Abstract
Chondroblastoma is a rare benign tumor, consisting of tissue resembling foetal cartilage, and arising in the epiphyses, or apophyses of long tubular bone. However, chondroblastoma of the cortex of the long bone metaphysis is extremely rare.
A 15-year-old girl presented a 10-month history of intermittent knee pain and without mobility limitation. X ray, computed tomography (CT), and magnetic resonance imaging (MRI) showed a slightly expansile lytic lesion involving the metaphyseal cortex of the left distal femur. During histological examination, typical features of chondroblastoma were observed. Chondroblastoma was definitely and histologically diagnosed. Surgical procedures included intralesional tumor curettage and allograft bone implantation. The patient was discharged without any complications 1 week after surgery and there was no recurrence during a 10-month follow-up.
This report describes a case of chondroblastoma in the metaphyseal cortex of the distal femur and serves as a reminder of the atypical anatomic location of chondroblastoma. Patients in an appropriate age group with typical imaging features may be diagnosed with chondroblastoma despite its rare location.
Keywords: chondroblastoma, magnetic resonance imaging, tomography, tumor, X-ray computed tomography
1. Introduction
Chondroblastoma is a rare type of benign cartilage tumor that accounts for approximately, 1% of all bone tumors, and affects mostly children, and young adults in the second, and third decades of life.[1] It is classically, located in the medullary cavity of long bone epiphyses, and apophyses, and it is rarely, found in the cortex of the long bone metaphysis. We describe a chondroblastoma in the cortex of the distal femur metaphysis, and emphasize imaging findings, and differential diagnosis. Due to the retrospective nature of the study, informed consent from patients and ethics committee approval were waived.
2. Case report
A 15-year-old girl visited our hospital with a 10-month history of intermittent knee pain and without mobility limitation. Her past medical history was unremarkable. Physical examination revealed that the lower end of the shaft of her left femur was swollen with tenderness. No signs of infection were observed, and laboratory data were within normal limits. The radiographs revealed an ovoid radiolucency with sclerotic margins in the metaphysis cortex of her distal left femur (Fig. 1). Computed tomography (CT) showed a 4 × 3 × 2 cm intracortical lesion that split the medial cortex and was surrounded by an eccentrically thickened cortical bone with a local cortical breach. The lesion was well defined, with internal stippled calcifications and without an apparent periosteal reaction (Figs. 2 and 3). In magnetic resonance imaging (MRI), the intracortical lesion exhibited low signal intensity on T1WI, and a mixed signal intensity on T2WI, and was peripherally, surrounded by a hypointense rim on T1WI, and T2WI. A soft tissue thickening medial to the lesion was also observed. Perilesional marrow, and soft tissue edema was found in the fat-suppressed T2WI, and a small amount of effusion was detected in the joint cavity of the left knee. In contrast-enhanced MRI, the lesions showed markedly, inhomogeneous enhancement, and the surrounding bone, and adjacent soft tissue showed a mild enhancement (Figs. 4 and 5). Intraperiosteal chondroma was preoperatively diagnosed based on clinical and radiographic findings.
Figure 1.

Lateral X-ray reveals the localized bone destruction of distal metaphysis of the left femur (white arrow) with internal matrix mineralization and marginal sclerosis.
Figure 2.
