Supplemental Digital Content is available in the text
Keywords: hypothermia, thoracic surgery, video-assisted minimally invasive surgery
Abstract
Hypothermia due to anaesthetic-induced impairment of thermoregulatory control and exposure to a cool environment is common in surgical patients. Peripheral vasodilation due to neuroaxial blockade may aggravate hypothermia. There is few data on perioperative hypothermia in patients undergoing thoracic surgery under combined general and regional anesthesia. We reviewed all thoracic surgical patients between 2006 and 2011 to determine the incidence and extent of hypothermia with or without an epidural anesthesia and evaluated its effect.
Around 339 patients underwent lung resection procedures with intraoperative forced-air warming: 197 with general and epidural anesthesia (GA + EPI), 199 with general anesthesia alone (GA). Statistical analyses were performed to determine the association between hypothermia (T < 36°C) and transfusion requirements, length of stay (LOS) in the intensive care unit (ICU), hospital LOS, and in hospital mortality.
The overall incidence of hypothermia was 64.3%. Multivariate regression analysis revealed three significant risk factors for the development of hypothermia: long induction time (P = .011), small body surface area (P = .003), and application of more fluid intraoperatively (P < .001). Factors determining the extent of hypothermia were: receiving an open thoracotomy (P = .009), placement and use of an epidural catheter (P = .002), and a lower body mass index (BMI) (P < .001). Additional epidural anesthesia reduced core temperature by 0.26°C (95% CI −0.414 to −0.095°C, P < .05). There was no difference in transfusion requirements, ICU LOS or mortality between both groups. Hospital LOS was longer in patients with hypothermia.
More than half of all thoracic patients suffered from hypothermia. A long induction time, small body surface area, and large intraoperative fluid application were independent risk factors for the development of perioperative hypothermia. Additional epidural anesthesia to general anesthesia did not increase the incidence of hypothermia but decreased body core temperature to an—albeit not clinically significant—degree. Patients scheduled for thoracic surgery will probably benefit from an additional period of prewarming prior to induction to reduce the high incidence of perioperative hypothermia.
1. Introduction
Unintentional hypothermia is defined as an accidental low body temperature.[1] The National Institute for Health and Care Excellence (NICE) estimates that 70% of patients admitted to the anaesthetic recovery room suffer from hypothermia.[2] The risk for ischaemic cardiac events (cardiac arrest, instable angina pectoris, cardiac infarction) is increased by threefold in patients with intraoperative hypothermia.[3] Furthermore, perioperative hypothermia hinders wound healing and hemostasis resulting in higher postoperative transfusion rates.[4,5]
General as well as epidural anaesthesia decreases the vasoconstriction and shivering threshold. Hence a combination of both—epidural and general anaesthesia—can promote perioperative hypothermia.[6,7] Other risk factors are the extent and the length of the surgical procedure.[8,9]
So far there are no large studies investigating the questions described above.
We reviewed all thoracic surgical patients undergoing either video-assisted minimally invasive surgery (VATS) or thoracotomy between 2006 and 2011 to determine the incidence and extent and risk factors of hypothermia. Further we set out to determine the influence of epidural anesthesia on the incidence of hypothermia.
The data gained may show how perioperative management positively or negatively influences hypothermia and how to improve the prevention of hypothermia.
2. Methods
2.1. Data extraction
This retrospective study analyzed the anaesthetic files of all patients undergoing a surgical intervention of the lung at the University Medical Center Göttingen between July 19, 2006 and February 10, 2011. All operations were documented electronically. For identifying suitable data sets we did an enquiry of the electronic documentation system AnDOK live (DATAPEC, Pliezhausen, Germany). 419 cases that complied with the criteria of pneumectomy, lobectomy or other kinds of lung resection were identified. We had to exclude data sets of 22 secondary operations. These cases were also excluded if the patients were temporally discharged between the interventions. Another 58 cases were excluded as no data on temperature was found. Finally, we were able to include 339 patients in this study. Information of postoperative LOS at the ICU, hospital LOS, and in hospital mortality were retrieved by an enquiry of the patient data management system (SAP Deutschland SE & Co. KG, Walldorf, Germany). The length of postoperative mechanical ventilation was calculated using the time of extubation, which is documented in our patient data management system ICIP (Philips Healthcare, BG Eindhoven, Netherlands).
