Abstract
Background. In 2017, a “Muslim ban” on immigrants to the United States was coupled with a continued rise in Islamophobia and hate crimes toward Muslims. Islamophobia undermines health equity, yet delineating the effects of Islamophobia globally is challenging as it affects a myriad of groups (geographically, racially, and socially). Additionally, stereotypes equate all Muslims with populations from the Middle East and South Asia. To date, health research pays insufficient attention to Islamophobia, Muslims, and those racialized to be Muslim.
Objectives. This literature review advances our understanding of racism and health by examining the racialization of religion, by specifically examining Islamophobia as a form of discrimination.
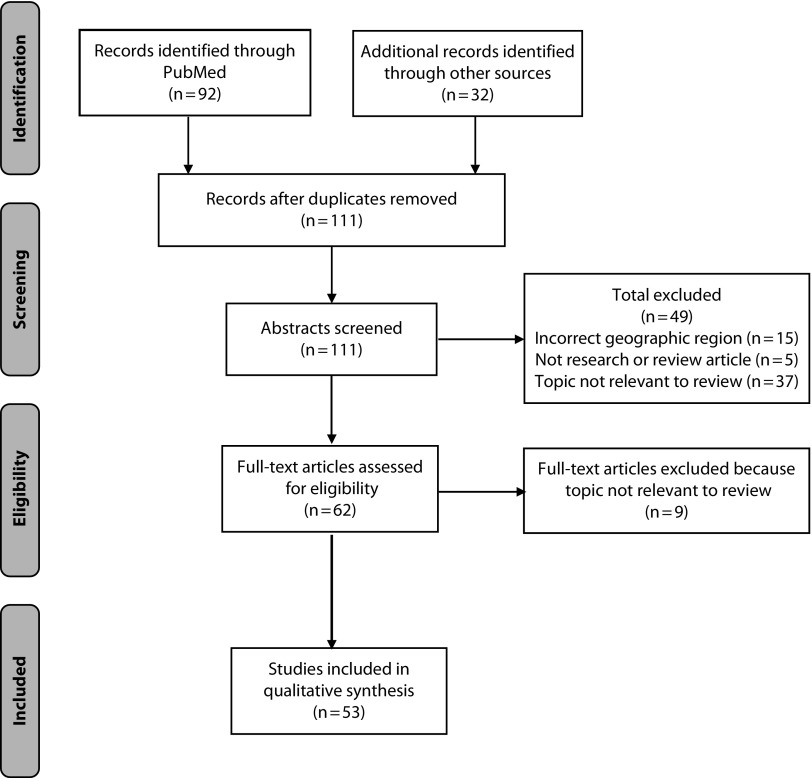
Search Methods. Per PRISMA guidelines, we conducted a search in October 2017 using PubMed–MEDLINE and a combination of terms. We identified additional articles using other search engines. For inclusion, articles needed to include a descriptor of discrimination, contain an identifier of Muslim or Muslim-like identity (i.e., groups commonly perceived as Muslim, including Arabs, Middle Easterners, North Africans, and South Asians), include a health outcome, be in English, and be published between 1990 and 2017.
Selection Criteria. We identified 111 unique peer-reviewed articles. We excluded articles that did not meet the following criteria: (1) examined Islamophobia, discrimination, or racism among a Muslim or Muslim-like population; (2) included a health outcome or discussion of health disparities; and (3) was conducted in North America, Europe, Australia, or New Zealand. This yielded 53 articles.
Results. The majority of studies (n = 34; 64%) were quantitative. The remaining studies were qualitative (n = 7; 13%), mixed methods (n = 2; 4%), or reviews (n = 10; 19%). Most studies were based in the United States (n = 31; 58%). Nearly half of the reviewed studies examined mental health (n = 24; 45%), and one fourth examined physical health or health behaviors (n = 13; 25%). Others focused on both physical and mental health (n = 10; 19%) or health care seeking (n = 7; 13%). Studies showed associations between Islamophobia and poor mental health, suboptimal health behaviors, and unfavorable health care–seeking behaviors.
Conclusions. This study elucidates the associations between Islamophobia, health, and socioecological determinants of health. Future studies should examine the intersectional nature of Islamophobia and include validated measures, representative samples, subgroup analyses, and comparison groups. More methodologically rigorous studies of Islamophobia and health are needed.
Public Health Implications. Addressing the discrimination-related poor health that Muslims and racialized Muslim-like subgroups experience is central to the goals of health equity and assurance of the fundamental right to health.
PLAIN-LANGUAGE SUMMARY
Islamophobia undermines health equity, yet little is known about how discrimination is associated with the health of Muslims. This systematic literature review describes and analyzes the current literature on Islamophobia and health. The included studies met the following criteria: they (1) were written in English; (2) examined Islamophobia, discrimination, or racism; (3) assessed a health outcome; (4) utilized a sample or population of Muslims of any racial and ethnic origin, Middle Easterners, North Africans, or South Asians; (5) were conducted in North America, Europe, Australia, or New Zealand; and (6) were peer-reviewed articles published between 1990 and 2017. Among the 53 studies identified, most were conducted in the United States and utilized cross-sectional study designs. The studies demonstrated associations between Islamophobia and poor mental health, suboptimal health behaviors, and a lack of health care–seeking behaviors. Fewer studies considered impacts on physical health conditions like cardiovascular disease. Future studies should examine the intersectional nature of Islamophobia, accounting for the diversity of people who are affected and making better use of validated measures and appropriate comparison groups. Additional methodologically rigorous research on Islamophobia and health is needed to address health disparities and promote health equity for all.