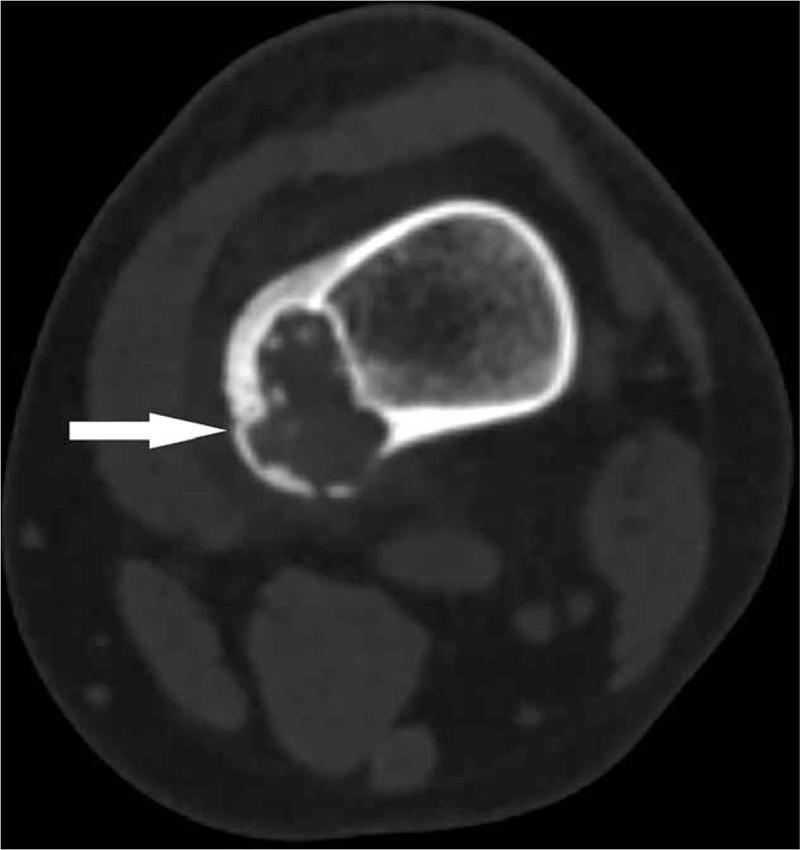
CT reveals the oval bone destruction of the medial-distal left femoral metaphysis (white arrow) with internally stippled calcification, marginal sclerosis, and local cortical breach. CT = computed tomography
Figure 3.

Coronary reconstruction CT images show the local cortical thickening, and lytic bone destruction of medial-distal left femoral metaphysis (white arrow) with internally, stippled calcification, and marginal sclerosis. CT = computed tomography.
Figure 4.
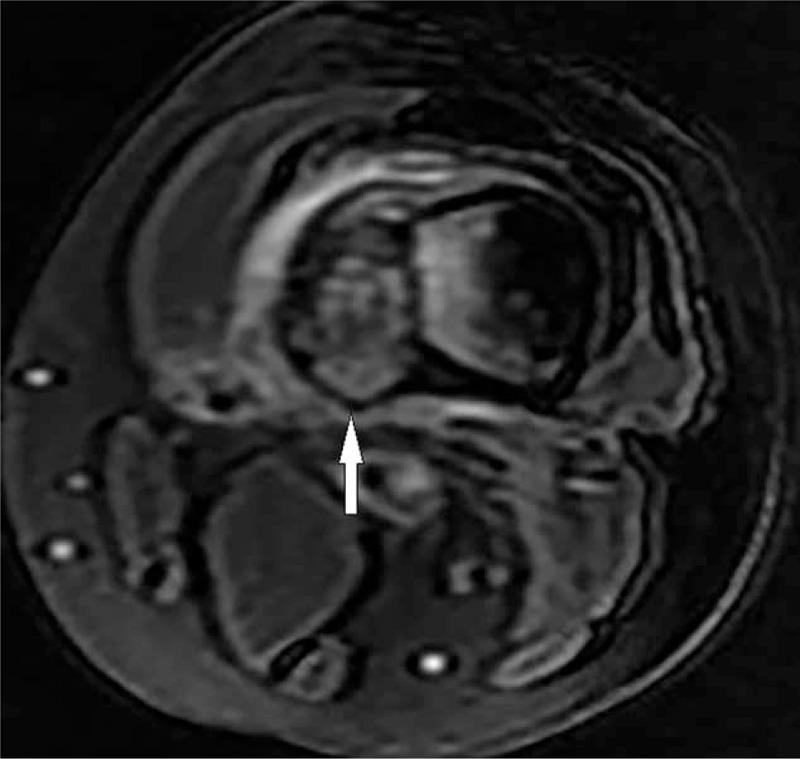
T2-FS FSE sequence shows a mixed long T2 signal mass (white arrow) with a low signal ring and peripheral edema.
Figure 5.

Coronal LAVA enhancement shows that the lesion is markedly and inhomogeneously enhanced (white arrow), and the surrounding bone and adjacent soft tissue are slightly enhanced.
