Supplemental Digital Content is available in the text
Keywords: comorbidities, hemophilia, workers, workplace health management
Abstract
Multiple comorbidities, especially musculoskeletal dysfunction and cerebrovascular disease, remain barriers to normal social participation among persons with hemophilia (PWH). However, the relative health effects of such comorbidities on workers with hemophilia have seldom been explored. In this study, we investigated the incidence of comorbidities and their risk factors among workers with hemophilia.
The study compared the incidence and risk factors of the major comorbidities of 411 workers with hemophilia enrolled in Taiwan's National Health Insurance Research Database between 1997 and 2010 with an age- and sex-matched general population.
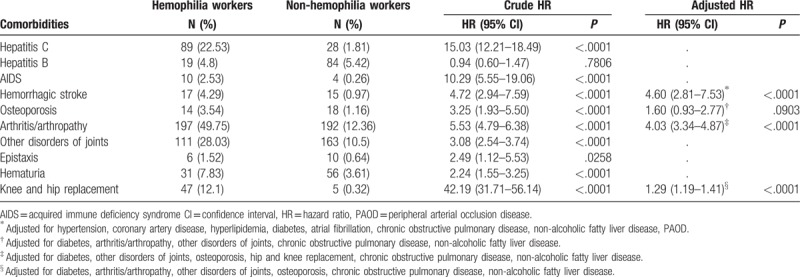
Compared with the general population, workers with hemophilia had higher risks for hemorrhagic stroke, arthritis/arthropathy, and knee/hip replacement among workers with hemophilia after multivariate adjustment, with hazard ratios (95% CI) of 4.60 (2.81–7.53), 4.03 (3.34–4.87), and 1.29 (1.10–1.41), respectively.
Disorder of joints, hemophilia-related arthritis/arthropathy, hemorrhagic stroke, and knee/hip replacement remain significant comorbidities among workers with hemophilia, which will result in increased social burden. Policymakers and employers should apply appropriate interventions to help prevent productivity losses, reduced workforce participation, sick leave, and work disability among hemophilia workers.
1. Introduction
Hemophilia is a rare hereditary bleeding disorder resulting from the absence or deficiency of coagulation factors and is characterized by increased bleeding into joints and muscles.[1,2] Repeated bleeding into joints may result in physical disability owing to hemophilic arthritis and thus restrict social participation among persons with hemophilia (PWH).[3] Since the introduction of clotting factor concentrates (CFCs), regular prophylaxis and more comprehensive care, the life expectancy, and quality of life of PWH have increased significantly.[4,5] However, social participation and employment in particular remain relatively difficult for PWH. Patients with severe hemophilia participate less in full-time work compared with the general population. Also, occupational disability is more often reported by PWH.[6] Several studies evaluated the quality of life of PWH[7–10] and most of these studies used a structured questionnaire to measure clinical outcome. However, the health effects, including major comorbidities in employed PWH, were seldom explored using longitudinal data. The National Health Insurance Research Database (NHIRD) in Taiwan, which was established in 1995, contains the medical records of 99.6% of the total population, which was approximately 23 million in 2009. The National Health Insurance (NHI) program in Taiwan is a unique health care system, which offers unrestricted access to any healthcare provider of the patient's choice. Owing to the unique single-payer system of Taiwan's NHI, the NHIRD is a powerful resource for conducting a national epidemiological investigation. All PWH in Taiwan receive good care, including free treatment with CFC covered by national health insurance if they were registered as having a catastrophic illness. There are >40 medical facilities providing outpatient clinic in Taiwan. The prevalence, incidence, factors usage, and mortality of PWH in Taiwan were discussed in previous studies.[11,12] In this study, we investigated the effect of employment on the health status of PWH compared with a matched general population.
1. Material and methods
1.1. Data sources
In this longitudinal population-based study, a catastrophic illness is defined as a severe illness requiring advanced health care. Patients certified with a catastrophic illness, including hemophilia, are exempt from paying NHI contributions and can be easily identified using the Registry of Catastrophic Illness Patient Database (RCIPD).
Each newly diagnosed patient of hemophilia A or hemophilia B must be certified by physicians, and PWH who registered as having a catastrophic illness in the NHI received free treatment with CFC, which was covered by insurance. Thus, the data of hemophilia patients in the catastrophic database were considered to be strongly representative of the national hemophiliac population. In this study, the retrieved data were verified by linking the encrypted personal identification number with the patient's catastrophic illness certificate.
