Abstract
Objectives. To evaluate the efficacy of an intervention targeted to commune health workers (CHWs) who deliver services to people who inject drugs (PWID) in Vietnam.
Methods. From 2014 to 2016, we conducted a cluster randomized controlled trial of 300 CHWs and 900 PWID in 60 communes in 2 provinces of Vietnam. Intervention CHWs participated in training sessions to enhance their communication skills. Trained CHWs were asked to deliver individual sessions to PWID. We assessed the outcomes at baseline and at 3-, 6-, 9-, and 12-month follow-ups.
Results. Intervention CHWs showed greater improvement in provider–client interactions than did control CHWs at all follow-ups (range of difference = 3.33–5.18; P < .001). Intervention CHWs showed greater reduction in negative attitudes toward PWID at the 12-month follow-up (mean ±SD = 1.75 ±0.50; P < .001). PWID in the intervention group exhibited greater improvement in drug avoidance than did those in the control group from the 6-month follow-up on (range of difference = 1.21–1.65; P < .001). We observed no intervention effect on heroin use as measured by urinalysis.
Conclusions. This intervention targeting CHWs could lead to desired outcomes for both CHWs and PWID.
ClinicalTrials.gov: NCT0213092.1
Drug use is the leading contributor to the HIV epidemic in Vietnam.1 There are 271 000 people who inject drugs (PWID) in Vietnam, and approximately 85% of PWID in Vietnam are heroin users.1 The prevalence of HIV among PWID is high, and two thirds of all HIV cases were infected through needle sharing related to drug use.2,3 Because heroin dependence is a chronic remitting condition, the postdetoxification relapse rate is as high as 90%.1 In response, the Vietnamese government has established and expanded harm-reduction programs, including methadone maintenance therapy and needle and syringe provision, to reduce substance abuse and its negative effects.4 Nonetheless, these programs face challenges, including a lack of infrastructure and skilled workers.5
Worldwide, community health workers play a critical role in the delivery of essential health services to underserved populations.6–10 In Vietnam, commune health centers (CHCs) are the first tier of health care at the local level.11,12 Commune health workers (CHWs) provide community PWID with routine preventive and treatment services.13 Because they have established, trusting relationships with PWID, CHWs have great potential to be mobilized to implement HIV prevention and harm-reduction programs at the commune level.13 The Vietnamese government is currently decentralizing methadone maintenance therapy, needle and syringe provision, HIV testing, and antiretroviral therapy services to CHCs.2,14 However, CHWs face significant barriers, including a lack of training in addiction and HIV-related areas and weak technical skills, such as effective counseling, to interact with PWID.4,12
Researchers in other countries have reported that providers’ negative attitudes toward PWID and their lack of skills to effectively communicate with clients may lead to suboptimal care provision and compromised outcomes.15–17 Similar issues may also exist among CHWs in Vietnam. Although interventions that directly target PWID exist in Vietnam,18 interventions that focus on the vital link between providers and the quality of care provided for PWID are lacking. Guided by Social Action Theory,19 we have implemented an intervention to strengthen the role of CHWs in service delivery for PWID in Vietnam, with the ultimate goal of influencing PWID’s behavioral outcomes. We conducted a cluster randomized controlled trial to examine the intervention’s efficacy. We hypothesized that (1) intervention CHWs would have more provider–client interactions and less negative attitudes toward PWID and (2) intervention PWID would have greater self-efficacy to avoid drug use and fewer drug-using behaviors than would control PWID.
METHODS
This cluster randomized controlled trial was conducted in the Vĩnh Phúc and Phú Thọ provinces of Vietnam, from October 2014 to October 2016. Sixty communes were selected and matched into pairs on the basis of the number of registered PWID in each commune. After baseline, the paired communes were randomized to either the intervention or the control group. We took into consideration the geographic distance between the intervention and control communes to ensure that participants in the 2 arms of the trial were isolated from each other. Intervention outcomes were evaluated at baseline and at 3-, 6-, 9-, and 12-month follow-ups.
Participants
The study participants included CHWs and PWID. A typical CHC usually has 5 CHWs who provide direct services to clients, and all were included (n = 300). The inclusion criteria for CHWs were (1) being aged 18 years or older and (2) being a doctor, assistant doctor, nurse, pharmacist, midwife, lab technician, or public health worker who had contact with PWID in the study communes (assistant doctors were those who had completed a 4-year post–high school medical training, as opposed to the 6-year training for doctors, to provide basic health services).20,21 The recruitment rate for CHWs was 100%.
To recruit PWID, we posted project flyers at CHCs, where PWID usually seek services.13 The eligibility criteria for PWID were (1) being aged 18 years or older, (2) having a history of injecting drug use, and (3) being a resident of the selected communes. Fifteen PWID were recruited from each commune (n = 900), with a recruitment rate of 95%. All participants were informed of the study’s purpose, procedures, and voluntary and confidential nature. The PWID participants, in particular, were assured that their decision to participate in the study and their responses to the assessment questions would not affect their health care services in any way. We obtained written informed consent from all participants.