The biopsy procedures were performed preoperatively and it was diagnosed as chondroblastoma. Operative procedures were chosen generally, according to biopsy results, and the extent of bone involvement. The intralesional curettage, and artificial bone grafting were performed, and intraoperative findings revealed intracortical expansive bone destruction in the distal femoral metaphysis. Subsequent histopathological examination of the surgical specimen showed that the tumor was composed of a mixture mononuclear cells, multinucleated giant cells, cartilage-like matrix, chicken-wire calcification, and small foci of bone tissue. Immunohistochemistry indicated the positivity for S100 protein. (Fig. 6). The final pathologic diagnosis was chondroblastoma. The patient survived the operation, and recovered uneventfully, was discharged after 9 days. The patient had no evidence of recurrence or metastasis 10 months after the operation.
Figure 6.
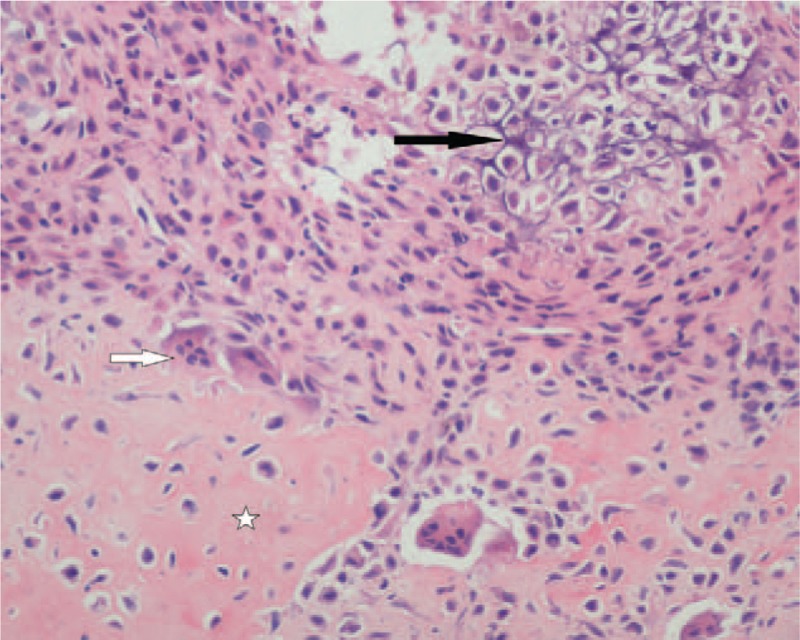
Light microscopy(hematoxylin and eosin staining,400×) reveals that chondrocytes are relatively, uniform in size and shape, with a clear boundary; eosinophilic-staining amorphous cartilage matrix (☆); osteoclast-like multinucleated giant cell (white arrow); chicken wire calcification (black arrow).
3. Discussion
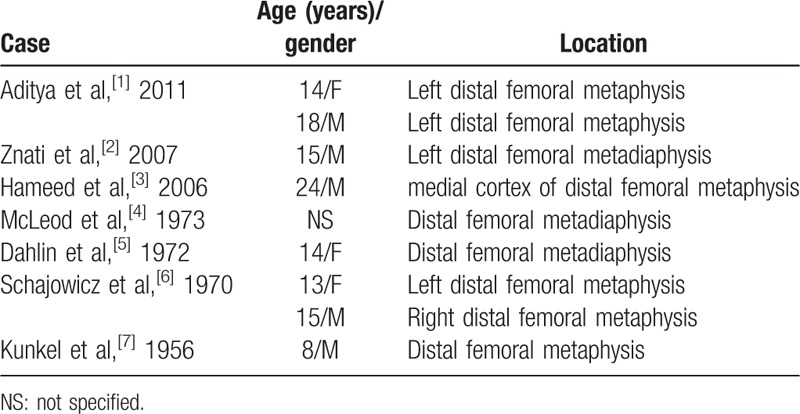
The incidence of metaphyseal or diaphyseal location in long bones accounts for only 2% of all chondroblastoma cases, and only 6 cases of metaphyseal/metadiaphyseal chondroblastoma of distal femur have been reported (Table 1).[2–8] Most chondroblastomas involve the medullary cavity, and rarely involve the cortex; furthermore, chondroblastomas originating within the cortex are rare.[9]
Table 1.
Previously reported cases of metaphyseal/metadiaphyseal chondroblastoma of distal femur.
Chondroblastomas rarely occur in the long bone metaphyseal/metadiaphyseal cortex, and only 2 cases have been designated as a long bone metaphyseal/metadiaphyseal cortex lesion in studies published in English.[2,4] It may radiographically mimic other lesions and frequently manifest as a diagnostic dilemma. In this study, we described the classical imaging features of chondroblastoma in a typical site and discussed its imaging differential diagnosis from other primary bone tumors that appear in similar sites.
