Abstract
Recently, clinical application of 3D printed model was increasing. However, there was no systemic study for confirming the precision and reliability of 3D printed model. Some senior clinical doctors mistrusted its reliability in clinical application. The purpose of this study was to evaluate the precision and reliability of stereolithography appearance (SLA) 3D printed model.
Some related parameters were selected to research the reliability of SLA 3D printed model. The computed tomography (CT) data of bone/prosthesis and model were collected and 3D reconstructed. Some anatomical parameters were measured and statistical analysis was performed; the intraclass correlation coefficient (ICC) was used to was used to evaluate the similarity between the model and real bone/prosthesis. the absolute difference (mm) and relative difference (%) were conducted. For prosthesis model, the 3-dimensional error was measured.
There was no significant difference in the anatomical parameters except max height (MH) of long bone. All the ICCs were greater than 0.990. The maximum absolute and relative difference were 0.45 mm and 1.10%; The 3-dimensional error analysis showed that positive/minus distance were 0.273 mm/0.237 mm.
The application of SLA 3D printed model in diagnosis and treatment process of complex orthopedic disease was reliable and precise.
Keywords: 3-dimensional printing, orthopedic application, precision, reliability, stereolithography appearance model ;
1. Introduction
In recent years, with the development of 3-dimensional (3D) printed technology, its application in medical field has become increasingly widespread, and its application value has been widely recognized especially in preoperative plan of arthroplasty.[1] The study by Lantada and Morgado[2] in 2012 showed that the medicine application occupy 15% share of a variety of 3D printing applications, and in medicine application, the radiographic imaging, orthopedic, and anatomy accounted for 43%. 3D printing technology can be divided into metallic materials printing and nonmetallic materials printing based on the materials used. Metallic materials printing includes selective laser melting (SLM), selective laser sintering (SLS), and electron beam melting (EBM); nonmetallic materials printing includes fused deposition modeling (FDM), stereolithography appearance (SLA), laminated object manufacturing (LOM), and so on.[3] Preoperative plan, simulation operation, and template design can be carried out based on 3D printed models fabricated by SLA, FDM, SLM, and SLS technology, which were all belong to 3D printing technology.[4–8]
The application of 3D printing technology could benefit the diagnosis and treatment procedure of complex orthopedic disease in following ways; First, it could make the diagnosis more accurate; Second, it could help the surgeon do the preoperative design to reduce the duration of operation and amount of bleeding, and it made a positive role in the postoperative rehabilitation process; Lastly, 3D printed model could provide a barrier-free communication between the surgeon and patients due to its visual characteristic. Recently, because 3D printed model can help doctors observe the illness intuitively and communicate with patients easily, the application of 3D printed model was common in preoperative aided diagnosis and operation simulation of the orthopedic diseases, such as clavicle fractures, old pelvic injuries, finger reconstruction, acetabular fractures, complex acetabular defects, femur fractures.[9–19] The most widely used technology was SLA, the principle was that using a particular wavelength and intensity of the laser focused to photosensitive material surface, made it solidification, and completed a level of drawing. Then, the platform was lifted a layer of height in the vertical direction, another level of material was solidificate again. A 3-dimensional entity was constituted by layer upon layer overlay.[3]
However, with the increase in orthopedic application of 3D printed model, there was no systemic study for confirming the precision of 3D printed bone and prosthesis model by SLA technology. And in the production process of SLA 3D printed model, there were some factors that would affected the precision of model such as artificial processing of the model, support structure, and thermal deformation of material. For the situation, some researchers, especially the senior clinical doctors, mistrusted its precision and tried to know the reliability in orthopedic application. For instance, the size precision of the prosthesis model was crucial for operation simulation; the discrepancy of marrow cavity between model and real bone was vital for the selection of prosthetic size; the distance error of some anatomic landmarks in irregular bone was important for accurate diagnosis of disease and preoperative plan. If the model error is beyond the acceptable range, it would make the surgical plan to be unreasonable, and the surgical duration, the risk of anesthesia, and the amount of bleeding would also increase. So, the research in precision of above content was imperative. Since 2013, there were 86 patients with the 3D printing aided diagnosis, preoperative plan, or operation simulation in Orthopedic 3D Printing Operation Design Center Affiliated to the Second Hospital of Jilin University.