In cooperation with the Bureau of National Health Insurance (BNHI), the National Health Research Institutes of Taiwan maintains the Longitudinal Health Insurance Database (LHID), a representative database of 1,000,000 subjects who were randomly sampled from the 2005 registry of all NHI enrollees using a systematic sampling method for research purposes. There were no statistically significant differences in age, sex, or healthcare costs between the sample group and all enrollees. These databases have previously been used for epidemiological research, and the information provided regarding prescription use, diagnoses, and hospitalizations is of high quality.[13–15] The accuracy of diagnosis of major diseases in the NHIRD, such as stroke and acute coronary syndrome, has been validated.[16–18] All patients’ records/information were anonymized and deidentified before analysis. Institutional Review Board of the Taichung Veterans General Hospital (TCVGH-IRB) Taiwan had approved this study.
1.2. Identification of study cohort
All male patients older than 16 years with hemophilia A and B were identified by the International Classification of Diseases Ninth Revision (ICD-9) codes 286.0 and 286.1 from the registration files and original claims data of the RCIPD between January 1, 1997 and December 31, 2010. The NHIRD patient files included an encrypted personal identification number, date of birth, date of enrollment, medical claims, work status, and work category. For comparisons with PWH with work history in 1997, a representative sample of the general male population without hemophilia between 1997 and 2010 and with a work history in 1997 was retrieved from the LHID 2005, matched for sex and month of birth with a ratio of 1:4.[19]Figure 1 showed the sampling process.
Figure 1.
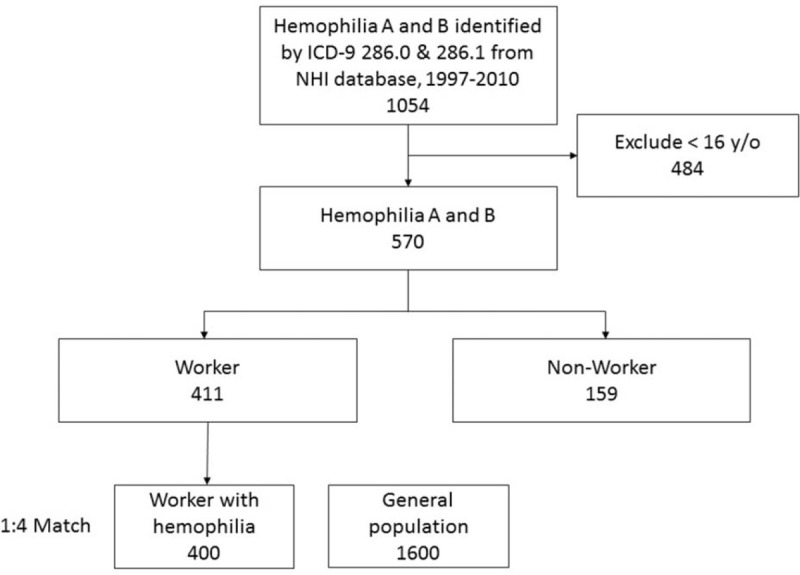
Patient selection. ICD-9 = International Classification of Diseases, ninth revision, NHI = National Health Insurance.
1.3. Outcome measurement
We further compared the incidence of newly diagnosed important comorbidities between employed PWH and the matched general population during the period January 1, 1998 to December 31, 2010. To avoid the possibility of reverse causality, any case with target comorbidities diagnosed before December 31, 1997 was washed out from the analysis. To select potential patients in this cohort, new cases with any target comorbidities (including hepatitis B virus infection, hepatitis C virus infection, chronic liver disease and cirrhosis, drug-induced liver injury, non-alcoholic fatty liver disease, acquired immune deficiency syndrome, hemorrhagic stroke, cerebral infarction, peripheral artery occlusive disease, deep vein thrombosis, arterial embolism and thrombosis, hypertension, hyperlipidemia, heart failure, chronic obstructive pulmonary disease, osteoporosis, arthritis and arthropathy, other disorder of joints, epistaxis, hematuria, depression, anxiety, and bipolar disorder) were identified for at least 1 time in the admission files as well as cases with diagnosis ≥3 times in 1 year of outpatient files between January 1, 1998, and December 31, 2010, and the date of the first diagnosis of each comorbidity was used as the index date. These stringent criteria enabled the researchers to confirm the diagnosis. The diagnosis of comorbidities was defined using ICD-9 codes, and described in Supplement 1.
