Abstract
Rationale:
Anuria is a severe symptom indicating severe kidney damage. Patient recovery from prolonged anuria is rarely reported.
Patient concerns:
A 15-year-old boy received gender- and weight-mismatch heart transplantation (HT) due to dilated cardiomyopathy. He developed severe hypotension, and heart failure 24 hours after surgery, which were relieved by preload reduction treatments. Although, routine examinations did not show any abnormalities in renal function before surgery, anuria occurred 4 days after preload reduction treatments (24-hour urine volume was 23 mL).
Diagnosis:
The patient was diagnosed with acute kidney injury (AKI).
Interventions:
He was admitted to continuous renal replacement therapy (CRRT) or hemodialysis.
Outcomes:
Surprisingly, his urine volume was gradually, and miraculously, restored to more than 1000 mL/24 hours after over 300 days of anuria. Hemodialysis was not needed in the twentieth month after surgery. Moreover, he partially, recovered renal function.
Lessons:
This case indicates the likelihood of recovery from long-term anuria.
Keywords: anuria, continuous renal replacement therapy, heart transplantation, hemodialysis
1. Introduction
Anuria is clinically, defined as a urine output of less than 100 mL/24 hours. It is often caused by total loss of renal function but is occasionally, caused by other pathological conditions, such as severe occlusion of urinal ducts, or heart failure. In general, a long duration of anuria represents irreversible renal failure. Previous reports[1–4] have demonstrated a recovery of urine volume, or renal function after a duration of anuria of approximately, between 14 to 30 days. However, the recovery of renal function after duration of anuria of more than 200 days is rarely reported. It is also seldom reported that anuria is factitiously induced to save a patient's life.
Herein, we report a case of gender- and weight-mismatch heart transplantation (HT) with iatrogenic anuria requiring dialysis in which the patient recovered renal function after 315 days.
2. Case report
A 15-year-old boy who had suffered from years of dilated cardiomyopathy received a HT on November 11, year 2015. His weight was 75 kg, and his height was 184 cm; the donor was a 17-year-old girl with a weight, and height of 50 kg, and 170 cm, respectively, who had experienced brain death after a vehicle accident. An informed consent form was signed by the parents of the recipient. Before surgery, his urine volume, and urine tests were normal, and his serum creatinine was 85 μM. Ultrasound showed no kidney abnormalities. He developed chest pain, tachycardia, more severe hypotension (increased doses of vasopressors, such as an increase in isoprenaline between 0.02 to 0.05 μg/kg.minute, and dopamine between 5 to 8 μg/kg.minute), and other heart failure performance in the 48 hours after HT. He was treated with anti-rejection drugs (mycophenolate mofetil 0.5 g, per os, q12 h; tacrolimus 1 mg, per os, q12 hour; prednisone 40 mg, per os, qd), and strategies to reduce his effective blood volume, and cardiac preload with diuresis by furosemide (10 mg, intravenous injection, q8 hour), and spironolactone (20 mg, per os, bid), and continuous renal replacement therapy (CRRT) (12∼24 hours/day, started on November 14, year 2015). His daily fluid balance from November 11 to 15 was − 183.55 , − 1112.76 , − 703.83 , − 1639.7 , and − 428.58 mL. His central venous pressure remained at approximately 5 mmHg, and his invasive systolic blood pressure remained at 70∼90 mmHg. The symptoms of cardiac failure were immediately, obviously, and lastingly relieved. Later, the doses of vasopressors were reduced appropriately. However, his urine 24-hour volume decreased gradually. Anuria occurred on November 15 year 2015 (urine volume was 23 mL/24 hours), and continued. He was treated with hemodialysis 3 months after the operation. Heart failure never presented again.
The patient had severe pressure sores on both hips 1 month after surgery, and later on, he had septic shock. Secretion cultures confirmed growth of Pseudomonas aeruginosa. Upgraded antibiotics were given, including meropenem (1.0 g, intravenous injection, q8 hour), and amikacin (0.6 g, intravenous injection, qd), and intense care was provided. His fever and infection were gradually, controlled in the next 2 weeks. The pressure sores recovered completely, 6 months after the operation.