In this study, the 61 unbroken 3D printed models of bones or prostheses of the patients were selected for verifying the precision so that the clinicians use the models safely. The models were divided into 3 groups, named long bone, irregular bone, and prosthesis, respectively. Some parameters of models were measured to analysis the precision of the SLA 3D printed model.
2. Materials and methods
2.1. Ethical statement
Before the study, the “informed consent” was obtained from all patients and the approval of Ethics committee of the Second Hospital of Jilin University was obtained, including any relevant details. All the study was performed in accordance with relevant guidelines and regulations.
2.2. The original data collection
A total of 61 SLA-3D printed models of 39 patients (22 Female, 17 Male, age: 19–67) were involved in the study during June 2014 to June 2016. The computed tomography (CT) (Philips iCT 256 with X-ray tube current 232 mA and KVP 120 kV, the pixel size is 0.52 mm, slice thickness is 0.9 mm, and spacing between slices is 0.45 m, PHILIPS, Amsterdam, Netherlands) data of patients were collected. Then, the CT data were exported in the format of DICOM, and 3D reconstruction of images by software MIMICS 19.0 (Materialise interactive medical image control system; Materialise, Belgium) was performed. Finally, the data were exported in the format of STL.
2.3. 3D printed models and CT data collection of models
After obtaining the STL file, we imported the file into MAGICS 18.0 (Materialise interactive medical image control system; Materialise, Belgium) to make the support structure, and then exported to 3D printing equipment (SLA-450; Shining, China) in format of magics to start printing. The model printing process is shown in Fig. 1. The models were photosensitive resin material. When the 61 unbroken 3D printed models were collected, the CT scan of models was performed by the above CT equipment.
Figure 1.
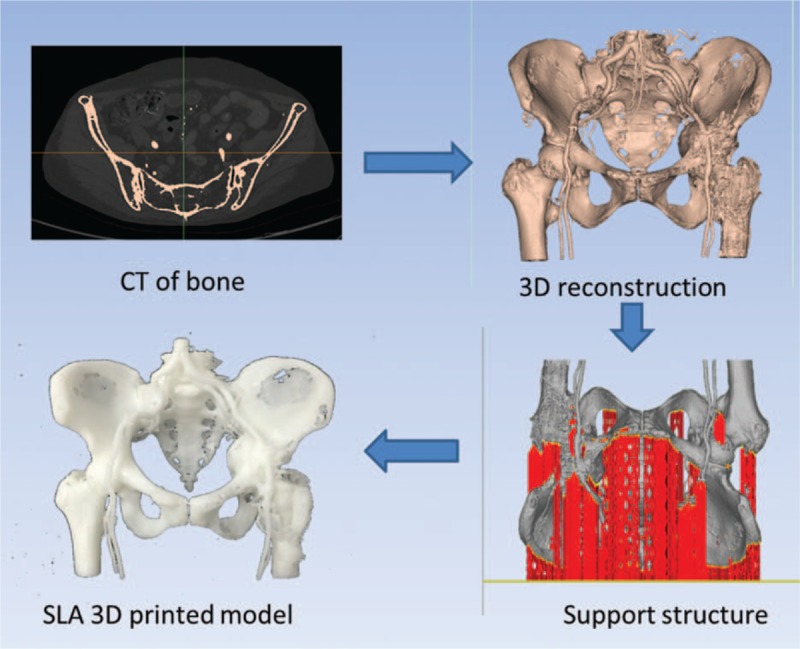
The printing process of model: First, the CT data of patient were collected, and then, the 3D reconstruction of data was performed; next, the support structure was added; finally, the SLA model was printed by SLA-450 printer.
2.4. Comparison of models and bones
The 61 unbroken models were divided into 3 groups according to their characteristics, including 28 long bone models, 11 irregular bone models, and 22 prosthesis models. The original CT data and model CT data of above 61 pairs were 3D reconstructed by MIMICS 19.0 (Fig. 2). According to the clinical practical application, some anatomical and dimensional parameters were selected, and then, these parameters (Table 1 and Fig. 3) of 3-dimensional data were measured by the measuring module of MIMICS 19.0. Next, the absolute error (mm) and relative error (%) of parameters were conducted by the following formulas:
Figure 2.