1.4. Statistical analysis
Cox proportional hazards regression model was used to estimate the relationship between each comorbidity and employment among all hemophiliacs, and between each comorbidity and hemophilia in the employed PWH group and general population. These patients were followed up from January 1, 1998. Follow-up ended on the incident date of target disease, the date of death, the date of withdrawal from the registry, or December 31, 2010.
The relationships between each job category and comorbidities were also evaluated. The hazard ratio (HR) for each comorbidity development was calculated in the employed hemophilic patients compared with the unemployed hemophilic patients, and in hemophilic patients compared with non-hemophiliacs. Accompanying 95% confidence intervals (CIs) were also calculated. A 2-tailed P value of 0.05 was considered significant. Study size was calculated under the condition of alpha = 0.05, beta = 0.2, effect size = 2.0, and calculated sample size was 148 by software G power (version 3.1.9.2). Since multiple confounding factors could alter the results,[3,20] we also analyzed the hazard ratios of comorbidities and risk factors for important comorbidities, such as hemorrhagic stroke and arthritis/arthropathy between the hemophilic patients and the general matched population using a multivariate Cox proportional hazards regression model. Furthermore, the relationships between different job categories and cumulative incidence of comorbidities were examined. Besides, because sample sized for some comorbidities was small, we also examined the results by Fisher exact test. All statistical analyses were conducted using SAS software (version 9.2; SAS Institute Inc., Cary, NC).
2. Results
A total of 570 patients with hemophilia A and hemophilia B were eligible for inclusion in this analysis. Among them, 411 patients had a history of employment in 1997. After matching, there were 400 employed PWH and 1600 individuals without coagulation disorders.
2.1. Demographics
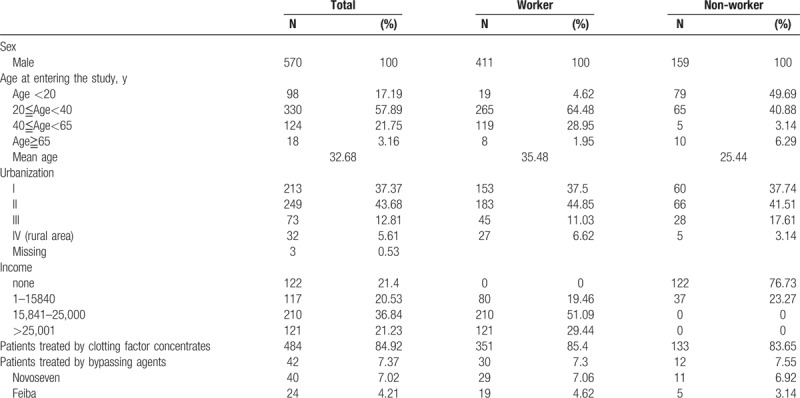
The age distribution of 570 PWH is presented in Table 1. All PWH were male. In the year of study entry, most of the patients (57.89%) were aged 20 to 40 years. Most (80.7%) PWH lived in modern cities of Taiwan. Most PWH (36.8%) had an income of 15841 to 25000 NT dollars a month. Among the 411 employed PWH, most of the patients (64.48%) were aged 20 to 40 years. Furthermore, 79.3% of the employed PWH lived in a modern city, and more than half of the employed PWH (51.1%) received an income of 15841 to 25000 NT dollars a month. There were few unemployed PWH who still had income because in some cases, government would provide a minimal insured amount for those unemployed population as social welfare. For types of hemophilia, there were 482 type A hemophiliacs and 88 type B hemophiliacs.
Table 1.
Characteristics of 570 hemophilia patients aged >16 years in 1997, enrolled during 1997 to 2010.
2.2. Clinical characteristics of 570 patients with hemophilia
In total, 4.7%, 20.5%, and 4.2% of PWH had hepatitis B virus (HBV), hepatitis C virus (HCV), and human immunodeficiency virus (HIV) infection, respectively. Approximately 85% of the hemophilia patients received CFC (Table 1). A total of 64 (11.2%) patients received bypassing agents during the study period. According to regulations from BNHI, bypassing agents can only be reimbursed for hemophiliac patients with inhibitors. Thus, we can assume that all 64 patients who received bypassing agents had inhibitors. It is hard to identify who received immune tolerance induction (ITI) from our database, but most of the physicians in Taiwan would try ITI before using bypassing agents.
