Abstract
Background and Aims: Low serum 25-OH D levels are associated with increased cardiovascular morbidity and mortality. Recent studies have linked 25-OH D deficiency with the presence of CAD. Women, especially post-menopausal, tend to suffer from accelerated atherosclerosis, along with vitamin D deficiency. In the present study we sought to investigate whether there is a direct association of coronary artery luminal stenosis with 25-OH D deficiency in women. Patients and methods: We enrolled women aged >40 who were scheduled to undergo elective coronary angiography between 3/2011 and 10/2016 in a prospective observational study. Results: We included a total of 105 women. Patients had hypertension (73%), hyperlipidemia (54%), diabetes (29%), smoking (31%), family history of CAD (62%), and known CAD (21%). Median 25-OH D levels were 15.8 ng/mL (range, 3.9-79). Patients had left-anterior descending (31%), left circumflex (22%), and right coronary artery disease (26%); 27% had 2-vessel and 11% had 3-vessel disease. There was a significant inverse correlation between 25-OH D levels and the degree of maximum luminal stenosis. The burden of CAD increased across categories of worsening 25-OH D deficiency. Conclusions: Vitamin D deficiency is associated with the degree of luminal stenosis and burden of CAD in women undergoing coronary angiography. Future studies should investigate if the repletion of 25-OH D impacts the progression of CAD and cardiovascular mortality.
Keywords: 25-OH D, vitamin D, coronary artery disease, women
Introduction
A growing body of evidence suggests that low serum levels of 25-OH D are associated with higher incidence of cardiovascular disease and increased cardiovascular and all-cause mortality [1-5]. Multiple studies have tried to elucidate a causal mechanism with inconclusive findings. Some authors suggest an association of vitamin D deficiency and coronary artery calcification [6,7], however others found no correlation [8]. Moreover, a large prospective study found an association of low 25-OH D levels with increased risk for myocardial infarction [9], and the Framingham Study revealed a graded increase in cardiovascular events with lower levels of 25-OH D [2]. However, vitamin D supplementation did not appear to affect the coronary artery calcified plaque burden [10].
It has been established that women who enter menopause suffer from accelerated atherosclerosis and increased cardiovascular mortality [11,12]. Similarly, the association of 25-OH D deficiency with CAD appears to be more pronounced amongst women [3,13], raising the question if there is a hormonal interaction linking 25-OH D with the development of CAD in this population.
Recognizing the paucity of literature in this topic, we aimed to prospectively investigate if there is an association of CAD with 25-OH D deficiency in women, in a geographical area with high prevalence of vitamin D deficiency.
Materials and methods
Women over the age of 40 who were scheduled to undergo elective coronary angiography (CAG) at West Pennsylvania Hospital between 3/2011 and 10/2016 were enrolled in a prospective observational study. All labs were drawn at the time of coronary angiography. Patients who received any vitamin supplements up to 1 month prior were excluded from the study, along with patients who had history of tumors affecting calcium and vitamin D homeostasis (parathyroid tumors, primary or metastatic bone tumors, and renal cell carcinoma). Only patients who signed informed consent were included in the study. The study was approved by the institutional review board.
The primary outcome was to investigate if there is a correlation of 25-OH D levels with the percentage of luminal stenosis, as measured with CAG. Secondary outcomes were to analyze the differences in percentage of luminal stenosis and CAD burden across categories of 25-OH D deficiency (<10, 10-20, and >20 ng/mL), and determine if there is a correlation between 25-OH D levels and high-sensitivity C-reactive protein (HsCRP). Presence of significant multi-vessel disease CAD was defined as at least ≥50% stenosis at more than one of the major coronary arteries [left anterior descending (LAD), left circumflex (LCx), and right coronary artery (RCA)].
Continuous variables were compared using the Wilcoxon rank-sum test and categorical variables were compared using the X2 test or Fisher’s exact test, as appropriate. Pearson’s and Spearman’s rank correlation coefficients were used to assess for linear and non-linear correlations between 25-OH D levels and CAD. Statistical significance for all tests was set at a two-tailed α<0.05. Data were analyzed with SPSS (v.22, IBM Corporation, Armonk, NY, USA).