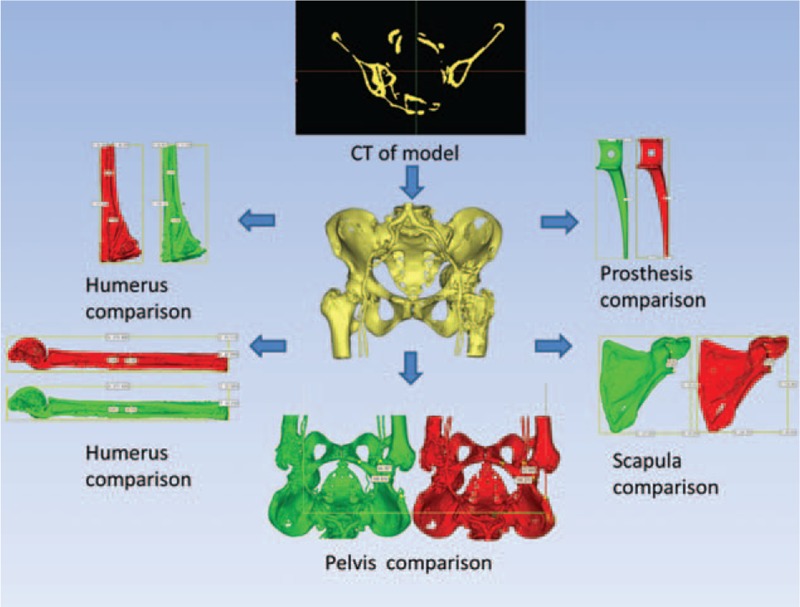
The comparison of bone and model: First, the CT data of SLA model were collected, and then, the 3D reconstruction of data was performed; finally, a comparison was made between the bone and model data.
Table 1.
Anatomical landmarks and linear measures.

Figure 3.
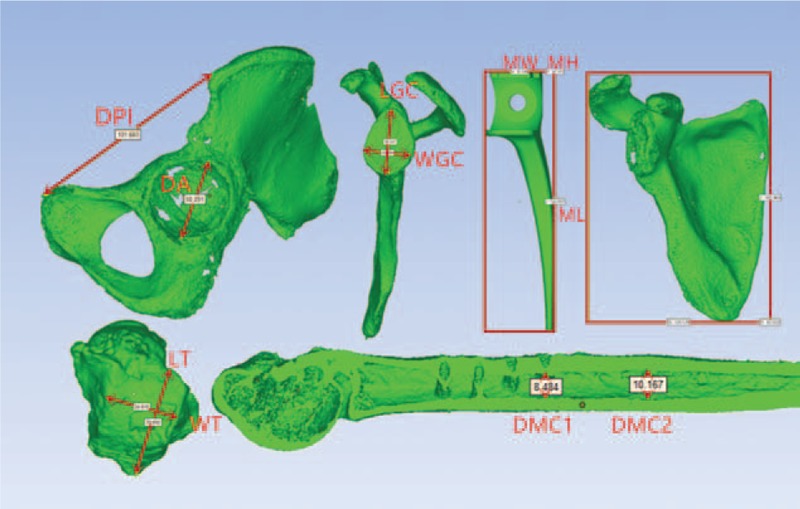
The selection of related parameters: The parameters were shown by red arrow and line, such as MW, MH, ML, LGC, WGC, DPI, DA, LT, WT, and DMC.
Absolute difference(mm)=
model group value – bone group value (Eq1.1)
Relative difference (%)=
100× (model group value-bone group value)÷bone group value (Eq1.2)
For prosthesis model, which inside was solid without the support structure, the 3-dimensional error was measured by Geomagic Studio 2012 (Geomagic, NC) (Table 2 and Fig. 4). The 3-dimensional error of other 2 groups was not measured due to the influence of support structure inside.
Table 2.
The 3D error (mm) analysis between the model and prosthesis.