From the anaesthetic documentation we obtained the following data:
Preoperative data such as age, ASA-Score, BMI, and comorbidities (e.g., lung impairment). Intraoperative data were obtained on anaesthetic induction time, length of anaesthesia, operation time, use of epidural anaesthesia, use of totally intravenous anesthesia (TIVA), lowest intraoperative temperature, incidence of hypothermia, warming measures, amount of intraoperative IV infusion, number of transfused packed red blood cells, platelet concentrates, and number of fresh frozen plasma concentrates. Postoperative data were documented as well: postoperative mechanical ventilation, length of postoperative mechanical ventilation, hospital LOS, ICU LOS, and hospital mortality.
The retrospective study was conducted after obtaining a positive vote from the local ethics committee Göttingen.
2.2. Statistics
2.2.1. Descriptive statistics
Relative frequency of dichotomous variables was compared using the Pearson χ2-test. Ordinal variables are described as median including interquartile range and average rank and then reviewed using the Wilcoxon–Mann–Whitney test. Normally distributed metric variables are described with mean and standard deviation using the Student's t test.
2.2.2. Logistic regression
Factors influencing the development of hypothermia and the lowest intraoperative temperature measured were analyzed by multivariate logistic regression including backward elimination using the Wald significance test, which excludes stepwise variables of the lowest informative value until only essential determining factors remain. We considered a P-value < .05 as significant.
3. Results
3.1. Descriptive statistics
The descriptive statistical analysis of patients undergoing a combination of general anaesthesia and epidural anaesthesia compared to patient undergoing only general anaesthesia is listed in and Table 1 and in the Supplementary Information.
Table 1.
Comparison of metric parameters with respect to the anesthetic procedure.
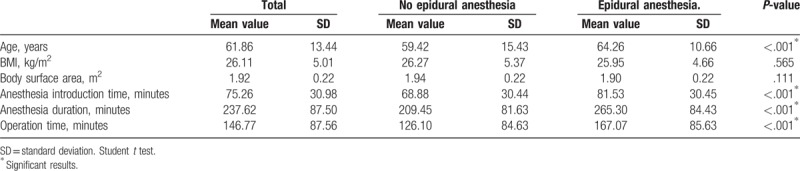
Patients undergoing general and epidural anaesthesia were more often smokers and received more frequently premedication. We detected less renal insufficiency in this group. These patients received significantly more intraoperative intravenous infusions. However, there is no difference in the preoperative ASA-Score between both the groups. These patients were also in average 5 years older than patients that underwent only general anaesthesia. Furthermore, the average induction time was 12 minutes longer in the first group as well as operation time and length of anaesthesia.
Altogether 218 of 339 patients showed perioperative hypothermia. This equals a percentage of 64.3%.
After multivariate logistic regression we identified body surface area (P-value = .006), induction time (P-value = .004), and impaired lung function (P-value = .006) as significant factors influencing the incidence hypothermia. The odds ratio for estimating the relative risk is depicted in Table 2.
Table 2.
Odds ratio of significant factors influencing the incidence of hypothermia.
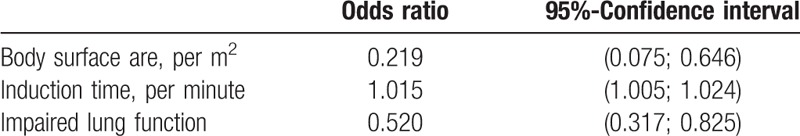
Multivariate logistic regression showed a small body surface area as factor promoting the incidence of perioperative hypothermia, while a preoperative existing lung impairment and larger body surface area were associated with a decreased incidence of perioperative hypothermia.
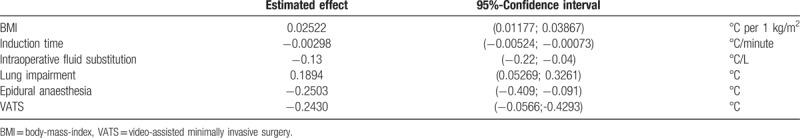
As factors significantly influencing the lowest perioperative body temperature we identified BMI (P-value < .001), induction time (P-value = .01), intraoperative fluid substitution (P-value = .005), impaired lung function (P-value = .008), epidural anaesthesia (P-value = .002), and thoracoscopy (P-value = .011)
The estimated quantitative effect of these significant factors is listed in Table 3.
Table 3.
Estimated quantitative effect of significant factors influencing the lowest body temperature measured. Multivariate logistic regression.
3.1.1. Intraoperative blood transfusion need
Overall 16 of 339 required at least 1 packed red blood cell unit. This equals a transfusion rate of 4.72%. Only 3 patients were treated with fresh frozen plasma (0.88%). No patient required transfusion of platelet concentrates. The intraoperative blood transfusion need was analyzed using the Wilcoxon–Mann–Whitney test as the data were not normally distributed (supplementary information).
No difference concerning blood transfusion need between both groups was detected.