Results
A total of 105 women were included in the study (Table 1). Patients had hypertension (73%), hyperlipidemia (54%), diabetes (29%), significant smoking history (31%), family history of premature CAD (62%), and known CAD (21%). Overall, 46% were receiving statin and 59% anti-platelet therapy. Median 25-OH D levels were 15.8 ng/mL (range, 3.9-79) and HsCRP 2.9 mg/L (range, 0.1-111).
Table 1.
Characteristics of 105 women who underwent CAG
| Characteristic | N (%) |
|---|---|
| Age, median (range) | 63 (40-90) |
| BMI, median (range) | 31.3 (18.3-51) |
| Hypertension | 77 (73) |
| Hyperlipidemia | 50/92 (54) |
| Diabetes | 30 (29) |
| Smoking | 33 (31) |
| Family history of CAD | 65 (62) |
| Prior PCI | 32 (31) |
| On statin | 48 (46) |
| On antiplatelet agents | 62 (59) |
| Vitamin D levels (ng/mL) | |
| <10 | 21 (20) |
| ≥10 and >20 | 51 (49) |
| ≥20 | 33 (31) |
| PTH, median (range) | 59.6 (249.4) |
Patients had LAD (31%), LCx (22%), and RCA (26%); 27% had 2-vessel and 11% had 3-vessel disease. There was a statistically significant inverse correlation between 25-OH D levels and the degree of maximum luminal stenosis in any coronary vessel (ρ=-0.21 P=0.02), which met borderline linearity (r=-0.19; P=0.05). This was also evident for LCx and RCA individually, whereas it was marginally non-significant for the LAD (Table 2). There was a statistical significant association between the prespecified categories of 25-OH D levels and degree of maximum luminal stenosis in any (ρ=-0.27; P<0.01) and all vessels individually (ρ=-0.2; P=0.03 for LAD; ρ=-0.33; P<0.001 for LCx; ρ=-0.29; P<0.01 for RCA). There was also a significant negative linear correlation between the prespecified 25-OH D categories and burden of CAD (r=-0.25; P=0.009). There was no association between the levels of 25-OH D levels and HsCRP. The percentage of patients with greater than 50% coronary artery stenosis significantly increased across categories of vitamin D sufficient (31% for 25-OH D level of >20 ng/mL), vitamin D insufficient (39% for 25-OH D level of 10-20 ng/mL), and vitamin D deficient (67% for 25-OH D level of <10 ng/mL) patients (P=0.03; Figure 1).
Table 2.
Association of 25-OH D levels with the degree of coronary artery stenosis
| Mean (SD) | ρ | P value | |
|---|---|---|---|
| LAD | 30.8 (34.1) | -0.17 | 0.06 |
| LCx | 22.7 (32.4) | -0.29 | <0.01 |
| RCA | 27.3 (36.4) | -0.24 | 0.01 |
| Maximum stenosis in any vessel | 40.7 (38.3) | -0.21 | 0.02 |
Figure 1.
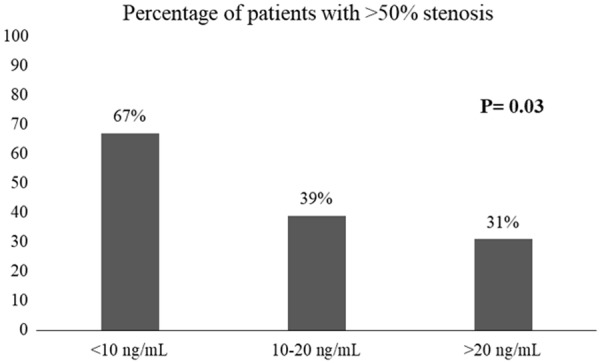
Distribution of patients with >50% coronary artery stenosis in 25-OH D deficient, insufficient and sufficient patients.