Mild anemia occurred after the surgery. The lowest hemoglobin concentration was 81 g/L on November 20, year 2015. Blood transfusions, and later, erythropoietin, were given to support oxygen demand. The hemoglobin concentrations were 91∼110 g/L most of the time.
Vasopressors were stopped after February 15, year 2016. The patient's heart has good function today (LVEF 62%, shown by ultrasound on August 7, year 2017). He has survived more than 2 years after gender- and weight-mismatch HT. However, the duration of anuria was 315 days (until October 2, year 2016) during which his urine volume reached up to 140 mL/24 hours. During this period, there were 225 days when his urine volume was 0, 8 days when it was less than 6 mL, 54 days when it was between 11 to 50 mL, 28 days when it was between 51 to 99 mL, and 7 discrete days when it was between 100 to 160 mL (Fig. 1). Oliguria was maintained for 19 days until October 21, year 2016, and after that time, his urine volume was more than 400 mL. Now, his urine volume is more than 1000 mL/day. His systolic blood pressure is between 80 to 100 mmHg. Hemodialysis was stopped on August 10, year 2017. His serum creatinine was 256 μM on January 4, year 2018. Urine tests were normal. Informed consent was obtained from the patient for publication of this case report, and accompanying images.
Figure 1.
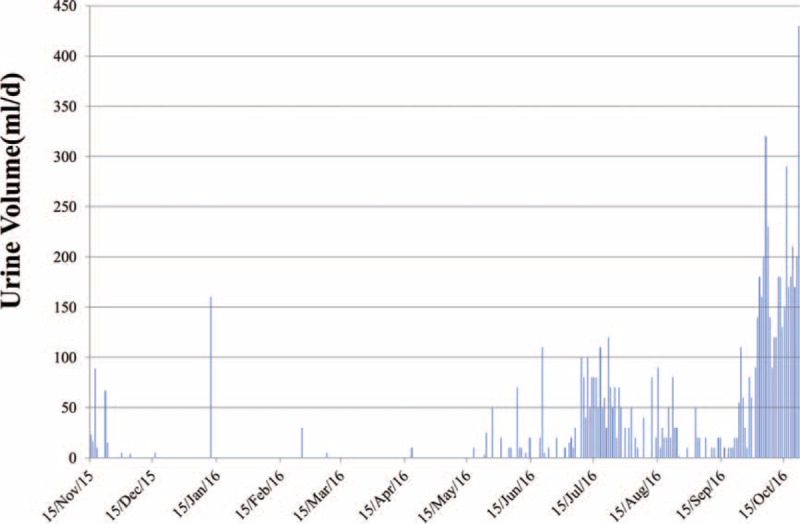
Urine volume during the anuria periods.
Other factors that might have affected his renal function were; 1. Vancomycin (500 mg intravenous injection, q8 hour), which was administered for 1 week after surgery. The drug blood levels were 21.22, 9.99, and 15.97 ug/mL. Two. Ganciclovir (0.25 g, intravenous injection, q12 hour), which was only used twice on the day of and after the operation. Three. Tacrolimus (1∼4 mg, per os, q12 hour), which was used between November 13, year 2015, and May 23, year 2017. The drug blood levels were between 15.0 and 20.4 ng/mL before December 28, year 2015, and they declined below 10.0 ng/mL afterwards. There were no other factors that affected renal function, such as nephrotoxicity drugs or ureteral obstruction.