3.1.2. Frequency and length of postoperative respiratory mechanical ventilation
There was no difference between normothermia and hypothermia concerning frequency (P = .959) and length of postoperative mechanical ventilation (P = .932, refer to Supplementary Information). Length of postoperative respiratory mechanical ventilation was analyzed using the Wilcoxin–Mann–Whitney test (Fig. 1)
Figure 1.
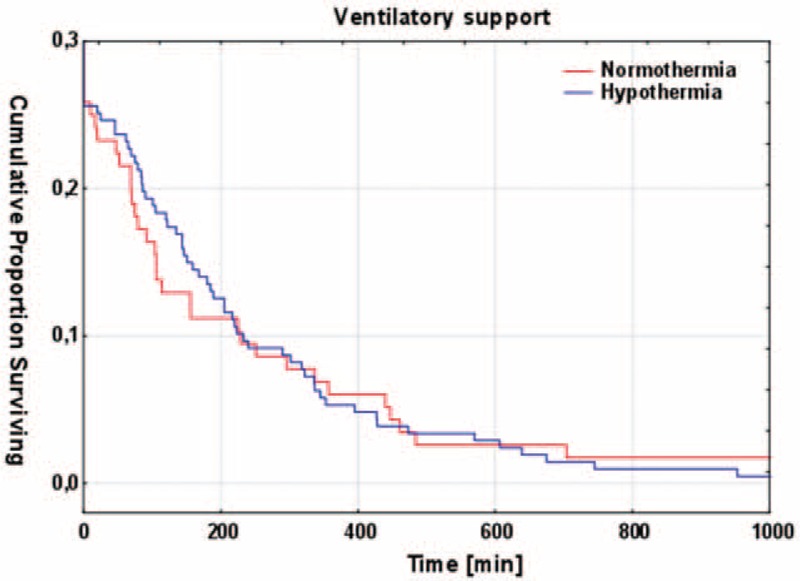
Length of postoperative respiratory assistance, normothermia compared to hypothermia. Kaplan–Meier curve.
We detected no correlation between perioperative hypothermia and frenquence and length of postoperative mechanical ventilation.
3.1.3. ICU and hospital LOS
ICU and hospital LOS were analyzed using the Wilcoxon–Mann–Whitney test. Results are depicted in Table 4 and Fig. 2. We could not detect any difference between both groups concerning ICU LOS. However, patients suffering from hypothermia were significantly earlier discharged from hospital.
Table 4.
Influence of ICU and hospital LOS on perioperative hypothermia. Wilcoxon–Mann–Whitney test.
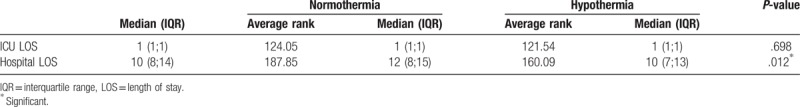
Figure 2.
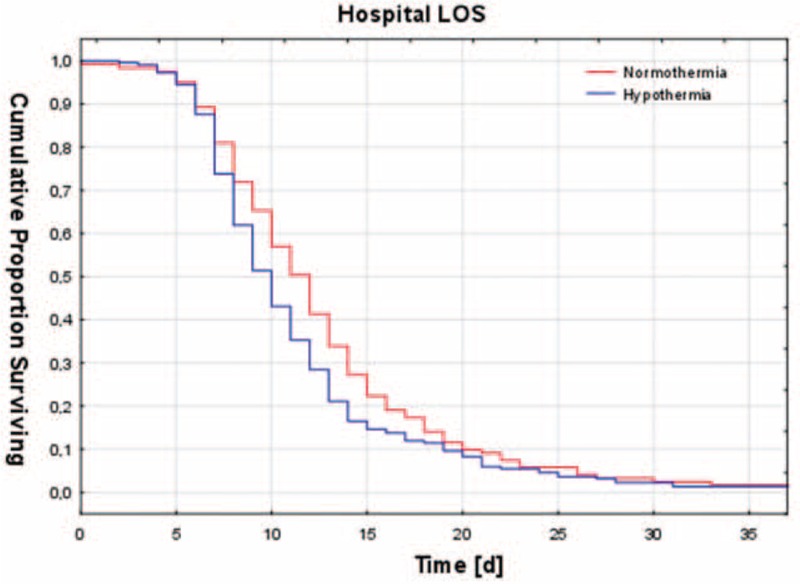
Hospital LOS. Normothermia compared to hypothermia. Kaplan–Meier curve. LOS = length of stay.
3.1.4. In hospital mortality
Perioperaitve hypothermia did not influence in hospital mortality (P = .773, Pearson χ2-test).
