Abstract
Objectives. To examine national trends in the use of various pharmacological pain medication classes by race/ethnicity among the US pain population.
Methods. We used data from the Medical Expenditure Panel Survey to conduct a nationally representative, serial cross-sectional study of the noninstitutionalized US adult population from 2000 to 2015. We identified adults with moderate or severe self-reported pain and excluded individuals with cancer. We used complex survey design to provide national estimates of the percentage of adults with noncancer pain who received prescription pain medications among 4 groups: non-Hispanic White, non-Hispanic Black, Hispanic or Latino, and other.
Results. The age- and gender-adjusted percentage of prescription opioid use increased across all groups, with the greatest increase among non-Hispanic White individuals. By 2015, the percentage of non-Hispanic Black adults using opioids approximated that of non-Hispanic White adults—in 2015, approximately 23% of adults in these 2 groups used opioids.
Conclusions. To our knowledge, this is the first evidence of a narrowing divide in opioid prescribing by race. However, in the context of the national epidemic of opioid-related addiction and mortality, opioid-related risks do not appear commensurate with the purported benefits.
Racial/ethnic disparities in pain management have been well documented in a variety of clinical settings.1–5 In the context of the growing opioid epidemic in the United States, non-Hispanic White individuals are known to be at elevated risk for opioid use for pain management compared with other racial/ethnic groups because of various patient and provider factors. In light of national policies and initiatives aimed at improving opioid prescribing practice, it is unclear whether racial/ethnic disparities have changed over time in regard to prescription pain medications; specifically, whether any potential shift in opioid prescribing has been coupled with substitution of other pain medication classes. Therefore, we examined the extent to which types of pain medications have changed over the past 15 years among racial/ethnic groups.
METHODS
We used data from the Medical Expenditure Panel Survey (MEPS) to conduct a nationally representative, serial cross-sectional study of the noninstitutionalized adult population from 2000 to 2015.6 The sampling frame for the MEPS is the civilian noninstitutionalized US population and therefore excludes adults confined to health facilities, inmates in correctional institutions, and those enlisted in the armed forces.
The MEPS inquires about the extent to which pain interferes with daily activities. From this, we identified adults (aged 18 or older) with moderate or severe self-reported pain and excluded individuals with cancer. Cancer and other medical conditions in the MEPS are self-reported. The MEPS collects outpatient prescription medication data via a combination of self-report and administrative data. We used prescription medication data to identify adults who received common pain medications including opioid and nonopioid analgesics (nonsteroidal anti-inflammatory drugs, muscle relaxants, and COX-2 inhibitors). We operationally defined a prescription opioid medication as any oral prescription with a National Drug Code classified as a “narcotic analgesic” or “narcotic analgesic combination.” To examine potential drivers of trends in prescription pain medications, we examined self-reported health status (i.e., those who reported “poor” or “fair” health compared with “excellent,” “very good,” or “good” health and health insurance coverage (as percentage uninsured) over time among each racial/ethnic group.
We used complex survey design methods to provide national estimates of the percentage of adults with noncancer pain who received prescription pain medications among 4 groups: non-Hispanic White, non-Hispanic Black, Hispanic or Latino, and other or multiple races/ethnicities. Complex survey design methods take into consideration the probability of selection, clustering of observations, and multiple stages of selection to produce national estimates.7 We used the direct rate adjustment method to adjust national trends for age and gender.
RESULTS
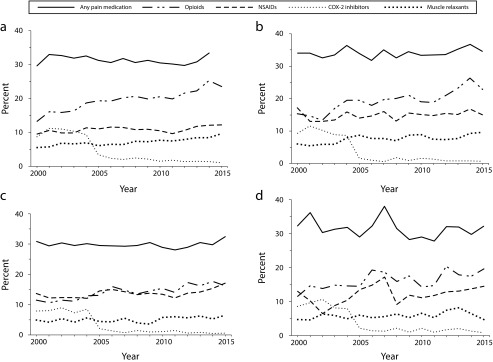
Among Americans who have pain, we found few differences in the likelihood of receiving any pain medication across racial/ethnic groups from 2000 to 2015—approximately 30% to 35% of adults who had pain received a pain medication. The age- and gender-adjusted percentage of prescription opioid use increased across all racial/ethnic groups, with the greatest increase observed among non-Hispanic White individuals (a 78% increase over the 15-year period; P < .001 for monotonic trend). By 2015, the percentage of non-Hispanic Black adults receiving opioid prescriptions approximated that of non-Hispanic White adults (P = .87)—in 2015, approximately 23% of American adults in these 2 groups used opioids (Figure 1).
FIGURE 1—
Age- and Gender-Adjusted Percentage of US Adults With Pain Who Use Prescription Pain Medications by (a) Non-Hispanic White, (b) Non-Hispanic Black, (c) Hispanic or Latino, and (d) Other: Medical Expenditure Panel Survey, United States, 2000–2015
Note. NSAIDs = nonsteroidal anti-inflammatory drugs. Direct rate adjustment method used to adjust national trends for age and gender. National estimates from 2007 used as the standard population.
Among adults with noncancer pain from 2000 to 2015, the percentage reporting poor or fair health increased among non-Hispanic White individuals from 24.4% to 34.2% and decreased from 52.4% to 40.6% among non-Hispanic Black individuals. No significant changes in health status were observed among Latino individuals. During this time period, all racial and ethnic groups experienced a decrease in the number of adults without health insurance (ranging from a decrease of 1 to 8 percentage points).