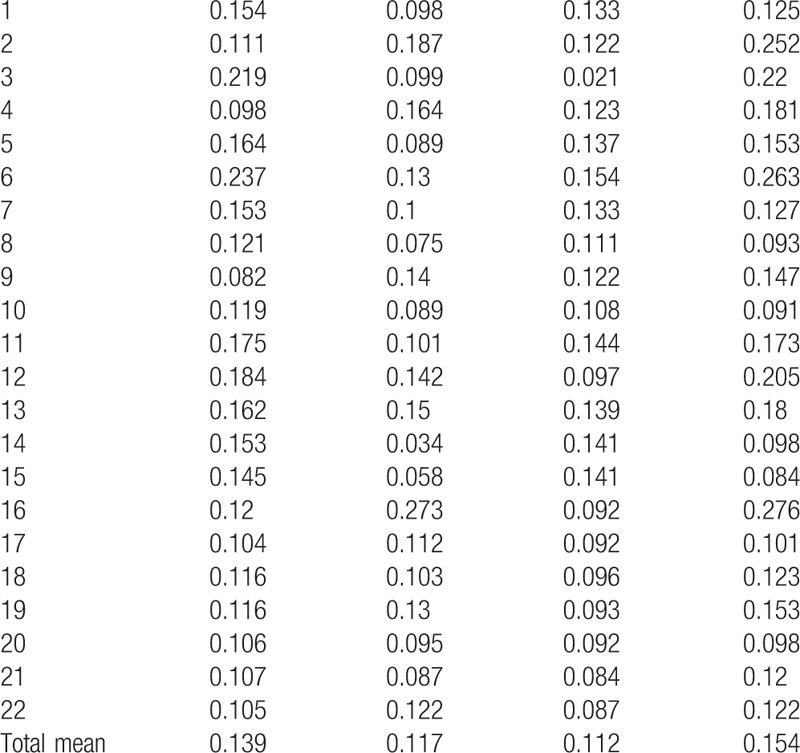
Figure 4.
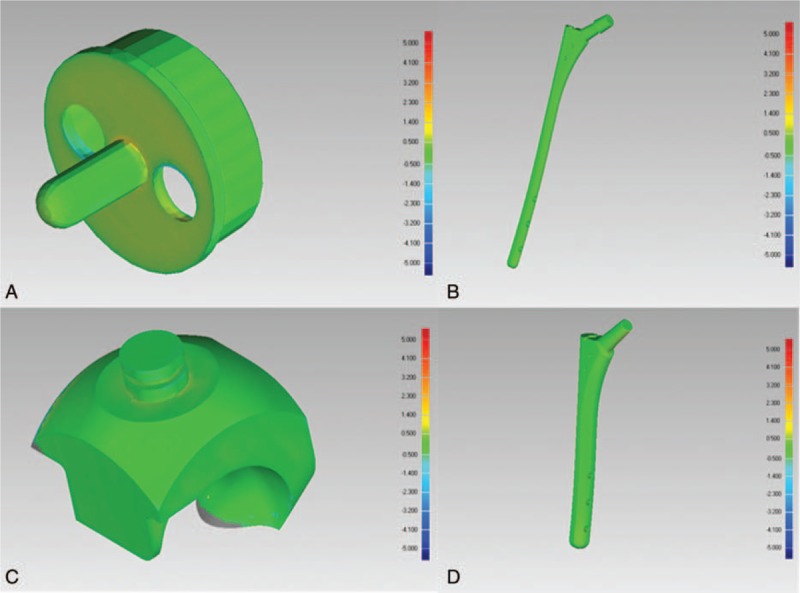
The measure of 3-dimensional error: The 3-dimensional error was shown by the chromatostrip, and the obvious error appears on the edge. (A) shoulder prosthesis; (B and D) femur prosthesis; (C) elbow prosthesis.
2.5. Statistical analysis
The above parameters of 3 groups were analyzed by the SPSS 10.0 (Statistical Product and Service Solutions; IBM, Chicago, Illinois, America), the paired t test was selected, with the level of significant set at P ≤ .05. The intraclass correlation coefficient (ICC) was used to evaluate the similarity between the model and real bone (Tables 1–4).
Table 4.
The parameters and comparison of irregular bones and models, N = 11.
All above studies were conducted during July 2016 to November 2016. After data collection, we did not had access to information that could identify individual participants.
3. Results
The maximum absolute and relative difference were 0.45 mm and 1.10%; the total mean was 0.18 mm and 0.37% (Table 3), respectively. The 3-dimensional error analysis showed that positive distance, minus distance, mean distance, and standard deviation were 0.237, 0.273, 0.154, and 0.276 mm, and the total mean were 0.139, 0.117, 0.112, and 0.154 mm (Table 2), respectively.
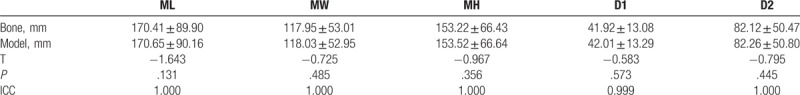
Table 3.
