Abstract
Background
Psychosis is among the most disabling complications of Parkinson's disease (PD). The chronicity of PD psychosis remains understudied, and the relative importance of dopaminergic therapy versus the disease process itself in engendering psychosis remains unclear. The objective of this study was to examine pharmacologic and motoric correlates of PD psychosis onset and remission in a longitudinally monitored PD cohort.
Methods
We analyzed data from 165 participants enrolled in a longitudinal PD study through the Morris K. Udall Parkinson's Disease Research Center of Excellence at Johns Hopkins University. Evaluations included formal psychiatric assessment and were conducted at 2‐year intervals. Regression with generalized estimated equations was used to produce unadjusted and adjusted estimates for time‐varying longitudinal associations between psychosis and putative risk factors.
Results
Sixty‐two participants (37.6%) were diagnosed with psychosis during at least 1 evaluation. Of 49 participants with psychosis who were followed over multiple evaluations, 13 (26.5%) demonstrated remission despite a significant increase in Hoehn & Yahr stage (P = 0.009); 2 of these individuals later relapsed. Multivariable regression with generalized estimated equations identified dementia diagnosis, akinesia‐rigidity, anticholinergic usage, and levodopa‐carbidopa dose as significantly associated with psychosis, whereas disease duration was not. A subanalysis of 30 incident psychosis cases suggested that the dopamine agonist dose was lowered after psychosis onset with a compensatory increase in the levodopa‐carbidopa dosage.
Conclusion
The current findings suggest that, in the context of standard therapy, PD‐related psychotic disorder can remit at a frequency of approximately 27%. In addition, akinetic‐rigid motor impairment was more strongly associated with psychosis than disease duration, independent of cognitive impairment and medications.
Keywords: hallucinations, motor subtypes, Parkinson's disease, psychosis, remission
The point‐prevalence of psychosis in patients with Parkinson's disease (PD) is approximately 30%,1 and it is the strongest predictor of nursing home placement in PD.2 The most common PD‐related psychotic symptom is visual hallucinations, which are experienced by 50% of patients at some point during their disease course.3 Even minor psychotic symptoms are strongly predictive of subsequent severe cognitive decline and behavioral disturbances.4 However, the typical course of psychotic phenomenology in PD has only been indirectly or partially addressed, for example, in prospective studies5, 6 with few assessments and follow‐up periods that do not capture the temporal dynamics of the disorder.
Historical accounts from the pre‐levodopa (pre–l‐dopa) era7 suggest that psychosis may be a “natural” component of PD, although it is typically thought to be largely related to dopaminergic medication—especially dopamine agonists.1, 8, 9 However, most cross‐sectional studies have found no link between psychosis and l‐dopa dose, l‐dopa equivalent daily dose (LEDD), or a particular “treatment profile.”1, 10 Changes in pharmacologic management prompted by the onset of psychotic symptoms have not been addressed in the context of longitudinal analyses; this information may help to clarify how methodological differences in prior studies have produced conflicting findings on the relationship between psychosis and medication profile.
Identifying clinical correlates of psychosis that are more specific to the disease process itself may also help formulate more unifying prognostic indicators of vulnerability to psychosis in PD. For example, 1 study11 used cluster analysis to show that hallucinations—measured with a corresponding item in the Unified Parkinson's Disease Rating Scale (UPDRS)—are more common among patients with akinetic‐rigid (AR) than among those with tremor‐dominant (TD) PD.12 However, the majority of patients convert to the AR subtype over time,13 making it unclear how psychotic phenomena relate to AR motor impairment longitudinally, as opposed to overall disease severity and duration. It may be more appropriate to treat AR and TD motor impairment as dimensional traits to differentially relate them to risk for undesirable outcomes like psychosis.14
For the current report, we analyzed patterns in the onset and remission of PD psychosis in 165 patients who were longitudinally assessed approximately every 2 years. Psychiatric diagnoses were guided by the Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM‐IV). In addition, we incorporated a risk‐factor analysis to identify clinical markers of PD psychosis and analyzed medication regimens according to LEDD contribution. Regression analyses were conducted using the generalized estimating equation (GEE) method, which allows for estimates of correlation within subjects; this feature facilitates the analysis of longitudinal repeated‐measures data with time‐varying measures.15 We hypothesized that DSM‐IV psychotic disorder—determined by psychiatrist interview to be directly caused by PD—would be associated over time with increased akinesia‐rigidity, measured according to convention,16 using neurologist‐rated UPDRS‐III (motor examination) scores. We also performed secondary analyses to test the hypothesis that incident psychosis results in reductions of dopaminergic medications.
Patients and Methods
Participants and Study Design
The Morris K. Udall Parkinson's Disease Research Center of Excellence, located at the Johns Hopkins School of Medicine, recruits individuals with PD, patients with related movement disorders, and healthy controls for several research studies. Participants included in this analysis were drawn from the Center's longitudinal study, a PD study that was initiated in 1998 and has enrolled 269 individuals since its inception. Of these 269 participants, 182 have a diagnosis of idiopathic PD according to UK Brain Bank criteria,17 19 have related movement disorders, and 68 are controls. At the time of enrollment and every 2 years thereafter, participants undergo a full psychiatric evaluation per DSM‐IV criteria. These visits also included a neurologist‐conducted UPDRS interview with Hoehn & Yahr stage18 determination and medication list updates.