2.3. Incidence of major comorbidities and its risk factors in 411 employed PWH and 159 unemployed PWH
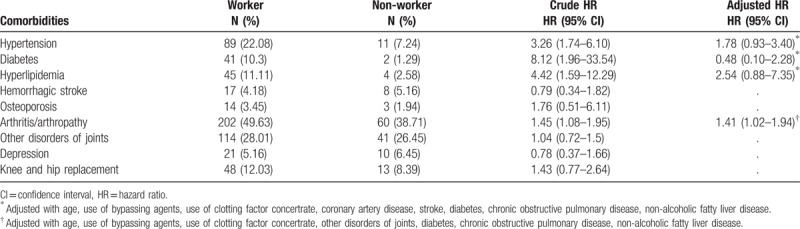
The proportions of persons with hemorrhagic stroke, disorders of joints, osteoporosis, depression, and knee/hip replacement were all nonsignificantly different between employed and unemployed PWH during the follow-up period (Table 2). Compared with PWH nonworkers, PWH workers were more often diagnosed with arthritis/arthropathy after adjusting age, use of bypassing agents, use of CFC, other disorders of joints, diabetes, chronic obstructive pulmonary disease (COPD), nonalcoholic fatty liver disease (NAFLD) (HR:1.41, 95% CI 1.02–1.94).
Table 2.
Cox proportional hazard ratio of major comorbidities among 411 employed and 159 unemployed persons with hemophilia.
2.4. Incidence of major comorbidities and its risk factors in 400 employed PWH and 1600 employed persons in the general population
Compared to the general population (Table 3), employed PWH had greater risks during the follow-up period for HCV (HR: 15.03, 95% CI 12.21–18.49), acquired immune deficiency syndrome (HR: 10.29, 95% CI 5.55–19.06), hemorrhagic stroke (HR: 4.72, 95% CI 2.94–7.59), osteoporosis (HR: 3.25, 95% CI 1.93–5.50), arthritis/arthropathy (HR: 5.53, 95% CI 4.79–6.38), other disorders of joints (HR: 3.08, 95% CI 2.54–3.74), epistaxis (HR: 2.49, 95% CI 1.12–5.53), hematuria (HR: 2.24, 95% CI 1.55–3.25), and knee/hip replacement (HR: 42.19, 95% CI 31.71–56.14). In the multivariate analysis, risk of hemorrhagic stroke was increased after adjusting for relative confounding factors (HR: 4.60, 95% CI 2.81–7.53). Risk of arthritis/arthropathy was increased after adjusting for relative confounding factors (HR: 4.03, 95% CI 3.34–4.87). Risk of hip/knee replacement was also increased (HR: 1.29, 95% CI 1.19–1.41). Because sample sized for some comorbidities was small, we also examined the results by Fisher exact test, and the results remained unchanged.
Table 3.
Cox proportional hazard ratio of major comorbidities among 400 employed persons with hemophilia and 1600 age-, sex-, and employment-matched persons in the general population.
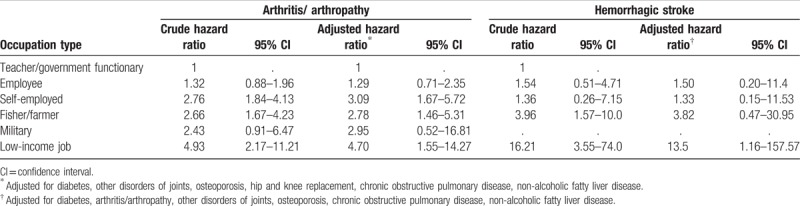
2.5. Relationships between different job categories and major comorbidities in the employed PWH group
Hemorrhagic stroke and arthritis/arthropathy were the main comorbidities that developed in the employed PWH group. To determine the risk of these main comorbidities among the different types of employment in PWH, we also analyzed job categories (Table 4). Using Cox proportional regression model, self-employed workers, fishermen, farmers, and workers with low-income jobs were found to be at greater risk for hemorrhagic stroke, compared to teachers. Fishermen, farmers, and workers with low-income jobs showed a significantly greater risk of developing arthritis/arthropathy, compared to teachers.
Table 4.
Cox proportional hazard ratios of hemorrhagic stroke and joint disease among employed persons with hemophilia based on types of occupation.
3. Discussion
This is the first study to explore the health consequences among employed PWH using a longitudinal study design. Our main findings were: compared to the unemployed PWH group, the employed PWH group did not have a greater risk of hemorrhagic stroke or hematogenous infection; however, a greater incidence of joint problems related to work status was found among PWH; compared to the employed general population, the employed PWH group was diagnosed with hemorrhagic stroke, arthritis/arthropathy and hip/knee replacement more frequently during the follow-up period; compared with employees with a light workload, those with a heavy workload carried a greater risk for hemorrhagic stroke and arthritis/arthropathy.