Intervention Description
The intervention focused on enhancing CHWs’ communication skills in providing services to PWID. In the intervention development stage, we conducted focus groups with local community stakeholders, CHWs, and PWID to assess their needs. On the basis of the focus group findings, we organized a series of workgroup meetings for the researchers and specialists in the United States and Vietnam to develop intervention topics, format, materials, and implementation plans. The intervention was pilot tested in 2 CHCs, and feedback was collected for intervention modifications. Local health educators were recruited and trained by the investigators to deliver the intervention.
Intervention CHWs participated in 3 weekly sessions that lasted 90 minutes each. The sessions were conducted with a group of CHWs at each CHC. Session 1 focused on the important roles and responsibilities of CHWs in HIV and drug control. The challenges of working with PWID and possible solutions were identified through group discussions. Interactive games were played to reduce stigma and promote equal treatment of PWID. Session 2 introduced the stages of behavioral change and client-centered goal setting. The intervention facilitators demonstrated several motivational communication tools, such as the decisional balance sheet and motivational ruler, and communication skills. Session 3 focused on applying the knowledge and skills learned in the previous sessions to interactions with PWID. The participants role-played these tools and skills with themes related to HIV testing and treatment seeking and adherence, and the facilitators and other CHWs provided feedback for the players to fine-tune their skills. Each session ended with take-home messages and homework, and the subsequent session started with a review of the homework and problem solving. The completion rate for the intervention sessions was 100%.
After the group intervention sessions, the intervention CHWs were required to conduct three 1-hour individual sessions with PWID, using the tools and skills that they had learned. To reduce PWID’s risky behaviors, the content of the individual sessions focused on improving PWID’s physical and mental health, engaging them in harm-reduction and HIV services, and enhancing their family and social support in positive behavioral change. CHWs received detailed instructions on the individual sessions and practiced mock sessions with their peers. Booster sessions were offered once every 2 months during the follow-up period so that CHWs could share their experiences, reinforce their knowledge and skills, and problem solve. None of the CHWs missed any booster session.
Control Condition
To distinguish the effects of the intervention from those of regular contact, CHWs in the control condition received 1 group lecture provided by local health educators on topics related to drug use.
Data Collection
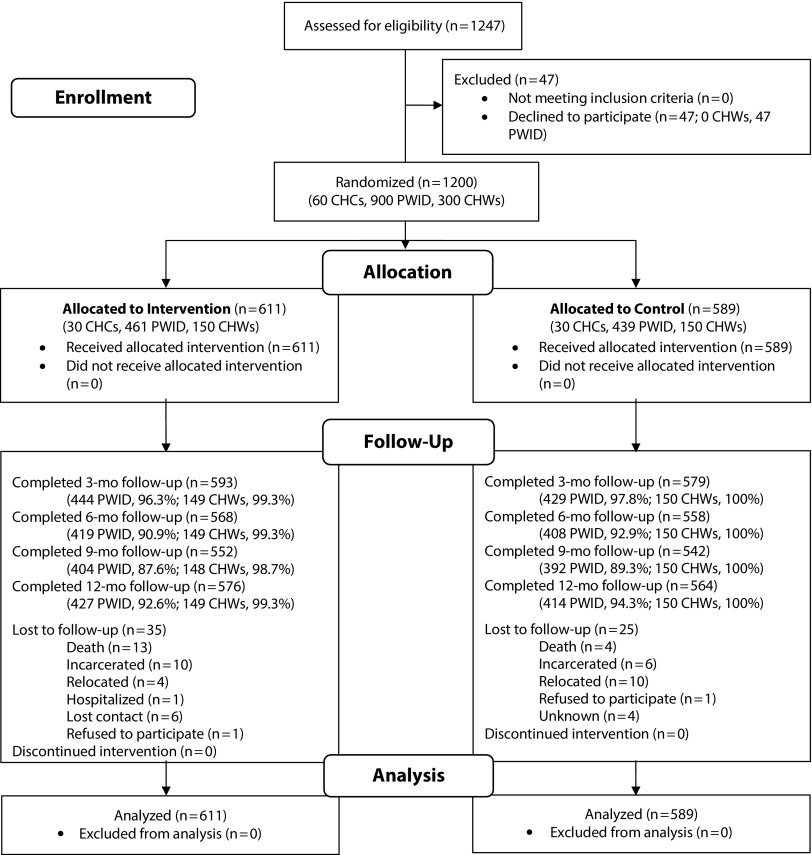
At baseline and 3-, 6-, 9-, and 12-month follow-ups, both CHWs and PWID completed the assessment in a private office at the CHC using an audio computer-assisted self-interview that was programmed to lesson nonresponses to sensitive questions.22 The participants read questions on the screen and input their answers directly into the computer. Participants whose reading level was limited could choose to listen as the questions were read from the audio system. Trained staff were available to provide instructions regarding the use of the audio computer-assisted self-interview. Each assessment took approximately 45 to 60 minutes, and no participants reported any difficulties in using the self-interview. All participants received ₫80 000 (equivalent to US $4) for each assessment. Figure 1 shows the flow of participants through the trial.
