Abstract
There is growing recognition that impulsivity may serve as an underlying risk factor for binge eating. In addition, the association of impulsivity with binge eating may be moderated by other affective and cognitive risk factors. This study examined independent and interactive associations of negative affect, dietary restraint, and facets of impulsivity with binge eating. A diverse sample of 566 undergraduate women completed online questionnaires of study variables. Results revealed a three-way interaction of negative affect, dietary restraint, and attentional impulsivity in relation to binge eating. Women who were high on each of these three variables reported the greatest levels of binge eating. In addition, a two-way interaction was found for negative affect and nonplanning impulsivity in relation to binge eating, such that nonplanning impulsivity strengthened the association between negative affect and binge eating. Attentional and nonplanning facets of impulsivity may function as an underlying trait-level risk factor interacts with affective and/or cognitive risk (e.g., negative affect, dietary restraint) factors to predict elevated binge eating.
Keywords: Binge eating, negative affect, impulsivity, dietary restraint
Binge eating is a maladaptive eating behavior characterized by consumption of an objectively large amount of food (i.e., overeating) and an associated sense of loss of control (American Psychiatric Association, 2013) that is prominent among women (Eisenberg, Nicklett, Roeder, & Kirz, 2011; Hudson, Hiripi, Pope, & Kessler, 2007). Those who engage in binge eating are at elevated risk for negative mental and physical health problems, notably psychiatric disorders and obesity (Hudson et al., 2007; Kessler et al., 2013). A myriad of psychobiological constructs have been implicated in relation to the occurrence of binge eating, including negative affect, dietary restraint, and impulsivity (Stice, 2001; Waxman, 2009). For instance, negative affect and dietary restraint have been shown to independently and interactively predict binge eating (Stice, 2001; Stice, Akutagawa, Gaggar, & Agras, 2000). Furthermore, there is growing recognition that impulsivity may be particularly significant in the onset and maintenance of binge eating and may have an interactive influence with other risk factors (e.g., Engel et al., 2007). In the current study, we examined main effects and interactions of negative affect, restraint, and three facets of impulsivity (i.e., attentional, nonplanning, and motor impulsivity) in relation to binge eating.
Negative Affect, Restraint, and Binge Eating
Several theories suggest that binge eating functions as a maladaptive method of coping with or avoiding negative affective states (Heatherton & Baumeister, 1991; Polivy & Herman, 1993). As a result, emotional functioning disturbances are common among individuals who engage in binge eating, and the salience of negative affect in binge eating has been supported in numerous studies across a range of samples and research methodologies (Chua, Touyz, & Hill, 2004; Hudson et al., 2007; Russell, Haynos, Crow, & Fruzzetti, 2017; Smyth et al., 2007). Importantly, research investigations have shown that increased binge eating is associated with more psychological distress and disturbances in mood (Didie & Fitzgibbon, 2005; Mason & Lewis, 2014; Pinaquy et al., 2003). Also, a meta-analysis of ecological momentary assessment studies found that momentary negative affect precipitates binge eating in the natural environment, supporting the role of negative affect in the maintenance of binge eating (Haedt-Matt & Keel, 2011).
The restraint model of binge eating posits that dietary restraint (i.e., cognitive attempts to eat less to control weight/shape) also predicts binge eating via a variety of possible affective, cognitive, and physiological pathways (Hagan, Chandler, Wauford, Rybak, Oswald, 2003; Polivy & Herman, 1985). For example, individuals attempting to restrain their eating may overcompensate by binge eating due to physiological hunger or perceived deprivation. Consistent with the restraint model, a plethora of studies in non-clinical samples have shown that individuals who report more dietary restraint engage in more frequent binge eating (e.g., Holmes, Fuller-Tyszkiewicz, Skouteris, & Broadbent, 2015; Mason, Heron, Braitman, & Lewis, 2016). Thus, although the purpose of dieting is usually to lose weight, the onset of binge eating after dieting creates a paradoxical effect whereby one may actually fail to lose weight and possibly gain weight.
Furthermore, it appears that negative affect and dietary restraint appear to have an interactive effect in predisposing individuals to engage in binge eating. The distraction model of binge eating suggests that when restrained individuals experience negative affect, it interferes with their dietary vigilance, which in turn results in binge eating (Stice et al., 2000). Experimental research has produced results consistent with the distraction model (Cools, Schotte, & McNally, 1992; Schotte, Cools, & McNally, 1990). Further, in a cross-sectional test of the distraction model among men and women, an interaction was found between negative affect and dietary restraint, suggesting that those who reported high restraint and high negative affect engaged in the greatest levels of binge eating (Stice et al., 2000). Similarly, in a separate sample of college women, dietary restraint was more strongly associated with binge eating for individuals who reported high levels of life stress (Woods, Racine, & Klump, 2010).
In addition, findings from empirical classification studies suggest that BN and BED can be subtyped along the dimensions of negative affect and dietary restraint (i.e., a dietary subtype characterized by high dietary restraint and minimal negative affect and a dietary-negative affect subtype characterized by high levels of both), such that individuals of the dietary-negative affect subtype evidence the most severe ED symptoms (Carrard, Crépin, Ceschi, Golay, & Van der Linden, 2012; Chen & Le Grange, 2007; Masheb & Grilo, 2008). However, a recent daily diary study found no interaction between daily restraint and daily negative affect in predicting binge eating (Mason et al., 2016). Therefore, examining the role of other variables in the distraction model may help to clarify these mixed findings.