Classical chondroblastoma appears as a well-defined eccentric oval lytic lesion with internal mottled calcification and a peripheral sclerotic margin. Periosteal reaction is also common. MRI shows a lobulated low T1, and variable T2 signal lesion, with a peripheral thin hypointense rim corresponding to marginal sclerosis. In contrast-enhanced MRI, the lesions show lobular, marginal, and septal enhancement. Perilesional marrow edema, soft tissue edema, and synovitis have been found in some cases.
The recognition of the classic features of chondroblastomas on plain radiography, CT, and MRI may help radiologists correctly diagnose this condition despite its unusual location. The imaging and differential diagnosis of chondroblastoma in the metaphyseal cortex of the long bone include the lesions described below (Table 2).
Table 2.
Differential diagnosis for metaphyseal/metadiaphyseal intracortical chondroblastoma of long tubular bone with other surface bone tumors.
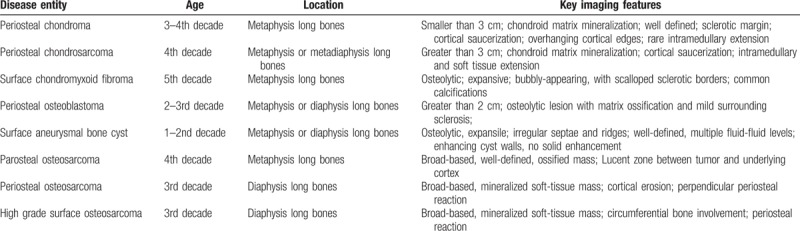
Lesion size is a distinguishing feature between periosteal chondromas and periosteal chondrosarcomas; for example, the former are typically smaller than 3 cm, whereas the latter tend to be larger than 3 cm.[10] Radiographs revealed that periosteal chondromas are soft tissue lesions with cortical scalloping, underlying cortical sclerosis, and overhanging margins. Periosteal chondrosarcomas appear as a juxtacortical soft tissue mass with chondroid matrix mineralization. In MRI, they appear as well-defined masses with a low to intermediate signal intensity on T1WI, and hyperintensity on T2WI with hypointense septa. A thin outer hypointense lining is noticeable on T2∗W gradient-echo images. Peripheral and septal enhancement may be observed in enhanced MRI.[11]
Surface chondromyxoid fibroma is radiographically characterized by a lobulated, well-defined, expansive, and osteolytic lesion with intralesional calcifications. In MRI, it appears as a lobulated hyperintense lesion on T2WI with hypointense septa and a peripheral rim.[12]
Osteoid osteoma radiographically appears as an ovoid well-defined and expansive osteolytic lesion with a central mottled or striped density. A perilesional sclerotic rim of variable thickness and a lamellar periosteal reaction may be observed. In MRI, it is isointense to the muscle on T1WI, hyperintense, or heterogeneous on T2WI, and moderate to intense enhancement after administration. Edema in the marrow and soft tissues is often prominent. Osteoblastoma usually appears more expansile, and larger than osteoid osteoma; furthermore, the former exhibits less osteosclerotic thickening of the cortex than the latter does (<2 cm).[13]
Radiographs show that an aneurysmal bone cyst (ABC) is a lobulated, expansile, and well-defined osteolytic lesion. CT may reveal cortical thinning, interrupted cortex, or periosteal reaction. ABC is hypointense on T1WI, and hyperintense on T2WI, with a hypointense rim, and internal septations. After gadolinium is administered, the septations and cyst walls may be enhanced. Fluid-fluid levels are suggestive of ABC but are non-specific. Adjacent soft tissue edema can also be observed.[14]
Parosteal osteosarcoma is radiographically described as a densely mineralized mass with irregular lobulations and attached to the underlying cortex by a broad base with a cleavage plane between the cortex and the tumor. In MRI, the tumor is hypointense on both T1WI, and T2WI because of dense osteoid components. Radiographs and CT reveal periosteal osteosarcoma as a lytic lesion with cortical erosion, and usually show a perpendicular periosteal reaction that extends into the surface soft tissue component. This tumor is low in attenuation on CT and hyperintense on T2WI due to the chondroid tissue. High-grade surface osteosarcoma often involves nearly, the entire circumference of the cortex, and likely, invades the underlying medullary cavity. Radiology findings indicate that the bulk of the lesion is external to the bone.[15]
4. Conclusion
Predilection age, predilection site, and imaging features are the major diagnostic criteria of chondroblastoma. Patients in an appropriate age group with typical imaging features, including presence of chondroid matrix, perilesional marrow, and soft tissue edema, marginal sclerosis, and periosteal reaction, may be diagnosed with chondroblastoma despite its rare location.