Discussion
Vitamin D deficiency is an emerging area of interest given the consistent association with cardiovascular morbidity and mortality in multiple studies [5]. Despite this, the exact mechanism has yet to be elucidated. Preclinical studies have demonstrated that 1,25-OH D is a negative endocrine regulator of the renin-angiotensin system and has a critical role in electrolytes, volume, and blood pressure homeostasis [14,15]. Additionally, studies on human subjects have shown that vitamin D deficiency is associated with vascular endothelial dysfunction, mediated by proinflammatory IL-6 and nuclear factor κB-related activation [16].
Analyses from the NHANES and Framingham datasets have linked low 25-OH D levels with higher incidence of CAD, heart failure and stroke [2,17]. Another study revealed that the severity of 25-OH D deficiency correlates with number of coronary vessels with significant atherosclerosis [18]. Women, particularly when post-menopausal, are at higher risk for vitamin D deficiency [3,19]. Furthermore, an Italian study revealed that lower 25-OH D levels in female patients have a stronger correlation with the prevalence and severity CAD, compared to male patients [13]. In the present study, we found that 25-OH D deficiency directly correlates with the degree of luminal stenosis and burden of CAD.
This association of CAD and vitamin D deficiency raise the question whether the repletion 25-OH D levels has any clinical impact on CAD and cardiovascular mortality. The Women’s Health Initiative trials revealed that supplementation with calcium and vitamin D3 leads to more favorable lipid profiles, with increased HDL levels, along with decrease in LDL and triglyceride levels [20]. These effects were not translated into a benefit in mortality or coronary events [21,22], although some subgroup analyses revealed a benefit in the prevention of heart failure and possible reduction in mortality in early post-menopausal women [22,23]. A meta-analysis of randomized clinical trials found that supplementation with vitamin D3 in 25-OH D deficient individuals is associated with decrease overall mortality [5].
Our study has its limitations. We studied a small sample of a predominantly 25-OH D deficient geographic region, which limits our conclusions whether our findings will be reproducible in different regions. On the other hand, our study had strict inclusion and exclusion criteria and patients were prospectively studied. Also the nature of a cross-sectional analysis precludes its utilization for risk factor identification, nevertheless, the association of 25-OH D deficiency and CAD has been reproducible in multiple trials and meta-analyses. Last, this was an observational study with no intervention group, thus we cannot answer the question if restoring the 25-OH D levels has any impact on the natural progression of CAD.
Conclusions
Our findings suggest an association of 25-OH D deficiency with the degree of luminal stenosis and burden of CAD in women undergoing elective CAG. This adds to the pool of evidence linking vitamin D deficiency to cardiovascular disease and underscores a potential mechanism that requires further investigation. Future studies should aim to elucidate whether the repletion of 25-OH D levels has any impact on CAD progression and cardiovascular mortality.
Disclosure of conflict of interest
None.