3.1. Hemophilia and employment
Since the 1970s, few studies have explored the health and socioeconomic status of PWH. A study conducted in London reported that the incidence of unemployment among PWH varied from 18% to 35%, compared with the national unemployment rate of around 7%.[21,22] After the introduction of treatment with CFC, the unemployment rate among PWH dropped significantly, but the disease itself still had a moderate to severe physical and psychological impact on hemophiliacs.[23–26] Our findings showed that compared with the unemployed PWH group, the employed PWH group had more joint problems, meaning employment results in increased risk of developing joint disease among PWH, especially for PWH with moderate and severe symptoms, who use CFC and bypassing agents. Therefore, for workers with moderate or severe hemophilia, employers should take the effect of the employees’ work, particularly with regard to job type and working hours, into consideration.
3.2. Hemorrhagic stroke in the employed PWH group compared with the employed general population group
Hemorrhagic stroke is the most serious type of bleeding in the PWH population. There was a 4.5 times greater risk of developing hemorrhagic stroke in the employed PWH group than the general population. Witmer et al reported a mortality rate of 19% if intracranial hemorrhage (ICH) occurs among PWH.[27] The most significant risk factors for ICH included the presence of an inhibitor, prior ICH, severity of hemophilia, and reported head trauma, while prescribed prophylaxis conferred a protective effect against ICH in patients with uncomplicated severe disease. Stieltjes et al[28] found that prognostic factors for death after ICH among PWH were thrombocytopenia, HCV infection, intraventricular, or intraparenchymatous hemorrhage. In our study, the employed PWH group had a greater incidence of hemorrhagic stroke during the follow-up period, whereas hypertension was an independent risk factor. Thus, hemophiliacs under employment should be monitored regularly, especially those with previous history of ICH or hypertension. For workers with a specific job, Hayashi et al[29] found that the 24-hour average blood pressure of overtime workers was higher than that of the control groups. Furthermore, Uchiyama et al[30] indicated that active jobs and high stress jobs were associated with increased risk of cardiovascular events for treated hypertensive workers. Our analysis of occupations revealed that PWH with low socioeconomic status, or with a job requiring a considerable amount of manual labor, such as fishermen or farmers, are at higher risk of hemorrhagic stroke. Thus, it is important for hemophiliac workers to carefully consider the effect of long working hours and work type.
3.3. Joint problems and hip/knee replacement
Bleeding may occur internally into the joints or muscles among PWH, which may cause joint destruction and eventually result in hip/knee replacement without proper treatment. Our results indicate that employed PWH had a greater risk of developing joint problems, and its risk factor including hemophilia status, disorder of joints, diabetes, hip/knee replacement, osteoporosis, COPD, and NAFLD. Thus, risk group identification, anticipating drug use, early recognition of hemarthrosis signs, appropriate fitness for work, and proper treatment after diagnosis, may allow hemophiliacs to avoid joint problems and thus be provided the opportunity to successfully participate in the workforce.
3.4. Prophylaxis with CFC and joint disease
As for prophylaxis with CFC and joint disease, it is hard to evaluate whether the treatment is for prophylaxis or for on-demand treatment in a large administrative database such as NHIRD. From the Malmo protocol and Utrecht protocol, the prophylaxis dose for hemophilia A is 15 to 40 IU/kg, thrice a week.[31] However, how it is done varies both from country to country. In Taiwan, few adults have prophylaxis, although their average dose is around 500 IU per week, equal to around 104,000 IU per year. Thus, we ran the analysis by assuming PWH who ever used 104,000–110,000 IU in a year during our follow-up period as PWH with prophylaxis treatment. Then we analyzed the relationship between major comorbidities, including hemorrhagic stroke, arthritis/arthropathy, and knee/hip replacement and PWH with/without prophylaxis by using Cox proportional hazards regression model. We also excluded PWH ever using bypassing agents from the analysis because they were indeed expected to have more severe complications related to bleeding. After excluding 29 PWH ever using bypassing agents, there were 371 PWH into the analysis. The result showed in Supplement Table 1. There was no significant difference between incidence of all 3 major comorbidities and PWH with/without prophylaxis. However, we can see a trend that prophylaxis has the effect of preventing comorbidities in PWH. There could be lots of causes for the insignificance, and one of them may be the small sample size with small power. Since the introduction of NHI in Taiwan in 1995, more and more adults started prophylaxis with CFC. There is a greater chance that prophylaxis treatment shows its real effect in future study.