We aimed to evaluate the longitudinal association between diagnosis of psychosis and medications or motor impairment phenotype. Inclusion criteria for this analysis were a clinical diagnosis of idiopathic PD and complete psychiatric assessment data, UPDRS‐III data, medications, and demographic information. Of the 182 enrolled participants with idiopathic PD, 15 were excluded for incomplete DSM‐IV diagnosis data, 1 was excluded for incomplete Hoehn & Yahr stage and UPDRS‐III data, and 1 was excluded for incomplete medication information. Therefore, 165 patients were included in the present analysis. Patient age was defined as age at enrollment, and disease duration was defined as the time that elapsed between diagnosis date and that evaluation. The LEDD contributed by each medication was calculated for each participant based on their medication lists in accordance with convention.19 Where carbidopa/l‐dopa was prescribed to be used “as needed,” we estimated its LEDD contribution as the midpoint between the typical maximum (3 doses per day) and minimum (0 doses per day) daily values.
Measures
The dependent variable for the present analysis was a diagnosis of psychotic disorder in accordance with DSM‐IV criteria. These criteria require that (1) prominent hallucinations or delusions are present; (2) historical or examination‐based indication that the disturbance is directly related to PD and not medications, alcohol, or substance abuse; (3) the disturbance is not better explained by another mental disorder (eg, major depression with psychosis); and (4) the disturbance does not exclusively occur during the course of delirium.20 The presence of insight is not a part of the diagnostic algorithm.
In total, 17 independent variables were entered into a saturated model for backward stepwise regression, as described below (see Statistical Analysis), including 2 other DSM‐IV diagnoses (dementia and major depression). Neurologist‐rated Hoehn & Yahr stage18 and mean AR and tremor motor impairment scores were included, with the latter calculated from UPDRS‐III motor examination findings as previously described.16 Age, sex, years of adult education, Mini‐Mental State Examination score, and disease duration (defined as the time between PD diagnosis and enrollment in the study) were included. LEDD contributions from l‐dopa/carbidopa formulations (immediate‐release separate from controlled‐release), dopamine agonists, monoamine‐oxidase inhibitors, amantadine, and entacapone were included separately for analyses as continuous variables. Each was divided by 100 for regression to facilitate interpretation of odds ratios (ORs).
Statistical Analysis
Logistic regression with GEE was used to model the longitudinal association between a binary outcome (psychosis diagnosis) and independent variables of interest.15 GEE allows for correlation within subjects to be estimated, facilitating analyses of repeated‐measures longitudinal data.15 In addition, time‐varying changes in the measures of interest over time are captured by GEE. An exchangeable correlation structure was employed in all GEE analyses, and robust parameter estimates are reported to ensure against biased or unstable estimates. The scale parameter was fixed at the default value of 1. The saturated model, as described above (see Measures) was subjected to backward, stepwise variable removal guided by a variant of Akaike's Information Criterion that is compatible with quasi‐likelihood estimation.21 We report ORs with corresponding 95% confidence intervals (CIs) and P values for each GEE model. ORs were calculated as the exponentiated regression coefficients and CI endpoints.
In our secondary analysis, significance estimates were produced using tests appropriate for paired data: the Wilcoxon signed‐rank test was used for continuous and ordinal variables, and McNemar's test was used for count variables. For all statistical tests reported in here, statistical significance was accepted at P < 0.05.
Standard Protocol Approvals, Registrations, and Patient Consents
The Johns Hopkins Institutional Review Board approved the study; participants—and when available, informants—provided written informed consent.
Results
Baseline characteristics for the sample are presented in Table 1. The majority of participants were men (61.8%), and the average age at enrollment (±standard deviation) was 67.9 ± 10.1 years. The mean disease duration was 7.6 ± 5.5 years and ranged from 0.7 to 31.2 years. The duration and frequency of follow‐up psychiatric and neurologic evaluations are presented in Table 2. In total, 111 of 165 participants were evaluated longitudinally (ie, at least once after their baseline assessment) for up to 15 years. The median total follow‐up time for participants who were evaluated longitudinally was 6.1 years (interquartile range, 2.3–8.1 years), and the number of serial evaluations per participant ranged from 2 to 8 evaluations.
Table 1.
Baseline clinical and demographic measures of participants (n = 165)
| Characteristic | Mean ± SD [range] |
|---|---|
| Age at enrollment, y | 67.9 ± 10.1 [42.1–90.6] |
| Age at PD diagnosis, y | 60.3 ± 10.3 [38–86] |
| Disease duration, y | 7.6 ± 5.5 [0.7–31.2] |
| MMSE score | 26.9 ± 3.8 [0–30] |
| Adult education, y | 10.2 ± 4.5 [2–27] |
| Male sex: No. (%) | 102 (61.8) |
| Hoehn & Yahr stage, % | |
| 1 | 7 |
| 1.5 | 4 |
| 2 | 36 |
| 2.5 | 24 |
| 3 | 18 |
| 4 | 8 |
| 5 | 4 |
Abbreviations: SD, standard deviation; PD, Parkinson's disease; MMSE, Mini‐Mental State Examination.