References
- 1.Dobnig H, Pilz S, Scharnagl H, Renner W, Seelhorst U, Wellnitz B, Kinkeldei J, Boehm BO, Weihrauch G, Maerz W. Independent association of low serum 25-hydroxyvitamin d and 1,25-dihydroxyvitamin d levels with all-cause and cardiovascular mortality. Arch Intern Med. 2008;168:1340–1349. doi: 10.1001/archinte.168.12.1340. [DOI] [PubMed] [Google Scholar]
- 2.Wang TJ, Pencina MJ, Booth SL, Jacques PF, Ingelsson E, Lanier K, Benjamin EJ, D’Agostino RB, Wolf M, Vasan RS. Vitamin D deficiency and risk of cardiovascular disease. Circulation. 2008;117:503–511. doi: 10.1161/CIRCULATIONAHA.107.706127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Melamed ML, Michos ED, Post W, Astor B. 25-hydroxyvitamin D levels and the risk of mortality in the general population. Arch Intern Med. 2008;168:1629–1637. doi: 10.1001/archinte.168.15.1629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kilkkinen A, Knekt P, Aro A, Rissanen H, Marniemi J, Heliovaara M, Impivaara O, Reunanen A. Vitamin D status and the risk of cardiovascular disease death. Am J Epidemiol. 2009;170:1032–1039. doi: 10.1093/aje/kwp227. [DOI] [PubMed] [Google Scholar]
- 5.Chowdhury R, Kunutsor S, Vitezova A, Oliver-Williams C, Chowdhury S, Kiefte-de-Jong JC, Khan H, Baena CP, Prabhakaran D, Hoshen MB, Feldman BS, Pan A, Johnson L, Crowe F, Hu FB, Franco OH. Vitamin D and risk of cause specific death: systematic review and meta-analysis of observational cohort and randomised intervention studies. BMJ. 2014;348:g1903. doi: 10.1136/bmj.g1903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lee S, Ahuja V, Masaki K, Evans RW, Barinas-Mitchell EJ, Ueshima H, Shin C, Choo J, Hassen L, Edmundowicz D, Kuller LH, Willcox B, Sekikawa A. A significant positive association of vitamin D deficiency with coronary artery calcification among middle-aged men: for the ERA JUMP study. J Am Coll Nutr. 2016;35:614–620. doi: 10.1080/07315724.2015.1118651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.de Boer IH, Kestenbaum B, Shoben AB, Michos ED, Sarnak MJ, Siscovick DS. 25-hydroxyvitamin D levels inversely associate with risk for developing coronary artery calcification. J Am Soc Nephrol. 2009;20:1805–1812. doi: 10.1681/ASN.2008111157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jorde UP, Aaronson KD, Najjar SS, Pagani FD, Hayward C, Zimpfer D, Schloglhofer T, Pham DT, Goldstein DJ, Leadley K, Chow MJ, Brown MC, Uriel N. Identification and management of pump thrombus in the heartware left ventricular assist device system: a novel approach using log file analysis. JACC Heart Fail. 2015;3:849–856. doi: 10.1016/j.jchf.2015.06.015. [DOI] [PubMed] [Google Scholar]
- 9.Giovannucci E, Liu Y, Hollis BW, Rimm EB. 25-hydroxyvitamin D and risk of myocardial infarction in men: a prospective study. Arch Intern Med. 2008;168:1174–1180. doi: 10.1001/archinte.168.11.1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Manson JE, Allison MA, Carr JJ, Langer RD, Cochrane BB, Hendrix SL, Hsia J, Hunt JR, Lewis CE, Margolis KL, Robinson JG, Rodabough RJ, Thomas AM Women’s Health Initiative and Women’s Health Initiative-Coronary Artery Calcium Study Investigators. Calcium/vitamin D supplementation and coronary artery calcification in the Women’s Health Initiative. Menopause. 2010;17:683–691. doi: 10.1097/gme.0b013e3181d683b5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Witteman JC, Grobbee DE, Kok FJ, Hofman A, Valkenburg HA. Increased risk of atherosclerosis in women after the menopause. BMJ. 1989;298:642–644. doi: 10.1136/bmj.298.6674.642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mondul AM, Rodriguez C, Jacobs EJ, Calle EE. Age at natural menopause and cause-specific mortality. Am J Epidemiol. 2005;162:1089–1097. doi: 10.1093/aje/kwi324. [DOI] [PubMed] [Google Scholar]