Discrimination of Muslims is a growing phenomenon in White, Christian-majority countries. In the United States, Muslims have been included in an immigration ban, harassed on college campuses, and experienced racial profiling.1,2 In 2015, hate crimes against Muslims and Arabs rose by 78% to an all-time high.3 In 2015 and 2016, assaults against Muslims in the United States surpassed the modern peak reached after 9/11.1,2 Considering that Islam is the world’s second largest religion,4 Islamophobia challenges health equity and population health.5
Islamophobia is social stigma toward Islam and Muslims, dislike of Muslims as a political force, and a distinct construct referring to xenophobia and racism toward Muslims or those perceived to be Muslim.5 Delineating the effects of Islamophobia globally is challenging, as it affects diverse groups of people (geographically, racially, and socially).6 For example, in the United Kingdom, Muslims are primarily immigrant South Asians.7 In the United States, nearly 30% of Muslims identify as Black, another 30% are Asian (primarily South Asian), and the largest racial group of Muslims are classified as White, many of whom are from the Middle East.4,8,9 Stereotypical representations equate all Muslims with populations from the Middle East and South Asia.8 Since the transatlantic slave trade, Muslims in the United States have not been considered “real Americans,” and Muslim identity has been used to deny citizenship, including for Christians perceived to be Muslims.10 As described by Naber,11 “racialization of religion” portrays Middle Eastern immigrants as inferior to Whites and racially marked on the assumption that they are all Muslim. As such, Islamophobia targets both Muslims and those who are perceived as Muslims (e.g., Arabs, Middle Easterners, South Asians, Sikhs).
Research explicitly links discrimination at multiple levels to poor health.12–14 Experiencing discrimination is associated with the onset of physiological responses to stress that have longer-term implications for health outcomes, including a “wear and tear” impact on regulatory systems.15 Moreover, “context matters” as the relationships (or magnitudes) of the effects of discrimination vary by racial and ethnic groups.16,17 As Gee et al. argue,16 1 race does not fit all for the relationship between discrimination and health.
To date, no reviews have considered the existing literature on the impact of Islamophobia as a form of discrimination on the health of Muslims or those who are perceived as Muslim. This literature review advances our understanding of racism and health by focusing on an understudied conceptualization on the role of racialization of religion for health—specifically, by examining the effect of Islamophobia, as stigma and a form of discrimination, and health outcomes for populations in North America, Europe, Australia, and New Zealand.
METHODS
This systematic literature review follows the guidelines and criteria set forth by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA).18 We conducted a search on October 19, 2017 that used PubMed–MEDLINE and a combination of terms (in abstracts and titles; The box on page e3). For inclusion, articles needed to contain 1 of 4 descriptors of discrimination—Islamophobia, discrimination, religious discrimination, or racism—and an identifier of Muslim or Muslim-like identity (i.e., groups racialized to have a Muslim identity or those affected by Islamophobia through being perceived as Muslim, including Arabs, Middle Easterners, North Africans, and South Asians). Notably, this does not explicitly exclude other groups that could be Muslim or Muslim-like (e.g., Indonesians, African American Muslims). Studies also needed to include a health outcome, to be in English, and to be published between January 1, 1990 and October 1, 2017. We supplemented the primary search on PubMed–MEDLINE with searches on PsycINFO, the Cumulative Index of Nursing and Allied Health Literature, Academic Search Complete, Web of Science, and Google Scholar and a review of references.
SEARCH TEXT ENTERED INTO PUBMED ADVANCED SEARCH BUILDER
(((((“Islamophobia”[Title/Abstract] OR “discrimination”[Title/Abstract] OR “religious discrimination”[Title/Abstract] OR “racism”[Title/Abstract])) AND English[Language]) AND (“Muslim”[Title/Abstract] OR “Arab”[Title/Abstract] OR “Middle Eastern”[Title/Abstract] OR “North African”[Title/Abstract] OR “South Asian”[Title/Abstract])) AND (“Health” [Title/Abstract]) AND (“1990/01/01”[Date - Publication]: “2017/10/01”[Date - Publication])).
RESULTS
The primary search produced 92 articles, and supplemental searches produced 32 articles. After we removed duplicates, the search yielded 111 articles. At least 1 of the study authors evaluated each title and abstract against the inclusion criteria. After all the authors conferred, we excluded articles that did not meet the following criteria: (1) examined Islamophobia, discrimination, or racism among a Muslim or Muslim-like population; (2) included a health outcome, structural determinant of health, or discussion of health disparities; (3) was conducted in North America, Europe, Australia, or New Zealand; (4) was a peer-reviewed article. On the basis of an evaluation of titles and abstracts, we excluded 49 articles that did not meet these criteria, yielding 62 articles. We evaluated the full texts of these 62 articles to ensure that each article was a true match. This resulted in the further exclusion of 9 articles, yielding 53 articles (Table A, available as a supplement to the online version of this article at http://www.ajph.org).5,17,19–69 Decisions were agreed upon through review and consensus by all authors (Figure 1). Using the ROBINS-I,70 we assessed the risk of bias in quantitative articles (Table B, available as a supplement to the online version of this article at http://www.ajph.org).
FIGURE 1—
Literature Review and Screening
Of the 53 reviewed studies, the majority (n = 34; 64%) were quantitative (Table 1). The remaining studies utilized primary data collection for qualitative (n = 7; 13%)19,20,26,27,44,60,69 or mixed methods analysis (n = 2; 4%)31,35 or conducted reviews (n = 10; 19%),5,22,25,28,30,41,42,45,56,63 and only 4 studies used repeated cross-sectional or longitudinal designs.43,46,50,62
TABLE 1—
Islamophobia and Health Literature Review Results: October 2017
| Characteristic | Studies (n = 53), No. (%) |
| Publication year | |
| Before 2001 | 1 (1.89) |
| 2002–2005 | 2 (3.77) |
| 2006–2010 | 18 (33.96) |
| 2011–2015 | 21 (39.62) |
| 2016–2017 | 11 (20.75) |
| Location | |
| Australia | 1 (1.89) |
| Canada | 4 (7.55) |
| Denmark | 2 (3.77) |
| France | 1 (1.89) |
| Global or multiple countries | 2 (3.77) |
| Netherlands | 3 (5.66) |
| Sweden | 1 (1.89) |
| United Kingdom | 8 (15.09) |
| United States | 31 (58.49) |
| Detroit, MI area | 6 (11.32) |
| Chicago, IL area | 4 (7.55) |
| Methods | |
| Qualitative | 7 (13.21) |
| Quantitative | 34 (64.15) |
| Cross-sectional | 30 (56.60) |
| Cross-sectional (repeated) | 3 (5.66) |
| Longitudinal | 1 (1.89) |
| Mixed methods | 2 (3.77) |
| Review (systematic or narrative) | 10 (18.87) |
| Included a measure or proxy measure of discrimination | |
| No | 36 (67.92) |
| Yes | 17 (32.08) |
| Health outcome (not mutually exclusive categories) | |
| Mental health | 24 (45.28) |
| Physical health and related health behaviors | 13 (24.53) |
| Both mental and physical health | 10 (18.87) |
| Health care seeking | 7 (13.21) |
| Sample size | |
| None given | 10 (18.87) |
| 1–100 | 9 (16.98) |
| 101–1000 | 23 (43.40) |
| > 1000 | 11 (20.75) |
| Measured religion or religiosity | |
| No | 34 (64.15) |
| Yes | 19 (35.85) |
| Source of article | |
| PubMed systematic search | 34 (64.15) |
| Other | 19 (35.85) |
| Final score for bias assessment | |
| Low | 4 (7.55) |
| Moderate | 6 (11.32) |
| Serious | 14 (26.42) |
| Critical | 10 (18.87) |
| Not applicable | 19 (35.85) |
The majority of studies were from the United States (n = 31; 58%).5,17,19–24,29–31,33,35–38,41,42,46,49,52–61,63,67 The remaining studies were from Australia, Canada, Denmark, France, Scotland, Sweden, the Netherlands, and the United Kingdom (n = 22, 42%).25–28,32,34,39,40,43–45,47,48,50,51,62,64–66,68,69 Ten studies used samples from Michigan and Chicago, Illinois.17,21,23,24,29,41,57–59,67 Several studies had samples of between 100 and 1000 people.