3.5. Strengths
There were several strengths in this study. First, this study was a large, population-based, prospective cohort study, which enrolled 570 patients with hemophilia A, who were followed up for a relatively long period, from 1998 to 2010. Second, previous studies generally used validated questionnaires for evaluating outcome. Our study used a national health database for determining outcomes, and thus a much more objective assessment of the outcome definition could be obtained. Third, our subjects were age-, sex-, and employment status-matched with the general population, which further improved the quality of the data and analyses in this investigation.
3.6. Limitations
This study also had several limitations. First, we used employment status in 1997 to define whether a PWH belongs to the employed or unemployed group. However, employment status was regarded as unchanged during the follow-up period. Participants who were considered employed could have lost their job during the study period; likewise, unemployed subjects may have found employment during follow-up. However, the effect was likely bidirectional and this would have diminished any potential bias to some extent. We also did the subgroup analysis between unemployed PWH and unemployed general population, trying to have more understanding of the effect of hemophilia itself to our target comorbidities, and described in Supplement Table 2. Second, the conclusion was made by analyzing data from Taiwan's NHIRD, which does not include potential confounding variables, such as smoking or body mass index (BMI). Usually, BMI (kilograms per square meters) is used as an acceptable surrogate index for defining obesity based on the WHO's recommendation. However, it has become apparent that the distribution of body fat has a more important role in obesity-associated comorbidities than the total fat mass. One study conducted in Korean showed that NAFLD was not only associated with obesity, but was also found to be a meaningful predictor of metabolic diseases in the non-obese population.[32,33] Furthermore, the relationship between smoking and COPD has been established.[34] Thus, we used surrogate indicators for the multivariate analysis, such as COPD for smoking, and NAFLD for obesity, with a view to mitigate any possible bias. Third, since the NHIRD was established in 1995, we hardly realized the intensity of replacement therapy with CFC among PWH during their childhood and adolescence. However, we did the subgroup analysis between PWH with prophylaxis and without prophylaxis, trying to understand the effect of CFC prophylaxis to our target comorbidities. Besides, since April 1, 2014, BNHI approved the reimbursement of prophylaxis with CFC for severe patients with hemophilia. We believed that PWH with CFC prophylaxis during childhood and adolescence would prevent future comorbidities. Fourth, it is also hard to evaluate the cause of each hemorrhagic stroke with their circumstances from a large administrative database. However, from our current data, after matching for age and working status with general population, there is still an increased risk of hemorrhagic stroke among PWH working group. Further study needs to focus on the mechanism of hemorrhagic stroke of PWH working group. Fifth, as we classified job category according to each participant's job in 1997, there is possibility of job change during our cohort period, and that could cause classification error. However, we additionally analyzed job status each year during study period among all 570 PWH. The result demonstrated that most PWH holding their jobs stably. And last, we used our data from 1997to 2010, and not to extend the inclusion period further, because we did a background analysis comprised data from 1997 to 2013, which resulted in even less eligible participants. That was because we can only access database from BNHI; thus, there will be slightly difference between 2010 database and 2013 database because the insured population are different each year.
4. Conclusions
This population-based longitudinal cohort study showed: the employed PWH group had more joint problems compared to the unemployed PWH group; the employed PWH group had a greater possibility of developing hemorrhagic stroke and joint problems, compared with the general population; occupations with low income and much labour, as well as fishermen and farmers, were associated with high risk of developing undesired comorbidities. Fitness for work and regular medical surveillance of PWH by practitioners of occupational medicine and employers are strongly recommended. Policymakers should give consideration to PWH with respect to equal job opportunities and employment rights.[35] Finally, further investigation should focus on: analyzing whether patients had inhibitors would be a risk factors for future comorbidities; whether there are different outcomes between PWH receiving episodic treatment versus prophylaxis treatment, or the influence of the intensity of prophylaxis regimen; to elucidate the relationships between comorbidities and specific occupations to improve the health status and quality of life of PWH in the workforce.
Acknowledgments
The authors thank TCVGH-1057203D and TCVGH-1047203C from Taichung Veterans General Hospital for the support.
Author's contributions: Y-TT conceived of the study and supervised all aspects of its implementation; W-MC completed the analyses and drafted the content; J-DW, H-EH, Y-SL, and S-YH assisted with the study design and revised the content; W-CC and W-CH assisted with the statistical analysis and revised the content; all authors helped to conceptualize ideas, interpret findings, and review drafts of the manuscript.