- 13.Verdoia M, Schaffer A, Barbieri L, Di Giovine G, Marino P, Suryapranata H, De Luca G Novara Atherosclerosis Study Group (NAS) Impact of gender difference on vitamin D status and its relationship with the extent of coronary artery disease. Nutr Metab Cardiovasc Dis. 2015;25:464–470. doi: 10.1016/j.numecd.2015.01.009. [DOI] [PubMed] [Google Scholar]
- 14.Li YC, Kong J, Wei M, Chen ZF, Liu SQ, Cao LP. 1,25-Dihydroxyvitamin D(3) is a negative endocrine regulator of the renin-angiotensin system. J Clin Invest. 2002;110:229–238. doi: 10.1172/JCI15219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li YC, Qiao G, Uskokovic M, Xiang W, Zheng W, Kong J. Vitamin D: a negative endocrine regulator of the renin-angiotensin system and blood pressure. J Steroid Biochem Mol Biol. 2004;89-90:387–392. doi: 10.1016/j.jsbmb.2004.03.004. [DOI] [PubMed] [Google Scholar]
- 16.Jablonski KL, Chonchol M, Pierce GL, Walker AE, Seals DR. 25-Hydroxyvitamin D deficiency is associated with inflammation-linked vascular endothelial dysfunction in middle-aged and older adults. Hypertension. 2011;57:63–69. doi: 10.1161/HYPERTENSIONAHA.110.160929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kim DH, Sabour S, Sagar UN, Adams S, Whellan DJ. Prevalence of hypovitaminosis D in cardiovascular diseases (from the national health and nutrition examination survey 2001 to 2004) Am J Cardiol. 2008;102:1540–1544. doi: 10.1016/j.amjcard.2008.06.067. [DOI] [PubMed] [Google Scholar]
- 18.Liew JY, Sasha SR, Ngu PJ, Warren JL, Wark J, Dart AM, Shaw JA. Circulating vitamin D levels are associated with the presence and severity of coronary artery disease but not peripheral arterial disease in patients undergoing coronary angiography. Nutr Metab Cardiovasc Dis. 2015;25:274–279. doi: 10.1016/j.numecd.2014.12.005. [DOI] [PubMed] [Google Scholar]
- 19.Mithal A, Wahl DA, Bonjour JP, Burckhardt P, Dawson-Hughes B, Eisman JA, El-Hajj Fuleihan G, Josse RG, Lips P, Morales-Torres J IOF Committee of Scientific Advisors (CSA) Nutrition Working Group. Global vitamin D status and determinants of hypovitaminosis D. Osteoporos Int. 2009;20:1807–1820. doi: 10.1007/s00198-009-0954-6. [DOI] [PubMed] [Google Scholar]
- 20.Schnatz PF, Jiang X, Vila-Wright S, Aragaki AK, Nudy M, O’Sullivan DM, Jackson R, LeBlanc E, Robinson JG, Shikany JM, Womack CR, Martin LW, Neuhouser ML, Vitolins MZ, Song Y, Kritchevsky S, Manson JE. Calcium/vitamin D supplementation, serum 25-hydroxyvitamin D concentrations, and cholesterol profiles in the Women’s Health Initiative calcium/vitamin D randomized trial. Menopause. 2014;21:823–833. doi: 10.1097/GME.0000000000000188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hsia J, Heiss G, Ren H, Allison M, Dolan NC, Greenland P, Heckbert SR, Johnson KC, Manson JE, Sidney S, Trevisan M Women’s Health Initiative Investigators. Calcium/vitamin D supplementation and cardiovascular events. Circulation. 2007;115:846–854. doi: 10.1161/CIRCULATIONAHA.106.673491. [DOI] [PubMed] [Google Scholar]
- 22.LaCroix AZ, Kotchen J, Anderson G, Brzyski R, Cauley JA, Cummings SR, Gass M, Johnson KC, Ko M, Larson J, Manson JE, Stefanick ML, Wactawski-Wende J. Calcium plus vitamin D supplementation and mortality in postmenopausal women: the Women’s Health Initiative calcium-vitamin D randomized controlled trial. J Gerontol A Biol Sci Med Sci. 2009;64:559–567. doi: 10.1093/gerona/glp006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Donneyong MM, Hornung CA, Taylor KC, Baumgartner RN, Myers JA, Eaton CB, Gorodeski EZ, Klein L, Martin LW, Shikany JM, Song Y, Li W, Manson JE. Risk of heart failure among postmenopausal women: a secondary analysis of the randomized trial of vitamin D plus calcium of the women’s health initiative. Circ Heart Fail. 2015;8:49–56. doi: 10.1161/CIRCHEARTFAILURE.114.001738. [DOI] [PMC free article] [PubMed] [Google Scholar]