Nearly half of the reviewed studies examined mental health (n = 24; 45%). A fourth of the studies examined physical health or health behaviors (n = 13; 25%).19,28,29,38,43,46,53,54,64,66,68 Others focused on both physical and mental health (n = 10; 19%) or health care seeking (n = 7; 13%).26,49,58–60,67,69 Only a third of the studies (n = 19; 36%) included a measure of religion. Bias was a serious or critical concern in most quantitative studies (n = 24). Several studies focused on refugees31,47,50,51 or women.35,46,58–60,67
Mental Health
The research showed consistent relationships between experiences of discrimination and poor mental health among Muslims and Muslim-like populations. Findings of worse mental health were largely consistent, irrespective of the population or the methodology used. Four studies examined mental health of Arab and Chaldean Americans in Detroit, Michigan.17,23,24,57 These studies found that ever experiencing discrimination due to race, ethnicity, or religion was associated with higher levels of psychological distress.17,23 This association was observed irrespective of racial identification (White or non-White), skin color (dark–medium or light), Arab American identification (yes or no), or area of residence (in ethnic enclave or outside of ethnic enclave),17 and it remained even after accounting for confounders.17,23 Gender moderates this relationship, as discrimination is associated with psychological distress among men but not women.24 Discrimination was also associated with higher levels of psychological distress among Christians but not Muslims.17
In several metropolitan areas in the United States, 2 studies found that discrimination due to Muslim identity was associated with a greater number of depressive symptoms36,37 but not with substance use.36 Among Arab Americans in Florida, discrimination due to Arab identity was associated with psychological distress.52 Among Arab Americans in New York City, qualitative research showed fears and anxiety about potential discrimination.20 Among Muslim Americans in Oklahoma, religious discrimination was associated with higher levels of paranoia among men but not women.61 Among South Asians in San Francisco, California, and Chicago, Illinois, experiences of discrimination were associated with higher depressive symptoms, anger, and anxiety.55 More traditional beliefs and utilizing an active coping style buffered some of these associations.55 Among adolescents, perceived racism was associated with poor mental health, and both religious support and religious coping were associated with positive mental health.21
Research has also examined the association between discrimination and mental health in Europe, Canada, and Australia. Among British Muslims, experiencing a racist or discriminatory incident attributed to 9/11 was positively associated with depressive symptomology.65 Describing oneself as “highly visible as a Muslim” was associated with depression.65 In Quebec, recent Arab and Haitian immigrants who experienced discrimination due to race, ethnicity, or religion had greater psychological distress.62 Arab immigrants reported lower levels of discrimination than did Haitian immigrants.34 In focus groups of South Asian women in the United Kingdom, religious discrimination, stereotyping, and social isolation were thought to influence self-harm.27 For Australian Muslims, interpersonal discrimination was associated with lower self-esteem, whereas systemic discrimination was associated with more self-esteem.32 Among Muslim-like groups in the Netherlands (e.g., South Asians, Turks, and Moroccans), perceived ethnic discrimination was associated with depressive symptoms, with religion not serving as a significant moderator.39,40 Qualitative research with Pakistanis and Bangladeshis in the United Kingdom showed that experiences of racism were sources of psychological distress.44 For North Africans in France, perceived ethnic discrimination was associated with more psychological distress among women but not men.48
A few studies examined discrimination and mental health among refugees. Among Middle Eastern refugees to Sweden, experiencing discrimination or status loss was correlated with symptoms of common mental disorders and posttraumatic stress disorder (PTSD).47 For children and young adult refugees in Denmark, discriminating experiences due to being a foreigner were associated with internalizing behaviors.50,51 For adolescent Somali refugees in the United States, greater reported everyday discriminatory events were associated with higher levels of PTSD and depression, after accounting for other trauma.31
Physical Health and Related-Health Behaviors
The literature yielded limited published evidence on the relationship between Islamophobic discrimination and specific physical health outcomes. Lauderdale46 described how there was an increase in the rates of preterm births and low birth weight among women with Arabic names in California who gave birth within 6 months after 9/11 relative to the year before. No differences were documented among women with non-Arabic names.