Mean absolute (mm) and relative (%) differences for all model measurements in comparison with bones.
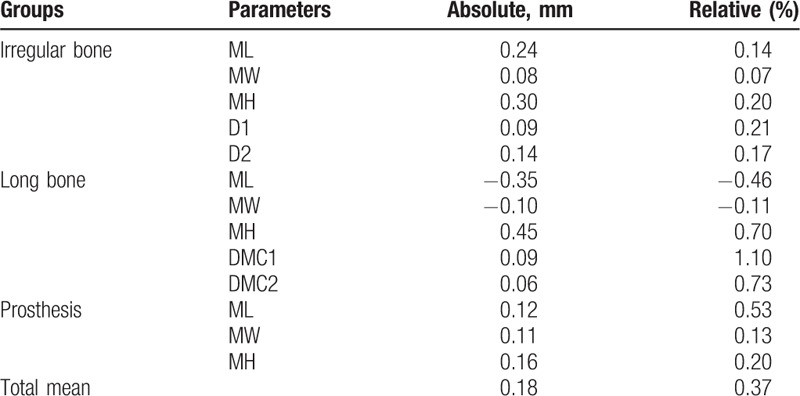
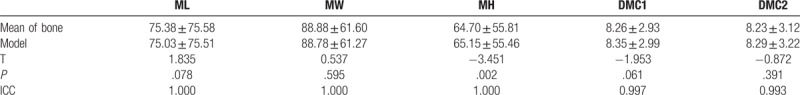
The statistical analysis showed all the ICC of parameters were greater than 0.990; there was a significant difference in MH of long bone groups (P = .002) and other parameters did not show a significant difference between bones and models (Tables 4–6).
Table 6.
The parameters and comparison of prostheses and models, N = 22.
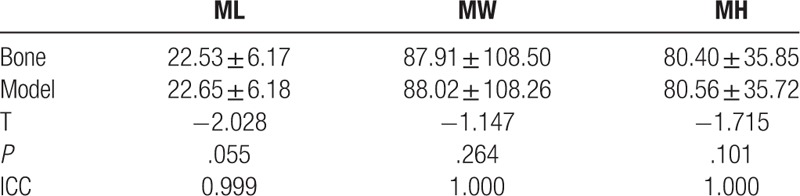
Table 5.
The parameters and comparison of long bones and models, N = 28.
4. Discussion
The diagnosis and treatment of complex orthopedic disease is a difficult problem for orthopedic surgeon. The application of 3D printing technology in medicine provides a new way to solve the problem. However, with the wide application of the 3D printed models,[9,11,13–16,18,19] the precision and reliability of model have also been questioned. Previous studies have reported on CT image dimensional errors ranging from 0.9 to 2.16%[12]; when images are converted to STL format, the surface of the model is converted into a large number of refined triangles that can improve the quality of image and add precision to the image-reslicing algorithm.[17] So, CT data were considered reliable, which were converted into STL format. In this study, the CT scan was chosen to make the reverse research on comparison of precision between the model and bone in STL format, and 61 models of bones or prostheses were provided. The precision and reliability of models were evaluated by the size precision, the absolute and relative difference of anatomic parameters between model and original data, as well as the 3-dimensional error of prosthesis.
The diameter of the medullary cavity of long bone, such as humerus, femur, tibia, ulna, and radius, was often concerned by the surgeon in the clinical procedure of arthroplasty and fixation surgery. During the arthroplasty and internal fixation, the size selection of intramedullary nail and prosthetic stem were influenced by the diameter of the medullary cavity. For irregular bone, such as ilium, scapula, and talus, the diameter of glenoid cavity and acetabulum and the distance between some anatomical landmarks were concerned by the surgeon, because the formulation of surgical plan and prosthetic selection was affected by that. For prosthetic model, the 3-dimensional error should be studied, because the precision of prosthetic location and the selection of prosthetic size were affected by that. In addition, the absolute and relative difference between the SLA 3D printed model and original CT data were studied to compare with the precision of model by other 3D printing technology, and they could show whether the error of model was acceptable or not in clinical application; the result was satisfactory, as described below.