Table 2.
Overview of patient participation and psychosis, depression, and dementia diagnoses throughout longitudinal follow‐up evaluations (n = 165)
| Variable | Statistic |
|---|---|
| Length of follow‐up: Median [IQR/range], ya | 6.1 [2.3–8.1/1.4–14.8] |
| Time between serial evaluations : Median [IQR/range], ya | 2.1 [1.9–2.5/0.9–6.5] |
| No. of serial evaluations, No. of participants | |
| 1 | 54 |
| 2 | 36 |
| 3 | 23 |
| 4 | 26 |
| 5 | 11 |
| 6 | 6 |
| 7 | 7 |
| 8 | 2 |
| Total no. of evaluations included in analysis | 455 |
| Psychosis: No. (%) | |
| Baseline prevalenceb | 32 (19.4) |
| Incidence during follow‐upc | 30 |
| Unique cases followed over multiple evaluations | 49 |
| Remissiond | |
| Without detected relapse | 11 |
| With later detected relapse | 2 |
| Persistent cases | 24 |
| Persistence duration: Median [IQR/range], y | 2.1 [1.9–4.1/1.2–10.4] |
| Total evaluations with psychosis present | 101 (22.2) |
Abbreviations: IQR, interquartile range.
Length of follow‐up and average time between evaluations were calculated only for patients who had at least 2 serial observations (n = 111).
Baseline prevalence is the number of unique participants diagnosed with the corresponding psychiatric diagnosis at baseline.
Incidence is the number of unique participants who were diagnosed for the first time at a subsequent visit. The percentage is not provided for incidence because of participant attrition (changing sample size).
Remission indicates cases where a diagnosis was not made for a participant who was diagnosed at a prior evaluation; for which the number of relapsing cases is also provided.
At baseline, the prevalence of psychosis was 19.4% (32 participants). During longitudinal follow‐up, an additional 30 participants were diagnosed with psychosis. Of these 62 unique cases, 24 were persistent (ie, present at multiple consecutive evaluations). This persistence ranged from 1.2 to 10.4 years. We possessed data for multiple evaluations for 49 of these 62 participants; among these 49 individuals, there were 13 instances of remission, suggesting an estimated remission frequency of 26.5% in our cohort. For 9 of the 13 patients who experienced remission, psychosis had been diagnosed only once at the immediately previous evaluation. For the remaining 4 remissions, psychosis had been long‐standing across multiple prior evaluations spanning 1.8 to 6.7 years. Of the 13 patients who experienced remission, 4 were demented, and 4 were receiving antipsychotic medications both before and after remission. Hoehn & Yahr stage significantly progressed despite remission (P = 0.009) from 2.2 ± 0.3 to 3.0 ± 1.1. Notably, 2 participants who were in remission exhibited a relapse of psychosis at a subsequent evaluation. However, for 5 of the 13 patients who experienced remission, we did not have data for an evaluation after remission due to participant attrition.
A diagnosis of psychosis was made at 101 of the 455 total evaluations included in our analysis. Backward stepwise regression produced a final model that included the variables listed in Table 3. Unadjusted and adjusted ORs, 95% confidence intervals, and significance measures are provided for each of these variables. Results from the multivariable model demonstrate that the presence of psychosis was associated with dementia, higher AR scores, higher l‐dopa/carbidopa dose (immediate‐release and controlled‐release separately), and anticholinergic medication usage for overactive bladder. Notably, disease duration and depression were significantly associated with psychosis only in univariable analysis. A higher dopamine agonist LEDD was significantly associated with a lower likelihood of psychosis in univariable, but not multivariable, regression. To visually represent the strength of the relationship between psychosis and AR score, we graphed a binomial logistic regression model (Fig. 1). We included only baseline evaluations (n = 165) for this model, which was not produced using GEE.
Table 3.
Logistic regression with generalized estimated equations for stepwise‐selected variables associated with psychosis
| Independent variable | Univariable | Multivariable | ||
|---|---|---|---|---|
| OR (95% CI), unadjusted | P value | OR (95% CI), adjusted | P value | |
| Dementia | 6.84 (3.86–12.11) | <0.001a | 3.13 (1.71–5.70) | <0.001a |
| Mean akinetic‐rigid score | 3.15 (2.14–4.64) | <0.001a | 2.38 (1.48–3.83) | <0.001a |
| Immediate‐release l‐dopa‐carbidopa LEDD, mg/d | 1.17 (1.10–1.23) | <0.001a | 1.16 (1.08–1.26) | <0.001a |
| Anticholinergic medication usage | 2.25 (1.204.24) | 0.012c | 2.83 (1.43–5.59) | 0.003b |
| Controlled‐release l‐dopa‐carbidopa LEDD, mg/d | 1.02 (0.95–1.10) | 0.530 | 1.09 (1.00–1.19) | 0.040c |
| Disease duration, y | 1.13 (1.07–1.18) | <0.001a | 1.04 (0.99–1.10) | 0.140 |
| Dopamine agonist LEDD, mg/d | 0.73 (0.60–0.89) | 0.002b | 0.86 (0.71–1.04) | 0.110 |
| Mean tremor score | 1.30 (0.86–1.95) | 0.210 | 0.67 (0.40–1.11) | 0.121 |
| Depression | 1.96 (1.18–3.26) | 0.009b | 1.50 (0.81–2.78) | 0.198 |
Abbreviations: OR, odds ratio; CI, confidence interval; LEDD, l‐dopa equivalent daily dosage; All LEDD variables were divided by 100 to facilitate OR interpretation.