Impulsivity and Binge Eating
Impulsivity, characterized by the tendency for rapid and rash reactions to internal or external stimuli without regard for the negative consequences of the reaction (Evenden, 1999), has been implicated as an important neurocognitive trait associated with binge eating (Dawe & Loxton, 2004; Kane, Loxton, Staiger, & Dawe, 2004). One widely used framework for impulsivity includes three facets (Patton, Stanford, & Barratt, 1995). Attentional impulsivity involves deficits in focusing attention as well as racing and intrusive thoughts; motor impulsivity involves acting without thinking or at the spur of the moment; and nonplanning impulsivity involves lack of consideration of the future and less careful planning. When considering facets of impulsivity, research is mixed as to which are associated with binge eating. One study of 76 women found significant positive correlations between attentional, motor, and nonplanning impulsivity and binge eating (Miller & Limberg, 2011). Further, a study examining associations between particular facets of impulsivity and binge eating among bariatric surgery patients found that attentional impulsivity was positively correlated with binge eating, whereas motor and nonplanning impulsivity were unrelated (Meule, Heckel, & Kübler, 2012). Another study found that individuals with binge eating disorder only reported elevated nonplanning impulsivity compared to healthy controls (Annagur, Orhan, Ozer, Yalcin, & Tamam, 2015). Finally, in other studies, no significant bivariate associations between impulsivity facets and binge eating emerged (Brownstone et al., 2013; Meule & Platte, 2015).
Notably, findings from research based on alternative impulsivity conceptualizations, such as the model proposed by Whiteside and Lynam (2001), also supports the salience of various impulsivity facets in relation to binge eating. For instance, a meta-analysis based on this framework found small to moderate correlations for multiple facets of impulsivity in relation to bulimic symptoms (Fischer, Smith, & Cyders, 2008). Importantly, the facet that emerged as most strongly associated with bulimic symptoms was negative urgency, which reflects tendencies for negative emotion-driven impulsiveness and conceptually relates to the attentional impulsivity facet described previously (Dick et al., 2010; Fischer et al., 2008; Whiteside & Lynam, 2001). This finding thus suggests the importance of considering potential interactions of negative emotion and impulsive tendencies in relation to binge eating.
Current Study
Although empirical evidence supports the salience of negative affect, dietary restraint, and impulsivity to binge eating, little research has examined interactive relationships among these constructs in relation to binge eating. As previously described, there is evidence in support of the distraction model (Stice et al., 2000), which posits an interaction between negative affect and restraint in relation to binge eating. In addition, one study found an interaction between anger variability (assessed via ecological momentary assessment) and impulsivity among women with bulimia nervosa, such that highly impulsive individuals who were also high in anger variability were most likely to engage in binge eating (Engel et al., 2007). There is also evidence of meaningful relationships between negative affect, restraint, and impulsivity among individuals who engage in binge eating, as evidenced by a cluster analysis of individuals with BED that found those high in both negative affect and dietary restraint (compared to those only high in restraint) exhibited the highest level of negative urgency and binge eating frequency (Carrard et al., 2012).
Given this evidence, examining interactions between negative affect, dietary restraint, and impulsivity facets may further explicate underlying mechanisms of binge eating and help explain some of the discrepant findings in the literature regarding the association between impulsivity facets and binge eating. Thus, the current study examined independent and interactive associations among negative affect, dietary restraint, and facets of impulsivity in relation to binge eating. Specifically, we examined the three facets described in Barrett’s model of impulsivity (attentional, motor, and nonplanning), which conceptually overlap with the negative urgency (attentional) and lack of planning (motor and nonpanning) facets in Whiteside and Lynam’s (2001) framework. It was hypothesized that the combination of high negative affect, restraint, and impulsivity would be associated with the greatest levels of binge eating. However, which specific facet(s) of impulsivity would emerge as most salient in these interactions was an exploratory question.
Method
Participants
Undergraduate women (N = 556) at a large Mid-Atlantic university completed an online survey. All participants were recruited through the psychology department participant pool and received research credit for completing the survey. The research was approved by the university institutional review board. The mean age was 22.42 (SD = 6.61) years and the mean body mass index was 25.00 (SD = 5.98) kg/m2. The majority of women were White (46.0%) or Black (34.7%), followed by other (7.2%) and two or more races (12.0%). Seven percent of women reported being Hispanic with the other 93% being non-Hispanic. About 85% of women described their sexual identity as only heterosexual, with the other 15% including women identifying as lesbian, bisexual, mostly heterosexual, or another sexual orientation. Women were asked about past week and past month dieting in separate questions; a minority of women endorsed dieting in the past week (22%) or past month (33%).
Measures
Negative affect
The five item (Mackinnon et al., 1999) Negative Affect subscale of the Positive and Negative Affect Schedule (PANAS; Watson, Clark, & Tellegen, 1988) was used to measure negative affect. Respondents were asked to report how distressed, upset, shamed, nervous, and afraid they felt in the past week using a scale ranging from 1 (very slightly/not at all) to 5 (extremely). Higher scores indicated more negative affect. The PANAS Negative Affect subscale is a valid and reliable measure of negative affect in non-clinical samples (Crawford & Henry, 2004). Cronbach’s alpha in the current study was .82.
Dietary restraint
The Dietary Restraint subscale of the Dutch Eating Behaviors Questionnaire (DEBQ; van Strien, Frijters, Bergers, & Defares, 1986) assessed dietary restraint. The restraint subscale included ten items that participants responded to using a scale ranging from 1 (never) to 5 (very often). A sample item is: “Do you try to eat less at mealtimes than you would like to eat?” The DEBQ demonstrates adequate reliability and factor validity (van Strien, et al., 1986). Cronbach’s alpha in the current study was .94.
