Abstract
Objectives. To examine the mechanisms of the association between age of sexual initiation and adult health.
Methods. Data from the Seattle Social Development Project (n = 808), in Seattle, Washington, included outcomes when participants were in their 30s (2005–2014): substance use disorders, depression, poor health, and obesity. Sexual consequence mediators included sexually transmitted infection, adolescent pregnancy, and a high number of sexual partners. We used linear logistic regression to model main effect and mediated associations.
Results. Age of sexual initiation was related to nicotine and marijuana disorders, physical health, and obesity, but not alcohol disorder or depression. Mediated association with nicotine disorder was not significant; association with marijuana disorder was reduced; significant relationships with poor health and obesity remained.
Conclusions. The relationship between age of sexual initiation and substance use was largely explained by consequences of sexual behavior. Earlier sexual initiation was linked to poorer physical health outcomes, though the nature of the association remains unclear.
Public Health Implications. Prevention approaches need to address multiple risk factors and emphasize contraceptive methods to avoid sexual consequences. For physical health outcomes, broad prevention approaches, including addressing early sexual initiation, may be effective.
On average, adolescents in the United States initiate sexual intercourse in their 17th year, and more than 75% of adolescents report having had sex by age 20 years.1 Yet, despite sexual behavior being normative among adolescents, public health literature often treats adolescent sexuality as generally risky, and it is typically categorized with other adverse behaviors such as delinquency and the use of addictive substances.2 However, recent perspectives have challenged this and have called for more rigorous quantitative research on the relationship between adolescent sexuality and health outcomes.3 Although previous investigations have linked early sexual initiation to negative health outcomes (for a review, see Zimmer-Gembeck and Helfand4), relatively few studies have examined the impact of later adolescent initiation or tested potential mediators and confounders of this association. In particular, few studies have examined the degree to which sexual consequences, which may follow adolescent sexual initiation, explain the relationship between age of sex and health.
In addition, there is limited understanding about whether reported negative health effects following adolescent sexual initiation are lasting and persist into adulthood. Finally, the degree to which the link between adolescent sex and later health outcomes may be attributable to common underlying risk factors, such as an earlier measure of the outcome variable, has not been consistently explored. Thus, it is unclear whether sexual initiation is still directly related to negative health outcomes when sexual initiation occurs beyond the early adolescent years, and when important controls and sexual consequences, such as early pregnancy or sexually transmitted infection (STI), are accounted for. Moreover, it is unclear if manifested short-term negative outcomes persist later into adulthood.
EARLY VS LATE INITIATION
Early sexual initiation, variably defined in the literature as occurring when one is aged younger than 15 years to younger than 17 years, has been widely linked to a number of adverse outcomes, including consequences directly related to sexual activity (e.g., STI)5,6 and other health-related outcomes (e.g., depression).7,8 Some studies have found that effects are stronger for girls than boys.4,9–11 Considered from a life course development perspective, the effects of timing of initiation may be explained by how normative or nonnormative the timing is. Indeed, some studies have found that those who initiate “on time”—approximately between ages 16 and 18 years—report higher sexual satisfaction and better mental health, well-being, and social–romantic development compared with those who initiate earlier or later (i.e., after age 18 years).4,7,12–14 Other studies have found that later initiation is a protective factor.4,6 However, most studies of outcomes of adolescent sexual initiation measure outcomes concurrently or just a few years after adolescence; longer-term consequences are rarely examined. Some also report only slight increases in distress that do not meet clinical levels.11 Thus, it is unclear if negative effects are temporary and fleeting or if they pose danger to adolescents’ health by triggering distress that persists into adulthood.
Previous examinations of early sexual initiation used a cutoff for “early” initiation that was either relatively arbitrary or tied to the age at which data were collected,8 based on national averages in age of initiation,15 or based on the distribution of age of initiation in the sample.11,16 The combination of these practices has contributed to inconsistencies in the effects of early versus on-time initiation. For example, studies labeling on-time sexual initiation as “early” because of sample makeup or study design may not find initiation associated with negative outcomes. A recent work by Vasilenko et al.,7 the first to model the relationship between age of initiation and outcomes, showed that the associations between age of sex and STI and depression were curvilinear and that, especially for males, only very early initiation (before age 14 years) was associated with increased risk. At later ages, the relationship was not consistent, suggesting that closer attention to the full range in age of initiation in its relationship to outcomes is needed.
MEDIATORS AND HEALTH OUTCOMES OF AGE OF INITIATION
The literature linking adolescent sexual activity and later health outcomes provides sparse consideration of mediators and confounders affecting this relationship. Much of the research is done with cross-sectional studies4 and studies that often lack sufficient controls. Several longitudinal studies highlight the importance of considering how previous levels of the outcome are confounders in the relationship between early sex and health. For example, 2 studies showed that depression among sexually active adolescents was explained by depression before sexual initiation.9,17 Furthermore, a number of propensity-matched and genetically informed studies concluded that third-variable confounders, such as shared genetic or environmental factors, account for the association between sexual initiation and substance use, mental health, and criminal behavior.11,14,16,18,19 These studies point to the need to include previous levels of the outcome in testing the association between age of sexual initiation and later health as possible confounders.