3. Discussion
HT isthe “gold standard” treatment for end-stage heart failure. Emerging studies have elucidated the impact of gender- and weight-mismatched on HT outcomes. It has been reported that donor-recipient gender mismatch significantly, reduced survival to date among male recipients after HT.[5,6] Bergenfeldt, H. et al found that inappropriate weight match ([IWM] defined as donor weight < 70% of recipient's weight) was associated with increased 30-day mortality, and cumulative mortality, and gender mismatch increased mortality, independently of weight match.[7] In addition, donor/recipient (D/R) body weight mismatch has been related to the occurrence of acute heart transplant failure.[8]
Due to the shortage of donor organs, marginal donors, and a certain degree of D/R mismatches have been admitted to reduce waiting list mortality. Our case of gender- and weight- mismatch HT had a male recipient who received a female donor's heart with a D/R body weight of 0.667, which may be the cause of acute transplant-heart failure. Strategies for reducing his efficient blood volume were performed to protect the transplanted heart, but they induced kidney damage. The therapies did work, and the patient has survived until now.
It was reported that acute kidney injury (AKI) occurred in 73% of children following HT.[9] Approximately, between 5% to 10% of heart-transplant recipients develop end-stage renal failure (ESRF).[10] However, intentionally, induced AKI to save a transplant heart is seldom reported. Despite the brief use of vancomycin, ganciclovir, and tacrolimus post-operatively, there was minimal potential that drugs affected the patient's delayed recovery of renal function. Although, the patient had severe pressure sores, and secondary septic shock 1 month after surgery, they gradually, improved after etiotropic treatment. Therefore, the main cause of renal failure in this patient was induced hypovolemia. The main risk factors for AKI were hypovolemia and hypotension in the intensive care unit.[11] During, and after surgery, normovolemia is of utmost importance. Hypotension should be avoided because even short periods of mean arterial pressure < 55– to 60 mm Hg carry a risk of postoperative AKI.[12] In our case, hypovolemia was a strategy to save the little mismatched heart, and the recipient's life by consequently, sacrificing the kidney. This approach worked based on the end result.
Chronic kidney disease is defined as kidney disease that lasts for more than 3 months.[13] Among these diseases, renal insufficiency is generally, considered to be not recoverable when it lasts for more than 3 months. Anuria is a severe situation that suggests a total loss of renal function. Jung H. Y. et al[14] found that compared with the incomplete recovery group, the complete recovery group included a significantly, higher percentage of patients whose anuria duration was shorter than 12 hours. Conversely, the percentage of patients with anuria duration longer than 10 days was significantly, higher in the incomplete recovery group than in the complete recovery group. Moreover, it has also been reported that between 10 to 70 days durations of anuria could recover renal function. Jongkind, V. et al [15] reported a period of anuria that lasted 14 days before restoring renal function in a case of acute suprarenal occlusion. Hata, M. et al[16] reported renal function recovery after 72 days of anuria that was caused by ureteral obstruction. Our case exceeded the general expectation for urine volume recovery with a 315-day period of anuria, and partial recovery of renal function. Possible reasons for the recovery include the patient's younger age, lack of basic kidney disease, and continuous, and adequate renal replacement therapy.
4. Conclusions
We reported a very rare case of restored urine volume, and partial renal function from over 300 days of anuria in a gender- and weight-mismatch HT recipient. Hypovolemia may be a potential strategy to save a mismatched transplanted heart and the recipient's life. This case demonstrates the likelihood of recovery from long-term anuria induced by hypovolemia.
Author contributions
Conceptualization: Yong-Hua Peng.
Data curation: Yong-Hua Peng.
Formal analysis: Yong-Hua Peng.
Funding acquisition: Yong-Hua Peng.
Investigation: Yong-Hua Peng, Tao-Sheng Li.
Methodology: Yong-Hua Peng, Jie Xiao.
Project administration: Yong-Hua Peng.
Resources: Yong-Hua Peng, Xiao-Min Yu, Chen Yan, Lan Luo, Jie Xiao.
Software: Yong-Hua Peng.
Supervision: Yong-Hua Peng.
Validation: Yong-Hua Peng.
Visualization: Yong-Hua Peng.
Writing – original draft: Yong-Hua Peng.
Writing – review & editing: Yong-Hua Peng.