Three studies assessed the relationship between discrimination and self-rated health—a valid measure of overall health38 and a reliable predictor of mortality.19 In Canada, mismatched racial identities corresponded with poor self-reported health, especially for respondents who considered themselves White but believed that others tended to think they were something else.66 In the United States, Hodge et al. examined self-reported health among Muslims,38 whereas Abdulrahim and Ajrouch considered this relationship specifically among immigrant Arab Americans.19 They found no differences by gender or ethnicity, but religiosity was associated with better self-rated health. Using 46 in-depth interviews within the Detroit area, they found no mention of discrimination or stereotyping despite expecting to do so.19
Several studies considered discrimination and physical activity or nutrition. A review found that discrimination was a contributing factor to the lack of physical activity among South Asian immigrants.28 In California, 822 South Asians who experienced discrimination had more activity limitation days annually than South Asians who did not report discrimination.33 However, another study found that frequency of experiencing discrimination had a significantly positive effect on daily step counts for South Asians in the United States.29 Relatedly, for South Asians in San Francisco and Chicago, discrimination was associated with higher consumption of sweets but not with consumption of fruits and vegetables or cardiovascular disease risk.53,54 In the Netherlands, perceived discrimination was positively associated with body mass index for Turks and Moroccans, with greater effects for men than women.64
Studies from the United Kingdom provide evidence for links to chronic diseases. The relationship between psychosocial factors and coronary heart disease risk was assessed among Sikh, Hindu, and Muslim South Asians.68 Muslim respondents reported the highest level of racial discrimination, chronic stress, and financial strain.68 Muslims also reported lower levels of physical activity than the other religious groups. In the United Kingdom, researchers also found that Pakistanis and Bangladeshis had worsening blood pressure, cholesterol, and self-rated health after 9/11, arguing that this was attributable to anti-Muslim discrimination.43
Health Care–Seeking Behavior
Seven studies examined discrimination and access to health care.26,49,58–60,67,69 All studies found that religious discrimination or perceived discrimination played a role in how Muslim and Muslim-like populations accessed health care. Three of these studies relied on the same survey of 240 Muslim women from mosques and Muslim organization sites in Greater Chicago.58,59,67 Perceived religious discrimination in health care was negatively associated with seeking any medical care and having a mammogram in the past 2 years, but it was not associated with cervical cancer screening.58,59,67 Martin used a nationwide convenience sample of 227 Muslim adults to create a Health Care Discrimination Scale,49 illuminating the effects of discrimination of Muslims in the US health care system. Discrimination limited access to health care services, and women who wore the veil reported more discrimination in health care settings than women who did not.49
Three qualitative studies explored patient perceptions of discrimination in accessing health care services.26,60,69 One study of 6 Muslim immigrant women identified significant gaps between existing maternity services and availability of culturally appropriate health information in Canada.60 Thirty-five South Asian parents in focus groups in Scotland felt that discrimination was a barrier for professionals to meet their children’s mental health needs.26 In Scotland, 25 interviews of South Asian Sikh and Muslim patients showed that personal racial and religious discrimination was a barrier to accessing health care.69
DISCUSSION
This study highlights the literature on the associations between Islamophobia, health outcomes, and socioecological determinants of health. Although it is well established that racial discrimination is a determinant of poor health,12,71 the contribution of this review lies in its attention to Islamophobia, which is currently a highly politicized and contentious topic, an example of the “racialization of religion,” and an understudied determinant of poor health outcomes. In subsequent sections, we present a summary of findings, the shortcomings of reviewed research, and suggestions for advancing future research.
Summary of Findings
In general, discrimination was negatively associated with mental health, indicators of physical health, and health care access. Most studies occurred after 2010, and since 2001 there has been an exponential increase in studies of the effects of discrimination on the health of Muslim and Muslim-like populations. Studies were mostly in agreement that discrimination of Muslims was associated with worse mental health. Findings did not vary by race and ethnicity, but there were variations by gender and immigration status. There was a dearth of studies on the effect of Islamophobia and physical health outcomes. Typically, a specific health condition was examined by only 1 or 2 studies, thus minimizing the strength of the physical health conclusions.
Findings also showed that discrimination of Muslims was associated with poor health care–seeking behavior. Women who reported wearing religious attire also reported more discrimination in health care settings, and a study has found that religious clothing influences the care Muslim patients receive.49 Notably, these studies did not clearly define religious attire (e.g., hijabs or veils). This showed how Islamophobia goes beyond our conventional understanding of the relationship between race, discrimination, and health disparities, as characteristics such as religious attire can put one at risk for less favorable treatment or outcomes.
Measures of Islamophobic Discrimination
Studies varied in how they defined and measured Islamophobic discrimination. The majority of studies did not use a specific measure of Islamophobia or discrimination and, at most, used 1 to 5 survey items that asked about general experiences of discrimination. Among these studies, racial/ethnic discrimination was used more frequently than religious discrimination. One study used the Schedule of Racist Events,52 and one used the full Everyday Discrimination Scale.31 A few studies used the Perceived Religious Discrimination Scale developed by Rippy and Newman61 to measure religious discrimination of Muslims in health care.32 Interestingly, some studies, using the same data, operationalized discrimination using a different number of scale items,36–38 thus limiting comparability.
Islamophobia, however, encompasses several types of discrimination, including racial or religious discrimination. Studies did not differentiate between the different types of discrimination that Islamophobia comprises (e.g., racism, religious discrimination, discrimination on the basis of gender) and they infrequently used multiple, multidimensional, or multilevel measures of Islamophobia. However, many of the reviewed studies intended to examine racial, ethnic, or religious discrimination in isolation and not the more complex construct of Islamophobia. Health research should draw from race and ethnicity research that demonstrates an understanding of racialization of religion and intersectionality of Muslim identity.11 Only 1 study distinguished between racial and religious discrimination and health outcomes,65 highlighting the importance of choosing multiple and appropriate measures of Islamophobia.
Given shortcomings in measuring Islamophobia, future studies should focus on different dimensions of discrimination, such as religious attire or immigration status, which may capture the nuances of the harmful effects of Islamophobia. Moreover, as Martin explains,49 religion-related discrimination is of interest given the heightened level of Islamophobia and that the US census does not currently document religion. Therefore, future research initiatives should collect, analyze, and disseminate data on the role of religious discrimination and health. Also, we must consider how the health impact of Islamophobia differs from the impact of religious or race-based discrimination among various groups, such as African Americans, to understand if the impact of Islamophobia is uniquely deleterious.