P < 0.001.
P < 0.01.
P < 0.05.
Figure 1.
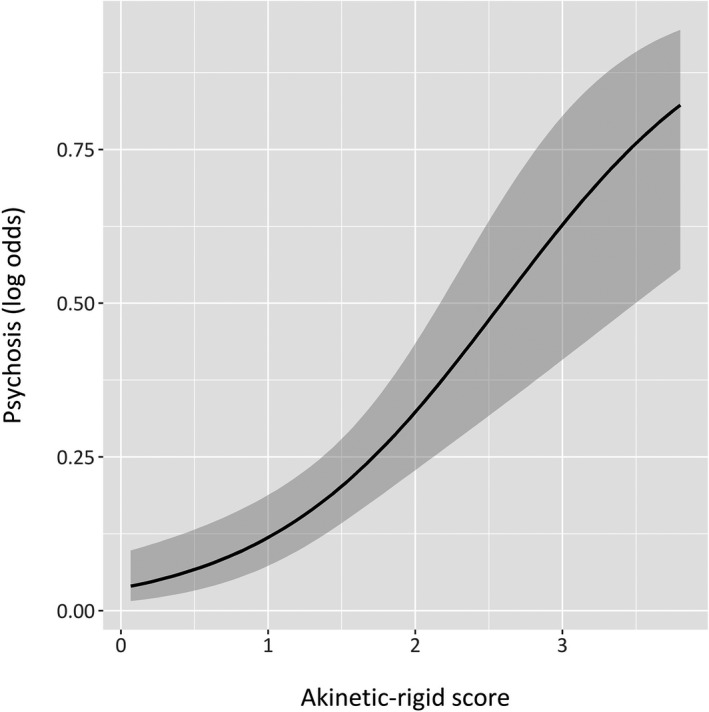
The odds of psychosis are proportional to the mean akinetic‐rigid score. We modeled psychosis as dependent on akinetic‐rigidity scores for the 165 participants in our longitudinal study at baseline. A binomial logistic regression model and smoothing function for binary outcomes were used to produce this graphic. Shaded regions surrounding the curve represent bounds of the 95% confidence interval.
To further characterize correlates of psychosis onset, we conducted a secondary analysis of 30 participants who had incident psychosis during follow‐up (Table 4). Our criteria for inclusion in this analysis were 2 consecutive evaluations in which a psychosis diagnosis was absent in the first but present in the second. We compared the characteristics of this sample before and after psychosis diagnosis. This comparison demonstrated an increased arithmetic difference between carbidopa/l‐dopa immediate‐release LEDD and dopamine agonist LEDD (P = 0.044) but a comparable arithmetic sum of these LEDD values across the consecutive evaluations, suggesting that an increase in l‐dopa dose compensated for the decrease in dopamine agonist dose. The mean AR score was significantly higher after psychosis diagnosis (P = 0.007). We also tested this using the conventional motor subtype approach, which showed that significantly greater numbers of participants were classified with AR disease after psychosis diagnosis (P < 0.001). In addition, Mini‐Mental State Examination scores decreased (P = 0.002), and a significant proportion of participants converted to dementia (P < 0.001). Finally, both anticholinergic medication (P < 0.001) and antipsychotic medication use (P = 0.025) were increased at psychosis diagnosis. Quetiapine (9 participants), clozapine (2 participants), and olanzapine (1 participant) were the antipsychotic medications used by these participants, with daily dosage ranges from 25 to 200 mg, from 25 to 37.5 mg, and 10 mg, respectively. No study participants were using a typical antipsychotic.
Table 4.
Correlates of psychosis onset (n = 30)
| Variable | Mean (95% CI)a | P value | |
|---|---|---|---|
| Pre‐psychosis | Diagnosis of psychosis and later | ||
| LEDD: (l‐dopa IR) − (DA agonist) | 299 [115–483] | 513 [372–653] | 0.044d |
| LEDD: (l‐dopa IR) + (DA agonist) | 738 [600–876] | 752 [579–926] | 0.994 |
| MMSE score | 26.9 [25.7–28.1] | 24.4 [22.2–26.6] | 0.002c |
| Mean akinetic‐rigid motor score | 1.2 [0.9–1.4] | 1.6 [1.2–1.9] | 0.007c |
| Hoehn & Yahr stage | <0.001b | ||
| 1 | 0 | 0 | |
| 1.5 | 0 | 0 | |
| 2 | 18 (60%) | 9 (30%) | |
| 2.5 | 5 (17%) | 5 (17%) | |
| 3 | 4 (13%) | 2 (7%) | |
| 4 | 2 (7%) | 8 (27%) | |
| 5 | 1 (3%) | 6 (20%) | |
| Dementia: No. (%) | 2 (6.7) | +16/−0 | <0.001b |
| Akinetic‐rigid motor subtype: No. (%) | 23 (76.7) | +7/−1 | <0.001b |
| Depression: No. (%) | 14 (46.7) | +5/−2 | 1.000 |
| Anticholinergic medication: No. (%) | 2 (6.7) | +4/−1 | <0.001b |
| Antipsychotic medication: No. (%) | 3 (10) | +11/−2 | 0.025d |
Abbreviations: CI, confidence interval; DA, dopamine; IR, immediate release; LEDD, l‐dopa‐equivalent daily dose; MMSE, Mini‐Mental State Examination.