Footnotes
Abbreviations: AKI = acute kidney injury, CRRT = continuous renal replacement therapy, D/R = donor/recipient, ESRF = end-stage renal failure, HT = heart transplantation, ISHLT = International Society for Heart and Lung Transplantation, IWM = inappropriate weight match.
The authors indicate no potential conflicts of interest.
References
- [1].Eknoyan G, Siegel MB. Recovery from anuria due to malignant hypertension. JAMA 1971;215:1122–5. [PubMed] [Google Scholar]
- [2].Georgaki-Angelaki H, et al. Atypical hemolytic-uremic syndrome (HUS) with recovery after a long-lasting anuria: a case report. Hippokratia 2011;15:90–2. [PMC free article] [PubMed] [Google Scholar]
- [3].Pereira S, Marwaha RK, Pereira BJG, et al. Haemolytic uraemic syndrome with prolonged anuria and cortical calcification: a case report. Pediatr Nephrol 1990;4:65–6. [DOI] [PubMed] [Google Scholar]
- [4].Dougherty JC, Stenzel KH, Scherr L, et al. Recovery from acute renal failure after 23 Days of anuria. JAMA 1963;186:68–9. [DOI] [PubMed] [Google Scholar]
- [5].Prendergast TW, Furukawa S, Beyer AJ, et al. The role of gender in heart transplantation. Ann Thorac Surg 1998;65:88–94. [DOI] [PubMed] [Google Scholar]
- [6].Martinez-Selles M, Almenar L, Paniagua-Martin MJ, et al. Donor/recipient sex mismatch and survival after heart transplantation: only an issue in male recipients? An analysis of the Spanish heart transplantation registry. Transpl Int 2015;28:305–13. [DOI] [PubMed] [Google Scholar]
- [7].Bergenfeldt H, Stehlik J, Hoglund P, et al. Donor-recipient size matching and mortality in heart transplantation: Influence of body mass index and gender. J Heart Lung Transplant 2017;36:940–7. [DOI] [PubMed] [Google Scholar]
- [8].Martinez-Dolz L, Almenar L, Arnau MA, et al. Analysis of factors that can influence the appearance of acute heart transplant failure. Rev Esp Cardiol 2003;56:168–74. [DOI] [PubMed] [Google Scholar]
- [9].MacDonald C, Norris C, Alton GY, et al. Acute kidney injury after heart transplant in young children: risk factors and outcomes. Pediatr Nephrol 2016;31:671–8. [DOI] [PubMed] [Google Scholar]
- [10].Frimat L, Villemot JP, Cormier L, et al. Treatment of end-stage renal failure after heart transplantation. Nephrol Dial Transplant 1998;13:2905–8. [DOI] [PubMed] [Google Scholar]
- [11].Medina Villanueva A, López-Herce Cid J, López Fernández Y, et al. Acute renal failure in critically-ill children. A preliminary study. An Pediatr (Barc) 2004;61:509–14. [DOI] [PubMed] [Google Scholar]
- [12].Goren O, Matot I. Perioperative acute kidney injury. Br J Anaesth 2015;115(Suppl 2):ii3–14. [DOI] [PubMed] [Google Scholar]
- [13].Patel SS, Kimmel PL, Singh A. New clinical practice guidelines for chronic kidney disease: a framework for K/DOQI. Semin Nephrol 2002;22:449–58. [DOI] [PubMed] [Google Scholar]
- [14].Jung HY, Lee JH, Park YJ, et al. Duration of anuria predicts recovery of renal function after acute kidney injury requiring continuous renal replacement therapy. Korean J Intern Med 2016;31:930–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Jongkind V, Kievit JK, Wiersema AM. Recovery of Renal Function after Prolonged Anuria in Acute Suprarenal Aortic Occlusion. Ann Vasc Surg 2016;30:e11–4. [DOI] [PubMed] [Google Scholar]
- [16].Hata M, Tachibana M, Deguchi N, et al. Recovery of renal function after 72 days of anuria caused by ureteral obstruction. J Urol 1983;130:537–8. [DOI] [PubMed] [Google Scholar]


