Abstract
Objective:
The controversy remains as to whether immediate prosthetic breast reconstruction with postmastectomy radiation therapy (PMRT) is associated with acceptable complications and aesthetic outcomes. The aim of this meta-analysis was to provide a pooled analysis of comparative clinical studies that evaluated breast cancer patients who were treated with a mastectomy and an immediate prosthetic breast reconstruction to compare the complications and satisfaction of those who underwent or did not undergo PMRT.
Methods:
According to the recommendations of the Cochrane Collaboration, we established a rigorous study protocol. We performed a systematic electronic search of the PubMed and Embase databases to identify articles for inclusion in our meta-analysis. Reconstruction failure, overall complications, capsular contracture, and patient satisfaction were analyzed individually.
Results:
Fifteen controlled trials were included, comprising 5314 patients (1069 PMRT vs 4245 non-PMRT). Primary outcomes revealed a statistically significant increase in overall complications [odds ratio (OR) 3.45; 95% confidence interval (95% CI) 2.62–4.54; P < .00001], reconstruction failure (OR: 2.59; 95% CI 1.46–4.62; P = .001), and capsular contracture (OR: 5.26, 95% CI: 2.73–10.13, P < .00001) after receiving PMRT.
Conclusion:
Our review found that PMRT for patients who underwent immediate implant-based breast reconstruction led to higher risks of reconstruction failure, overall complications, and capsular contracture. However, it is still the standard adjuvant therapy for mastectomy patients who have opted for immediate implant-based breast reconstruction.
Keywords: complications, immediate breast reconstruction, meta-analysis, PMRT, radiation therapy
1. Introduction
Currently, radiation therapy is the standard of care for breast cancer treatment following lumpectomy.[1] It may be utilized either following lumpectomy or after mastectomy, and postmastectomy radiation therapy (PMRT) in patients with locally advanced breast cancer has been demonstrated to improve both local control and patient survival.[2] As a result, PMRT is routinely used to prevent local recurrence in patients who have close or positive mastectomy margins or to obtain long-term, local-regional control in patients who have suffered a chest wall recurrence.[3,4]
As proven in women treated for primary breast cancer, immediate breast reconstruction, performed at the time of mastectomy, is a procedure that offers good clinical, aesthetic, and psychological results and is oncologically safe in terms of local recurrence and long-term survival rates.[4–6] Two major breast reconstruction options are currently available, namely autologous reconstruction and implant-based reconstruction. Implant reconstruction has a major role in immediate breast reconstruction today because some patients do not wish to undergo a major surgical procedure and others are deemed to be unsuitable candidates for autologous reconstruction.
Indeed, the presence of a reconstruction can complicate plans for radiation therapy. Similarly, the effects of radiation therapy on the immediate breast reconstruction has generated significant discussion and controversy. Several studies have demonstrated that PMRT may compromise aesthetic outcomes and increase the complication rates for immediate breast reconstruction, especially in implant breast reconstructions.[7–9] These authors reported that PMRT engenders changes in mastectomy flap perfusion, which may result in infection, tissue necrosis, capsular contracture, implant extrusion, wound dehiscence, and complete reconstructive failures. However, other studies[10] have demonstrated that there is no significant difference in the overall rate of major or minor complications between the PMRT group and non-PMRT group.
Despite these established complications, many patients seem to successfully undergo both PMRT and breast reconstruction when treated with a systematic and carefully considered approach. The objective of this study was to analyze whether the following outcomes were affected by PMRT: reconstruction failure, overall complications, capsular contracture, and the patients’ satisfaction with cosmetic and functional outcomes. Knowledge of these outcomes will allow clinicians to provide women who are candidates for immediate implant breast reconstruction with information about the risks and benefits of PMRT.