FIGURE 1—
CONSORT Flow Diagram for the Cluster Randomized Controlled Trial: Vĩnh Phúc and Phú Thọ provinces, Vietnam, October 2014–October 2016
Note. CHC = commune health centers; CHW = commune health worker; CONSORT = Consolidated Standards of Reporting Trials; PWID = people who inject drugs. Intent-to-treat analyses were performed. All participants who underwent randomization were included in the analyses.
Commune Health Worker Outcomes
Provider–client interaction was measured using a 12-item instrument, developed and pilot tested in a previous study.23 The questions on the instrument measured different ways in which the providers interacted with PWID in general, such as providing spontaneous counseling, identifying reasons for missed appointments, and feeling comfortable working with PWID. The responses were scored on a scale ranging from 1 = “not at all” to 5 = “very much.” The overall score was constructed by summing all the items, with higher scores indicating better provider–client interactions (α = .91).
Negative attitude toward drug users was measured by means of a 7-item scale, which focused on providers’ feelings of anger, disappointment, blame, and lack of concern toward drug users.24 Sample items included “To what extent do you feel disappointed towards people using drugs?” and “To what extent do you feel angry towards people using drugs?” Each question was scored on a scale ranging from 1 = “not at all” to 5 = “very much.” Scores for all items were summed, and a higher score indicated a greater level of negative attitudes toward drug users (α = .69).
We also collected information on CHWs’ demographic and career-related characteristics, including their age, gender, years of employment in the medical field, and years of service at the current CHC.
Outcomes for People Who Inject Drugs
Drug avoidance self-efficacy was measured using a 5-item scale adapted from the Drug Avoidance Self-Efficacy Scale.25 Sample questions included “Imagine that you have just blown a good job, you are home alone and depressed. Would you use drugs that are available at home?” and “Imagine that it is the Lunar New Year and you plan to do something special to celebrate. Would you use drugs?” For each question, participants rated their level of confidence (self-efficacy) that they would resist drug use in that situation on a 5-point Likert scale ranging from 1 = “certainly yes” to 5 = “certainly no.” Some items were reverse coded, and a higher overall score indicates a higher level of self-efficacy in drug avoidance (α = .94).
Current heroin use was measured by means of a urinalysis after each assessment. A participant was considered a current heroin user if he or she had a positive urine morphine test result (positive = 1, negative = 0). In addition, we collected semiannual HIV test results and linked them to our assessment data. We also collected PWID’s demographic data, including age, gender, education, marital status, annual income, and length of drug use.
Statistical Analysis
Our proposed sample sizes of 150 CHW and 450 PWID (5 CHW and 15 PWID per commune by 30 communes) per intervention condition were powered to examine intervention effects of the outcome measures. The proposed sample size for CHW provided at least 80% power at a .05 level of significance to detect a standardized effect size of 0.40, which Cohen26 considered a medium effect size. Similarly, the proposed sample size for PWID provided at least 85% power at a .05 level of significance to detect a standardized effect size of 0.35. We assumed an attrition rate of 6% for CHW and of 10% for PWID at 12-month follow-up and an a priori intraclass correlation of 0.10 for both study samples in the calculations.
Descriptive statistics and frequencies of individual-level characteristics at baseline were summarized by study group. Baseline comparisons of categorical and continuous variables were performed using the χ2 test and commune-level random effects model, respectively.
We analyzed all intervention outcomes on an intent-to-treat basis; all participants who underwent randomization were included in the analyses. For CHWs, we used mixed-effects regression models to assess the intervention effects on the outcome measures (main model). The fixed effects included preselected individual characteristics (age, gender, occupation, years worked at the CHC), group assignment (control vs intervention), visit (baseline and 3-, 6-, 9-, and 12-month follow-ups), and group by visit interaction. We included commune- and participant-level random effects to account for dependence within communes and the correlation between repeated observations for each participant. The intervention effect at each follow-up visit was defined as the difference in the changes from baseline between the intervention and control groups and was estimated through model contrasts. We graphically presented the adjusted mean scores estimated from the regressions over time by study group (Figures A and B, available as a supplement to the online version of this article). The observed intraclass correlations were 0.13 and 0.20 for CHW provider–client interactions and negative attitude, respectively. In addition, we explored whether the intervention effect on CHW outcomes varied across provider types by using 3-way models (i.e., the main models plus two 2-way interactions: intervention by provider type and visit by provider type) and a 3-way interaction term (intervention by visit by provider type).