In addition to testing for confounders, it is important to examine the mechanisms or mediators by which sexual initiation leads to poorer health. A number of studies have done this, with a variety of mediators, including those related to sexual activity (e.g., STI20) and those that are more social developmental in nature (e.g., antisocial peers5). For example, Epstein et al.15 showed that impulsivity and antisocial peers explained the association between early sexual initiation and sexual health in one’s 20s and 30s. Early sexual initiation is related to a variety of adolescent behaviors, such as early substance use and depression, all of which are multiply determined. The choice of mediators thus also spans multiple domains. What is missing from the literature is a systematic analysis of which factors carry the most mediating power in the relationship between early sex and health. Sexual initiation is a prerequisite to early pregnancy and STI, and earlier sexual initiation carries a greater risk of adolescent pregnancy, multiple sexual partners, and STI.18,21 Thus, the first step in this work is to investigate the degree to which sexual consequences, the most proximal and causally determined by early sex, are not in fact the primary mechanisms connecting early sex to later problems.
Only a few studies have addressed sexual consequences as mediators, and results have been mixed, possibly because many used a mix of sexual and social developmental mediators in their analyses. For example, Epstein et al.5 showed that unsafe sexual practices (e.g., sex under the influence of alcohol or drugs, multiple sexual partners) mediated the relationship between early sexual initiation and STI alongside school bonding and early alcohol use.5 We are aware of 2 studies that have examined only sexual consequences as mediators. Both found that the link between age of initiation and poorer outcomes persisted after controlling for lifetime number of partners and adolescent pregnancy,8,20 although each study examined only a single sexual consequence (STI and adolescent pregnancy, respectively), pointing to the need for more research.
Effective programs to promote correct and consistent use of contraception already exist and greatly reduce the likelihood that adolescents experience sexual consequences following sexual initiation.22 Thus, to the extent that associations between adolescent sexual initiation and health are mediated through more proximal sexual consequences, more focused sexual education programs that promote and facilitate correct and consistent contraceptive use are likely to make a significant difference without needing to intervene on a broader level. If, however, addressing sexual consequences alone is insufficient, more comprehensive programs aimed at a broad range of risk factors and sexual risk-taking behavior will be needed to help reduce the prevalence of negative health outcomes.
CURRENT STUDY
The current study builds on existing research on the relationship between timing of sexual initiation and health consequences for adults aged in their 30s in 4 important ways. First, we examined a broad set of outcomes, including indicators of physical health that, although not directly related to sexual initiation, are correlated with substance use and mental health in adulthood. Second, we considered the full range of age of sexual initiation and tested both linear and nonlinear relationships to outcomes. Third, using longitudinal data, we controlled for previous levels of the outcome, as well as known confounders such as demographics, pubertal age,23 experiences of childhood sexual abuse,24 and individual differences in internalizing and externalizing behavior.15 Fourth, we tested the degree to which sexual consequences mediate the relationship between age of sexual initiation and outcomes. Our analyses were driven by the following research questions:
Does timing of adolescent sexual activity have long-term effects on substance use, mental health, and physical health for men and women, after accounting for known confounders?
Does accounting for sexual consequences (adolescent pregnancy, STI, and high number of sexual partners) mediate those relationships?
METHODS
We drew data from the Seattle Social Development Project (SSDP), a prospective longitudinal study of prosocial and antisocial behavior in Seattle, Washington.25 Beginning in 1985, SSDP drew 808 fifth graders (77% of eligible students) from 18 Seattle public schools that overrepresented high-crime neighborhoods. Participants have been interviewed 15 times from age 10 (1985) to age 39 (2014) years. The sample is gender balanced (396 females, 412 males). Of the participants, 47% identified as White, 26% as Black, 22% as Asian American, and 5% as Native American. When the study began, the sample was overly representative of low-income families; 46% of families reported annual incomes less than $20 000, and 52% of participants qualified for the National School Lunch/School Breakfast Program. Retention has remained greater than 87% every year since 1989.
Part of the sample was exposed to a preventive intervention in the elementary grades.25 Previous analyses of sexual behavior in this sample showed few differences in the covariance structures of the intervention and control groups5; thus, we based the current analyses on the full sample, with control for intervention status.
Measures
Adult health outcomes.
Health outcomes were measured at ages 30, 33, and 39 years. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV)26 diagnoses for alcohol or marijuana abuse or dependence, nicotine dependence, and major depressive disorder were based on the Diagnostic Interview Schedule27 at each time point. If respondents met diagnostic criteria in any of the 3 assessments, disorder was coded as 1 (0 otherwise). Participants were asked “How would you describe your general health?” Response options of “fair” and “poor” were coded as 1, and “excellent” and “good” were coded as 0 for a measure of poor health. Interviewer-measured height and weight were used to calculate body mass index at each time point; the maximum value was used in analyses to calculate whether participants met criteria for being obese (defined as a body mass index of ≥ 30 kg/m2.).
Age of sexual initiation was self-reported prospectively starting at age 14 years. Participants were asked “Have you ever had sex with a boy [girl]?” and “How old were you the first time you had sex?” at ages 14 to 16 years. Starting at age 18 years, the question was reworded to “Have you had sex with another person?” Behaviors constituting “sex” were not defined. At age 24 years, participants were asked retrospectively how old they were the first time they had sex, whether first sex was consensual, and age at first consensual sex. Because discrepancies in reports of sexual initiation are common in longitudinal studies and do not consistently correspond to either prospective or retrospective reports,28 we used an average of all existing reports to determine age of initiation. We used age of first consensual sex if it was later than the average calculated from all other reports. Sexual initiation before age 12 years was coded as missing because of concerns that very early sex may not have been consensual.