2. Materials and methods
We performed a systematic electronic search of PubMed, Embase, the Cochrane Library databases, Web of Science, Chinese Biomedical Database, and Chinese Scientific Journals database to identify articles for inclusion in our meta-analysis. And ethical approval was not necessary for this meta-analysis. The search terms “breast reconstruction,” “radiation therapy,” “immediate,” and “mastectomy” and the Medical Subjects Headings (MeSH) terms of “breast reconstruction” (MeSH), “radiation therapy” (MeSH), “immediate” (MeSH), and “mastectomy” (MeSH) were used in combination with the Boolean operators AND or OR. The electronic search was supplemented by a hand-search of published abstracts from the annual meetings of relevant surgical societies. Reference searches were also conducted, where lists of trials selected from the electronic search were scanned to identify further relevant trials.
Abstracts of the citations that were identified by the search were then scrutinized by 2 observers to determine the eligibility of the corresponding study for inclusion in the meta-analysis. Studies were included if they met each of the following criteria: it was a comparative study, and the study sample was separated into groups based on the use or nonuse of PMRT among patients with immediate implant breast reconstructions. Studies without non-PMRT controls were excluded from our study. Our search identified 15 studies that met our criteria in the meta-analysis. The data extracted from each article included the following: the study design, number of subjects, male/female ratio, mean age of subjects, and any preoperative interventions performed.
3. Statistical analysis
The data from the eligible trials were entered into a computerized spreadsheet for analysis. The quality of each trial was assessed using the Jadad scoring system. We performed the meta-analysis using RevMan 5.1.9 software (provided by the Cochrane Collaboration, Oxford, UK) for the controlled studies. The relative risk (RR) was calculated with a 95% confidence interval (95% CI). We used χ2 to assess statistical heterogeneity and the Higgins I2 statistic to determine the percentage of total variations across studies due to heterogeneity. If the I2 statistic was ≤ 50%, then a fixed-effect model was used to pool studies; otherwise, a random-effects model was used.
4. Results
4.1. Study characteristics
A total of 15 studies were included.[11–25] All eligible studies were published between 2000 and 2016. Table 1 summarizes the details of each trial, including baseline characteristics, the publication year of the study, the surgical method, and tumor stage for each trial. A PRISMA flowchart (Fig. 1) describes the details of the literature search for this meta-analysis.
Table 1.
Demographic data.
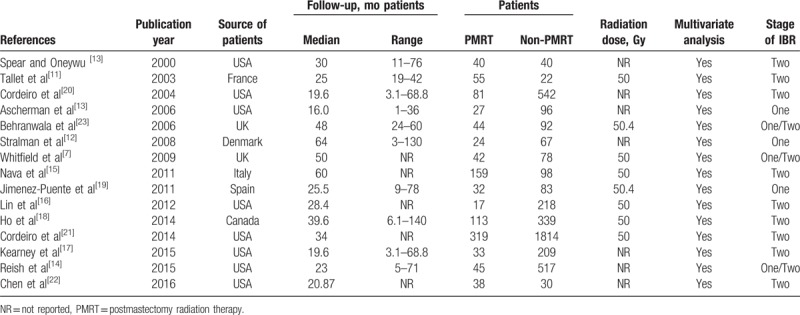
Figure 1.