For PWID, we used generalized linear mixed-effects regression models with identity and logit link to estimate the intervention effects on drug avoidance (continuous) and urinalysis results (binary), respectively. The fixed effects were the same as in the CHW models except for the preselected individual characteristics (age, gender, marital status, education, annual income, HIV status, PWID’s years of drug use). The intervention effect on drug avoidance self-efficacy was estimated and summarized similarly to that for the CHW outcomes. The observed intraclass correlation for drug avoidance self-efficacy was 0.33. For the binary outcome, we estimated the adjusted odds ratio (AOR) and 95% confidence interval (CI) for change from baseline to each follow-up. We also graphically illustrated the estimated reduction in odds of a positive urinalysis result (AOR and 95% CI) and the estimated improvement in drug avoidance self-efficacy (adjusted change score with 95% CI) over time by study group (Figures A and B). All statistical analyses were conducted using SAS version 9.4 (SAS Institute, Cary, NC).
RESULTS
As shown in Table 1, the intervention and control groups had an equal number of CHWs (150). Their average age was 39 years, and about 25% were men. Of the CHWs, 17% were doctors, and 39% were assistant doctors. Except for the number of years working at the current CHC (mean = 12 years), we observed no significant between-groups differences in CHW characteristics at baseline.
TABLE 1—
Sample Characteristics of Commune Health Workers and People Who Inject Drugs in Vĩnh Phúc and Phú Thọ Provinces, Vietnam, October 2014–October 2016
| Background | Control, No. (%) or Mean ±SD | Intervention, No. (%) or Mean ±SD | P |
| Community Health Worker | |||
| Total sample size | 150 | 150 | |
| Age,a y | 39.5 ±10.2 | 39.0 ±10.5 | .68 |
| Maleb | 38 (25.3) | 35 (23.3) | .69 |
| Occupationb | .35 | ||
| Doctor | 27 (18.0) | 23 (15.3) | |
| Assistant doctor | 52 (34.7) | 65 (43.3) | |
| Nurse | 31 (20.7) | 22 (14.7) | |
| Other | 40 (26.7) | 40 (26.7) | |
| Time at CHC,b y | .05 | ||
| ≤ 5 | 41 (27.3) | 56 (37.3) | |
| > 5–10 | 42 (28.0) | 28 (18.7) | |
| > 10–20 | 26 (17.3) | 35 (23.3) | |
| > 20 | 41 (27.3) | 31 (20.7) | |
| Mean ±SDa | 12.6 ±10.4 | 12.1 ±10.1 | .67 |
| People Who Inject Drugs | |||
| Total sample size | 439 | 461 | |
| Age,a y | 37.2 ±7.91 | 36.2 ±8.14 | .23 |
| Maleb | 429 (97.7) | 451 (97.8) | .91 |
| Marriedb | 337 (76.8) | 315 (68.3) | .005 |
| Education,b y | .43 | ||
| ≤ 6 | 62 (14.1) | 56 (12.2) | |
| 7–12 | 342 (78.1) | 360 (78.1) | |
| ≥ 13 | 34 (7.7) | 45 (9.8) | |
| Income (per 1000),b ₫ | .28 | ||
| < 30 000 | 98 (22.5) | 87 (18.9) | |
| 30 000 to < 50 000 | 72 (16.5) | 94 (20.4) | |
| 50 000 to < 75 000 | 152 (34.9) | 150 (32.6) | |
| ≥ 75 000 | 114 (26.2) | 129 (28.0) | |
| HIV | 66 (15.0) | 86 (18.7) | .15 |
| Drug use,b y | .06 | ||
| ≤ 5 | 92 (21.0) | 124 (26.9) | |
| > 5–10 | 151 (34.4) | 162 (35.1) | |
| > 10 | 196 (44.7) | 175 (38.0) | |
| Mean ±SDa | 10.6 ±6.11 | 10.0 ±6.36 | .48 |
Note. CHC = community health center.
Random effects model was used.
χ2 test was used. Percentages may not total 100 because of a few missing cases.
Among the 900 PWID, 461 were in the intervention group and 439 were in the control group. Most (97.8%) of the PWID were men; their average age was 37 years. Of the PWID, 73% had an annual family income of less than ₫750 000 (US $3290). Approximately 5% of the PWID came from poor households, based on the country’s standard.27 All PWID in the study were heroin users. They reported on average 10 years of drug use, and 17% were HIV-positive. Except for marital status, we found no other significant differences between the intervention and control groups in PWID’s characteristics at baseline.
Intervention Effects on Commune Health Workers
The adjusted means for provider–client interactions at baseline were comparable between groups. Doctors had a significantly better level of provider–client interaction than did assistant doctors (mean ±SD = −2.10 ±0.83; P = .018) and other types of provider (−2.98 ±0.92; P = .001; Table 2). Intervention CHWs exhibited a significant increase in provider–client interaction scores from baseline to 3-month follow-up (5.63 ±0.71; P ≤ .001), whereas the increase for control CHWs was not significant (0.46 ±0.71; P = .52; Figure A, part 1). The difference in improvement in provider–client interactions between the groups was largest at the 3-month follow-up (5.18 ±1.00; P < .001) and remained significant until the 12-month follow-up (range of difference = 3.33–4.72; P < .001; Table 2). Results from the exploratory analyses indicated that the intervention doctors had the highest increase in level of provider–client interactions compared with the control doctors (difference between intervention and control = 5.77 ±1.92; P = .003), followed by the nurses (5.44 ±2.53; P = .032) and assistant doctors (4.42 ±1.61; P = .006) at the 12-month follow-up. However, the intervention effects on the level of interaction did not significantly differ across provider types.