Young adult mediators included early (adolescent) pregnancy, STI acquisition, and high number of sexual partners. Adolescent pregnancy was coded as 1 if respondents reported pregnancy by age 18 years (0 otherwise). Female participants reported whether they had ever been pregnant, and male participants reported whether they had ever gotten a woman pregnant. Lifetime STI acquisition was self-reported at age 21 years. Number of male and female lifetime sexual partners was assessed at age 24 years and was coded as having 10 or more partners (1) versus fewer (0). Sensitivity analyses showed that 10 or more partners (72nd percentile) gave the most reliable estimates across the 6 outcomes, compared with 3 or more and 5 or more, or 15 or more partners. We intended this to measure outliers in sexual behavior that may signal other risk-taking tendencies.
Control variables.
All analyses included race, gender, eligibility for the National School Lunch/School Breakfast Program in grades 5 through 7 (childhood socioeconomic status), and intervention status. Additional childhood covariates included self-reported pubertal age (reported retrospectively at ages 18 and 24 years); sexual abuse before age 10 years (reported retrospectively at age 24); alcohol or tobacco use at ages 10 through 12 years; and teacher-reported externalizing and internalizing behavior29 as well as teacher-reported “child overweight” from the Child Behavior Checklist30—both measured at ages 10 through 12 years.
Analyses
Analyses in the current study followed the 4-step approach outlined by Baron and Kenny31 and MacKinnon et al.32 The first step tested the associations between predictor (early sex) and outcomes. Next, we established associations between predictor and mediator (step 2) and between mediator and outcome (step 3). Step 4 was to test the association between predictor and outcome, accounting for the mediators. Because steps 2 and 3 have been well established in the literature, the primary focus of the current analysis was on steps 1 and 4. Table 1 shows variable descriptors and Tables 2 and 3 show multivariate regressions with each of the 6 outcomes before and after we added mediators. We tested associations in steps 2 and 3 and found them to be significant, through bivariate correlations (Table A, available as a supplement to the online version of this article at http://www.ajph.org).
TABLE 1—
Analysis Variables by Outcome: Seattle Social Development Project; Seattle, WA; 2005–2014
| Variable | All (n = 731), Mean (SD) or % | Alcohol Disordera (n = 199), Mean (SD) or % | Nicotine Disordera (n = 173), Mean (SD) or % | Marijuana Disordera (n = 96), Mean (SD) or % | Depressiona (n = 160), Mean (SD) or % | Poor Healthb (n = 319), Mean (SD) or % | Obesityc (n = 332), Mean (SD) or % |
| Main effect: age of initiation, y | 15.72 (2.39) | 15.24 (2.06) | 14.79 (2.03) | 14.40 (1.99) | 15.35 (2.27) | 15.23 (0.66) | 15.22 (2.19) |
| Mediators | |||||||
| STI | 17.6 | 18.2 | 22.9 | 26.1 | 25.0 | 18.0 | 20.1 |
| Adolescent pregnancy | 24.3 | 23.6 | 35.0 | 40.2 | 33.7 | 29.6 | 29.8 |
| High number of sexual partners | 28.5 | 48.6 | 40.3 | 59.5 | 33.8 | 31.7 | 28.5 |
| Controls | |||||||
| Early substance used | 0.22 (0.51) | 0.27 (0.60) | 0.35 (0.71) | 0.34 (0.75) | 0.24 (0.46) | 0.26 (0.59) | 0.26 (0.59) |
| Early internalizingd | 0.09 (0.13) | 0.10 (0.15) | 0.13 (0.15) | 0.10 (0.12) | 0.11 (0.14) | 0.09 (0.11) | 0.09 (0.11) |
| Early overweightd | 0.16 (0.42) | 0.15 (0.42) | 0.21 (0.46) | 0.22 (0.49) | 0.23 (0.50) | 0.22 (0.50) | 0.22 (0.50) |
| Externalizingd | 0.23 (0.34) | 0.28 (0.36) | 0.36 (0.43) | 0.35 (0.43) | 0.24 (0.33) | 0.26 (0.35) | 0.26 (0.35) |
| Black | 25.6 | 26.1 | 28.9 | 40.6 | 33.8 | 29.8 | 33.7 |
| Asian American | 21.9 | 12.6 | 13.3 | 6.3 | 9.4 | 20.1 | 14.5 |
| Native American | 5.3 | 6.0 | 8.1 | 3.1 | 8.8 | 6.9 | 5.4 |
| Male | 51.0 | 63.8 | 59.0 | 68.8 | 35.6 | 48.0 | 46.4 |
| Low childhood SES | 52.4 | 44.2 | 57.8 | 51.0 | 56.9 | 58.6 | 56.9 |
| Pubertal age, y | 12.49 (1.63) | 12.41 (1.59) | 12.07 (1.86) | 12.18 (1.78) | 12.08 (1.72) | 12.27 (1.66) | 12.27 (1.66) |
| Sexual abuse | 10.6 | 12.8 | 17.7 | 16.1 | 24.0 | 13.3 | 13.5 |
Note. SES = socioeconomic status; STI = sexually transmitted infection.
Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV)26 diagnoses for alcohol or marijuana abuse or dependence, nicotine dependence, and major depressive disorder were based on the Diagnostic Interview Schedule27 at each time point (at ages 30, 33, and 39 years). If respondents met diagnostic criteria in any of the 3 assessments, disorder was coded as 1 (0 otherwise).
Participants were asked “How would you describe your general health?” Response options of “fair” and “poor” were coded as 1, and “excellent” and “good” were coded as 0 for a measure of poor health.
Interviewer-measured height and weight were used to calculate body mass index at each time point; the maximum value was used in analyses to calculate whether participants met criteria for being obese. Obesity was defined as a body mass index of ≥ 30 kg/m2.
Average frequency of use of nicotine, alcohol, and marijuana in grades 5, 6, and 7 (1 = never; 2 = once or twice; 3 = 3 or 4 times; 4 = more than 4 times in the past month).
TABLE 2—
Association Between Age of Sexual Initiation and Adult Substance Use for Main Effects and Mediated Through Sexual Consequences: Seattle Social Development Project; Seattle, WA; 2005–2014
| Variable | Alcohol Disorder,a OR (95% CI) | Nicotine Disorder,a
OR (95% CI) |
Marijuana Disorder,a OR (95% CI | |||
| Unmediated | Mediated | Unmediated | Mediated | Unmediated | Mediated | |
| Main effect: age of initiation | 0.92 (0.85, 1.00) | 0.96 (0.88, 1.06) | 0.88 (0.79, 0.97) | 0.90 (0.81, 1.00) | 0.77 (0.66, 0.90) | 0.83 (0.70, 0.99) |
| Mediators | ||||||
| STI | . . . | 0.96 (0.56, 1.71) | . . . | 0.84 (0.48, 1.50) | . . . | 1.16 (0.61, 2.22) |
| Adolescent pregnancy | . . . | 0.82 (0.50, 1.35) | . . . | 1.43 (0.87, 2.36) | . . . | 1.76 (0.93, 3.33) |
| High number of sexual partners | . . . | 2.24 (1.46, 3.56) | . . . | 1.20 (0.75, 1.94) | . . . | 2.14 (1.18, 3.91) |
| Gender interactions: gender × pubertal age | NS | NS | 1.31 (1.00, 1.72) | 1.33 (1.06, 1.75) | NS | NS |
| Controls | ||||||
| Outcome at ages 10–12 y | 1.07 (0.74, 1.55) | 1.07 (0.71, 1.65) | 1.06 (0.71, 1.57) | 1.04 (0.71, 1.52) | 1.13 (0.73, 1.75) | 1.05 (0.66, 1.69) |
| Externalizing | 1.30 (0.70, 2.43) | 1.29 (0.68, 2.45) | 3.16 (1.65, 6.03) | 3.24 (1.68, 6.39) | 1.23 (0.59, 2.59) | 1.11 (0.51, 2.43) |
| Black | 0.84 (0.52, 1.37) | 0.89 (0.53, 1.56) | 0.78 (0.46, 1.33) | 0.75 (0.43, 1.30) | 1.53 (0.87, 2.71) | 1.40 (0.80, 2.45) |
| Asian American | 0.59 (0.34, 1.02) | 0.65 (0.37, 1.16) | 0.70 (0.38, 1.30) | 0.71 (0.39, 1.31) | 0.39 (0.16, 1.00) | 0.42 (0.16, 1.09) |
| Native American | 0.95 (0.48, 2.30) | 1.11 (0.51, 2.33) | 1.34 (0.58, 3.07) | 1.33 (0.59, 3.00) | 0.49 (0.13, 1.88) | 0.52 (0.14, 1.90) |
| Male | 2.20 (1.51, 3.21) | 1.98 (1.32, 2.99) | 2.04 (1.29, 3.23) | 2.06 (1.27, 3.33) | 2.58 (1.48, 4.51) | 2.65 (1.47, 4.78) |
| Low childhood SES | 0.65 (0.44, 0.98) | 0.95 (0.47, 1.05) | 1.25 (0.80, 1.94) | 1.22 (0.78, 1.91) | 0.73 (0.44, 1.22) | 0.72 (0.43, 1.30) |
| Treatment | 0.97 (0.57, 1.65) | 0.71 (0.54, 1.64) | 0.87 (0.49, 1.53) | 0.88 (0.49, 1.55) | 0.72 (0.34, 1.49) | 0.75 (0.34, 1.54) |
| Pubertal age | 1.04 (0.93, 1.17) | 1.05 (0.93, 1.18) | 0.73 (0.61, 0.89) | 0.73 (0.60, 0.88) | 1.07 (0.90, 1.26) | 1.10 (0.92, 1.32) |
| Sexual abuse | 2.00 (1.15, 3.47) | 1.94 (1.11, 3.35) | 2.01 (1.14, 3.57) | 1.87 (1.05, 3.35) | 2.83 (1.39, 5.79) | 2.38 (1.19, 4.78) |
Note. CI = confidence interval; NS = not significant (omitted from the model); OR = odds ratio; SES = socioeconomic status; STI = sexually transmitted infection. Ellipses indicate values were not calculated as part of the analysis design. The sample size was n = 770.
Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV)26 diagnoses for alcohol or marijuana abuse or dependence, and nicotine dependence were based on the Diagnostic Interview Schedule27 at each time point (at ages 30, 33, and 39 years). If respondents met diagnostic criteria in any of the 3 assessments, disorder was coded as 1 (0 otherwise).
TABLE 3—
Association Between Age of Sexual Initiation and Adult Depression and Physical Health for Main Effects and Mediated Through Sexual Consequences: Seattle Social Development Project; Seattle, WA; 2005–2014
| Variable | Depression,a OR (95% CI) | Poor Health,b OR (95% CI) | Obesity,c OR (95% CI) | |||
| Unmediated | Mediated | Unmediated | Mediated | Unmediated | Mediated | |
| Main effect: age of initiation | 0.97 (0.89, 1.05) | 0.99 (0.90, 1.08) | 0.87 (0.81, 0.93) | 0.87 (0.80, 0.95) | 0.88 (0.81, 0.94) | 0.85 (0.78, 0.92) |
| Mediators | ||||||
| STI | . . . | 1.10 (0.65, 1.71) | . . . | 0.61 (0.38, 0.91) | . . . | 0.93 (0.55, 1.45) |
| Adolescent pregnancy | . . . | 1.10 (0.66, 1.67) | . . . | 1.10 (0.72, 1.57) | . . . | 0.83 (0.53, 1.21) |
| High number of sexual partners | . . . | 1.12 (0.69, 1.69) | . . . | 1.16 (0.78, 1.61) | . . . | 0.75 (0.49, 1.07) |
| Gender interactions: gender × pubertal age | NS | NS | NS | NS | NS | NS |
| Controls | ||||||
| Outcome at ages 10–11 y | 2.81 (0.65, 9.58) | 2.83 (0.60, 11.50) | 1.52 (1.03, 2.10) | 1.55 (1.05, 2.14) | 8.27 (3.43, 17.33) | 8.22 (3.43, 17.12) |
| Externalizing | . . . | . . . | 1.11 (0.62, 1.81) | 1.17 (0.65, 1.91) | 0.97 (0.52, 1.63) | 1.02 (0.54, 1.74) |
| Black | 1.27 (0.79, 1.89) | 1.24 (0.76, 1.86) | 1.25 (0.81, 1.80) | 1.30 (0.84, 1.89) | 1.54 (0.98, 2.26) | 1.58 (0.99, 2.33) |
| Asian American | 0.39 (0.20, 0.68) | 0.39 (0.20, 0.70) | 1.21 (0.79, 1.75) | 1.23 (0.79, 1.78) | 0.67 (0.42, 0.98) | 0.65 (0.41, 0.96) |
| Native American | 1.58 (0.76, 2.92) | 1.57 (0.76, 2.89) | 1.25 (0.60, 2.32) | 1.26 (0.59, 2.37) | 0.79 (0.37, 1.51) | 0.81 (0.38, 1.55) |
| Male | 0.48 (0.32, 0.68) | 0.48 (0.31, 0.69) | 0.77 (0.55, 1.02) | 0.72 (0.51, 0.96) | 0.69 (0.48, 0.92) | 0.69 (0.48, 0.93) |
| Low childhood SES | 1.16 (0.77, 1.64) | 1.15 (0.76, 1.63) | 1.43 (1.01, 1.92) | 1.44 (1.01, 1.93) | 1.40 (0.98, 1.89) | 1.41 (0.98, 1.91) |
| Treatment | 0.59 (0.32, 0.99) | 0.59 (0.32, 0.99) | 0.89 (0.55, 1.32) | 0.89 (0.55, 1.33) | 0.73 (0.44, 1.11) | 0.72 (0.44, 1.10) |
| Pubertal age | 0.86 (0.75, 0.97) | 0.87 (0.76, 0.97) | 0.92 (0.83, 1.02) | 0.92 (0.83, 1.00) | 0.88 (0.79, 0.97) | 0.88 (0.79, 0.96) |
| Sexual abuse | 2.78 (1.56, 5.05) | 2.65 (1.48, 4.32) | 1.20 (0.71, 1.88) | 1.24 (0.74, 1.94) | 1.33 (0.76, 2.13) | 1.40 (0.80, 2.25) |
Note. CI = confidence interval; NS = not significant (omitted from the model); OR = odds ratio; SES = socioeconomic status; STI = sexually transmitted infection. Ellipses indicate values were not calculated as part of the analysis design. The sample size was n = 769.
Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV)26 diagnosis for major depressive disorder was based on the Diagnostic Interview Schedule27 at each time point (at ages 30, 33, and 39 years). If respondents met diagnostic criteria in any of the 3 assessments, disorder was coded as 1 (0 otherwise).
Participants were asked “How would you describe your general health?” Response options of “fair” and “poor” were coded as 1, and “excellent” and “good” were coded as 0 for a measure of poor health.
Interviewer-measured height and weight were used to calculate body mass index at each time point; the maximum value was used in analyses to calculate whether participants met criteria for being obese. Obesity was defined as a body mass index of ≥ 30 kg/m2.