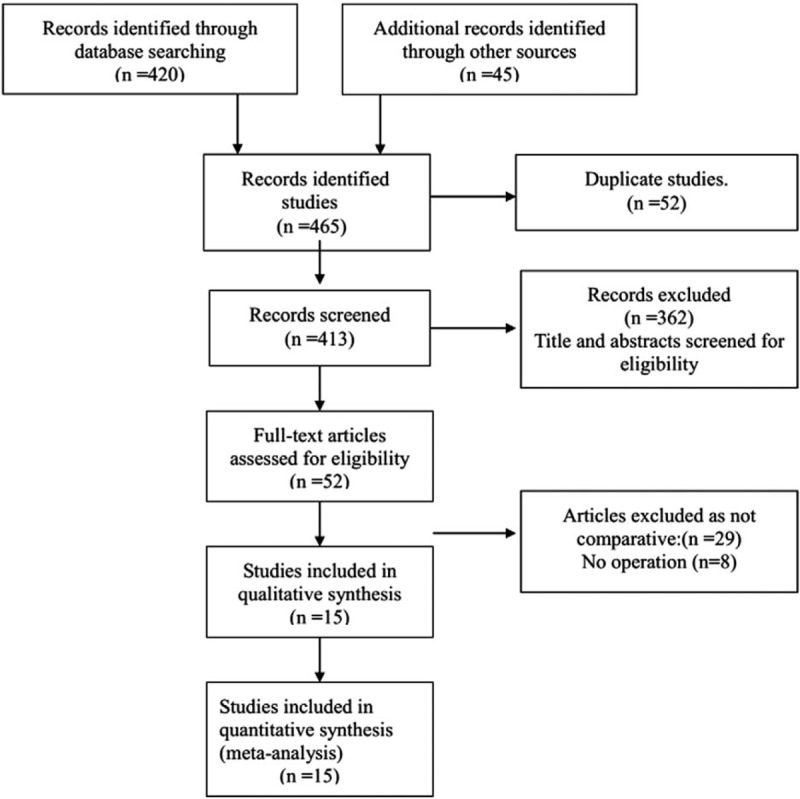
Flow chart of the literature search according to PRISMA.
4.2. Reconstruction failure
The rates of reconstruction failure of the immediate implant breast reconstructions were available in 10 studies. The use of PMRT increased the rates of reconstruction failure of immediate implant breast reconstruction [odds ratio (OR): 2.59; 95% CI 1.46–4.62; P = .001]. Heterogeneity was found to be significant [I2 = 73%, χ2 = 33.39 (df = 9), P = 0.001] (Fig. 2).
Figure 2.
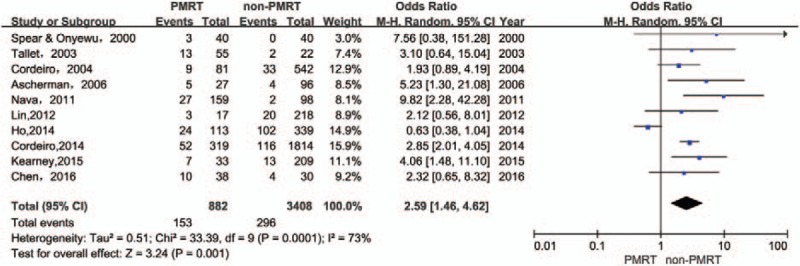
Forest plot for the impact of PMRT on reconstruction failure.
4.3. Overall complications
Overall complications were measured in 9 studies, totaling 495 patients with PMRT and 1752 patients without PMRT. It was found that there was a significant difference in the overall complications between those treated with PMRT and without PMRT (OR 3.45; 95% CI 2.62–4.54; P < .00001). Statistical heterogeneity was not detected (I2 = 36%, χ2 = 12.52, df = 8, P = .13) (Fig. 3).
Figure 3.
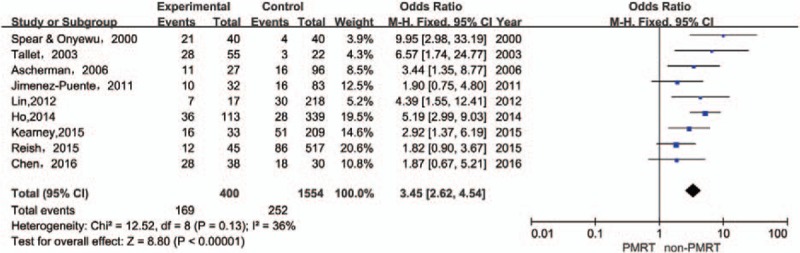
Forest plot for the impact of PMRT on overall complications.
4.4. Capsular contracture
Eleven studies reported the incidence of capsular contracture after immediate implant breast reconstruction. The analysis found a significant positive correlation between receiving PMRT and the formation of capsular contractures (OR: 5.26, 95% CI: 2.73–10.13, P < .00001). Heterogeneity was found to be significant [I2 = 77%, χ2 = 42.58 (df = 10), P < .00001] (Fig. 4).
Figure 4.