TABLE 2—
Adjusted Difference in Change Scores From Baseline Between Intervention and Control for Commune Health Workers: Vĩnh Phúc and Phú Thọ Provinces, Vietnam, October 2014–October 2016
| Provider–Client Interactiona |
Negative Attitudeb |
|||
| Estimate (SE) | P | Estimate (SE) | P | |
| Comparison of Interest | ||||
| Baseline | −0.731 (1.189) | .54 | −0.123 (0.639) | .85 |
| Intervention effectsc | ||||
| 3 mo | 5.175 (0.998) | < .001 | −1.213 (0.500) | .016 |
| 6 mo | 3.567 (0.999) | < .001 | −0.797 (0.501) | .11 |
| 9 mo | 3.325 (1.001) | < .001 | −0.784 (0.501) | .12 |
| 12 mo | 4.721 (0.999) | < .001 | −1.747 (0.501) | < .001 |
| Individual Characteristics | ||||
| Age | 0.034 (0.044) | .44 | −0.040 (0.019) | .035 |
| Male | 1.007 (0.743) | .18 | −0.164 (0.304) | .59 |
| Occupation (Ref = doctor) | ||||
| Assistant doctor | −2.098 (0.831) | .018 | 0.912 (0.337) | .007 |
| Nurse | −1.924 (1.018) | .06 | −0.016 (0.419) | .97 |
| Other | −2.982 (0.921) | .001 | −1.074 (0.382) | .005 |
| Time at CHC, y (Ref > 20) | ||||
| ≤ 5 | 0.846 (1.152) | .46 | −0.417 (0.473) | .38 |
| > 5–10 | −0.308 (1.127) | .79 | 0.402 (0.466) | .39 |
| > 10–20 | −0.315 (0.934) | .74 | −0.152 (0.383) | .69 |
Note. CHC = community health center.
The observed provider–client interaction score ranged from 12 to 60 (the observed change score ranged from −26 to 39).
The observed negative attitude score ranged from 7 to 33 (the observed change score ranged from −17 to 14).
The estimated difference in change scores from baseline between intervention and control (i.e., intervention − control).
The adjusted means of CHWs’ negative attitudes toward drug users were statistically comparable between the intervention and control groups at baseline (18.6 vs 18.7, respectively). CHWs in the intervention group reported a significant decline in negative attitudes at the 3-month follow-up (1.35 ±0.35; P ≤ .001), whereas those in the control group showed no significant changes from baseline (0.13 ±0.35; P = .71; Figure A, part 2). The intervention group exhibited a significantly greater reduction in negative attitudes at the 3-month follow-up (1.21 ±0.50; P = .016), which increased slightly at the 6- and 9-month follow-ups, and decreased again at the 12-month follow-up (1.75 ±0.50; P < .001; Table 2). Exploratory analysis indicated that the intervention assistant doctors showed a significant decrease in negative attitude compared with the control assistant doctors (difference between intervention and control = −2.49 ±0.81; P = .002), but we found no significant differences in change of negative attitude between the study groups for the other 3 types of providers.
Intervention Effects on People Who Inject Drugs
At baseline, the adjusted mean scores for drug avoidance self-efficacy for PWID were not significantly different between groups (Table 3). The following characteristics were significantly associated with a higher level of drug avoidance: older age (0.04 ±0.01; P < .001), female gender (1.14 ±0.55; P = .037), and use of drugs over 10 years compared with 5 years or less (0.53 ±0.26; P = .036). At 6-month follow-up, the intervention PWID exhibited greater improvement in drug avoidance self-efficacy than did the control group (1.21 ±0.34; P < .001; Table 3). The intervention group improved more rapidly than the control group at both 9- and 12-month follow-ups (3.17 vs 1.51 and 2.97 vs 1.59, respectively; Figure B, part 1). In summary, the intervention group showed significantly greater improvement in drug avoidance self-efficacy than did the control group from 6-month follow-up on (all P < .001; Table 3).