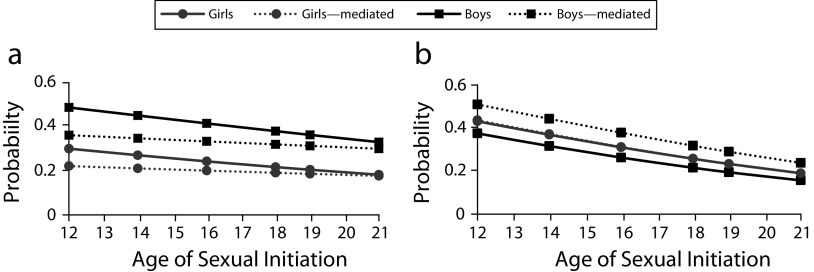
For all outcomes, we conducted logistic regressions with MLR estimator in Mplus 7.4 (Muthén and Muthén, Los Angeles, CA). Figure 1 shows the predicted probability of alcohol disorder and poor general health at a given age of sexual initiation. (These 2 plots are presented as representative examples; plots for the other outcomes are in Figure A, available as a supplement to the online version of this article at http://www.ajph.org.) Each plot shows the unmediated relationship between age of sexual initiation and outcome (step 1) and the same relationship after sexual consequences were added (step 4), separately by gender.
FIGURE 1—
Predicted Probabilities, Based on Age of Sexual Initiation, of (a) Alcohol Disorder and (b) Poor General Health: Seattle Social Development Project; Seattle, WA; 2005–2014
Note. For all plots, race = White; no early substance use; childhood externalizing = 0.23; internalizing = 0.09; not overweight; pubertal age = 13 years; no childhood sexual abuse. For mediated plots, no STI, no adolescent pregnancy, not 10 or more sexual partners.
We tested linear and quadratic terms for the age of initiation to test for nonlinear trends. Quadratic terms were not consistently significant, did not improve model fit, and were not included in the final models. In all models, we tested gender moderation in the relationship between age of initiation and the outcome through a multiplicative interaction term. Main effects of gender were significant in analyses of 4 of the 6 outcomes and are shown in the graphs in Figure 1 (also see Tables 2 and 3); however, none of the gender interaction terms were significant. In addition, because earlier pubertal age has been shown to be risky for girls,23 we tested for an interaction between pubertal age and gender in each of the models. For parsimony, we dropped interaction terms from the model if they were not significant. Race by age of initiation interactions were not significant, nor were race by pubertal age interactions. Race also did not consistently moderate the relationship between mediators and outcomes.
RESULTS
As shown in Table 2, the relationship between age of sexual initiation and alcohol disorder when participants were in their 30s was not significant (P = .054). These results suggest that the risk of alcohol disorder was similar regardless of age of sexual initiation. Male gender, childhood socioeconomic status, and sexual abuse predicted increased risk for developing an alcohol disorder.
A significant relationship between age of initiation of sex and risk of nicotine disorder emerged in the unmediated model, with delay of sex predicting less disorder. In addition, higher externalizing, male gender, pubertal age, and sexual abuse all predicted nicotine disorder. A gender by pubertal timing interaction was also significant, indicating that for boys, pubertal age played a minimal role in the risk of nicotine addiction. For girls, earlier pubertal age was a strong risk factor for nicotine disorder. After we added the mediators, age of initiation was not related to nicotine disorder (P = .059). No additional predictors emerged.
Marijuana disorder was associated with earlier age of sexual initiation in the unmediated models. Identifying as Asian American, male gender, and sexual abuse also increased the likelihood of marijuana disorder. Once we added the mediators, the relationship of age of initiation with marijuana disorder was reduced but remained significant. Having a high number of sexual partners also predicted marijuana disorder in the mediated model.
In Table 3, the unmediated model showed no association between age of sexual initiation and later meeting criteria for major depression. Being Asian American, male, and reporting later puberty all reduced the risk of depression; experiencing sexual abuse increased the risk. These findings remained significant after we added the mediators to the model. None of the mediators predicted depression when participants were in their 30s.
There was a strong association between age of sexual initiation and poor health, with older age of initiation predicting a lower likelihood of poor health in adulthood. Other than being overweight in childhood, none of the other predictors, including the mediators, were related to poor health when the participants were in their 30s. In the mediated model, having had an STI was also associated with poorer health.
Similar to our findings for poor health, we found that older age of initiation was linked to a lower likelihood of obesity when participants were in their 30s. Being overweight and male increased the risk of adult obesity; higher pubertal age lowered the risk. These results held after we added the mediators into the model. None of the mediators were significantly associated with obesity.
DISCUSSION
We examined the degree to which the relationships between adolescent sexual initiation and later health outcomes are explained by sex-related consequences of initiation (STI, adolescent pregnancy, high number of sexual partners). That is, if adolescents can avoid getting an STI, becoming pregnant or getting their partner pregnant, and engaging in intercourse with a high number of partners, does age of initiation still predict adult health? Overall, the pattern of findings suggests that alcohol and nicotine disorders and depression are not directly related to age of sexual initiation or may be preventable if certain sexual consequences are avoided. Accounting for sexual consequences reduced but did not fully explain the relationship between age of sexual initiation and marijuana disorder; however, the relationships of physical health and obesity with earlier sexual initiation were not explained by sexual consequences.