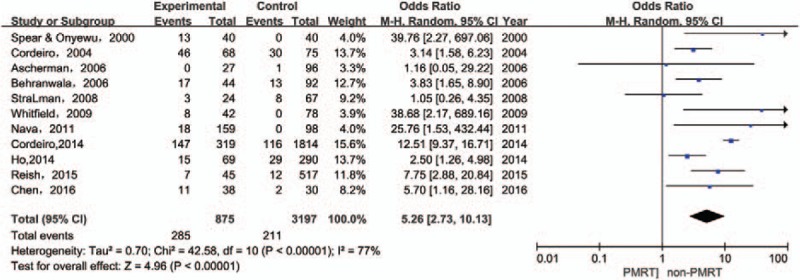
Forest plot for the impact of PMRT on capsular contracture.
4.5. Patient satisfaction
The patient satisfaction outcomes were available in 3 studies. There were significant differences in patient satisfaction between the PMRT and the non-PMRT groups (OR: 0.28, 95% CI: 0.19–0.42; P < .00001). There was no evidence of statistical heterogeneity [I2 = 31%, χ2 = 2.92, (df = 2), P = .23] (Fig. 5).
Figure 5.
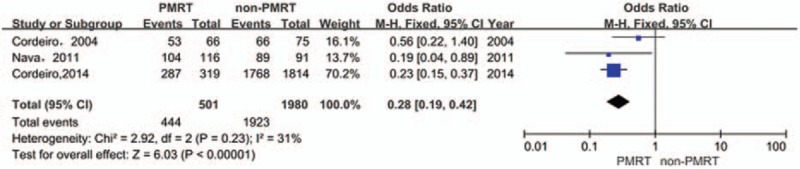
Forest plot for the impact of PMRT on patient satisfaction.
4.6. Publication bias
Funnel plots (for log OR) were drawn for each outcome. The graphical checks showed no asymmetry of the funnel plots. Assessment with the Egger method revealed no evidence of publication bias for any outcomes (P = .402, Fig. 6).
Figure 6.
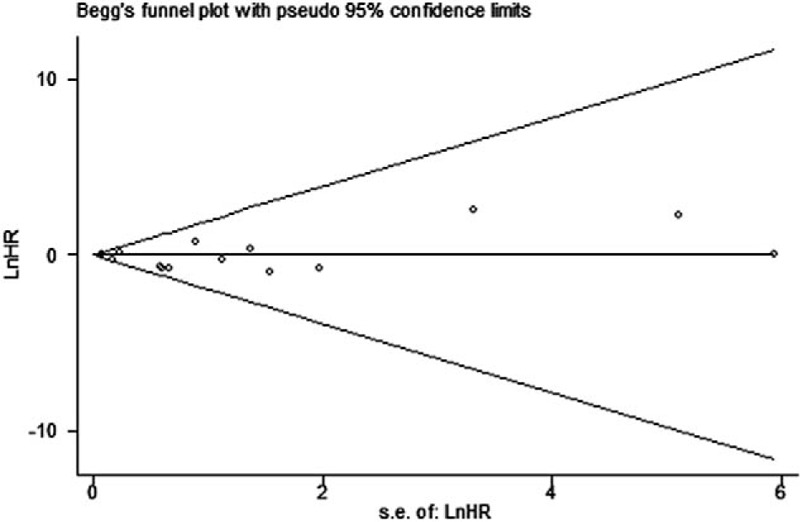
Funnel plot for publication bias.
5. Discussion
During the past decade, immediate implant-based breast reconstruction has become a widely accepted method for breast reconstruction after mastectomy. It has an acceptable rate of postoperative complications and is considered oncologically safe with a local recurrence rate ranging from 2% to 10%. It is well established that PMRT is increasingly used and improves survival for patients with breast cancer. As the indications for PMRT increase, there will be an increase in the number of patients opting for breast reconstruction, who will require radiotherapy as part of their treatment. However, a concern could be raised regarding the possible negative effects of radiotherapy on long-term outcomes after breast reconstruction. In general, the impact of PMRT on implant-based breast reconstruction has been documented in multiple studies over many years, but it continues to be a topic of discussion. Specifically, concerns still exist regarding complication rates, reconstruction failure, capsular contracture, and patient satisfaction, and there is debate regarding the results obtained by delivering PMRT to the permanent implant.