Impulsivity
The Barratt Impulsiveness Scale – Short Form (BIS-SF, Spinella, 2007) was used to measure trait impulsivity. There are three subscales of the BIS-SF: attentional impulsivity (e.g., “I don’t pay attention”), motor impulsivity (e.g., “I act on the spur of the moment”), and nonplanning (e.g., “I plan tasks carefully” [reverse scored]). The BIS-SF has 15 items that participants rate on a scale from 1 (rarely/never) to 4 (almost always). Spinella (2007) demonstrated the validity of the BIS-SF based on correlations with the full scale BIS as well as measures of prefrontal system function. Cronbach’s alphas in the current study were .71, .83, and .76, for attentional, motor, and nonplanning impulsivity, respectively.
Binge eating
Binge eating was measured with items derived from the Eating Disorder Inventory – Bulimia Scale (EDI-B; Garner, Olmstead, & Polivy, 1983) and the Eating Disorder Diagnostic Scale (EDDS; Stice, Telch, & Rizvi, 2000). Consistent with Sherry and Hall (2009), only the items measuring the behavioral components of binge eating (e.g., consumption of food, loss of control over eating) were used. Participants responded to four items from the EDI-B (e.g., “I ate until I was stuffed” and seven items from the EDDS (e.g., “There were times when I ate an unusually large amount of food and experienced a loss of control”). Participants rated items on a Likert-type scale ranging from 1 (strongly disagree) to 7 (strongly agree). The 11 items were summed to create one binge eating score with higher scores indicating greater binge eating severity, including more overeating and loss of control over eating. Given the self-report nature of the measure, and the lack of an objective assessment of the large amount of food criterion, this measure likely captured both objective (i.e., consumption of an objectively large amount food with a sense of loss of control over eating) and subjective (i.e., consumption of a small or normative amount of food with a sense of loss of control) binge eating behavior. Evidence suggests that this measure of binge eating represents a unidimensional factor with excellent psychometric properties (Mason & Lewis, 2016). The Cronbach’s α in this study was .94.
Statistical Analyses
Descriptive statistics were calculated for study variables (see Table 1). Ordinary least squares (OLS) multiple regressions conducted in SPSS 23.0 were used to independently examine main effects and interactions between negative affect, dietary restraint, and facets of impulsivity in relation to binge eating. All independent variables were centered and used to create interaction terms. Three multiple regression analyses were calculated: 1) negative affect, dietary restraint, and attentional impulsivity predicting binge eating; 2) negative affect, dietary restraint, and motor impulsivity predicting binge eating; and 3) negative affect, dietary restraint, and nonplanning impulsivity predicting binge eating.
Table 1.
Descriptive Statistics among Study Variables
| M | SD | 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|---|---|
| 1. Negative affect | 10.98 | 4.35 | – | .18*** | .27*** | .20*** | .07 | .36*** |
| 2. Dietary restraint | 25.86 | 9.51 | – | .10* | .04 | −.04 | .32*** | |
| 3. Attention impulsivity | 10.57 | 2.83 | – | .51*** | .35*** | .27*** | ||
| 4. Motor impulsivity | 10.16 | 3.14 | – | .24*** | .20*** | |||
| 5. Nonplanning impulsivity | 10.80 | 3.03 | – | .14** | ||||
| 6. Binge eating | 24.60 | 14.82 | – |
p < .001,
p < .01,
p < .05
Results
Prior to conducting the analyses, patterns of missing data were examined: 12.95% of participants (n = 72) were missing at least one value and 2.67% of total values were missing. Binge eating had the highest amount of missing data with 24 individuals missing binge eating data (4.3% of total sample). The expectation-maximization (EM) algorithm was used to replace missing values. Bivariate correlations showed that negative affect, dietary restraint, and the three impulsivity facets were all significantly and positively associated with binge eating (see Table 1).
Negative Affect, Dietary Restraint, and Attentional Impulsivity
Table 2 displays the results of the first multiple regression. Main effects were significant for negative affect, dietary restraint, and attentional impulsivity. The two-way interaction between negative affect and attentional impulsivity was significant, as well as the three-way interaction among negative affect, dietary restraint, and attentional impulsivity. The interaction depicted in Figure 1 shows that the combination of high negative affect, high restraint, and high attentional impulsivity is associated with the highest levels of binge eating.
Table 2.
Main Effects and Interaction of NA, Restraint, and Attentional Impulsivity Predicting Binge Eating
| B | β | CI | R | R2 | F | |
|---|---|---|---|---|---|---|
| .50 | .25 | 26.54* | ||||
| NA | .91 | .27 | [.65, 1.17] | |||
| Dietary restraint | .38 | .24 | [.26, .50] | |||
| Attention | .75 | .14 | [.35, 1.16] | |||
| NA X Dietary restraint | −.001 | −.003 | [−.03, .02] | |||
| NA X Attention | .90 | .09 | [.01, .17] | |||
| Dietary restraint X Attention | .04 | .07 | [−.003, .08] | |||
| NA X Dietary restraint X Attention | .01 | .10 | [.001, .02] |
Note. NA = negative affect. For individual predictors, CIs that do not include 0 are significant (bolded).
p < .001.
Figure 1.