Importantly, the studies we reviewed focused overwhelmingly on the acts of discrimination perpetrated by 1 individual against another, meaning that the roles of structural discrimination and Islamophobia were ignored. Because systems of oppression operate at multiple levels,13,22 the effects of Islamophobia on health also have to be understood at multiple levels, ranging from the individual to the structural.5 Measures of residential segregation, racialized institutional policies, and internalized Islamophobia could help researchers understand how multiple levels of Islamophobia operate to affect health. Overall, more research is needed in this area to disentangle the independent and joint influences of religion, race, and ethnicity on health.
Mediators and Moderators
The reviewed literature omitted key variables that provide important context for Islamophobia research; namely, studies largely failed to test the moderating or mediating role(s) of measures, including status loss; refugee, immigrant, or citizenship status; gender; class; language; skin color; and religious attire. Exceptions include 3 recent studies that considered gender as a moderator,24,48,64 1 study that considered the moderating role of religion,39 and 1 study that examined additional independent variables like persecution in country of origin, religious group, and length of stay in host country.62
Future research should continue to evaluate the role of religious identification as a moderator and religiosity as a mediator in the relationship between Islamophobia and health. For example, examination of religious identity as a moderator could help health researchers understand how Islamophobic discrimination affects the health of Middle Eastern immigrants who are racialized as Muslim but who may in fact be of a variety of religious affiliations. Islamophobia itself could also be a moderator or mediator of the relationship between race/ethnicity and health, particularly for groups that are racialized as Muslim.
Subgroup Identification and Distinction
Studies generally did not include measures that capture the heterogeneity or subgroups of Muslims. The importance of delineating subgroups within this body of work is imperative. However, studies on Muslim subgroups entail a unique challenge to researchers regarding the classification and construction of race, considering the multiple paradoxes of Muslim and Middle Eastern immigrant identities.11 Relatedly, because most studies did not compare Muslim individuals with non-Latino Whites, health disparities are poorly understood. This is a noteworthy limitation because, as previously noted, many Muslims are categorized as being racially White.11 Including a Middle Eastern and North African racial category would allow researchers, at the very least, to consider if that identity affects health.
Including measures that capture the diversity of experiences among Muslims will allow health researchers to explore many unanswered questions. For example, to what extent does the relationship differ by the level of one’s “Whiteness” or Muslim-like appearance? Specifically, a study could examine the experiences and outcomes between women who do and do not wear hijabs (traditional religious head covering). Moreover, does the relationship differ between men and women, and if so, how? These omissions may affect individual vulnerability to discrimination (i.e., by appearing more or less Muslim) or affect what he or she attributes ambiguous experiences of discrimination to (e.g., their ethnicity, nativity, country of origin). Among immigrants, is there a difference by age at migration? How do these relationships vary between immigrants and refugees? In sum, our ability to understand the impacts of discrimination remains greatly hindered.
Need for Validated Measures
The field can greatly benefit from the development and application of discrimination measures that are developed and validated for use among Muslim populations. Only 1 measure of religious discrimination in health care has been developed for use among Muslims.61 A Perceived Islamophobia Scale has been validated across different Muslim groups in Europe and could be validated and used in other settings for health research.72 We found that a majority of studies in this review adopted existing measures, and sometimes evaluated their psychometric properties among their samples.31,68 For, example, Hassouneh and Kulwicki35 showed that several measures of mental illness (Beck Depression Inventory and the Center for Epidemiological Studies Depression Scale) had high Cronbach α scores, suggesting high internal consistency and providing evidence that these measures may be used among Arab Americans. Relatedly, more objective measures of health outcomes (e.g., biomarkers) can circumvent the problems with validation of self-reported instruments.
Although most studies undertook a quantitative approach, several studies included qualitative or mixed methods approaches. Thus, the context in which discrimination and Islamophobia occurred could be better understood. However, with the qualitative studies, the specific way of measuring or probing for discrimination was not described in detail, making it harder to reproduce these findings. Relatedly, it is possible to expect discrimination to be a topic of discussion in interviews, but not have it arise because researchers do not specifically probe for it.
Methodological Concerns
The present review also highlighted several important methodological and conceptual shortcomings. First, many of the studies relied on nonprobability and cross-sectional study design, which hinders the ability to draw conclusions about the impact of Islamophobia. Future studies must adopt more rigorous designs, including adopting probability samples, using longitudinal data, and using qualitative research to better understand more implicit experiences of discrimination. Multilevel and longitudinal designs are some of the ways researchers can capture structural changes in the sociopolitical climate.
Second, because many studies relied on limited or nonprobabilistic samples, there were concerns about generalizability. Most of the evidence presented in this review relied on small samples yielded primarily from convenience or snowball designs of specific populations, further limiting the representativeness of the findings for the general population. Few studies used nationally representative probability samples that would bolster generalizability. Instead, studies were limited to specific geographic areas, particularly the Detroit and Chicago areas, thereby undermining our ability to understand this phenomenon on a global level.
Third, because studies focused on limited geographic regions, we do not know if the health impact of Islamophobia operates the same way across geopolitical contexts. Future work should consider the role of geography, urbanicity, socioeconomic status, and neighborhoods. Muslims live in both rural and urban areas. Although there is scholarship on how particular cities shape Muslim experiences,8,73 the health impact of Islamophobia may also vary greatly by neighborhood and by a community’s socioeconomic context. Transnational studies should compare experiences of Muslims across countries. Comparative studies between North America and Europe can help determine if differences in national-level structural factors such as immigration policies, media coverage, and access to health care alter the deleterious health impact of Islamophobia on individuals. Future studies that incorporate such structural factors can guide the development of more refined theoretical frameworks for understanding discrimination for racialized religious groups and facilitate analytic approaches that include moderators, mediators, and appropriate comparison groups.
This review is subject to some limitations. Delineating the search parameters is challenging because the racialization of religion makes it hard to define Muslims and Muslim-like groups who experience Islamophobia. Even after we fully reviewed the search articles, it was difficult to capture how Islamophobia intersects with other experiences of discrimination. Although much of this area of health research is new and developing, this review systematically captures what may be Islamophobia for groups that are likely to experience it. Finally, given the quality of the reviewed articles, more methodologically rigorous studies of Islamophobia and health are needed.