TABLE 3—
Adjusted Difference in Change Scores of Drug Avoidance Self-Efficacy From Baseline Between Intervention and Control Groups for People Who Inject Drugs: Vĩnh Phúc and Phú Thọ Provinces, Vietnam, October 2014–October 2016
| Drug Avoidance Self-Efficacya |
||
| Estimate (SE) | P | |
| Comparison of Interest | ||
| Baseline | −0.525 (0.829) | .53 |
| Intervention effectsb | ||
| 3 mo | 0.358 (0.335) | .29 |
| 6 mo | 1.210 (0.341) | < .001 |
| 9 mo | 1.653 (0.345) | < .001 |
| 12 mo | 1.380 (0.341) | < .001 |
| Individual Characteristics | ||
| Age | 0.043 (0.012) | < .001 |
| Male | −1.138 (0.546) | .037 |
| Married | 0.274 (0.184) | .14 |
| Education (Ref ≥ 13) | ||
| ≤ 6 | 0.676 (0.349) | .053 |
| 7–12 | 0.133 (0.274) | .63 |
| Income (Ref = 75 000 000 +) | ||
| < 30 000 000 | 0.329 (0.281) | .24 |
| 30 000 000 to < 50 000 000 | −0.381 (0.277) | .17 |
| 50 000 000 to < 75 000 000 | −0.354 (0.232) | .13 |
| HIV | −0.423 (0.243) | .08 |
| Drug use (Ref > 10) | ||
| ≤ 5 | −0.534 (0.255) | .036 |
| > 5–10 | −0.063 (0.208) | .76 |
The observed score ranged from 5 to 25 (the observed change score ranged from −20 to 20).
Estimated difference in change scores from baseline between intervention and control (i.e., intervention—control).
Figure B, part 2, shows the adjusted reduction (with 95% CI) in odds of a positive urinalysis result at baseline compared with each follow-up by study group (data not shown). At baseline, 33% of the control PWID versus 28% of intervention PWID had positive urinalysis results, and they both showed a reduction of approximately 10% at the 12-month follow-up (23% vs 18%, respectively). However, none of the group differences at the follow-ups were statistically significant.
DISCUSSION
Traditional programs often segregate intervention efforts by targeting either service providers for skills training or at-risk populations for prevention.18,28,29 This intervention trial focused on CHWs as a crucial link in providing services to PWID. Our findings suggest that both CHWs and PWID could benefit from an intervention that addresses CHWs’ challenges in caring for PWID. This intervention strategy has implications for health care system enhancement and service provider training in Vietnam.
The improvements in provider outcomes resulting from this intervention may inform current service decentralization efforts in Vietnam.30–32 To deliver HIV and harm-reduction services at the community level, the vital first step is to eliminate CHWs’ negative attitudes and to equip them with the necessary skills to reach, motivate, and engage community PWID. This intervention showed promising outcomes in this direction. During informal interviews with the study investigators, CHWs in the study indicated that the communication skills and tools taught in this intervention were well accepted because of their simplicity and relevance to practice. The interactive intervention activities prepared CHWs to apply these tools and skills in routine service provision for PWID. The intervention may be a useful addition to the current in-service training for CHWs.
After the intervention, PWID reported significantly increased self-efficacy in drug avoidance. This finding is encouraging, because previous studies have shown that high levels of self-efficacy are associated with better drug use outcomes.33,34 In the context of this study, we anticipate that the PWID’s improved drug avoidance self-efficacy may stem from the individual sessions delivered by trained CHWs. Yet, this intervention effect on PWID was not reflected in the heroin use outcomes measured by urinalysis, which could be interpreted in several ways. First, in this study, participants in both conditions completed urinalysis and drug-related assessments once every 3 months. The repeated assessments and urinalyses themselves could possibly have influenced the target behaviors (i.e., drug use) in this study. Second, a change in self-efficacy was necessary but not sufficient to change addictive behaviors,35 and drug use behavior could have been influenced by other factors. In addition, it may not be realistic to expect that our training, which directly targeted CHWs, would translate into desired PWID outcomes in a limited period. Nevertheless, we believe that reduced stigmatizing attitudes and enhanced communication skills in CHWs are the prerequisites for community-based health care delivery for PWID.
Limitations
The study has several limitations. First, the study results may not be generalizable to PWID living outside of the study areas, those not visiting CHCs, or those who refused to participate in the study. Second, our self-report measures could suffer from social desirability and recall biases. Specifically, CHWs may limit full disclosure of negative attitudes toward PWID, and their interactions with PWID were not verified by medical record. Objective measures of CHWs’ change in knowledge or skills to serve PWID were lacking. Drug avoidance self-efficacy was measured on the basis of hypothetical situations, and PWID may have falsely reported their ability to avoid drugs in real-life situations. Third, drug use status was based on urine morphine tests, which did not include detection of other drugs such as amphetamine-type stimulants. Fourth, although the difference in CHWs’ attitudinal changes between groups reached statistical significance, it may not practically reflect the enhancement of CHWs’ capacity to deliver services. Last, the change in outcome measures could be confounded by factors that were not measured in this study.
Conclusions
This study highlights the positive outcomes of a provider-targeted intervention on both CHWs and PWID. Given that drug use is the primary driving force of the HIV epidemic in Vietnam, the strengthened community health care workforce can also play a role in HIV prevention and care. The lessons learned from this study can inform efforts to enhance community capacity building in other resource-limited countries to deliver harm-reduction and HIV-related services to drug-using populations.