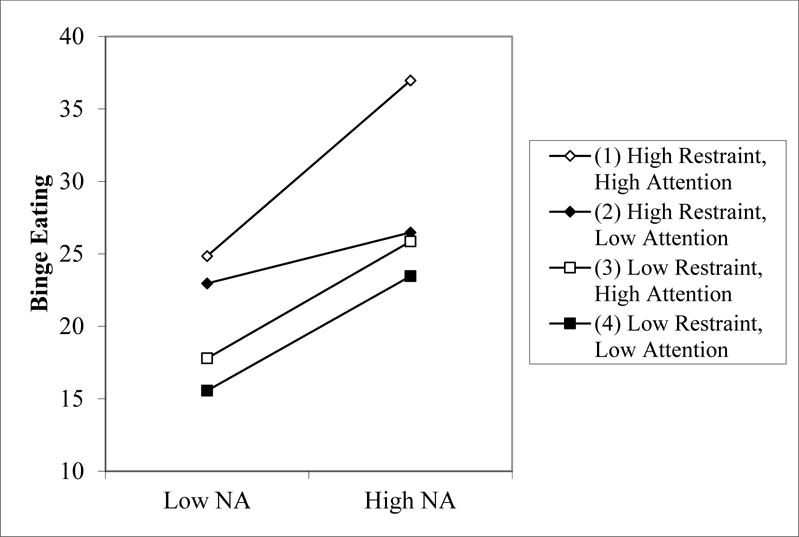
Three way interaction of negative affect (NA), restraint, and attentional impulsivity in relation to binge eating.
Negative Affect, Dietary Restraint, and Motor Impulsivity
Table 3 shows the results of the multiple regression. Main effects were significant for negative affect, dietary restraint, and motor impulsivity. There were no significant interactions.
Table 3.
Main Effects and Interaction of NA, Restraint, and Motor Impulsivity Predicting Binge Eating
| B | β | CI | R | R2 | F | |
|---|---|---|---|---|---|---|
| .48 | .23 | 22.97* | ||||
| NA | .98 | .29 | [.72, 1.24] | |||
| Dietary restraint | .41 | .26 | [.29, .53] | |||
| Motor | .57 | .12 | [.20, .93] | |||
| NA X Dietary restraint | .01 | .03 | [−.02, .03] | |||
| NA X Motor | .03 | .04 | [−.04, .10] | |||
| Dietary restraint X Motor | .03 | .07 | [−.003, .07] | |||
| NA X Dietary restraint X Motor | .000 | .00 | [−.01, .01] |
Note. NA = negative affect. For individual predictors, CIs that do not include 0 are significant (bolded).
p < .001.
Negative Affect, Dietary Restraint, and Nonplanning Impulsivity
Table 4 shows the results of the multiple regression. Main effects were significant for negative affect, dietary restraint, and nonplanning impulsivity. The two-way interaction between negative affect and nonplanning impulsivity was significant. No other interactions were significant. The interaction depicted in Figure 2 demonstrates that nonplanning impulsivity strengthened the association between negative affect and binge eating, such that high nonplanning impulsivity in combination with high negative affect was associated with the greatest levels of binge eating.
Table 4.
Main Effects and Interaction of NA, Restraint, and Nonplanning Impulsivity Predicting Binge Eating
| B | β | CI | R | R2 | F | |
|---|---|---|---|---|---|---|
| .50 | .25 | 25.52* | ||||
| NA | 1.06 | .31 | [.81, 1.32] | |||
| Dietary restraint | .42 | .27 | [.30, .54] | |||
| Nonplanning | .53 | .11 | [.16, .89] | |||
| NA X Dietary restraint | .02 | .05 | [−.01, .04] | |||
| NA X Nonplanning | .13 | .13 | [.05, .20] | |||
| Dietary restraint X Nonplanning | .03 | .06 | [−.01, .06] | |||
| NA X Dietary restraint X Nonplanning | .01 | .07 | [−.001, .01] |
Note. NA = negative affect. For individual predictors, CIs that do not include 0 are significant (bolded).
p < .001.
Figure 2.
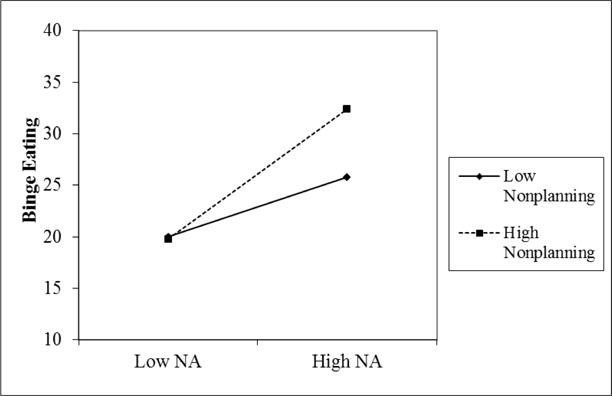
Two way interaction of negative affect (NA) and nonplanning impulsivity in relation to binge eating.
Discussion
The purpose of this study was to examine the independent and interactive associations of negative affect, dietary restraint, and three facets of impulsivity (i.e., attentional, motor, and nonplanning) with binge eating. Results indicated that negative affect, dietary restraint, and each of the three facets of impulsivity were positively correlated with binge eating. Significant positive associations of negative affect and restraint with binge eating are consistent with existing theories (e.g., dual pathway model; Stice, 2001) and previous empirical research (e.g., Haedt-Matt & Keel, 2011; Mason et al., 2016). Further, in contrast to findings from certain previous studies (e.g., Annagur et al., 2015; Brownstone et al., 2013; Meule, Heckel, & Kübler, 2012), we found associations between each of the three facets of impulsivity and binge eating. Mixed findings may be due to differences in sample (e.g., clinical vs. non-clinical) or varying measures of binge eating (e.g., Likert-type scales vs. episode count vs. diagnosis). Our findings suggest that in a diverse sample of college women, greater scores on attentional, motor, and nonplanning impulsivity are associated with greater severity of self-reported binge eating assessed with Likert-type items. This approach may represent a more integrated conceptualization of binge eating pathology that could be more sensitive than other measures that have been used, such as frequency of binge eating. In addition, assessments of binge eating frequency may be more subject to retrospective recall biases given the difficulty of remembering specific eating episodes, especially given that assessment of binge eating frequency typically focuses on the past month.