Several studies found that patients with immediate implant-based breast reconstructions who received PMRT had worse outcomes than patients who did not receive PMRT. Multiple complications have been reported in these studies for patients who received PMRT, including infection, tissue necrosis, capsular contracture, implant extrusion, wound dehiscence, and complete reconstruction failures. One of the main complications has been the formation of capsular contractures, leading to poor cosmetic outcome, an increased reoperation rate, and a loss of the breast reconstruction. A study by Spear and Onyewu[13] evaluated patients with immediate implant-based reconstructions and compared PMRT with non-PMRT patients; it was the first study to evaluate the impact of PMRT on immediate implant-based reconstructions. Over their 10-year experience, they reported total complication rates of 52.5% (21 of 40) and 10% (4 of 40) for the PMRT and non-PMRT groups, respectively. In particular, the incidence of capsular contracture was 32.5% for patients who underwent PMRT compared with 0% for those who did not receive PMRT. A limitation of that study is the lack of patient satisfaction outcome data. Similarly, Cordeiro et al[20] conducted a larger series (n = 623) that compared patients who received PMRT (n = 81) with a control group of 542 non-PMRT patients. The incidence of capsular contracture was also significantly higher in the PMRT group. However, there was little difference in patient satisfaction between groups. Although many previous studies have shown that the use of PMRT results in a significantly higher complication rate in patients who underwent immediate implant-based breast reconstruction, 2 recent series demonstrated acceptable results in uniformly treated samples.[12,18] Stralman et al[12] performed a retrospective study (n = 91) that compared patients who received PMRT (n = 24) with a control group of 67 non-PMRT patients. Among the patients who received PMRT, 3 (13%) developed capsular contracture, and among the patients who did not receive PMRT, 8 (12%) developed capsular contracture. The authors found no significant increase in the occurrence of capsular contracture in their study of patients who received PMRT.
As the present review details, the vast majority of studies have been small, retrospective case series that lack the statistical power to make a clear statement regarding the utility of PMRT. A meta-analysis, such as that performed in this study, is a potentially useful tool because it pools data into a very powerful study. In this meta-analysis, we selected all well-controlled cohort studies that evaluated breast cancer patients who were treated with a mastectomy and an immediate prosthetic breast reconstruction and that compared the complications and satisfaction of those who underwent and did not undergo PMRT. This is the first meta-analysis to focus on the risks of PMRT with respect to each type of complication encountered with immediate implant-based breast reconstruction, and it provides a clear trend based on 15 well-controlled cohort studies that were published in the past 15 years, comprised of more than 8200 prosthetic reconstruction cases.
Not surprisingly, we found a significant trend toward higher rates of total complications, capsular contracture, and reconstruction failure in patients who received PMRT as we have previously observed. Furthermore, we also observed a higher rate of grade III/IV capsular contractures that require capsulotomy among patients with reconstructions who received PMRT. We also demonstrated an increased rate of severe capsular contractures and worse cosmetic and satisfaction results among patients who received PMRT.
Although complication rates were higher in patients who received PMRT, the reconstruction failure rate was acceptably low (11.1%), and rates of capsular contracture (30.7%) were acceptable in light of the high patient satisfaction. On the basis of the evidence from this meta-analysis, we think that patients who are motivated enough should certainly undergo immediate breast reconstruction, particularly if the approach that we have outlined is followed carefully. Patients with advanced breast cancers often do not have the opportunity to return for delayed reconstruction because of disease progression. We propose that undergoing both immediate implant-based breast reconstruction and PMRT is still quite acceptable.
