Abstract
Introduction
For many people with alcohol use disorders, alcohol drinking is a highly ingrained and automatized behavior with negative long-term health consequences. Implementation intentions, a behavioral intervention that links high-risk drinking situations with alternative, healthier responses, provide a means to intervene on habitual drinking behaviors. Here, a pilot treatment using implementation intentions was assessed with remote assessments and treatment prompts.
Methods
Treatment-seeking individuals with alcohol use disorder between the ages of 18 and 65 were recruited from the community from October 2014 to November 2016. Participants (N=35) were quasi-randomly assigned to complete either active (n=18) or control (n=17) two-week implementation intention interventions. Active implementation intentions linked high-risk situations with alternative responses whereas the control condition selected situations and responses but did not link these together. Daily ecological momentary interventions of participant-tailored implementation intentions were delivered via text message. Alcohol consumption was assessed once daily with self-reported ecological momentary assessments (EMAs) of drinks consumed the previous day and thrice daily remotely submitted breathalyzer samples to assess reliability of self-reports.
Results
On drinking days (80% of days), the active implementation intentions group reduced alcohol consumption during the intervention period compared to the control condition; however the difference between consumption was not observed at one-month follow-up.
Discussion
The implementation intention intervention was associated with a 1.09 drink per day decrease in alcohol consumption on drinking days compared to a decrease of 0.29 drinks per day in the control condition. Future studies may combine implementation intentions with other treatments to help individuals to reduce alcohol consumption.
Keywords: alcohol use, ecological momentary assessment, ecological momentary intervention, implementation intentions, remote treatment
1. Introduction
Alcohol use disorders are major contributors to morbidity and mortality in the United States and worldwide (Rehm et al., 2009). Treatments to cut back on alcohol use may help to reduce the overall burden of disease such as decreasing risk for several types of cancer, mental health problems, and heart disease (Rehm et al., 2003). One strategy to reduce drinking, called implementation intentions, identifies common antecedents to use and links these to alternative responses that aim to avoid or cope with these situations instead of drinking. Here, a pilot, proof-of-concept trial using ecological momentary assessments (EMAs) and ecological momentary interventions (EMIs) was employed to test the real-world efficacy of individually-tailored implementation intentions on alcohol use.
Proposed by Gollwitzer (1999), implementation intentions aim to decrease the disparity between goal setting and attainment. A prior meta-analysis found that implementation intentions have a medium to large effect size on goal attainment (Gollwitzer & Sheeran, 2006). Implementation intentions first seek to identify a critical risky situation (e.g., attending a party where others are drinking) and then to link them with appropriate responses (e.g., attending meetings with others who are attempting to remain abstinent) using an “if-then” framework.. Implementation intentions increase healthy behaviors (e.g., de Vet, Oenema, & Brug, 2011; Guillaumie, Godin, Manderscheid, Spitz, & Muller, 2012) and accumulating evidence suggests that implementation intentions are also effective in reducing unhealthy behaviors (e.g., Armitage, 2007, 2008, 2016; Sullivan & Rothman, 2008) including alcohol consumption (Armitage, 2009a; Armitage & Arden, 2012; Norman & Wrona-Clarke, 2016).
The implementation intention intervention used in the current study was adapted from the volitional help sheet developed by Armitage and Arden (2012). The active implementation intentions were in the form of if-then statements linking high-risk situations with healthier responses. In contrast, the control implementation intention condition presented the same critical situations and responses but participants choose useful phrases without linking them together in an if-then structure.
Previous studies have found reductions in alcohol use following implementation intention interventions when consumption is assessed retrospectively with the Timeline Followback (TLFB; Armitage & Arden, 2012). However, the TLFB is associated with underreporting of drinking on drinking days, compared to daily EMAs (Carney, Tennen, Affleck, Del Boca, & Kranzler, 1998; Dulin, Alvarado, Fitterling, & Gonzalez, 2017; Searles, Helzer, & Walter, 2000). To increase reliability of amount of drinking on drinking days, daily EMAs were collected. The self-reports of previous day alcohol consumption were complemented by three breathalyzer samples throughout the day. The biologic breath alcohol content (BrAC) samples provide an objective measurement to corroborate the self-report EMAs.
Building on the innovations of EMAs, EMIs have more recently been recommended to provide frequent prompting or cueing of participants outside of the laboratory (Cohn, Hunter-Reel, Hagman, & Mitchell, 2011; Heron & Smyth, 2010). EMIs can be stand alone treatments or treatment boosters that are provided to individuals in real-time and in the real world. For example, one study using EMIs observed reductions in alcohol use following daily text messages encouraging drinking moderation to incoming college students (Riordan, Conner, Flett, & Scarf, 2015). Similarly, in the current study EMIs of participant-tailored active or control implementation intention cues were provided via once-daily text message throughout the intervention period. To reduce barriers to participation and increase external validity of measures, all EMIs and EMAs were remotely delivered and collected, respectively.