Mean group values are provided for continuous variables with 95% CIs in brackets. “Pre‐psychosis” refers to the evaluation in which a diagnosis of psychotic disorder was not made; and “post‐psychosis” refers to the subsequent evaluation in which psychosis was present. The median length of the intervals between these evaluations was 2.2 years, with an interquartile range of 2.0 to 2.6 years (the full range was from 0.9 to 6.5 years). For count variables at diagnosis, the number of new positive cases/medication users (+) is compared with the number of patients who discontinued the corresponding medication or who carried the corresponding diagnosis at the pre‐psychosis evaluation but not at the time of psychosis (−). Significance estimates were produced using tests appropriate for paired data: the Wilcoxon signed‐rank test (continuous and ordinal variables) and the McNemar test (count variables).
P < 0.001.
P < 0.01.
P < 0.05.
Discussion
In this report, we demonstrate that PD psychosis can have an unstable course characterized by remission and relapse. To our knowledge, these temporal dynamics have not been previously characterized. Although a 4‐year prospective study5 showed that remission occurred in 14% of patients who had hallucinations at baseline, our analysis allows for a more temporally encompassing description. In addition, the aforementioned study5 utilized a nonstandard definition of psychosis based on a custom scale and did not describe the use of antipsychotic medications. In our study, 26.5% of the longitudinally monitored participants with DSM‐IV–indicated psychosis exhibited remission; only two of these participants relapsed to psychosis again at a later visit. The true frequencies of remission and relapse potentially may be somewhat higher, because we evaluated participants only at 2‐year intervals, which may have missed relapsing and remitting psychotic states between visits. Importantly, our analysis is the first to utilize a diagnosis of psychotic disorder per DSM‐IV criteria to examine the chronicity of PD psychosis. This remains the gold standard of psychiatric diagnostics and emphasizes the attribution of prominent hallucinations and/or delusions to PD itself as opposed to a transient or apparent medication‐induced phenomenon.
It is noteworthy that the frequency of antipsychotic medication use at the time of psychosis onset was approximately 33%, which might be considered low, although there are two important explanations for this. First, antipsychotic medications are relatively contraindicated in the presence of dementia, which is highly comorbid with psychosis in PD—over one‐half of our patients who had a new‐onset psychosis diagnosis also carried a DSM‐IV dementia diagnosis. Second, given the variable efficacy profile and adverse drug reactions (eg, sedation, motor worsening, granulocytosis, and sialorrhea) carried by even newer atypical antipsychotics,22 both clinicians and patients are often hesitant to initiate antipsychotic treatment until symptoms become psychologically distressing or impair functioning. Even in the absence of comorbid dementia, antipsychotic medications may engender increased mortality risk in PD.23 The potential benefits of starting antipsychotic medication early in PD psychosis remains an area for investigation.
Psychosis is also marked by remission and relapse in other neurodegenerative disorders, such as AD. Psychosis reportedly remits frequently in patients with advanced Alzheimer's disease, but impaired verbal communication and the consequential inability to relate psychotic phenomena complicate the assessment of psychosis in these patients.24, 25 Alternatively, a certain degree of neuronal integrity may be required for psychosis in Alzheimer's disease. A recent study of patients who had dementia with Lewy bodies found that the severity of hallucinations was positively correlated with neuronal density in the stratum griseum superficiale of the superior colliculus.26 This finding lends credulity to the notion that structure‐specific neurodegeneration can effect cessation of psychotic phenomena.27 Notably, among our participants with psychosis remission, there significant Hoehn & Yahr progression still was observed; however, potential pathologic correlates of remission remain in PD.
l‐Dopa/carbidopa dosage was significantly higher among participants with psychosis in our study after adjusting for other factors that might lead to increased medication dosage. Despite the common clinical intuition that high LEDD can induce psychosis, studies examining this relationship have not consistently produced evidence for this hypothesis.1 Our secondary analyses among incident psychosis cases suggests that dopamine agonists were decreased or removed and replaced with carbidopa/l‐dopa, which is believed to be less hallucinogenic. However, we also noted a significant association between anticholinergic medications and psychosis in both our multivariable and secondary psychosis onset analyses. Cholinergic deficits in PD are thought to increase the likelihood of psychosis, which often dictates a change in the use of anticholinergics.8, 28 The participants in our study who had new‐onset psychosis were taking oxybutynin (4 participants) or tolterodine (1 participant). Among all participants with psychosis, these 2 medications were the most common anticholinergics used. It is unclear why their use was continued in the presence of psychotic symptoms, because medication regimens were not under the control of study investigators.