This meta-analysis has several potential limitations that should be taken into account. First, a limitation of the current study is the quality of the supporting literature. No randomized trials address the efficacy of PMRT. All the published data were obtained from retrospective cohort studies. Second, only English language articles were considered in our analysis. If the search had been extended to include literature published in other languages, then it is possible that additional relevant trials may have been identified. In addition, many of the aforementioned studies are limited by a small number of patients; heterogeneous patient populations; and variations in the timing, dosage, and duration of irradiation.
6. Conclusion
Our study found that PMRT for patients who underwent immediate implant-based breast reconstruction resulted in higher risks of total complications, capsular contracture, and reconstruction failure. However, PMRT is still the standard adjuvant therapy for mastectomy patients who have opted for immediate implant-based breast reconstruction. Thus, it is important that patients are well prepared and preoperatively counseled for the possibility of these complications. A longer follow-up is warranted to assess recurrent cancer, revision surgery, and reconstruction failure.
Footnotes
Abbreviations: CI = confidence interval, HR = hazard ratio, MeSH = Medical Subjects Headings, OR = odds ratio, PMRT = postmastectomy radiation therapy.
Authorship: DLF and SLW contributed substantially to the conception and design of this study, and they approved the final version for publication. YP and TCM contributed to the analysis, interpreted all of the data, and drafted the article. YP critically revised the article for important intellectual content.
The authors have no conflict of interest.
References
- [1].Overgaard M, Hansen PS, Overgaard J, et al. Postoperative radiotherapy in high-risk premenopausal women with breast cancer who receive adjuvant chemotherapy. Danish Breast Cancer Cooperative Group 82b Trial. N Engl J Med 1997;337:949–55. [DOI] [PubMed] [Google Scholar]
- [2].Overgaard M, Jensen MB, Overgaard J, et al. Postoperative radiotherapy in high-risk postmenopausal breast-cancer patients given adjuvant tamoxifen: Danish Breast Cancer Cooperative Group DBCG 82c randomised trial. Lancet 1999;353:1641–8. [DOI] [PubMed] [Google Scholar]
- [3].Tendulkar RD, Rehman S, Shukla ME, et al. Impact of postmastectomy radiation on locoregional recurrence in breast cancer patients with 1-3 positive lymph nodes treated with modern systemic therapy. Int J Radiat Oncol Biol Phys 2012;83:e577–81. [DOI] [PubMed] [Google Scholar]
- [4].Delanian S, Lefaix JL. The radiation-induced fibroatrophic process: therapeutic perspective via the antioxidant pathway. Radiother Oncol 2004;73:119–31. [DOI] [PubMed] [Google Scholar]
- [5].Disa JJ, McCarthy CM, Mehrara BJ, et al. Postmastectomy reconstruction: an approach to patient selection. Plast Reconstr Surg 2009;124:43–52. [DOI] [PubMed] [Google Scholar]
- [6].Percec I, Bucky LP. Successful prosthetic breast reconstruction after radiation therapy. Ann Plast Surg 2008;60:527–31. [DOI] [PubMed] [Google Scholar]
- [7].Whitfield GA, Horan G, Irwin MS, et al. Incidence of severe capsular contracture following implant-based immediate breast reconstruction with or without postoperative chest wall radiotherapy using 40 Gray in 15 fractions. Radiother Oncol 2009;90:141–7. [DOI] [PubMed] [Google Scholar]
- [8].Taghizadeh R, Moustaki M, Harris S, et al. Does post-mastectomy radiotherapy affect the outcome and prevalence of complications in immediate DIEP breast reconstruction? A prospective cohort study. J Plast Reconstr Aesthet Surg 2015;68:1379–85. [DOI] [PubMed] [Google Scholar]