There was a significant three-way interaction among negative affect, dietary restraint, and attentional impulsivity associated with binge eating. However, there were no significant three way interactions involving motor or nonplanning impulsivity, and additionally, the two-way interactions between negative affect and restraint were not significant in models including motor or nonplanning impulsivity. This suggests specificity of the interaction of negative affect and restraint to attentional impulsivity. That is, the interaction between negative affect and restraint appears to be dependent upon level of attentional impulsivity rather than other forms of impulsivity. Notably, the finding that this interaction was unique to the attentional impulsivity facet is consistent with the apparent salience of negative urgency, which is conceptually related to attentional impulsivity, in relation to bulimic symptoms (Fischer et al., 2008).
The three-way interaction among negative affect, dietary restraint, and attentional impulsivity is consistent with the distraction model (Stice et al., 2000). It appears that women who are attempting to restrict their caloric intake are more likely to engage in binge eating if they also report a tendency for experiencing greater aversive affect, and this effect is strongest specifically for women that also have more impulsivity-related attentional difficulties. Thus, attentional impulsivity may serve as a trait-based neurocognitive risk factor for binge eating that interacts with cognitive and affective risk factors. The specificity of our findings with respect to attentional impulsivity is also interesting in light of previous studies that found only attentional impulsivity was associated with concerns about dieting (van Koningsbruggen, Stroebe, & Aarts, 2013), eating concerns (von Ranson, Wallace, Hollub, & Hodgins, 2013), and pleasantness ratings of high-calorie foods (Nolan, 2012); moreover, it has been suggested that attentional impulsivity is most strongly related to overeating compared to other BIS subscales (Muele, 2013). This is also in line with Fischer and colleagues’ (2008) meta-analytic finding that, of the facets in the Lynam and Whiteside (2001) model, negative urgency was most strongly associated with bulimic symptoms.
One possible interpretation of the three-way interaction is that the tendency to be less attentive may interfere with restrained individuals’ ability to engage in goal-directed behavior (i.e., less caloric intake), especially when experiencing negative affective states. Essentially, with multiple demands requiring these women’s attention, such as limiting caloric intake and managing emotions, women with increased attentional impulsivity may have decreased ability to attend to all demands; regulating emotion may become more important in the moment than more long-term goals (e.g., losing weight by restricting calories) (see Loth et al., 2015). Consistent with this assertion, in patients with BED, attentional impulsivity was related to decreased response inhibition, or ability to suppress actions inconsistent with goal-directed behavior (Hege et al., 2015). In addition, others have suggested that individuals with higher attentional impulsivity are more susceptible to be distracted by palatable food cues, which could predispose individuals to binge eating (Hou, Mogg, Bradley, Moss-Morris, Peveler, & Roefs, 2011); furthermore, this effect may be magnified among who are attempting to restrict their intake and who may therefore be more sensitive to such cues.
In addition to the three way-interaction involving negative affect and attentional impulsivity, we found a significant two-way interaction between nonplanning impulsivity and negative affect, such that nonplanning impulsivity strengthened the association between negative affect and binge eating. Individuals who are less careful at planning may be more likely to engage in binge eating, regardless of levels of restraint, because they may be less able to plan meals and snacks. Thus, when experiencing negative affect, both restrained and non-restrained individuals may be similarly likely to engage in binge eating due to failure to plan meals. These interactions are congruent with research showing that binge eating is associated with a tendency to act more impulsively when experiencing negative affect, (i.e., negative urgency; Fischer, Peterson, & McCarthy, 2013; Kelly, Cotter, & Mazzeo, 2014), and are consistent with previous studies showing associations between nonplanning impulsivity and binge eating (Miller & Limberg, 2011) and binge eating disorder (Annagur et al., 2015). Taken together, the current findings suggest that both attentional and nonplanning impulsivity may be relevant to negative urgency, and the influence of attentional impulsivity is particularly in the context of high levels of restraint.
Our study has several notable strengths and limitations. A strength of this study included recruitment of a diverse sample of women with regard to race, sexual orientation, and BMI. However, given this was a convenience sample of college women from one university, generalizability of the findings to other groups including clinical populations is limited. Relatedly, since we did conduct diagnostic interviews, the extent to which the sample included participants with full-threshold eating disorders is unclear. Furthermore, while we used traditional self-report measures that demonstrated adequate psychometric properties, self-report measures are limited by a number of inherent biases, notably retrospective recall bias. Future studies could benefit from the use of multimodal assessment methods, including ecological momentary assessment, neurocognitive measures, behavioral tasks, and neuroimaging. In addition, we assessed binge eating with Likert-type items focused on components of binge eating behavior (e.g., overeating, loss of control eating); this approach may have captured both objective and subjective binge eating behavior. It may be important in future research to determine if different processes distinguish between objective and subjective binge eating. However, research indicates that the loss of control feature of binge eating, regardless of quantity consumed, appears to be most clinically relevant (e.g., Jenkins et al., 2012; Mond et al., 2010). Regarding the measure of impulsivity, the BIS assesses multiple facets, but does not directly assess other facets identified in alternative models (e.g., lack of perseverance, sensation seeking, negative urgency). Additional research utilizing other measures such as the UPPS Impulsive Behavior Scale (Whiteside & Lynam, 2001) will help to clarify whether the interactive associations found in this study may also apply to these other facets of impulsivity. Further, the correlational design of this study limits ability to make causal inferences from the data. Future studies using experimental and longitudinal designs are needed to replicate and extend our findings and make inferences about causality.