Despite these limitations, capturing all the existing literature on Islamophobia and health is a crucial step in making advances in research on racism, racialization of religion, discrimination, and health. This review provides an analysis of studies assessing the relationship between Islamophobia and health, serving as a resource to researchers, practitioners, and policymakers to shape directions for future research, policies, and programmatic efforts. Addressing the discrimination-related poor health that Muslims and racialized Muslim-like subgroups experience is central to the goals of health equity and assurance of the fundamental right to health.
ACKNOWLEDGMENTS
G. Samari was supported by a Eunice Kennedy Shriver National Institute of Child Health & Human Development training grant at the University of Texas at Austin (T32HD007081) and the Population Research Center at the University of Texas at Austin (R24HD041022). M. Z. Sharif was supported by the Health Resources and Services Administration Leadership Education in Neurodevelopmental and Related Disorders Training Program (T73MC30114) and Maternal and Child Health Bureau (T16MC06956).
Note. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
HUMAN PARTICIPANT PROTECTION
Institutional review board approval is not required as this is a systematic literature review of existing studies.
Footnotes
See also Levin and Idler, p. 718.
REFERENCES
- 1.Kishi K. Assaults against Muslims in US surpass 2001 level. Pew Research Center. November 15, 2017. Available at: http://www.pewresearch.org/fact-tank/2017/11/15/assaults-against-muslims-in-u-s-surpass-2001-level. Accessed February 12, 2018.
- 2.Federal Bureau of Investigation. Uniform Crime Report: Hate Crime Statistics, 2016. Available at: https://ucr.fbi.gov/hate-crime/2016/resource-pages/hate-crime-2016-_summary. Accessed February 12, 2018.
- 3.Levin B, Grisham K. Hate crime in the United States: 20 state compilation of official data. Center for the Study of Hate & Extremism at California State University, San Bernardino. 2016. Available at: https://csbs.csusb.edu/hate-and-extremism-center/data-reports/original-reports-hate-and-terrorism-center-staff. Accessed February 12, 2018.
- 4.Lipka M. Muslims and Islam: key findings in the US and around the world. Pew Research Center. 2015. Available at: http://www.pewresearch.org/fact-tank/2017/08/09/muslims-and-islam-key-findings-in-the-u-s-and-around-the-world. Accessed February 12, 2018.
- 5.Samari G. Islamophobia and public health in the United States. Am J Public Health. 2016;106(11):1920–1925. doi: 10.2105/AJPH.2016.303374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gottschalk P, Greenberg G. Islamophobia: Making Muslims the Enemy. Lanham, MD: Rowman & Littlefield; 2008. [Google Scholar]
- 7.Weller P. Addressing religious discrimination and Islamophobia: Muslims and liberal democracies. The case of the United Kingdom. J Islamic Stud. 2006;17(3):295–325. [Google Scholar]
- 8.Ewing KP. Being and Belonging: Muslims in the United States Since 9/11. New York, NY: Russell Sage Foundation; 2008. [Google Scholar]
- 9.The Pew Research Center. US Muslims concerned about their place in society, but continue to believe in the American dream: findings from Pew Research Center’s 2017 survey of US Muslims. 2017. Available at: http://www.pewforum.org/2017/07/26/findings-from-pew-research-centers-2017-survey-of-us-muslims. Accessed November 18, 2017.
- 10.Rana J. The story of Islamophobia. Souls. 2007;9(2):148–161. [Google Scholar]
- 11.Naber N. Ambiguous insiders: an investigation of Arab American invisibility. Ethn Racial Stud. 2010;23(1):37–61. [Google Scholar]
- 12.Williams DR, Mohammed SA. Discrimination and racial disparities in health: evidence and needed research. J Behav Med. 2009;32(1):20–47. doi: 10.1007/s10865-008-9185-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gee GC, Ford CL. Structural racism and health inequities: old issues, new directions. Du Bois Rev. 2011;8(1):115–132. doi: 10.1017/S1742058X11000130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hatzenbuehler ML, Phelan JC, Link BG. Stigma as a fundamental cause of population health inequalities. Am J Public Health. 2013;103(5):813–821. doi: 10.2105/AJPH.2012.301069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pascoe EA, Smart Richman L. Perceived discrimination and health: a meta-analytic review. Psychol Bull. 2009;135(4):531–554. doi: 10.1037/a0016059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gee GC, Spencer MS, Chen J, Takeuchi D. A nationwide study of discrimination and chronic health conditions among Asian Americans. Am J Public Health. 2007;97(7):1275–1282. doi: 10.2105/AJPH.2006.091827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Abdulrahim S, James SA, Yamout R, Baker W. Discrimination and psychological distress: does whiteness matter for Arab Americans? Soc Sci Med. 2012;75(12):2116–2123. doi: 10.1016/j.socscimed.2012.07.030. [DOI] [PubMed] [Google Scholar]
- 18.Moher D, Shamseer L, Clarke M et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Abdulrahim S, Ajrouch K. Social and cultural meanings of self-rated health: Arab immigrants in the United States. Qual Health Res. 2010;20(9):1229–1240. doi: 10.1177/1049732310371104. [DOI] [PubMed] [Google Scholar]
- 20.Abu-Ras W, Abu-Bader SH. The impact of the September 11, 2001, attacks on the well-being of Arab Americans in New York City. J Muslim Ment Health. 2008;3(2):217–239. [Google Scholar]
- 21.Ahmed SR, Kia-Keating M, Tsai KH. A structural model of racial discrimination, acculturative stress, and cultural resources among Arab American adolescents. Am J Community Psychol. 2011;48(3–4):181–192. doi: 10.1007/s10464-011-9424-3. [DOI] [PubMed] [Google Scholar]
- 22.Alcalá HE, Sharif MZ, Samari G. Social determinants of health, violent radicalization, and terrorism: a public health perspective. Health Equity. 2017;1(1):87–95. doi: 10.1089/heq.2016.0016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Aprahamian M, Kaplan DM, Windham AM, Sutter JA, Visser J. The relationship between acculturation and mental health of Arab Americans. J Ment Health Couns. 2011;33(1):80–92. [Google Scholar]