ACKNOWLEDGMENTS
This work was supported by the National Institutes of Health (grants R01DA033609 and P30MH058107).
The authors gratefully acknowledge the project team members in Vietnam for their contributions to this study.
HUMAN PARTICIPANT PROTECTION
This research was approved by the institutional review boards of the University of California, Los Angeles, and the National Institute of Hygiene and Epidemiology, Hanoi, Vietnam.
REFERENCES
- 1.Harm Reduction International. Community-based drug treatment models for people who use drugs: six experiences on creating alternatives to compulsory detention centres in Asia. Available at: https://www.hri.global/files/2015/10/19/Community_based_drug_treatment_models_for_people_who_use_drugs.pdf. Accessed December 17, 2017.
- 2.UNAIDS. Optimizing Viet Nam’s HIV response: an investment case. Available at: http://unaids.org.vn/en/optimizing-viet-nams-hiv-response-investment-case. Accessed October 30, 2017.
- 3.Vietnam Ministry of Labor, Invalids, and Social Affairs. Overview of the Impact of Policies on Drug Rehabilitation Treatment on Its Implementation in Vietnam. Hanoi, Vietnam: Vietnam Ministry of Labor, Invalids, and Social Affairs; 2010. [Google Scholar]
- 4.Global Fund. TB and HIV concept note: investing for impact against tuberculosis and HIV. Available at: http://www.unaids.org/sites/default/files/country/documents/VNM_narrative_report_2015.pdf. Accessed October 17, 2017.
- 5.Vuong T, Nguyen N, Le G, Shanahan M, Ali R, Ritter A. The political and scientific challenges in evaluating compulsory drug treatment centers in Southeast Asia. Harm Reduct J. 2017;14(1):2. doi: 10.1186/s12954-016-0130-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Haines A, Sanders D, Lehmann U et al. Achieving child survival goals: potential contribution of community health workers. Lancet. 2007;369(9579):2121–2131. doi: 10.1016/S0140-6736(07)60325-0. [DOI] [PubMed] [Google Scholar]
- 7.Singh P, Sachs JD. 1 million community health workers in sub-Saharan Africa by 2015. Lancet. 2013;382(9889):363–365. doi: 10.1016/S0140-6736(12)62002-9. [DOI] [PubMed] [Google Scholar]
- 8.Global Health Alliance, World Health Organization. Global Experience of Community Health Workers for Delivery of Health Related Millennium Development Goals: A Systematic Review, Country Case Studies, and Recommendations for Integration Into National Health Systems. Geneva, Switzerland: World Health Organization; 2010. [Google Scholar]
- 9.Nguyen HT, Tran AV, Nguyen NB et al. Community mobilization to reduce drug use, Quang Ninh, Vietnam. Am J Public Health. 2015;105(1):189–195. doi: 10.2105/AJPH.2014.302101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Scott VK, Gottschalk LB, Wright KQ et al. Community health workers’ provision of family planning services in low-and-middle-income countries: a systematic review of effectiveness. Stud Fam Plann. 2015;46(3):241–261. doi: 10.1111/j.1728-4465.2015.00028.x. [DOI] [PubMed] [Google Scholar]
- 11.Shelley D, Tseng TY, Pham H et al. Factors influencing tobacco use treatment patterns among Vietnamese health care providers working in community health centers. BMC Public Health. 2014;14(1):68. doi: 10.1186/1471-2458-14-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shelley D, Nguyen L, Pham H, VanDevanter N, Nguyen N. Barriers and facilitators to expanding the role of community health workers to include smoking cessation services in Vietnam: a qualitative analysis. BMC Health Serv Res. 2014;14(1):606. doi: 10.1186/s12913-014-0606-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.World Health Organization. Good Practice in Asia: Targeted HIV Prevention for IDU and Sex Workers, Viet Nam’s First Large-Scale National Harm Reduction Initiative. Geneva, Switzerland: World Health Organization; 2010. [Google Scholar]
- 14.Duong BD. Adapting Treatment 2.0 in Viet Nam—toward universal and sustainable access. Available at: http://www.who.int/hiv/events/duong_treatment2.0.pdf. Accessed December 30, 2017.
