional method, assessment, and intended learning outcome by using SMART learning objectives rather than learning goals. In closing, we revisit the learning goals in the opening anecdote of this review article.
Upon completion of the grand rounds presentation, participants will be able to:
Describe at least 3 intracellular mechanisms within the muscle cells during an episode of malignant hyperthermia (MH). The description must include: unregulated calcium release from sarcoplasmic reticulum, sustained muscle contractures, and the resulting hypermetabolic response.
Relate the 4 most common clinical signs of MH (hypercarbia, tachycardia/tachypnea, generalized muscle rigidity, and hyperthermia) to the underlying physiological mechanisms in the muscle cells.
Summarize, in order, the critical steps in the intraoperative management of an MH crisis according to recommendations from the Malignant Hyperthermia Association of the United States.
Formulate an anesthetic plan for management of a MH-susceptible patient that must include the use of: non-triggering anesthetic agents, monitoring for signs of MH, and preparedness to treat acute MH.
Critically appraise the role of caffeinehalothane testing for MH including indications, location, sensitivity, and specificity.
Footnotes
rrh: Learning Objectives
Financial Disclosures: None.
Conflicts of Interest: None.
Author Contributions: Debnath Chatterjee, MD, wrote the manuscript and reviewed the final draft before submission. Janet Corral, PhD, reviewed the initial and final draft and contributed to the content.
References
- 1. Thomas PA. Goals and objectives, : Thomas PA, Kern DE, Hughes MT Chen BY. (Eds.) Curriculum Development for Medical Education: A Six Step Approach, 3rd ed. Baltimore, MD: Johns Hopkins University Press; 2016; 50– 64. [Google Scholar]
- 2. Skrbic N, Burrows J.. Specifying Learning Objectives, : Ashmore L, Robinson D. (Eds.) Learning, Teaching and Development: Strategies for Action. London: Sage Publications; 2014; 54– 87. [Google Scholar]
- 3. Bloom BS. Taxonomy of Educational Objectives: Handbook I: Cognitive Domain. New York: Longman; 1984; 201– 7 [Appendix]. [Google Scholar]
- 4. Anderson LW, Krathwohl DR.. A Taxonomy for Learning, Teaching, and Assessing: A Revision of Bloom's Taxonomy of Educational Objectives. New York: Addison Wesley Longman; 2001. [Google Scholar]
- 5. Cohen SA. Instructional alignment: Searching for a magic bullet. Educ Res. 1987; 16 8: 16– 20. [Google Scholar]
- 6. Liaison Committee on Medical Education Standards for Accreditation of Medical Education Programs Leading to the MD Degree. http://www.lcme.org/publications/#Standards. Published March 2016. Accessed May 10, 2017.
- 7. Accreditation Council for Graduate Medical Education Common Program Requirements. http://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/CPRs_07012016.pdf. Published February 11, 2007. Accessed May 10, 2017.
- 8. American Medical Association Guidance on New Procedure for CME. www.ama-assn.org/ama/pub/education-careers/continuing-medical-education/physicians-recognition-award-credit-system/cme-help/guidance-new-procedure-cme.page. Accessed May 10, 2017.