- 24.Assari S, Lankarani MM. Discrimination and psychological distress: gender differences among Arab Americans. Front Psychiatry. 2017;8:23. doi: 10.3389/fpsyt.2017.00023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bhui KS, Hicks MH, Lashley M, Jones E. A public health approach to understanding and preventing violent radicalization. BMC Med. 2012;10(1):16. doi: 10.1186/1741-7015-10-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bradby H, Varyani M, Oglethorpe R, Raine W, White I, Helen M. British Asian families and the use of child and adolescent mental health services: a qualitative study of a hard to reach group. Soc Sci Med. 2007;65(12):2413–2424. doi: 10.1016/j.socscimed.2007.07.025. [DOI] [PubMed] [Google Scholar]
- 27.Chew-Graham C, Bashir C, Chantler K, Burman E, Batsleer J. South Asian women, psychological distress and self-harm: lessons for primary care trusts. Health Soc Care Community. 2002;10(5):339–347. doi: 10.1046/j.1365-2524.2002.00382.x. [DOI] [PubMed] [Google Scholar]
- 28.Daniel M, Wilbur J. Physical activity among South Asian Indian immigrants: an integrative review. Public Health Nurs. 2011;28(5):389–401. doi: 10.1111/j.1525-1446.2010.00932.x. [DOI] [PubMed] [Google Scholar]
- 29.Daniel M, Wilbur J, Fogg LF, Miller AM. Correlates of lifestyle: physical activity among South Asian Indian immigrants. J Community Health Nurs. 2013;30(4):185–200. doi: 10.1080/07370016.2013.838482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.El-Sayed AM, Galea S. The health of Arab-Americans living in the United States: a systematic review of the literature. BMC Public Health. 2009;9(1):272. doi: 10.1186/1471-2458-9-272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ellis BH, MacDonald HZ, Klunk-Gillis J, Lincoln A, Strunin L, Cabral HJ. Discrimination and mental health among Somali refugee adolescents: the role of acculturation and gender. Am J Orthopsychiatry. 2010;80(4):564–575. doi: 10.1111/j.1939-0025.2010.01061.x. [DOI] [PubMed] [Google Scholar]
- 32.Every D, Perry R. The relationship between perceived religious discrimination and self-esteem for Muslim Australians. Aust J Psychol. 2014;66(4):241–248. [Google Scholar]
- 33.Gee GC, Ponce N. Associations between racial discrimination, limited English proficiency, and health-related quality of life among 6 Asian ethnic groups in California. Am J Public Health. 2010;100(5):888–895. doi: 10.2105/AJPH.2009.178012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hassan G, Rousseau C, Moreau N. Ethnic and religious discrimination: the multifaceted role of religiosity and collective self-esteem. Transcult Psychiatry. 2013;50(4):475–492. doi: 10.1177/1363461513495586. [DOI] [PubMed] [Google Scholar]
- 35.Hassouneh DM, Kulwicki A. Mental health, discrimination, and trauma in Arab Muslim women living in the US: a pilot study. Ment Health Relig Cult. 2007;10(3):257–262. [Google Scholar]
- 36.Hodge DR, Zidan T, Husain A. Modeling the relationships between discrimination, depression, substance use, and spirituality with Muslims in the United States. Soc Work Res. 2015;39(4):223–233. [Google Scholar]
- 37.Hodge DR, Zidan T, Husain A. Depression among Muslims in the United States: examining the role of discrimination and spirituality as risk and protective factors. Soc Work. 2016;61(1):45–52. doi: 10.1093/sw/swv055. [DOI] [PubMed] [Google Scholar]
- 38.Hodge DR, Zidan T, Husain A, Hong PYP. Correlates of self-rated health among Muslims in the United States. Fam Soc. 2015;96(4):284–291. [Google Scholar]
- 39.Ikram UZ, Snijder MB, de Wit MA, Schene AH, Stronks K, Kunst AE. Perceived ethnic discrimination and depressive symptoms: the buffering effects of ethnic identity, religion and ethnic social network. Soc Psychiatry Psychiatr Epidemiol. 2016;51(5):679–688. doi: 10.1007/s00127-016-1186-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ikram UZ, Snijder MB, Fassaert TJ, Schene AH, Kunst AE, Stronks K. The contribution of perceived ethnic discrimination to the prevalence of depression. Eur J Public Health. 2015;25(2):243–248. doi: 10.1093/eurpub/cku180. [DOI] [PubMed] [Google Scholar]
- 41.Inhorn MC. Multiculturalism in Muslim America? The case of health disparities and discrimination in “Arab Detroit,” Michigan. In: Ennaji M, editor. New Horizons of Muslim Diaspora in North America and Europe. New York, NY: Palgrave Macmillan; 2016. pp. 177–187. [Google Scholar]
- 42.Inhorn MC, Serour GI. Islam, medicine, and Arab-Muslim refugee health in America after 9/11. Lancet. 2011;378(9794):935–943. doi: 10.1016/S0140-6736(11)61041-6. [DOI] [PubMed] [Google Scholar]
- 43.Johnston DW, Lordan G. Discrimination makes me sick! An examination of the discrimination–health relationship. J Health Econ. 2012;31(1):99–111. doi: 10.1016/j.jhealeco.2011.12.002. [DOI] [PubMed] [Google Scholar]
- 44.Kai J, Hedges C. Minority ethnic community participation in needs assessment and service development in primary care: perceptions of Pakistani and Bangladeshi people about psychological distress. Health Expect. 1999;2(1):7–20. doi: 10.1046/j.1369-6513.1999.00033.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Laird LD, Amer MM, Barnett ED, Barnes LL. Muslim patients and health disparities in the UK and the US. Arch Dis Child. 2007;92(10):922–926. doi: 10.1136/adc.2006.104364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lauderdale DS. Birth outcomes for Arabic-named women in California before and after September 11. Demography. 2006;43(1):185–201. doi: 10.1353/dem.2006.0008. [DOI] [PubMed] [Google Scholar]
- 47.Lindencrona F, Ekblad S, Hauff E. Mental health of recently resettled refugees from the Middle East in Sweden: the impact of pre-resettlement trauma, resettlement stress and capacity to handle stress. Soc Psychiatry Psychiatr Epidemiol. 2008;43(2):121–131. doi: 10.1007/s00127-007-0280-2. [DOI] [PubMed] [Google Scholar]