4. Discussion
The accidental perioperative hypothermia is a common event during surgical interventions and increases itself perioperative morbidity impairing haemostasis, wound healing, and increasing cardiac events.[10] Little is known regarding to the surgical interventions of the lung and the anaesthetic procedures described in our study, their relevance, and factors influencing hypothermia.
Our analysis of 339 cases showed an incidence of hypothermia of 64.3%. This percentage is higher than the 46% to 50% described in the literature.[10,11] However, it should be considered that most of patients included were warmed by a forced-air warming blanket laying under or above the patient. The effectivity of this procedure was shown by previous studies.[2,12] Furthermore, “hypothermia” was diagnosed in the literature by measuring body temperature at the arrival at the ICU.[10] The patients included in this study were already diagnosed with hypothermia, if intraoperative hypothermia was noted. Due to intraoperative warming procedures and the influence of operation time some of these patients might have reached normothermia already when being admitted to the ICU or anaesthetic recovery room.
4.1. Risk factors for the development and depth of hypothermia
A larger body surface (P = .008) decreased the frequency of hypothermia. There is evidence for the hypothesis that the fat tissue of overweight patients has an isolating function. Furthermore, it has been shown that these patients have a higher vasoconstriction threshold.[13,14]
Lung impairment (P = ,007) decreased the frequency of hypothermia as well. There are no studies that have found such a correlation. A possible explanation might be a more invasive ventilation or the existence of an intrinsic positive end expiratory pressure (PEEP) in patients with COPD that may influence thermoregulatory thresholds indirectly.[15]
Multivariate analysis showed that induction time (P = .004) was a hypothermia promoting factor. The effect is estimated −0.00298°C per minute in a time-dependent multivariate logistic regression model. This is plausible as patients did not receive prewarming during this time. Warming was started only after the patient arrived in the operation theatre. We could detect no influence of length of anaesthesia on the incidence of hypothermia, which mirrors the results of Abelha and Frank.[3,8] Furthermore, we observed that additional epidural anesthesia to general anesthesia did not increase the incidence of hypothermia but decreased body core temperature to an—albeit not clinically significant—degree. The decrease in body temperature during VATS might be explained by irrigation used during the procedure.
Operation time had neither an influence on the incidence of hypothermia nor on the (lowest) body temperature measured in our study. Kongsayreepong et al[9] showed that the incidence of hypothermia (<36°C) was higher when operation time exceeded 2 hours. Albeit this study did not include forced-air warming in their multivariate analysis as only half of all patients were warmed with this procedure.
4.2. Outcomes associated with hypothermia
Several studies show a higher blood transfusion needing hypothermic patients.[16] In our study, we could not confirm this as we could not find an influence of hypothermia on the transfusion rate. This may be caused by our low frequency of transfusion (4.7%) compared to other studies with a perioperative need of transfusion between 9.4% and 55.4%.[17]
In accordance to findings of Frank et al[3] we found that perioperative hypothermia did not influence the incidence and length of postoperative mechanical ventilation. Astonishingly patients with hypothermia showed a shorter hospital LOS than normothermic patients (P = .012). However, this patient group showed in the rank sum test a significantly higher ASA-score. It seems that not hypothermia or normothermia but the comorbidities of this group have led to the longer hospital LOS. This could also explain why we could not detect any difference between both groups concerning the ICU LOS.
A review by the guidelines of National Institute for Health and Clinical Excellence from 2016 yielded no studies showing a correlation between perioperative hypothermia and in hospital mortality,[2] which is confirmed by our data.
Of course, the retrospective character of this study is limiting, but the findings of this study, especially those concerning introduction time and the influence of lung impairment may be promising starting points for further studies.
Acknowledgments
We acknowledge support by the German Research Foundation and the Open Access Publication Funds of Göttingen University.
Author contributions
Conceptualization: Gereon Gries, Anselm Bräuer, Michael Quintel, Ivo F Brandes.
Data curation: Anselm Bräuer.
Formal analysis: Alexander Emmert, Gereon Gries, Saskia Wand, Anselm Bräuer, Ivo F Brandes.
Funding acquisition: Gereon Gries, Saskia Wand, Anselm Bräuer.
Investigation: Gereon Gries, Anselm Bräuer, Ivo F Brandes.
Methodology: Alexander Emmert, Judith Buentzel, Anselm Bräuer, Ivo F Brandes.
Project administration: Anselm Bräuer.
Resources: Michael Quintel.
Supervision: Anselm Bräuer, Michael Quintel, Ivo F Brandes.
Validation: Alexander Emmert, Anselm Bräuer.