The maximum absolute difference was 0.45 mm, and the mean absolute difference was 0.18 mm (Table 3); it can be ignored for the CT data whose thickness was 0.9 mm. The maximum relative difference was 1.10%, and the mean relative difference was 0.37%; it was lower than SLS, 3DP, and PolyJet technology reported by Ibrahim et al.[12] The error of 0.45 mm could also be accepted in the orthopedic surgery.
Only the 3-dimensional error of prosthesis group is analyzed, because prosthesis was solid without the influence of the internal support structure. The support structure was necessary in the manufacturing process of 3D printed model, and it would be artificially removed after the finishing of model, but the internal support structure could not be removed. The 3-dimensional error analysis of long bone and irregular bone group was not performed, because the analysis result would be affected by the internal support structure in pulp cavity and cancellous bone. The positive distance, minus distance, and mean distance were 0.237, 0.273, and 0.154 mm, respectively; obviously, the error can be accepted for 3D printing devices with a precision of 0.1 mm. The mean space error of 22 models, 9 were fine, 13 were medium based on ISO 2768-1 (International Organization for Standardization, 1987).[17] For the orthopedic clinical application, the error of 0.273 mm can be ignored.
There was no significant difference in all selected parameters except MH of long bone between the bone and model group; All the ICCs were greater than 0.990; It means that the CT data of bone and model can be considered to be the same. According to the result, the precision of SLA 3D printed model was better than the precision of model printed by polylactic acid (PLA).[20]
In this study, MH of long bone, and the maximum absolute difference of 0.45 mm were not expected results; the partial volume effect of CT scan may be the reason, as Fig. 4 showed that the obvious error appears on the edge; if the measurement was performed on the real model, the value should be more consistent with the original CT data of bone. In addition, the result can be affected by the artificial processing of the model, removal of support structure, and thermal deformation of material and other factors in printing procedure. The anthropic factors can be avoided by improving operation process as far as possible.
On the basis of the above results, the 3D printed model can be safely used in aided diagnosis, preoperative plan, and operation simulation in complex orthopedic disease. 3D printing technology can help doctors to improve the diagnosis and treatment level, and can also make patients have an intuitionistic understanding of their condition; the model can increase the satisfaction of both doctors and patients on diagnosis and treatment process.[9] Compared with conventional imaging methods, 3D printed model was applied in clinic with intuitionistic, clear and exercisable advantage, and the preoperative application of 3D printing technology for aided diagnosis of patients can shorten operation time and reduce surgical trauma.[10,13] This study provides sufficient theoretical support for the reliability and precision of clinical application of 3D printed model. In the future, long-term follow-up of patients who used 3D printing technology was needed; the retrospective study would be performed to observe the long-term effect of 3D printing technology application.
5. Conclusion
The 3-dimensional error and absolute/relative difference of SLA 3D printed model were controlled in the range of satisfaction. The data of the model were highly consistent with the original CT data. The application of model in diagnosis and treatment process of complex orthopedic disease was reliable and precise.
Footnotes
Abbreviations: CT = computed tomography, DA = diameter of the acetabulum, DMC = diameter of the marrow cavity, DPI = distance of pubic tubercle-anterior superior iliac spine, EBM = electron beam melting, FDM = fused deposition modeling, ICC = intraclass correlation coefficient, LGC = length of the glenoid cavity, LOM = laminated object manufacturing, LT = length of the trochlear, MH = max height, ML = max length, MW = max width, SLA = stereolithography appearance, SLM = selective laser melting, SLS = selective laser sintering, WGC = width of the glenoid cavity, WT = width of the trochlear.
YZ and QH contribute equally to this work
Funding/support: This work was supported by the Department of Jilin province natural science foundation of China [NO: 2015Q019], Jilin province health department of scientific research funds of China [NO:2013WST046].
The authors declare that there is no conflict of interest related to this paper.