These results suggest that interventions targeting safe sexual practices may be one important strategy for preventing some substance use disorders in adulthood. Comprehensive sexual education and access to contraception have been shown to be effective at boosting consistent use of contraception and reducing sexual risk taking.22 For example, a recent study showed that making long-acting reversible contraceptives or intrauterine devices available to adolescent girls reduced pregnancy risk by as much as 29%.33 However, results also showed that focusing on prevention of sexual consequences alone is unlikely to reduce the risk of early sexual initiation having an impact on marijuana dependence or physical health. Instead, more comprehensive prevention programs that target a number of risk factors, including early sexual initiation, are needed. Although waiting to have sex can be a healthy choice,34 we caution that efforts focused on delaying sexual initiation alone are likely to be insufficient, especially given the body of research that reports common early risk factors that drive the association between early sex and health.5,9,15 Evaluations of previous efforts to delay sexual initiation without addressing the broader context of other early risk factors have shown that such programs are either ineffective or may delay initiation by several months but lead to more risk-taking activity once adolescents do initiate sexual activity.34,35
Strengths and Limitations
This study is one of the first to extend the relationship between adolescent sexual initiation and health into one’s 30s. Strengths include a longitudinal design with prospective measurement and time-ordered control variables that include earlier manifestations of the outcome variables and childhood internalizing and externalizing behavior. Assessment of age of sexual initiation included multiple, prospective reports. This study is also one of the first to test the degree to which sexual consequences are the mechanism by which early sexual initiation is linked to later health.
There are, however, some notable limitations. We relied on a single teacher report of early overweight status, and some of the measures were retrospective. We purposefully did not include other mediators beyond those directly linked to sexual initiation to establish whether sexual consequences alone, which are more common among early sexual initiators,18 may explain the relationship between age of initiation and health. Future studies need to more fully examine the role of the broader social developmental context in which early sexual initiation occurs to better understand the association between early sexual initiation and adult health and to identify potential preventive intervention targets.
Public Health Implications
Addressing sexual consequences of early sex may be effective at curbing the risk posed by early sexual initiation on later substance use in adulthood. Future research needs to examine the mechanisms linking early sexual initiation and other health outcomes, in particular physical health and obesity.
ACKNOWLEDGMENTS
This research was supported by the National Institute on Drug Abuse (grants R01DA033956, 1R01DA024411, and 1R01DA009679).
Note. Content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agency. The National Institute on Drug Abuse played no role in the study design; in the collection, analysis, and interpretation of data; in the writing of the report; nor in the decision to submit the article for publication.
HUMAN PARTICIPANT PROTECTION
All research activities were reviewed and approved by the University of Washington institutional review board.
Footnotes
See also Galea and Vaughan, p. 722.
REFERENCES
- 1.Finer LB, Philbin JM. Sexual initiation, contraceptive use, and pregnancy among young adolescents. Pediatrics. 2013;131(5):886–891. doi: 10.1542/peds.2012-3495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McGue M, Iacono WG. The association of early adolescent problem behavior with adult psychopathology. Am J Psychiatry. 2005;162(6):1118–1124. doi: 10.1176/appi.ajp.162.6.1118. [DOI] [PubMed] [Google Scholar]
- 3.Harden KP. A sex-positive framework for research on adolescent sexuality. Perspect Psychol Sci. 2014;9(5):455–469. doi: 10.1177/1745691614535934. [DOI] [PubMed] [Google Scholar]
- 4.Zimmer-Gembeck MJ, Helfand M. Ten years of longitudinal research on US adolescent sexual behavior: developmental correlates of sexual intercourse, and the importance of age, gender and ethnic background. Dev Rev. 2008;28(2):153–224. [Google Scholar]
- 5.Epstein M, Bailey JA, Manhart LE et al. Understanding the link between early sexual initiation and later sexually transmitted infection: test and replication in two longitudinal studies. J Adolesc Health. 2014;54(4):435–441.e2. doi: 10.1016/j.jadohealth.2013.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sandfort TG, Orr M, Hirsch JS, Santelli J. Long-term health correlates of timing of sexual debut: results from a national US study. Am J Public Health. 2008;98(1):155–161. doi: 10.2105/AJPH.2006.097444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vasilenko SA, Kugler KC, Rice CE. Timing of first sexual intercourse and young adult health outcomes. J Adolesc Health. 2016;59(3):291–297. doi: 10.1016/j.jadohealth.2016.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Finger R, Thelen T, Vessey JT, Mohn JK, Mann JR. Association of virginity at age 18 with educational, economic, social, and health outcomes in middle adulthood. Adolesc Fam Health. 2004;3(4):164–170. [Google Scholar]