- [9].Jhaveri JD, Rush SC, Kostroff K, et al. Clinical outcomes of postmastectomy radiation therapy after immediate breast reconstruction. Int J Radiat Oncol Biol Phys 2008;72:859–65. [DOI] [PubMed] [Google Scholar]
- [10].Anderson PR, Freedman G, Nicolaou N, et al. Postmastectomy chest wall radiation to a temporary tissue expander or permanent breast implant: is there a difference in complication rates? Int J Radiat Oncol Biol Phys 2009;74:81–5. [DOI] [PubMed] [Google Scholar]
- [11].Tallet AV, Salem N, Moutardier V, et al. Radiotherapy and immediate two-stage breast reconstruction with a tissue expander and implant: complications and esthetic results. Int J Radiat Oncol Biol Phys 2003;57:136–42. [DOI] [PubMed] [Google Scholar]
- [12].Stralman K, Mollerup CL, Kristoffersen US, et al. Long-term outcome after mastectomy with immediate breast reconstruction. Acta Oncol 2008;47:704–8. [DOI] [PubMed] [Google Scholar]
- [13].Spear SL, Onyewu C. Staged breast reconstruction with saline-filled implants in the irradiated breast: recent trends and therapeutic implications. Plast Reconstr Surg 2000;105:930–42. [DOI] [PubMed] [Google Scholar]
- [14].Reish RG, Lin A, Phillips NA, et al. Breast reconstruction outcomes after nipple-sparing mastectomy and radiation therapy. Plast Reconstr Surg 2015;135:959–66. [DOI] [PubMed] [Google Scholar]
- [15].Nava MB, Pennati AE, Lozza L, et al. Outcome of different timings of radiotherapy in implant-based breast reconstructions. Plast Reconstr Surg 2011;128:353–9. [DOI] [PubMed] [Google Scholar]
- [16].Lin KY, Blechman AB, Brenin DR. Implant-based, two-stage breast reconstruction in the setting of radiation injury. Plast Reconstr Surg 2012;129:817–23. [DOI] [PubMed] [Google Scholar]
- [17].Kearney AM, Brown MS, Soltanian HT. Timing of radiation and outcomes in implant-based breast reconstruction. J Plast Reconstr Aesthet Surg 2015;68:1719–26. [DOI] [PubMed] [Google Scholar]
- [18].Ho AL, Bovill ES, Macadam SA, et al. Postmastectomy radiation therapy after immediate two-stage tissue expander/implant breast reconstruction. Plast Reconstr Surg 2014;134:1e–0e. [DOI] [PubMed] [Google Scholar]
- [19].Jimenez-Puente A, Prieto-Lara E, Rueda-Dominguez A, et al. Complications in immediate breast reconstruction after mastectomy. Int J Technol Assess Health Care 2011;27:298–304. [DOI] [PubMed] [Google Scholar]
- [20].Cordeiro PG, Pusic AL, Disa JJ, et al. Irradiation after immediate tissue expander/implant breast reconstruction: outcomes, complications, aesthetic results, and satisfaction among 156 patients. Plast Reconstr Surg 2004;113:877–81. [DOI] [PubMed] [Google Scholar]
- [21].Cordeiro PG, Albornoz CR, McCormick B, et al. The impact of postmastectomy radiotherapy on two-stage implant breast reconstruction. Plast Reconstr Surg 2014;134:588–95. [DOI] [PubMed] [Google Scholar]
- [22].Chen TA, Momeni A, Lee GK. Clinical outcomes in breast cancer expander-implant reconstructive patients with radiation therapy, Journal of Plastic. J Plast Reconstr Aesthet Surg 2016;69:14–22. [DOI] [PubMed] [Google Scholar]
- [23].Behranwala KA, Dua RS, Ross GM, et al. The influence of radiotherapy on capsule formation and aesthetic outcome after immediate breast reconstruction using biodimensional anatomical expander implants. J Plast Reconstr Aesthet Surg 2006;59:1043–51. [DOI] [PubMed] [Google Scholar]
- [24].Ascherman JA, Hanasono MM, Newman MI, et al. Implant reconstruction in breast cancer patients treated with radiation therapy. Plast Reconstr Surg 2006;117:359–65. [DOI] [PubMed] [Google Scholar]
- [25].Anderson PR, Freedman G, Nicolaou N, et al. Postmastectomy chest wall radiation to a temporary tissue expander or permanent breast implant—is there a difference in complication rates? Int J Radiat Oncol Biol Phys 2009;74:81–5. [DOI] [PubMed] [Google Scholar]