References
- [1].Rengier F, Mehndiratta A, von Tengg-Kobligk H, et al. 3D printing based on imaging data: review of medical applications. Int J Comput Assist Radiol Surg 2010;5:335–41. [DOI] [PubMed] [Google Scholar]
- [2].Lantada AD, Morgado PL. Rapid prototyping for biomedical engineering: current capabilities and challenges. Annu Rev Biomed Eng 2012;14:73–96. [DOI] [PubMed] [Google Scholar]
- [3].Webb PA. A review of rapid prototyping (RP) techniques in the medical and biomedical sector. J Med Eng Technol 2000;24:149–53. [DOI] [PubMed] [Google Scholar]
- [4].Starosolski ZA, Kan JH, Rosenfeld SD, et al. Application of 3-D printing (rapid prototyping) for creating physical models of pediatric orthopedic disorders. Pediatr Radiol 2014;44:216–21. [DOI] [PubMed] [Google Scholar]
- [5].Rose AS, Kimbell JS, Webster CE, et al. Multi-material 3D models for temporal bone surgical simulation. Ann Otol Rhinol Laryngol 2015;124:528–36. [DOI] [PubMed] [Google Scholar]
- [6].Hochman JB, Kraut J, Kazmerik K, et al. Generation of a 3D printed temporal bone model with internal fidelity and validation of the mechanical construct. Otolaryngol Head Neck Surg 2014;150:448–54. [DOI] [PubMed] [Google Scholar]
- [7].Bagaria V, Deshpande S, Rasalkar DD, et al. Use of rapid prototyping and three-dimensional reconstruction modeling in the management of complex fractures. Eur J Radiol 2011;80:814–20. [DOI] [PubMed] [Google Scholar]
- [8].Chung KJ, Hong DY, Kim YT, et al. Preshaping plates for minimally invasive fixation of calcaneal fractures using a real-size 3D-printed model as a preoperative and intraoperative tool. Foot Ankle Int 2014;35:1231–6. [DOI] [PubMed] [Google Scholar]
- [9].Bizzotto N, Tami I, Tami A, et al. 3D Printed models of distal radius fractures. Injury 2016;47:976–8. [DOI] [PubMed] [Google Scholar]
- [10].Chae MP, Lin F, Spychal RT, et al. 3D-printed haptic “reverse” models for preoperative planning in soft tissue reconstruction: a case report. Microsurgery 2015;35:148–53. [DOI] [PubMed] [Google Scholar]
- [11].Hurson C, Tansey A, O’Donnchadha B, et al. Rapid prototyping in the assessment, classification and preoperative planning of acetabular fractures. Injury 2007;38:1158–62. [DOI] [PubMed] [Google Scholar]
- [12].Ibrahim D, Broilo TL, Heitz C, et al. Dimensional error of selective laser sintering, three-dimensional printing and PolyJet models in the reproduction of mandibular anatomy. J Craniomaxillofac Surg 2009;37:167–73. [DOI] [PubMed] [Google Scholar]
- [13].Kim HN, Liu XN, Noh KC. Use of a real-size 3D-printed model as a preoperative and intraoperative tool for minimally invasive plating of comminuted midshaft clavicle fractures. J Orthop Surg Res 2015;10:91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Li H, Wang L, Mao Y, et al. Revision of complex acetabular defects using cages with the aid of rapid prototyping. J Arthroplasty 2013;28:1770–5. [DOI] [PubMed] [Google Scholar]
- [15].Park JH, Lee Y, Shon OJ, et al. Surgical tips of intramedullary nailing in severely bowed femurs in atypical femur fractures: simulation with 3D printed model. Injury 2016;47:1318–24. [DOI] [PubMed] [Google Scholar]
- [16].Tan H, Yang K, Wei P, et al. A novel preoperative planning technique using a combination of CT angiography and three-dimensional printing for complex toe-to-hand reconstruction. J Reconstr Microsurg 2015;31:369–77. [DOI] [PubMed] [Google Scholar]
- [17].Winder J, Bibb R. Medical rapid prototyping technologies: state of the art and current limitations for application in oral and maxillofacial surgery. J Oral Maxillofac Surg 2005;63:1006–15. [DOI] [PubMed] [Google Scholar]
- [18].Wu XB, Wang JQ, Zhao CP, et al. Printed three-dimensional anatomic templates for virtual preoperative planning before reconstruction of old pelvic injuries: initial results. Chin Med J 2015;128:477–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Zeng C, Xing W, Wu Z, et al. A combination of three-dimensional printing and computer-assisted virtual surgical procedure for preoperative planning of acetabular fracture reduction. Injury 2016;47:2223–7. [DOI] [PubMed] [Google Scholar]
- [20].Wu AM, Shao ZX, Wang JS, et al. The accuracy of a method for printing three-dimensional spinal models. PLoS One 2015;10:e0124291. [DOI] [PMC free article] [PubMed] [Google Scholar]