Limitations of our study design include variability in the consistency of participant follow‐up and attrition. Variability in the time separating serial evaluations was not dramatic, with a median of 2.1 years (interquartile range, 1.9–2.5 years). GEE models are considered flexible enough to remain robust, even when measures are not equally spaced in time.15 In addition, GEE permits for changing outcome values to be representatively related to changes in independent variables, suggesting that the remission and relapse recorded in our study are not statistically concerning.15 For our analysis, we used a binary outcome to represent the presence or absence of psychosis, which may be objectionable, because psychotic symptoms exist on a clinical continuum of severity in PD. The DSM‐IV criteria for psychotic disorder require prominent hallucinations or delusions, which makes our findings less generalizable to patients who have minor illusions/hallucinations. Importantly, these criteria do exclude cases of apparently medication‐induced symptoms, such as hallucinosis that began soon after initiating a dopamine agonist, which may partly explain the negative association noted between dopamine agonist use and psychosis. This exclusion may reduce the remission rate observed, because drug‐induced hallucinosis would be expected to remit after adjusting the therapeutic regimen, which was not under the control of the study investigators but, rather, was controlled by participants’ individual clinicians. The psychiatric diagnoses themselves were made based on the clinical discretion and expertise of psychiatrists participating in the research effort, but we lack detailed data for the basis on which those decisions were made (eg, types of hallucinations or delusions). In other words, 27% of patients who have PD psychosis not attributable to hallucinogenic medication exposure would be expected to remit, acknowledging the difficulty in determining the medication relatedness of psychosis. Another limitation of our approach is that we did not have data on the duration of dopamine replacement therapy in our patients, which could be important given the putative role of medications in precipitating psychosis. However, it seems reasonable to assume that most individuals with PD begin treatment soon after diagnosis, which we used as the starting time‐point for disease duration. Finally, because psychosis is associated with advanced disease and dementia, high attrition among these cases in a longitudinal study is expected. This is demonstrated by our lack of follow‐up data for several participants who exhibited remission.
Conclusion
In this report, we identify psychotic remission and relapse as important possibilities in the typical course of PD. This may have importance for our understanding of disease progression and underlying pathology. We also provide novel evidence that the inconsistently noted associations between LEDD and psychosis in PD may be due to changes in specific treatment strategy rather than changes in total dopamine equivalents. Finally, we show that akinesia‐rigidity is a stronger independent marker of psychosis likelihood than disease duration in multivariable regression. Assuming a fundamentally dopaminergic etiology of PD psychosis, this finding is consistent with the generally accepted notion that AR patients exhibit more severe dopaminergic dysfunction and disease severity.29 Given the incredibly heterogeneous nature of PD,12 utilizing akinesia‐rigidity and tremor as dimensional traits may facilitate refinements in our understanding of how they relate to associated non‐motor comorbidities.
Author Roles
1. Research Project: A. Conception, B. Organization, C. Execution; 2. Statistical Analysis: A. Design, B. Execution, C. Review and Critique; 3. Manuscript Preparation: A. Writing the First Draft, B. Review and Critique.
J.T.H.: 2A, 2B, 3A
K.P.: 2C, 3B
C.C.B.: 1B, 1C, 3B
M.P.G.B.: 3B
K.C.: 3B
T.M.D.: 1A, 1B, 3B
V.J.: 1C, 3B
Z.M.: 3B
C.L.M.: 3B
K.A.M.: 2C, 3B
A.P.: 1C, 3B
O.P.: 1C
L.S.R.: 1A, 1B, 1C, 3B
M.D.S.: 3B
D.A.S.: 3B
J.C.T.:1C
J.W.: 2A, 2C, 3B
G.M.P.: 1A, 1B; 2C; 3B
Disclosures
Ethical Compliance Statement: We confirm that we have read the Journal's position on issues involved in ethical publication and affirm that this work is consistent with those guidelines.
Funding Sources and Conflict of Interest: This study was supported by grants from the National Institutes of Health (NIH)/National Institute of Neurological Disorders and Stroke (NINDS) (P50 NS38377 to T.M.D.), the NIH/National Institute on Aging (K23 AG044441 to G.M.P.), the NIH/National Institute of General Medical Sciences (NIGMS) (5 T32 GM007309 to J.T.H. and D.A.S.), the NIH/National Eye Institute (P30 EY01765 to J.W.), and the NIH (1U54RR023561‐01A1 to J.W.).