Supplementary Material
Footnotes
Abbreviations: BMI = body mass index, BNHI = Bureau of National Health Insurance, CFC = clotting factor concertrates, CI = confidence interval, COPD = chronic obstructive pulmonary disease, HBV = hepatitis B virus, HCV = hepatitis C virus, HIV = human immunodeficiency virus, HR = hazard ratio, ICD-9 = International Classification of Diseases Ninth Revision, ICH = intracranial hemorrhage, ITI = immune tolerance induction, LHID = Longitudinal Health Insurance Database, NAFLD = non-alcoholic fatty liver disease, NHI = National Health Insurance, NHIRD = National Health Insurance Research Database, PWH = persons with hemophilia, RCIPD = Registry of Catastrophic Illness Patient Database, TCVGH-IRB = Institutional Review Board of the Taichung Veterans General Hospital.
The authors report no conflicts of interest.
Supplemental Digital Content is available for this article.
References
- [1].Dunn AL. Pathophysiology, diagnosis and prevention of arthropathy in patients with haemophilia. Haemophilia 2011;17:571–8. [DOI] [PubMed] [Google Scholar]
- [2].Plug I, van der Bom JG, Peters M, et al. Thirty years of hemophilia treatment in the Netherlands, 1972–2001. Blood 2004;104:3494–500. [DOI] [PubMed] [Google Scholar]
- [3].Aledort LM, Haschmeyer RH, Pettersson H. A longitudinal study of orthopaedic outcomes for severe factor-VIII-deficient haemophiliacs. The Orthopaedic Outcome Study Group. J Intern Med 1994;236:391–9. [DOI] [PubMed] [Google Scholar]
- [4].Poon JL, Zhou ZY, Doctor JN, et al. Quality of life in haemophilia A: Hemophilia Utilization Group Study Va (HUGS-Va). Haemophilia 2012;18:699–707. [DOI] [PubMed] [Google Scholar]
- [5].Darby SC, Kan SW, Spooner RJ, et al. Mortality rates, life expectancy, and causes of death in people with hemophilia A or B in the United Kingdom who were not infected with HIV. Blood 2007;110:815–25. [DOI] [PubMed] [Google Scholar]
- [6].Plug I, Peters M, Mauser-Bunschoten EP, et al. Social participation of patients with hemophilia in the Netherlands. Blood 2008;111:1811–5. [DOI] [PubMed] [Google Scholar]
- [7].Solovieva S. Clinical severity of disease, functional disability and health-related quality of life. Three-year follow-up study of 150 Finnish patients with coagulation disorders. Haemophilia 2001;7:53–63. [DOI] [PubMed] [Google Scholar]
- [8].Tusell JM, Aznar JA, Querol F, et al. Results of an orthopaedic survey in young patients with severe haemophilia in Spain. Haemophilia 2002;8(suppl 2):38–42. [DOI] [PubMed] [Google Scholar]
- [9].Talaulikar D, Shadbolt B, McDonald A, et al. Health-related quality of life in chronic coagulation disorders. Haemophilia 2006;12:633–42. [DOI] [PubMed] [Google Scholar]
- [10].Wang T, Zhang L, Li H, et al. Assessing health-related quality-of-life in individuals with haemophilia in China. Haemophilia 2004;10:370–5. [DOI] [PubMed] [Google Scholar]
- [11].Tu TC, Liou WS, Chou TY, et al. Prevalence, incidence, and factor concentrate usage trends of hemophiliacs in Taiwan. Yonsei Med J 2013;54:71–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Chang CY, Yeh GC, Lin SY, et al. Trends in the epidemiology, diagnosed age and mortality rate of haemophiliacs in Taiwan: a population-based study, 1997–2009. Haemophilia 2014;20:535–40. [DOI] [PubMed] [Google Scholar]
- [13].Tsan YT, Lee CH, Ho WC, et al. Statins and the risk of hepatocellular carcinoma in patients with hepatitis C virus infection. J Clin Oncol 2013;31:1514–21. [DOI] [PubMed] [Google Scholar]
- [14].Tsan YT, Lee CH, Wang JD, et al. Statins and the risk of hepatocellular carcinoma in patients with hepatitis B virus infection. J Clin Oncol 2012;30:623–30. [DOI] [PubMed] [Google Scholar]
- [15].Wu CY, Chen YJ, Ho HJ, et al. Association between nucleoside analogues and risk of hepatitis B virus-related hepatocellular carcinoma recurrence following liver resection. JAMA 2012;308:1906–14. [DOI] [PubMed] [Google Scholar]