In the current study, we examined how individual differences in negative affect and impulsivity were associated with binge eating. Future studies should examine how momentary negative affect and impulsivity are associated with binge eating using ecological momentary assessment and laboratory-based experimental designs. Also, future research should examine how specific facets of negative affect (e.g., sadness, anger, guilt) interact with various facets of impulsivity in relation to binge eating. Finally, studies should replicate findings in samples of individuals with eating disorders. This would also include understanding the relevance of the current findings to specific disorders, such as bulimia nervosa and binge eating disorder.
Overall, our results show that the combination of negative affect, restraint, and attentional impulsivity is associated with the highest levels of binge eating. Also, high levels of nonplanning impulsivity and negative affect may increase risk for binge eating. While modification of one or more of these risk factors could potentially result in reductions in binge eating, targeting all these three risk factors may theoretically be most efficacious in reducing binge eating. Treatments for binge eating have been previously developed that focus on reducing negative affect and emotion dysregulation (e.g., integrative cognitive affective therapy; ICAT; Wonderlich et al., 2015) and rigid dietary restraint (e.g., cognitive behavior therapy-enhanced, CBT-E; Fairburn, 2008). Recently treatments have also emerged that explicitly target impulsivity-related mechanisms (i.e., cognitive control training; Juarascio, Manasse, Espel, Kerrigan, & Forman, 2015) and attentional control (i.e., attentional bias modification; Renwick, Campbell, & Schmidt, 2013), though empirical support for these approaches is preliminary. Thus, the present findings lend support for further study of novel approaches that combine elements from each of these therapeutic approaches.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th. Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- Annagur BB, Orhan O, Ozer A, Yalcin N, Tamam L. The effects of depression and impulsivity on obesity and binge eating disorder. Klinik Psikofarmakoloji Bulteni. 2015;25:162–70. [Google Scholar]
- Brownstone LM, Bardone-Cone AM, Fitzsimmons-Craft EE, Printz KS, Le Grange D, Mitchell JE, Wonderlich SA. Subjective and objective binge eating in relation to eating disorder symptomatology, negative affect, and personality dimensions. International Journal of Eating Disorders. 2013;46:66–76. doi: 10.1002/eat.22066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carrard I, Crépin C, Ceschi G, Golay A, Van der Linden M. Relations between pure dietary and dietary-negative affect subtypes and impulsivity and reinforcement sensitivity in binge eating individuals. Eating Behaviors. 2012;13:13–19. doi: 10.1016/j.eatbeh.2011.10.004. [DOI] [PubMed] [Google Scholar]
- Chen EY, Le Grange D. Subtyping adolescents with bulimia nervosa. Behaviour Research and Therapy. 2007;45:2813–2820. doi: 10.1016/j.brat.2007.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chua JL, Touyz S, Hill AJ. Negative mood-induced overeating in obese binge eaters: an experimental study. International Journal of Obesity. 2004;28:606–610. doi: 10.1038/sj.ijo.0802595. [DOI] [PubMed] [Google Scholar]
- Cools J, Schotte DE, McNally RJ. Emotional arousal and overeating in restrained eaters. Journal of Abnormal Psychology. 1992;101:348–351. doi: 10.1037//0021-843x.101.2.348. [DOI] [PubMed] [Google Scholar]
- Crawford JR, Henry JD. The Positive and Negative Affect Schedule (PANAS): Construct validity, measurement properties and normative data in a large non-clinical sample. British Journal of Clinical Psychology. 2004;43:245–265. doi: 10.1348/0144665031752934. [DOI] [PubMed] [Google Scholar]
- Dawe S, Loxton NJ. The role of impulsivity in the development of substance use and eating disorders. Neuroscience & Biobehavioral Reviews. 2004;28:343–351. doi: 10.1016/j.neubiorev.2004.03.007. [DOI] [PubMed] [Google Scholar]
- Dick DM, Smith G, Olausson P, Mitchell SH, Leeman RF, O’Malley SS, Sher K. Understanding the construct of impulsivity and its relationship to alcohol use disorders. Addiction Biology. 2010;15:217–226. doi: 10.1111/j.1369-1600.2009.00190.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Didie ER, Fitzgibbon M. Binge eating and psychological distress: Is the degree of obesity a factor? Eating Behaviors. 2005;6:35–41. doi: 10.1016/j.eatbeh.2004.08.007. [DOI] [PubMed] [Google Scholar]
- Eisenberg D, Nicklett EJ, Roeder K, Kirz NE. Eating disorder symptoms among college students: Prevalence, persistence, correlates, and treatment-seeking. Journal of American College Health. 2011;59:700–707. doi: 10.1080/07448481.2010.546461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engel SG, Boseck JJ, Crosby RD, Wonderlich SA, Mitchell JE, Smyth J, Steiger H. The relationship of momentary anger and impulsivity to bulimic behavior. Behaviour Research and Therapy. 2007;45:437–447. doi: 10.1016/j.brat.2006.03.014. [DOI] [PubMed] [Google Scholar]
- Evenden JL. Varieties of impulsivity. Psychopharmacology. 1999;146:348–361. doi: 10.1007/PL00005481. [DOI] [PubMed] [Google Scholar]