Visualization: Alexander Emmert, Judith Buentzel, Anselm Bräuer, Ivo F Brandes.
Writing – original draft: Alexander Emmert.
Writing – review & editing: Judith Buentzel, Anselm Bräuer, Michael Quintel, Ivo F Brandes.
Supplementary Material
Footnotes
Abbreviation: BMI = body-mass-index, EPI = epidural anesthesia, GA = general anesthesia, ICU = intensive care unit, LOS = length of stay, TIVA = totally intravenous anaesthesia, VATS = video-assisted minimally invasive surgery.
The authors have no conflicts of interest to disclose.
Supplemental Digital Content is available for this article.
References
- [1].Aronoff DM, Neilson EG. Antipyretics: mechanisms of action and clinical use in fever suppression. Am J Med 2001;111:304–15. [DOI] [PubMed] [Google Scholar]
- [2].National Institute for Health and Clinical Excellence Inadvertent perioperative hypothermia: The management of inadvertent perioperative hypothermia in adults having surgery [Internet]. [cited Apr. 2008; Last updated Dec. 2016]. Available at: https://www.nice.org.uk/guidance/cg65/evidence. Accessed October 8, 2016. [Google Scholar]
- [3].Frank SM, Fleisher LA, Breslow MJ, et al. Perioperative maintenance of normothermia reduces the incidence of morbid cardiac events. A randomized clinical trial. JAMA 1997;277:1127–34. [PubMed] [Google Scholar]
- [4].Valeri CR, Feingold H, Cassidy G, et al. Hypothermia-induced reversible platelet dysfunction. Ann Surg 1987;205:175–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Rajagopalan S, Mascha E, Na J, et al. The effects of mild perioperative hypothermia on blood loss and transfusion requirement. Anesthesiology 2008;108:71–7. [DOI] [PubMed] [Google Scholar]
- [6].Lau LL, Hung CT, Chan CK, et al. Anaesthetic clinical indicators in public hospitals providing anaesthetic care in Hong Kong: prospective study. Hong Kong Med J 2001;7:251–60. [PubMed] [Google Scholar]
- [7].Joris J, Ozaki M, Sessler DI, et al. Epidural anesthesia impairs both central and peripheral thermoregulatory control during general anesthesia. Anesthesiology 1994;80:268–77. [DOI] [PubMed] [Google Scholar]
- [8].Abelha FJ, Castro MA, Neves AM, et al. Hypothermia in a surgical intensive care unit. BMC Anesthesiol 2005;5:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Kongsayreepong S, Chaibundit C, Chadpaibool J, et al. Predictor of core hypothermia and the surgical intensive care unit. Anesth Analg 2003;96:826–33. [DOI] [PubMed] [Google Scholar]
- [10].Karalapillai D, Story D, Hart GK, et al. Postoperative hypothermia and patient outcomes after major elective non-cardiac surgery. Anaesthesia 2013;68:605–11. [DOI] [PubMed] [Google Scholar]
- [11].Cywinski JB, Xu M, Sessler DI, et al. Predictors of prolonged postoperative endotracheal intubation in patients undergoing thoracotomy for lung resection. J Cardiothorac Vasc Anesth 2009;23:766–9. [DOI] [PubMed] [Google Scholar]
- [12].Emmert A, Franke R, Brandes IF, et al. Comparison of conductive and convective warming in patients undergoing video-assisted thoracic surgery: a prospective randomized clinical trial. Thorac Cardiovasc Surg 2017;65:362–6. [DOI] [PubMed] [Google Scholar]
- [13].Kasai T, Hirose M, Matsukawa T, et al. The vasoconstriction threshold is increased in obese patients during general anaesthesia. Acta Anaesthesiol Scand 2003;47:588–92. [DOI] [PubMed] [Google Scholar]
- [14].Kurz A, Sessler DI, Narzt E, et al. Morphometric influences on intraoperative core temperature changes. Anesth Analg 1995;80:562–7. [DOI] [PubMed] [Google Scholar]
- [15].Mizobe T, Nakajima Y, Sunaguchi M, et al. Clonidine produces a dose-dependent impairment of baroreflex-mediated thermoregulatory responses to positive end-expiratory pressure in anaesthetized humans. Br J Anaesth 2009;94:536–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Schmied H, Kurz A, Sessler DI, et al. Mild hypothermia increases blood loss and transfusion requirements during total hip arthroplasty. Lancet 1996;347:289–92. [DOI] [PubMed] [Google Scholar]
- [17].Luan H, Ye F, Wu L, et al. Perioperative blood transfusion adversely affects prognosis after resection of lung cancer: a systematic review and a meta-analysis. BMC Surg 2014;14:34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