- 48.Loose F, Tiboulet M, Maisonneuve C, Taillandier-Schmitt A, Dambrun M. Blood pressure and psychological distress among North Africans in France: the role of perceived personal/group discrimination and gender. Am J Hum Biol. 2017;29(5) doi: 10.1002/ajhb.23026. [DOI] [PubMed] [Google Scholar]
- 49.Martin MB. Perceived discrimination of Muslims in health care. J Muslim Ment Health. 2015;9(2):41–69. [Google Scholar]
- 50.Montgomery E. Long-term effects of organized violence on young Middle Eastern refugees’ mental health. Soc Sci Med. 2008;67(10):1596–1603. doi: 10.1016/j.socscimed.2008.07.020. [DOI] [PubMed] [Google Scholar]
- 51.Montgomery E, Foldspang A. Discrimination, mental problems and social adaptation in young refugees. Eur J Public Health. 2008;18(2):156–161. doi: 10.1093/eurpub/ckm073. [DOI] [PubMed] [Google Scholar]
- 52.Moradi B, Hasan NT. Arab American persons’ reported experiences of discrimination and mental health: the mediating role of personal control. J Couns Psychol. 2004;51(4):418–428. [Google Scholar]
- 53.Nadimpalli S, Keita A, Wang J et al. Are experiences of discrimination related to poorer dietary intakes among South Asians in the MASALA Study? J Nutr Educ Behav. 2017;49(10):872–876.e1. doi: 10.1016/j.jneb.2017.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Nadimpalli SB, Dulin-Keita A, Salas C, Kanaya AM, Kandula NR. Associations between discrimination and cardiovascular health among Asian Indians in the United States. J Immigr Minor Health. 2016;18(6):1284–1291. doi: 10.1007/s10903-016-0413-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Nadimpalli SB, Kanaya AM, McDade TW, Kandula NR. Self-reported discrimination and mental health among Asian Indians: cultural beliefs and coping style as moderators. Asian Am J Psychol. 2016;7(3):185–194. doi: 10.1037/aap0000037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Padela A, Raza A. American Muslim health disparities: the state of the MEDLINE literature. J Health Dispar Res Pract. 2015;8(1):1–9. [Google Scholar]
- 57.Padela AI, Heisler M. The association of perceived abuse and discrimination after September 11, 2001, with psychological distress, level of happiness, and health status among Arab Americans. Am J Public Health. 2010;100(2):284–291. doi: 10.2105/AJPH.2009.164954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Padela AI, Murrar S, Adviento B et al. Associations between religion-related factors and breast cancer screening among American Muslims. J Immigr Minor Health. 2015;17(3):660–669. doi: 10.1007/s10903-014-0014-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Padela AI, Peek M, Johnson-Agbakwu CE, Hosseinian Z, Curlin F. Associations between religion-related factors and cervical cancer screening among Muslims in greater Chicago. J Low Genit Tract Dis. 2014;18(4):326–332. doi: 10.1097/LGT.0000000000000026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Reitmanova S, Gustafson DL. “They can’t understand it”: maternity health and care needs of immigrant Muslim women in St. John’s, Newfoundland. Matern Child Health J. 2008;12(1):101–111. doi: 10.1007/s10995-007-0213-4. [DOI] [PubMed] [Google Scholar]
- 61.Rippy AE, Newman E. Perceived religious discrimination and its relationship to anxiety and paranoia among Muslim Americans. J Muslim Ment Health. 2006;1(1):5–20. [Google Scholar]
- 62.Rousseau C, Hassan G, Moreau N, Thombs BD. Perceived discrimination and its association with psychological distress among newly arrived immigrants before and after September 11, 2001. Am J Public Health. 2011;101(5):909–915. doi: 10.2105/AJPH.2009.173062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Sayegh P, Kellough J, Otilingam PG, Poon CYM. South Asian and Middle Eastern American older adults: dementia, mood disorders, and anxiety disorders. Clin Gerontol. 2013;36(3):216–240. [Google Scholar]
- 64.Schmengler H, Ikram UZ, Snijder MB, Kunst AE, Agyemang C. Association of perceived ethnic discrimination with general and abdominal obesity in ethnic minority groups: the HELIUS study. J Epidemiol Community Health. 2017;71(5):453–460. doi: 10.1136/jech-2016-207875. [DOI] [PubMed] [Google Scholar]
- 65.Sheridan LP. Islamophobia pre- and post-September 11th, 2001. J Interpers Violence. 2006;21(3):317–336. doi: 10.1177/0886260505282885. [DOI] [PubMed] [Google Scholar]
- 66.Veenstra G. Mismatched racial identities, colourism, and health in Toronto and Vancouver. Soc. Sci. Med. 2011;73(8):1152–1162. doi: 10.1016/j.socscimed.2011.07.030. [DOI] [PubMed] [Google Scholar]
- 67.Vu M, Azmat A, Radejko T, Padela AI. Predictors of delayed healthcare seeking among American Muslim women. J Womens Health (Larchmt). 2016;25(6):586–593. doi: 10.1089/jwh.2015.5517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Williams ED, Nazroo JY, Kooner JS, Steptoe A. Subgroup differences in psychosocial factors relating to coronary heart disease in the UK South Asian population. J Psychosom Res. 2010;69(4):379–387. doi: 10.1016/j.jpsychores.2010.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Worth A, Irshad T, Bhopal R et al. Vulnerability and access to care for South Asian Sikh and Muslim patients with life limiting illness in Scotland: prospective longitudinal qualitative study. BMJ. 2009;338:b183. doi: 10.1136/bmj.b183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Sterne JA, Hernán MA, Reeves BC et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919. doi: 10.1136/bmj.i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Williams DR, Mohammed SA. Racism and health I: pathways and scientific evidence. Am Behav Sci. 2013;57(8):1152–1173. doi: 10.1177/0002764213487340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Kunst JR, Sam DL, Ulleberg P. Perceived Islamophobia: scale development and validation. Int J Intercult Relat. 2013;37(2):225–237. [Google Scholar]
- 73.Abraham N, Howell S, Shryock A. Arab Detroit 9/11: Life in the Terror Decade. Detroit, MI: Wayne State University Press; 2014. [Google Scholar]