Author contributions
Conceptualization: Qing Wang.
Supervision: Qing Wang.
Writing – original draft: Fang Wang, Jizhen Li.
Writing – review & editing: Dexin Yu.
Footnotes
Abbreviations: CT = computed tomography, MRI = magnetic resonance imaging.
FW and JL contributed equally to this article and should be considered co-first authors.
The authors have no conflicts of interest to disclose.
References
- [1].Edel G, Ueda Y, Nakanishi J, et al. Chondroblastoma of bone. A clinical, radiological, light and immunohistochemical study. Virchows Arch A Pathol Anat Histopathol 1992;421:355–66. [DOI] [PubMed] [Google Scholar]
- [2].Maheshwari AV, Jelinek JS, Song AJ, et al. Metaphyseal and diaphyseal chondroblastomas. Skeletal Radiol 2011;40:1563–73. [DOI] [PubMed] [Google Scholar]
- [3].Znati K, Ahaouch M, Fatemi H, et al. Femoral metaphyso-diaphyseal chondroblastoma: a case report(Chondroblastome métaphyso-diaphysaire du fémur). Rev Chir Orthop Reparatrice Appar Mot 2007;93:283–7. [DOI] [PubMed] [Google Scholar]
- [4].Hameed MR, Blacksin M, Das K, et al. Cortical chondroblastoma: report of a case and literature review of this lesion reported in unusual locations. Skeletal Radiol 2006;35:295–7. [DOI] [PubMed] [Google Scholar]
- [5].McLeod RA, Beabout JW. The roentgenographic features of chondroblastoma. Am J Roentgenol Radium Ther Nucl Med 1973;118:464–71. [DOI] [PubMed] [Google Scholar]
- [6].Dahlin DC, Ivins JC. Benign chondroblastoma: a study of 125 cases. Cancer 1972;30:401–13. [DOI] [PubMed] [Google Scholar]
- [7].Schajowicz F, Gallardo H. Epiphyseal chondroblastoma of bone: a clinico-pathological study of 69 cases. J Bone Joint Surg Br 1970;52:205–26. [PubMed] [Google Scholar]
- [8].Kunkel MG, Dahlin DC, Young HH. Benign chondroblastoma. J Bone Joint Surg Am 1956;38-A:817–26. [PubMed] [Google Scholar]
- [9].Ishida T, Goto T, Motoi N, et al. Intracortical chondroblastoma mimicking intra-articular osteoid osteoma. Skeletal Radiol 2002;31:603–7. [DOI] [PubMed] [Google Scholar]
- [10].Chaabane S, Bouaziz MC, Drissi C, et al. Periosteal chondrosarcoma. AJR Am J Roentgenol 2009;192:W1–6. [DOI] [PubMed] [Google Scholar]
- [11].Robinson P, White LM, Sundaram M, et al. Periosteal chondroid tumors: radiologic evaluation with pathologic correlation. AJR Am J Roentgenol 2001;177:1183–8. [DOI] [PubMed] [Google Scholar]
- [12].Abdelwahab IF, Klein MJ. Surface chondromyxoid fibroma of the distal ulna: unusual tumor, site, and age. Skeletal Radiol 2014;43:243–6. [DOI] [PubMed] [Google Scholar]
- [13].Nakatani T, Yamamoto T, Akisue T, et al. Periosteal osteoblastoma of the distal femur. Skeletal Radiol 2004;33:107–11. [DOI] [PubMed] [Google Scholar]
- [14].Maiya S, Davies M, Evans N, et al. Surface aneurysmal bone cysts: a pictorial review. Eur Radiol 2002;12:99–108. [DOI] [PubMed] [Google Scholar]
- [15].Yarmish G, Klein MJ, Landa J, et al. Imaging characteristics of primary osteosarcoma: nonconventional subtypes. Radiographics 2010;30:1653–72. [DOI] [PubMed] [Google Scholar]