- 15.Marsh JC, Angell B, Andrews CM, Curry A. Client-provider relationship and treatment outcome: a systematic review of substance abuse, child welfare, and mental health services research. J Soc Social Work Res. 2012;3(4):233–267. [Google Scholar]
- 16.Lang K, Neil J, Wright J, Dell CA, Berenbaum S, El-Aneed A. Qualitative investigation of barriers to accessing care by people who inject drugs in Saskatoon, Canada: perspectives of service providers. Subst Abuse Treat Prev Policy. 2013;8(1):35. doi: 10.1186/1747-597X-8-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.van Boekel LC, Brouwers EP, van Weeghel J, Garretsen HF. Stigma among health professionals towards patients with substance use disorders and its consequences for healthcare delivery: systematic review. Drug Alcohol Depend. 2013;131(1–2):23–35. doi: 10.1016/j.drugalcdep.2013.02.018. [DOI] [PubMed] [Google Scholar]
- 18.Go VF, Frangakis C, Le Minh N et al. Effects of an HIV peer prevention intervention on sexual and injecting risk behaviors among injecting drug users and their risk partners in Thai Nguyen, Vietnam: a randomized controlled trial. Soc Sci Med. 2013;96:154–164. doi: 10.1016/j.socscimed.2013.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ewart CK. Social action theory for a public health psychology. Am Psychol. 1991;46(9):931–946. doi: 10.1037//0003-066x.46.9.931. [DOI] [PubMed] [Google Scholar]
- 20.Do K, Minichiello V, Hussain R, Khan A. Sexual history taking in general practice: managing sexually transmitted infections for female sex workers by doctors and assistant doctors in Vietnam. Int J STD AIDS. 2015;26(1):55–64. doi: 10.1177/0956462414529553. [DOI] [PubMed] [Google Scholar]
- 21.Fan AP, Tran DT, Kosik RO, Mandell GA, Hsu HS, Chen YS. Medical education in Vietnam. Med Teach. 2012;34(2):103–107. doi: 10.3109/0142159X.2011.613499. [DOI] [PubMed] [Google Scholar]
- 22.Des Jarlais DC, Paone D, Milliken J et al. Audio-computer interviewing to measure risk behaviour for HIV among injecting drug users: a quasi-randomised trial. Lancet. 1999;353(9165):1657–1661. doi: 10.1016/s0140-6736(98)07026-3. [DOI] [PubMed] [Google Scholar]
- 23.Li L, Wu Z, Liang LJ et al. An intervention targeting service providers and clients for methadone maintenance treatment in China: a cluster-randomized trial. Addiction. 2013;108(2):356–366. doi: 10.1111/j.1360-0443.2012.04020.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.National Center for Education and Training on Addiction. Health Professionals’ Attitudes Towards Licit and Illicit Drug Users: A Training Resource. Adelaide, South Australia, Australia: National Center for Education and Training on Addiction; 2006. [Google Scholar]
- 25.Martin GW, Wilkinson DA, Poulos CX. The Drug Avoidance Self-Efficacy Scale. J Subst Abuse. 1995;7(2):151–163. doi: 10.1016/0899-3289(95)90001-2. [DOI] [PubMed] [Google Scholar]
- 26.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum; 1988. [Google Scholar]
- 27.Government Portal of Vietnam. Decision No. 9/2011/QD-TTG of the Prime Minister promulgating standards of poor households, near poor households for 2011–2015 period. Available at: http://vanban.chinhphu.vn/portal/page/portal/chinhphu/hethongvanban?class_id=1&_page=37&mode=detail&document_id=98923. Accessed December 30, 2017.
- 28.Gates LB, Mandiberg JM, Akabas SH. Building capacity in social service agencies to employ peer providers. Psychiatr Rehabil J. 2010;34(2):145–152. doi: 10.2975/34.2.2010.145.152. [DOI] [PubMed] [Google Scholar]
- 29.Go VF, Frangakis C, Minh NL et al. Efficacy of a multi-level intervention to reduce injecting and sexual risk behaviors among HIV-infected people who inject drugs in Vietnam: a four-arm randomized controlled trial. PLoS One. 2015;10(5):e0125909. doi: 10.1371/journal.pone.0125909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ramesh M. Health care reform in Vietnam: chasing shadows. J Contemp Asia. 2013;43(3):399–412. [Google Scholar]
- 31.Thien LQ. Hanoi struggles to attract new methadone treatment patients. Vietnam Times. August 4, 2015. Available at: http://vietnamfriendship.vn/Hanoi-struggles-to-attract-new-methadone-treatment-patients-07-8049.html. Accessed December 17, 2017.
- 32.Joint United Nations Programme on HIV/AIDS. Decentralization of HIV testing services to increase access for people who inject drugs in Vietnam. Available at: http://www.unaids.org/en/resources/presscentre/featurestories/2016/october/20161012_vietnam. Accessed October 17, 2017.
- 33.Kadden RM, Litt MD. The role of self-efficacy in the treatment of substance use disorders. Addict Behav. 2011;36(12):1120–1126. doi: 10.1016/j.addbeh.2011.07.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kuerbis A, Armeli S, Muench F, Morgenstern J. Motivation and self-efficacy in the context of moderated drinking: global self-report and ecological momentary assessment. Psychol Addict Behav. 2013;27(4):934–943. doi: 10.1037/a0031194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hyde J, Hankins M, Deale A, Marteau TM. Interventions to increase self-efficacy in the context of addiction behaviours: a systematic literature review. J Health Psychol. 2008;13(5):607–623. doi: 10.1177/1359105308090933. [DOI] [PubMed] [Google Scholar]