- 9.Sabia JJ. Does early adolescent sex cause depressive symptoms? J Policy Anal Manage. 2006;25(4):803–825. doi: 10.1002/pam.20209. [DOI] [PubMed] [Google Scholar]
- 10.Spriggs AL, Halpern CT. Sexual debut timing and depressive symptoms in emerging adulthood. J Youth Adolesc. 2008;37(9):1085–1096. doi: 10.1007/s10964-008-9303-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Meier AM. Adolescent first sex and subsequent mental health. Am J Sociol. 2007;112(6):1811–1847. [Google Scholar]
- 12.Haase CM, Landberg M, Schmidt C, Lüdke K, Silbereisen RK. The later, the better? Early, average, and late timing of sexual experiences in adolescence and psychosocial adjustment in young adulthood. Eur Psychol. 2012;17(3):199–212. [Google Scholar]
- 13.Vrangalova Z, Savin-Williams RC. Adolescent sexuality and positive well-being: a group-norms approach. J Youth Adolesc. 2011;40(8):931–944. doi: 10.1007/s10964-011-9629-7. [DOI] [PubMed] [Google Scholar]
- 14.Harden KP. True love waits? A sibling-comparison study of age at first sexual intercourse and romantic relationships in young adulthood. Psychol Sci. 2012;23(11):1324–1336. doi: 10.1177/0956797612442550. [DOI] [PubMed] [Google Scholar]
- 15.Epstein M, Bailey JA, Manhart LE, Hill KG, Hawkins JD. Sexual risk behavior in young adulthood: broadening the scope beyond early sexual initiation. J Sex Res. 2014;51(7):721–730. doi: 10.1080/00224499.2013.849652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Samek DR, Iacono WG, Keyes MA, Epstein M, Bornovalova MA, McGue M. The developmental progression of age 14 behavioral disinhibition, early age of sexual initiation, and subsequent sexual risk-taking behavior. J Child Psychol Psychiatry. 2014;55(7):784–792. doi: 10.1111/jcpp.12176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Monahan KC, Lee JM. Adolescent sexual activity: links between relational context and depressive symptoms. J Youth Adolesc. 2008;37(8):917–927. [Google Scholar]
- 18.Kugler KC, Vasilenko SA, Butera NM, Coffman DL. Long-term consequences of early sexual initiation on young adult health: a causal inference approach. J Early Adolesc. 2015;37(5):662–676. doi: 10.1177/0272431615620666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Donahue KL, Lichtenstein P, Långström N, D’Onofrio BM. Why does early sexual intercourse predict subsequent maladjustment? Exploring potential familial confounds. Health Psychol. 2013;32(2):180–189. doi: 10.1037/a0028922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Miller HG, Cain VS, Rogers SM, Gribble JN, Turner CF. Correlates of sexually transmitted bacterial infections among US women in 1995. Fam Plann Perspect. 1999;31(1):4–23. [PubMed] [Google Scholar]
- 21.Sneed CD. Sexual risk behavior among early initiators of sexual intercourse. AIDS Care. 2009;21(11):1395–1400. doi: 10.1080/09540120902893241. [DOI] [PubMed] [Google Scholar]
- 22.Kirby D. Emerging answers: research findings on programs to reduce teen pregnancy (summary) Am J Health Educ. 2001;32(6):348–355. [Google Scholar]
- 23.Hummel A, Shelton KH, Heron J, Moore L, van den Bree MBM. A systematic review of the relationships between family functioning, pubertal timing and adolescent substance use. Addiction. 2013;108(3):487–496. doi: 10.1111/add.12055. [DOI] [PubMed] [Google Scholar]
- 24.Simpson TL, Miller WR. Concomitance between childhood sexual and physical abuse and substance use problems: a review. Clin Psychol Rev. 2002;22(1):27–77. doi: 10.1016/s0272-7358(00)00088-x. [DOI] [PubMed] [Google Scholar]
- 25.Hawkins JD, Kosterman R, Catalano RF, Hill KG, Abbott RD. Promoting positive adult functioning through social development intervention in childhood: long-term effects from the Seattle Social Development Project. Arch Pediatr Adolesc Med. 2005;159(1):25–31. doi: 10.1001/archpedi.159.1.25. [DOI] [PubMed] [Google Scholar]
- 26.Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 27.Robins L, Cottler L, Bucholz K, Compton W. National Institute of Mental Health Diagnostic Interview Schedule for DSM-IV. St Louis, MO: Washington University, Department of Psychiatry; 1998.
- 28.Johnson TP, Mott JA. The reliability of self-reported age of onset of tobacco, alcohol and illicit drug use. Addiction. 2001;96(8):1187–1198. doi: 10.1046/j.1360-0443.2001.968118711.x. [DOI] [PubMed] [Google Scholar]
- 29.Lengua LJ, Sadowski CA, Friedrich WN, Fisher J. Rationally and empirically derived dimensions of children’s symptomatology: expert ratings and confirmatory factor analyses of the CBCL. J Consult Clin Psychol. 2001;69(4):683–698. [PubMed] [Google Scholar]
- 30.Achenbach TM. Manual for the Child Behavior Checklist/4-18 and 1991 Profile. Burlington, VT: University of Vermont Department of Psychiatry; 1991. [Google Scholar]
- 31.Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 32.MacKinnon DP, Fairchild AJ, Fritz MS. Mediation analysis. Annu Rev Psychol. 2006;58(1):593–614. doi: 10.1146/annurev.psych.58.110405.085542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ricketts S, Klingler G, Schwalberg R. Widespread use of long-acting reversible contraceptives and rapid decline in births among young, low-income women. Perspect Sex Reprod Health. 2014;46(3):125–132. doi: 10.1363/46e1714. [DOI] [PubMed] [Google Scholar]
- 34.Santelli JS. Abstinence-only education: politics, science, and ethics. Soc Res (New York) 2006;73(3):835–858. [Google Scholar]
- 35.Kirby D. Emerging answers 2007: new research findings on programs to reduce teen pregnancy and sexually transmitted diseases. Washington, DC: Power to Decide; 2007. Available at: https://powertodecide.org/what-we-do/information/resource-library/emerging-answers-2007-new-research-findings-programs-reduce. Accessed February 18, 2017.