- Fischer S, Smith GT, Cyders MA. Another look at impulsivity: A meta-analytic review comparing specific dispositions to rash action in their relationship to bulimic symptoms. Clinical Psychology Review. 2008;28:1413–1425. doi: 10.1016/j.cpr.2008.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garner DM, Olmstead MP, Polivy J. Development and validation of a multidimensional eating disorder inventory for anorexia nervosa and bulimia. International Journal of Eating Disorders. 1983;2:15–34. [Google Scholar]
- Haedt-Matt AA, Keel PK. Revisiting the affect regulation model of binge eating: a meta-analysis of studies using ecological momentary assessment. Psychological Bulletin. 2011;137:660–681. doi: 10.1037/a0023660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagan MM, Chandler PC, Wauford PK, Rybak RJ, Oswald KD. The role of palatable food and hunger as trigger factors in an animal model of stress induced binge eating. International Journal of Eating Disorders. 2003;34:183–197. doi: 10.1002/eat.10168. [DOI] [PubMed] [Google Scholar]
- Heatherton TF, Baumeister RF. Binge eating as escape from self-awareness. Psychological Bulletin. 1991;110:86–108. doi: 10.1037/0033-2909.110.1.86. [DOI] [PubMed] [Google Scholar]
- Hege MA, Stingl KT, Kullmann S, Schag K, Giel KE, Zipfel S, Preissl H. Attentional impulsivity in binge eating disorder modulates response inhibition performance and frontal brain networks. International Journal of Obesity. 2015;39:353–360. doi: 10.1038/ijo.2014.99. [DOI] [PubMed] [Google Scholar]
- Holmes M, Fuller-Tyszkiewicz M, Skouteris H, Broadbent J. Understanding the link between body image and binge eating: a model comparison approach. Eating and Weight Disorders. 2015;20:81–89. doi: 10.1007/s40519-014-0141-4. [DOI] [PubMed] [Google Scholar]
- Hou R, Mogg K, Bradley BP, Moss-Morris R, Peveler R, Roefs A. External eating, impulsivity and attentional bias to food cues. Appetite. 2011;56:424–427. doi: 10.1016/j.appet.2011.01.019. [DOI] [PubMed] [Google Scholar]
- Hudson J, Hiripi E, Pope H, Kessler R. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biological Psychiatry. 2007;61:348–358. doi: 10.1016/j.biopsych.2012.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jenkins PE, Conley CS, Rienecke Hoste R, Meyer C, Blissett JM. Perception of control during episodes of eating: relationships with quality of life and eating psychopathology. International Journal of Eating Disorders. 2012;45:115–119. doi: 10.1002/eat.20913. [DOI] [PubMed] [Google Scholar]
- Juarascio AS, Manasse SM, Espel HM, Kerrigan SG, Forman EM. Could training executive function improve treatment outcomes for eating disorders? Appetite. 2015;90:187–193. doi: 10.1016/j.appet.2015.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kane TA, Loxton NJ, Staiger PK, Dawe S. Does the tendency to act impulsively underlie binge eating and alcohol use problems? An empirical investigation. Personality and Individual Differences. 2004;36:83–94. doi: 10.1016/S0191-8869(03)00070-9. [DOI] [Google Scholar]
- Loth KA, Goldschmidt AB, Wonderlich SA, Lavender JM, Neumark-Sztainer D, Vohs KD. Could the resource depletion model of self-control help the field to better understand momentary processes that lead to binge eating? International Journal of Eating Disorders. 2016;49:998–1001. doi: 10.1002/eat.22641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackinnon A, Jorm AF, Christensen H, Korten AE, Jacomb PA, Rodgers B. A short form of the Positive and Negative Affect Schedule: Evaluation of factorial validity and invariance across demographic variables in a community sample. Personality and Individual Differences. 1999;27:405–416. doi: 10.1016/S0191-8869(98)00251-7. [DOI] [Google Scholar]
- Masheb RM, Grilo CM. Prognostic significance of two sub-categorization methods for the treatment of binge eating disorder: Negative affect and overvaluation predict, but do not moderate, specific outcomes. Behaviour Research and Therapy. 2008;46:428–437. doi: 10.1016/j.brat.2008.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason TB, Heron KE, Braitman AL, Lewis RJ. A daily diary study of perceived social isolation, dietary restraint, and negative affect in binge eating. Appetite. 2016;97:94–100. doi: 10.1016/j.appet.2015.11.027. [DOI] [PubMed] [Google Scholar]
- Mason TB, Lewis RJ. Profiles of binge eating: The interaction of depressive symptoms, eating styles, and body mass index. Eating Disorders. 2014;22:450–460. doi: 10.1080/10640266.2014.931766. [DOI] [PubMed] [Google Scholar]
- Mason TB, Lewis RJ. Minority stress, body shame, and binge eating among lesbian women social anxiety as a linking mechanism. Psychology of Women Quarterly. 2016;40:428–440. doi: 10.1177/0361684316635529. [DOI] [Google Scholar]
- Meule A. Impulsivity and overeating: A closer look at the subscales of the Barratt Impulsiveness Scale. Frontiers in Psychology. 2013;4:177. doi: 10.3389/fpsyg.2013.00177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meule A, Heckel D, Kübler A. Factor structure and item analysis of the Yale Food Addiction Scale in obese candidates for bariatric surgery. European Eating Disorder Review. 2012;20:419–422. doi: 10.1002/erv.2189. [DOI] [PubMed] [Google Scholar]
- Meule A, Platte P. Facets of impulsivity interactively predict body fat and binge eating in young women. Appetite. 2015;87:352–357. doi: 10.1016/j.appet.2015.01.003. [DOI] [PubMed] [Google Scholar]
- Miller KY, Limberg B. Binge eating behaviors and motoric, attentional, and nonplanning impulsivity. Graduate Student Journal of Psychology. 2011;13:45–51. [Google Scholar]