Financial Disclosures (past 12 months): Jared T. Hinkle is supported by the Medical Scientist Training Program at the Johns Hopkins School of Medicine (NIH/NIGMS 5 T32 GM007309). Catherine C. Bakker is supported by the NIH/National Institute of Neurological Disorders and Stroke (P50 NS38377). Ted M. Dawson acknowledges support from the Adrienne Helis Malvin and Diana Henry Helis Medical Research Foundations and their research partnership with The Johns Hopkins Hospital, The Johns Hopkins University School of Medicine, and the Foundation's Parkinson's Disease Programs; he is supported by NIH/NINDS P50NS038377, NIH/NINDS U01NS082133, NIH/NINDS R37NS067525, NIH/National Institute on Drug Abuse P50 DA00266, the JPB Foundation; Dr. Dawson is the Leonard and Madlyn Abramson Professor in Neurodegenerative Diseases, chair of the Dystonia Prize committee of the Bachmann Strauss Dystonia and Parkinson's Disease Foundation and the Michael J. Fox Foundation; he is on the Board of Directors of the Bachmann Strauss Dystonia and Parkinson's Disease Foundation, is on the Scientific Advisory Board of CurePSP, and is a member of the American Gene Technologies International Inc. advisory board (the terms of this arrangement are being managed by The Johns Hopkins University in accordance with its conflict of interest policies); in addition, Dr. Dawson is a founder of Valted, LLC, and holds an ownership equity interest in the company (this arrangement has been reviewed and approved by the Johns Hopkins University in accordance with its conflict of interest policies). Vanessa Johnson is supported by the NIH/NINDS (P50 NS38377). Zoltan Mari is supported by the National Parkinson's Foundation with a Center of Excellence Grant and is supported by the NIH/NINDS (U01 NS082133); he is a founder of Neuraly, Inc., and holds ownership equity interest in the company (this arrangement has been reviewed and approved by Johns Hopkins University to be in accordance with its conflict of interest policies). Cherie L. Marvel is supported by the NIH/National Institute on Drug Abuse (R01 DA041264), The Margaret Q. Landenberger Research Foundation, and the Marilyn and Edward Macklin Foundation. Kelly A. Mills receives salary support through the NIH National Center for Advancing Translational Sciences (KL2TR001077; principal investigator, Daniel Ford) and has received funding from Northwestern University. Alexander Pantelyat is supported for this project by the NIH/NINDS (U01 NS082133 and P50 NS38377). Olga Pletnikova receives funding from the NIH through the National Institute on Aging (U19AG033655, P50AG005146), through NINDS (P50NS38377), and from the NIH (R01MH096636, R01NS086074); she receives support from an NIH subcontract with Emory University (U01AG046161), and she also receives funding through the BrightFocus Foundation. Liana S. Rosenthal has received support from the NIH/NINDS (P50NS038377), the Marilyn and Edward Macklin Foundation, and the Michael J. Fox Foundation; she also received an honorarium from the Edmond J. Safra Foundation and Functional Neuromodulation. Daniel A. Stevens is supported by the Medical Scientist Training Program at the Johns Hopkins School of Medicine (NIH/NIGMS 5 T32 GM007309). Juan C. Troncoso receives funding from the NIH through the National Institute on Aging (U19AG033655, P50AG005146), through NINDS (P50NS38377, R25NS079185), and from the NIH (R01MH096636, R01NS086074); he also receives support from an NIH subcontract with Emory University (U01AG046161), funding through the BrightFocus Foundation, and NIH funding through collaborations (RO1NS086888, R01HL091541). Jiangxia Wang receives salary support through the Wilmer Ophthalmological Institute Core Grant (NIH/National Eye Institute P30 EY01765) and the Institute for Clinical and Translational Science Award (NIH 1U54RR023561‐01A1). Gregory M. Pontone receives funding through the NIH/National Institute on Aging as part of a K23 award (AG044441‐01A1) He is also co‐sponsored by Acadia Pharmaceuticals, Inc., for writing a book on psychosis in Parkinson's that was co‐written by the National Parkinson's Foundation. The remaining authors made no disclosures.
Relevant disclosures and conflicts of interest are listed at the end of this article.