- [16].Lin CC, Lai MS, Syu CY, et al. Accuracy of diabetes diagnosis in health insurance claims data in Taiwan. J Formos Med Assoc 2005;104:157–63. [PubMed] [Google Scholar]
- [17].Cheng CL, Kao YH, Lin SJ, et al. Validation of the National Health Insurance Research Database with ischemic stroke cases in Taiwan. Pharmacoepidemiolo Drug Saf 2011;20:236–42. [DOI] [PubMed] [Google Scholar]
- [18].Cheng CL, Lee CH, Chen PS, et al. Validation of acute myocardial infarction cases in the national health insurance research database in Taiwan. J Epidemiol 2014;24:500–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Wachoider S, Silverman DT, McLaughlin JK, et al. Selection of controls in case-control studies III. Design options. Am J Epidemiol 1992;135:1042–50. [DOI] [PubMed] [Google Scholar]
- [20].Sharathkumar AA, Soucie JM, Trawinski B, et al. Prevalence and risk factors of cardiovascular disease (CVD) events among patients with haemophilia: experience of a single haemophilia treatment centre in the United States (US). Haemophilia 2011;17:597–604. [DOI] [PubMed] [Google Scholar]
- [21].Prothero J. Haemophilia society survey. London: Haemophilia Society; 1977. [Google Scholar]
- [22].Markova ILR, Forbes CD. Haemophilia: a survey on social issues. Health Bull 1977;35:177–82. [PubMed] [Google Scholar]
- [23].Varekamp I, Smit C, Rosendaal FR, et al. Employment of individuals with haemophilia in The Netherlands. Soc Sci Med (1982) 1989;28:261–70. [DOI] [PubMed] [Google Scholar]
- [24].Lineberger HP. Social characteristics of a hemophilia clinic population. A survey and literature review. Gen Hosp Psychiatry 1981;3:157–63. [DOI] [PubMed] [Google Scholar]
- [25].Nimorwicz P, Tannebaum J. Educational and vocational achievement among hemophiliacs: the Pennsylvania experience. J Chronic Dis 1986;39:743–50. [DOI] [PubMed] [Google Scholar]
- [26].Goldsmith MF. Hemophilia, beaten on one front, is beset on others. JAMA 1986;256:3200. [PubMed] [Google Scholar]
- [27].Witmer C, Presley R, Kulkarni R, et al. Associations between intracranial haemorrhage and prescribed prophylaxis in a large cohort of haemophilia patients in the United States. Br J Haematol 2011;152:211–6. [DOI] [PubMed] [Google Scholar]
- [28].Stieltjes N, Calvez T, Demiguel V, et al. Intracranial haemorrhages in French haemophilia patients (1991–2001): clinical presentation, management and prognosis factors for death. Haemophilia 2005;11:452–8. [DOI] [PubMed] [Google Scholar]
- [29].Hayashi T, Kobayashi Y, Yamaoka K, et al. Effect of overtime work on 24-hour ambulatory blood pressure. J Occup Environ Med 1996;38:1007–11. [DOI] [PubMed] [Google Scholar]
- [30].Uchiyama S, Kurasawa T, Sekizawa T, et al. Job strain and risk of cardiovascular events in treated hypertensive Japanese workers: hypertension follow-up group study. J Occup Health 2005;47:102–11. [DOI] [PubMed] [Google Scholar]
- [31].Blanchette VS, Manco-Johnson M, Santagostino E, et al. Optimizing factor prophylaxis for the haemophilia population: where do we stand? Haemophilia 2004;10(suppl 4):97–104. [DOI] [PubMed] [Google Scholar]
- [32].Kwon Y-M, Oh S-W, Hwang S-s, et al. Association of nonalcoholic fatty liver disease with components of metabolic syndrome according to body mass index in Korean adults. Am J Gastroenterol 2012;107:1852–8. [DOI] [PubMed] [Google Scholar]
- [33].Pagadala MR, McCullough AJ. Non-alcoholic fatty liver disease and obesity: not all about body mass index. Am J Gastroenterol 2012;107:1859–61. [DOI] [PubMed] [Google Scholar]
- [34].Forey BA, Thornton AJ, Lee PN. Systematic review with meta-analysis of the epidemiological evidence relating smoking to COPD, chronic bronchitis and emphysema. BMC Pulm Med 2011;11:36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Srivastava A, Brewer AK, Mauser-Bunschoten EP, et al. Guidelines for the management of hemophilia. Haemophilia 2013;19:e1–47. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