DISCUSSION
Despite national health policy efforts to improve the safety of pain management, prescription opioids have become the most commonly prescribed pain medication across all racial/ethnic groups examined. Among non-Hispanic White adults who have pain, prescription opioids are the predominant pain medication, and the use of opioids has continued to rise in recent years. We were surprised to find that opioid use among non-Hispanic Black individuals has approached that of non-Hispanic White individuals. To our knowledge, this is the first evidence of a potential narrowing of the divide in opioid prescribing by race. This shift may reflect gains in public insurance coverage since 2010—however, all racial/ethnic groups experienced similar declines in private health insurance coverage. We found some evidence of changes in health status (among adults with noncancer pain, we identified a relative decrease in the percentage of non-Hispanic Black individuals in poor or fair health, whereas poor or fair health increased among non-Hispanic White individuals). This is somewhat paradoxical when, historically, non-Hispanic White individuals have been more likely to receive opioids, and opioid-related deaths continue to occur predominantly among this group.8 Future work is needed to explain the rise in opioid use among non-Hispanic Black individuals to determine the extent to which it is related to prescribing practices in managing noncancer pain.9,10
Several limitations of this study must be acknowledged. First, MEPS data are only generalizable to noninstitutionalized Americans; trends may differ among institutionalized and noncivilian populations such as those in the armed forces. Second, although information collected from respondents is augmented with data obtained directly from health care providers, MEPS data are still fundamentally based on self-report—thus, we cannot completely rule out reporting errors in the data we analyzed. Cancer and other medical conditions are self-reported. Third, our analyses considered only outpatient prescription medication data and did not take into account inpatient prescriptions or unprescribed pain medication use. However, despite these inherent limitations, to our knowledge, this was the first nationally representative study to examine trends over time in the use of various prescription pain medications by race/ethnicity among the general pain population.
PUBLIC HEALTH IMPLICATIONS
Often in health disparities research, the focus is on examining underserved populations. However, in the context of the national epidemic of prescription opioid–related addiction and mortality, opioid-related risks do not appear commensurate with the purported benefits, especially for chronic pain. In addition to documenting the persistent reliance on opioids, our findings suggest elevated opioid use among non-Hispanic Black individuals, despite improvements in self-reported health status.
Emerging guidelines and policy efforts emphasize the use of nonopioid pain medications and nonpharmacological treatment strategies for chronic pain.11 These efforts may lead to increased disparities across racial/ethnic groups dependent on access to alternative treatments that may be more costly and resource intensive. Future policies should be mindful of these shifting disparities in the treatment of pain and focus on ensuring equitable treatment across racial/ethnic groups.
ACKNOWLEDGMENTS
This work was previously presented at the Academy Health Annual Research Meeting; June 25–27, 2017; New Orleans, LA.
HUMAN PARTICIPANT PROTECTION
Institutional review board approval was not needed for this study because it used publicly available de-identified data.
REFERENCES
- 1.Pletcher MJ, Kertesz SG, Kohn MA, Gonzales R. Trends in opioid prescribing by race/ethnicity for patients seeking care in US emergency departments. JAMA. 2008;299(1):70–78. doi: 10.1001/jama.2007.64. [DOI] [PubMed] [Google Scholar]
- 2.Ringwalt C, Roberts AW, Gugelmann H, Skinner AC. Racial disparities across provider specialties in opioid prescriptions dispensed to Medicaid beneficiaries with chronic noncancer pain. Pain Med. 2015;16(4):633–640. doi: 10.1111/pme.12555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Singhal A, Tien Y-Y, Hsia RY. Racial-ethnic disparities in opioid prescriptions at emergency department visits for conditions commonly associated with prescription drug abuse. PLoS One. 2016;11(8):e0159224. doi: 10.1371/journal.pone.0159224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Meghani SH, Byun E, Gallagher RM. Time to take stock: a meta-analysis and systematic review of analgesic treatment disparities for pain in the United States. Pain Med. 2012;13(2):150–174. doi: 10.1111/j.1526-4637.2011.01310.x. [DOI] [PubMed] [Google Scholar]
- 5.Becker WC, Starrels JL, Heo M, Li X, Weiner MG, Turner BJ. Racial differences in primary care opioid risk reduction strategies. Ann Fam Med. 2011;9(3):219–225. doi: 10.1370/afm.1242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cohen JW, Cohen SB, Banthin JS. The Medical Expenditure Panel Survey: a national information resource to support healthcare cost research and inform policy and practice. Med Care. 2009;47(7) suppl 1:S44–S50. doi: 10.1097/MLR.0b013e3181a23e3a. [DOI] [PubMed] [Google Scholar]
- 7.Saylor J, Friedmann E, Lee HJ. Navigating complex sample analysis using national survey data. Nurs Res. 2012;61(3):231–237. doi: 10.1097/NNR.0b013e3182533403. [DOI] [PubMed] [Google Scholar]
- 8.Kaiser Family Foundation. Opioid overdose deaths by race/ethnicity. 2016. Available at: https://www.kff.org/other/state-indicator/opioid-overdose-deaths-by-raceethnicity. Accessed October 31, 2017.
- 9.Boudreau D, Von Korff M, Rutter CM et al. Trends in long-term opioid therapy for chronic non-cancer pain. Pharmacoepidemiol Drug Saf. 2009;18(12):1166–1175. doi: 10.1002/pds.1833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Guy GP, Zhang K, Bohm MK et al. Vital signs: changes in opioid prescribing in the United States, 2006–2015. MMWR Morb Mortal Wkly Rep. 2017;66(26):697–704. doi: 10.15585/mmwr.mm6626a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Qaseem A, Wilt TJ, McLean RM, Forciea MA Clinical Guidelines Committee of the American College of Physicians. Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2017;166(7):514–530. doi: 10.7326/M16-2367. [DOI] [PubMed] [Google Scholar]