References
- 1. Fenelon G, Alves G. Epidemiology of psychosis in Parkinson's disease. J Neurol Sci 2009;289:12–17. [DOI] [PubMed] [Google Scholar]
- 2. Aarsland D, Larsen JP, Tandberg E, Laake K. Predictors of nursing home placement in Parkinson's disease: a population‐based, prospective study. J Am Geriatr Soc 2000;48:938–942. [DOI] [PubMed] [Google Scholar]
- 3. Williams DR, Lees AJ. Visual hallucinations in the diagnosis of idiopathic Parkinson's disease: a retrospective autopsy study. Lancet Neurol 2005;4:605–610. [DOI] [PubMed] [Google Scholar]
- 4. Goetz CG, Fan W, Leurgans S, Bernard B, Stebbins GT. The malignant course of “benign hallucinations” in Parkinson disease. Arch Neurol 2006;63:713–716. [DOI] [PubMed] [Google Scholar]
- 5. Goetz CG, Leurgans S, Pappert EJ, Raman R, Stemer AB. Prospective longitudinal assessment of hallucinations in Parkinson's disease. Neurology 2001;57:2078–2082. [DOI] [PubMed] [Google Scholar]
- 6. Holroyd S, Currie L, Wooten GF. Prospective study of hallucinations and delusions in Parkinson's disease. J Neurol Neurosurg Psychiatry 2001;70:734–738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Fenelon G, Goetz CG, Karenberg A. Hallucinations in Parkinson disease in the prelevodopa era. Neurology 2006;66:93–98. [DOI] [PubMed] [Google Scholar]
- 8. Poewe W. When a Parkinson's disease patient starts to hallucinate. Pract Neurol 2008;8:238–241. [DOI] [PubMed] [Google Scholar]
- 9. Stowe R, Ives N, Ce C, et al. Dopamine agonist therapy in early Parkinson's disease. Cochrane Database Syst Rev 2008;2:1–3. [DOI] [PubMed] [Google Scholar]
- 10. De Deurwaerdere P, Di Giovanni G, Millan MJ. Expanding the repertoire of L‐DOPA's actions: a comprehensive review of its functional neurochemistry. Prog Neurobiol 2017;151:57–100. [DOI] [PubMed] [Google Scholar]
- 11. Reijnders JS, Ehrt U, Lousberg R, Aarsland D, Leentjens AF. The association between motor subtypes and psychopathology in Parkinson's disease. Parkinsonism Relat Disord 2009;15:379–382. [DOI] [PubMed] [Google Scholar]
- 12. Von Coelln R, Shulman LM. Clinical subtypes and genetic heterogeneity: of lumping and splitting in Parkinson disease. Curr Opin Neurol 2016;29:727–734. [DOI] [PubMed] [Google Scholar]
- 13. Alves G, Larsen JP, Emre M, Wentzel‐Larsen T, Aarsland D. Changes in motor subtype and risk for incident dementia in Parkinson's disease. Mov Disord 2006;21:1123–1130. [DOI] [PubMed] [Google Scholar]
- 14. Kotagal V. Is PIGD a legitimate motor subtype in Parkinson disease? Ann Clin Transl Neurol 2016;3:473–477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Locascio JJ, Atri A. An overview of longitudinal data analysis methods for neurological research. Dement Geriatr Cogn Dis Extra 2011;1:330–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kang G, Bronstein JM, Masterman DL, Redelings M, Crum J, Ritz B. Clinical characteristics in early Parkinson's disease in a central California population‐based study. Mov Disord 2005;20:1133–1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hughes AJ, Daniel SE, Kilford L, Lees AJ. Accuracy of clinical diagnosis of idiopathic Parkinson's disease: a clinico‐pathological study of 100 cases. J Neurol Neurosurg Psychiatry 1992;55:181–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hoehn MM, Yahr MD. Parkinsonism: onset, progression, and mortality. Neurology 1967;17:427–442. [DOI] [PubMed] [Google Scholar]
- 19. Tomlinson CL, Stowe R, Patel S, Rick C, Gray R, Clarke CE. Systematic review of levodopa dose equivalency reporting in Parkinson's disease. Mov Disord 2010;25:2649–2653. [DOI] [PubMed] [Google Scholar]
- 20. American Psychiatric Association . The Diagnostic and Statistical Manual of Mental Disorders. 4th ed (DSM‐IV). Lake St Louis, MO: American Psychiatric Association; 2000. [Google Scholar]
- 21. Pan W. Akaike's information criterion in generalized estimating equations. Biometrics 2001;57:120–125. [DOI] [PubMed] [Google Scholar]
- 22. Yuan M, Sperry L, Malhado‐Chang N, et al. Atypical antipsychotic therapy in Parkinson's disease psychosis: a retrospective study [serial online]. Brain Behav 2017;7:e00639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Weintraub D, Chiang C, Kim HM, et al. Association of antipsychotic use with mortality risk in patients with Parkinson disease. JAMA Neurol 2016;73:535–541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Jeste DV, Finkel SI. Psychosis of Alzheimer's disease and related dementias. Am J Geriatr Psychiatry 2000;8:29–34. [DOI] [PubMed] [Google Scholar]
- 25. Jeste DV, Wragg RE, Salmon DP, Harris MJ, Thal LJ. Cognitive deficits of patients with Alzheimer's disease with and without delusions. Am J Geriatr Psychiatry 1992;149:184–189. [DOI] [PubMed] [Google Scholar]
- 26. Erskine D, Thomas AJ, Taylor JP, et al. Neuronal loss and α‐synuclein pathology in the superior colliculus and its relationship to visual hallucinations in dementia with Lewy bodies. Am J Geriatr Psychiatry 2017;25:595–604. [DOI] [PubMed] [Google Scholar]
- 27. Hinkle J, Pontone GM. Visual hallucinations in neurodegenerative diseases: focus on selective tissue vulnerability. Am J Geriatr Psychiatry 2017;25:605–606. [DOI] [PubMed] [Google Scholar]
- 28. Hoeh N, Gyulai L, Weintraub D, Streim J. Pharmacologic management of psychosis in the elderly: a critical review. J Geriatr Psychiatry Neurol 2003;16:213–218. [DOI] [PubMed] [Google Scholar]
- 29. Rajput A, Voll A, Rajput M, Robinson C, Rajput A. Course in Parkinson disease subtypes: a 39‐year clinicopathologic study. Neurology 2009;73:206–212. [DOI] [PubMed] [Google Scholar]