- Mond JM, Latner JD, Hay PH, Owen C, Rodgers B. Objective and subjective bulimic episodes in the classification of bulimic-type eating disorders: another nail in the coffin of a problematic distinction. Behaviour Research and Therapy. 2010;48:661–669. doi: 10.1016/j.brat.2010.03.020. [DOI] [PubMed] [Google Scholar]
- Nolan LJ. Association between impulsiveness and pleasantness ratings for food and drugs. Appetite. 2012;59:e43. doi: 10.1016/j.appet.2012.05.003. [DOI] [Google Scholar]
- Patton JH, Stanford MS, Barratt ES. Factor structure of the Barratt Impulsiveness Scale. Journal of Clinical Psychology. 1995;51:768–774. doi: 10.1002/1097-4679(199511)51:6<768::aid-jclp2270510607>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- Pinaquy S, Chabrol H, Simon C, Louvet JP, Barbe P. Emotional eating, alexithymia, and binge-eating disorder in obese women. Obesity. 2003;11:195–201. doi: 10.1038/oby.2003.31. [DOI] [PubMed] [Google Scholar]
- Polivy J, Herman CP. Dieting and binging: A causal analysis. American Psychologist. 1985;40:193–201. doi: 10.1037/0003-066X.40.2.193. [DOI] [PubMed] [Google Scholar]
- Polivy J, Herman CP. Etiology of binge eating: Psychological mechanisms. In: Fairburn F, Wilson G, editors. Binge eating: Nature, assessment, and treatment. New York: Guilford Press; 1993. pp. 173–205. [Google Scholar]
- Renwick B, Campbell IC, Schmidt U. Attention bias modification: A new approach to the treatment of eating disorders? International Journal of Eating Disorders. 2013;46:496–500. doi: 10.1002/eat.22107. [DOI] [PubMed] [Google Scholar]
- Russell SL, Haynos AF, Crow SJ, Fruzzetti AE. An experimental analysis of the affect regulation model of binge eating. Appetite. 2017;110:44–50. doi: 10.1016/j.appet.2016.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schotte DE, Cools J, McNally RJ. Film-induced negative affect triggers overeating in restrained eaters. Journal of Abnormal Psychology. 1990;99:317–320. doi: 10.1037/0021-843X.99.3.317. [DOI] [PubMed] [Google Scholar]
- Sherry SB, Hall PA. The perfectionism model of binge eating: Tests of an integrative model. Journal of Personality and Social Psychology. 2009;96:690–709. doi: 10.1037/a0014528. [DOI] [PubMed] [Google Scholar]
- Smyth JM, Wonderlich SA, Heron KE, Sliwinski MJ, Crosby RD, Mitchell JE, Engel SG. Daily and momentary mood and stress are associated with binge eating and vomiting in bulimia nervosa patients in the natural environment. Journal of Consulting and Clinical Psychology. 2007;75:629–638. doi: 10.1037/0022-006X.75.4.629. [DOI] [PubMed] [Google Scholar]
- Spinella M. Normative data and a short form of the Barratt Impulsiveness Scale. International Journal of Neuroscience. 2007;117:359–368. doi: 10.1080/00207450600588881. [DOI] [PubMed] [Google Scholar]
- Stice E. A prospective test of the dual-pathway model of bulimic pathology: mediating effects of dieting and negative affect. Journal of Abnormal Psychology. 2001;110:124–135. doi: 10.1037/0021-843X.110.1.124. [DOI] [PubMed] [Google Scholar]
- Stice E, Akutagawa D, Gaggar A, Agras WS. Negative affect moderates the relation between dieting and binge eating. International Journal of Eating Disorders. 2000;27:218–229. doi: 10.1002/(SICI)1098-108X(200003)27:2<218::AID-EAT10>3.0.CO;2-1. [DOI] [PubMed] [Google Scholar]
- Stice E, Telch CF, Rizvi SL. Development and validation of the Eating Disorder Diagnostic Scale: a brief self-report measure of anorexia, bulimia, and binge-eating disorder. Psychological Assessment. 2000;12:123–131. doi: 10.1037/1040-3590.12.2.123. [DOI] [PubMed] [Google Scholar]
- van Koningsbruggen GM, Stroebe W, Aarts H. Successful restrained eating and trait impulsiveness. Appetite. 2013;60:81–84. doi: 10.1016/j.appet.2012.09.016. [DOI] [PubMed] [Google Scholar]
- van Strien T, Frijters JE, Bergers G, Defares PB. The Dutch Eating Behavior Questionnaire (DEBQ) for assessment of restrained, emotional, and external eating behavior. International Journal of Eating Disorders. 1986;5:295–315. doi: 10.1002/1098-108X(198602)5:2<295::AID-EAT2260050209>3.0.CO;2-T. [DOI] [Google Scholar]
- von Ranson KM, Wallace LM, Holub A, Hodgins DC. Eating disorders, substance use disorders, and impulsiveness among disordered gamblers in a community sample. European Eating Disorders Review. 2013;21:148–154. doi: 10.1002/erv.2207. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. Journal of Personality and Social Psychology. 1988;54:1063–1070. doi: 10.1037/0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Waxman SA. A systematic review of impulsivity in eating disorders. European Eating Disorders Review. 2009;17:408–425. doi: 10.1002/erv.952. [DOI] [PubMed] [Google Scholar]
- Whiteside SP, Lynam DR. The five factor model and impulsivity: Using a structural model of personality to understand impulsivity. Personality and individual differences. 2001;30:669–689. doi: 10.1016/S0191-8869(00)00064-7. [DOI] [Google Scholar]
- Wonderlich SA, Peterson CB, Smith TL, Klein MH, Mitchell JE, Crow SJ. Integrative cognitive-affective therapy for bulimia nervosa: A treatment manual. Guilford Publications; 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woods AM, Racine SE, Klump KL. Examining the relationship between dietary restraint and binge eating: Differential effects of major and minor stressors. Eating Behaviors. 2010;11:276–280. doi: 10.1016/j.eatbeh.2010.08.00. [DOI] [PubMed] [Google Scholar]