This exploratory proof-of-concept study capitalizes on the availability of technological advancements to reduce the burden of treatment for individuals with alcohol use disorders. The current study provides two improvements to build on previous research showing that implementation intentions can help to reduce drinking. First, this study provides technological and assessment advancements to improve accuracy of measurement of alcohol consumption. Second, the frequent remote collection of alcohol consumption provides the ability to disentangle the effect of implementation intentions on two processes associated with alcohol reduction: (1) abstaining from alcohol and (2) reducing amount of alcohol consumption when drinking. The research team hypothesized that active implementation intentions would be associated with a greater reduction in alcohol consumption than control implementation intentions, and that biologic EMAs would corroborate the reliability and consistency of the self-reported EMAs.
2. Methods
Treatment-seeking participants completed either an active or active control implementation intention intervention. From the original sample that completed through the intervention period (n=36), one participant in the control condition was excluded because of a disclosure to research staff that they had provided false responses throughout the study. To gain a representative sample, participants were recruited in a range of social and work settings, including flyers, online advertisements, and referrals in Roanoke, Virginia and surrounding areas. Participants were eligible if they: (a) were between the ages of 18 and 65; (b) met criteria for alcohol use disorder, as defined by two or more symptom criteria based on the DSM-5 (American Psychiatric Association, 2013); and (c) reported a desire to cut down or quit drinking. Individuals who were pregnant or lactating, taking over-the-counter medicines containing alcohol, or had immediate plans to move away from the area were excluded. Additionally, for safety purposes a score of 23 or greater on the Alcohol Withdrawal Symptom Checklist (a score indicative of the requirement for medical oversight during alcohol detoxification, see (Pittman et al., 2007)) was exclusionary to avoid participants cutting down on alcohol use if medical management was likely to be needed. Participants who met this criterion were offered access to medical care in addition to an emergency contact card for local medical facilities.
2.1 Procedures
The Virginia Polytechnic Institute and State University Institutional Review Board approved all methods and protocols in the current study. All participants provided informed consent. The study design was adapted from study procedures proposed by Koffarnus et al. (2015). Participants were invited to attend four sessions, including a baseline (consent), intervention, post-intervention, and 1-month follow-up assessment. Participants were allocated to active (n = 18) or control (n = 17) implementation intention treatment condition. Participants were assigned to groups with a variation of the Frane (1998) procedure wherein new participants were allocated to the group that yielded the least overall significant difference across three preselected variables (i.e. average daily drinking during the baseline period, Treatment Services Review (McLellan, Alterman, Cacciola, Metzger, & O’Brien, 1992) total score, and number of years drinking alcohol) with a 0.8 probability, which left an element of random assignment. Stated differently, each participant had a 20% chance of random assignment and an 80% chance of being allocated to the group that minimized differences across the pre-selected variables.
2.1.1. Baseline period
During a baseline assessment session participants completed the Readiness to Change Questionnaire (Heather, Gold, & Rollnick, 1991) and Alcohol Use Disorder Identification Test (AUDIT; Saunders, Aasland, Babor, de la Fuente, & Grant, 1993).
2.1.1.2. AUDIT
The AUDIT is a 10-item self-report questionnaire developed by the World Health Organization and assesses alcohol use, drinking behaviors, and problems related to alcohol use (Saunders, Aasland, Babor, de La Fuente, & Grant, 1993). AUDIT scores range from 0 to 40 where 0 indicates no alcohol use. AUDIT scores between 8 and 15 indicate medium levels of alcohol problems and scores of 16 and above are associated with high levels of alcohol-related problems.
Following this session, participants were instructed to drink as usual and were prompted via text message to give daily self-reports of previous-day drinking for one week. Participants were provided with verbal instruction as well as a card of standard drink sizes to inform reporting of drinks consumed. If participants did not have a cell phone or did not want to use a personal cell phone, then one was provided for use throughout the study. No intervention was implemented during the baseline period. Reports of alcohol consumption on at least two days of the baseline period were required to continue.
2.1.2. Intervention period
After completion of the baseline period, participants were assigned to a treatment condition, completed the active or active control implementation intentions interventions worksheet, and were asked to try to cut back on drinking over the following two weeks.
2.1.2.1. Implementation intentions
Consistent with implementation intention cues used by Armitage and Arden (2012), the cues were adapted from the transtheoretical model (Procheska & Diclemante, 1983; can be viewed at http://web.uri.edu/cprc/measures/) and are recommended for use in the planning intervention literature (Armitage, 2009b). The implementation intention worksheet was an expanded and adapted volitional help sheet initially adapted from previous work on this topic by Armitage and Arden (2012). The implementation intention worksheet consisted of a list of 24 critical risky situations (e.g., “I am tempted to drink when things are not going my way and I am frustrated”) followed by a list of 24 possible appropriate responses (e.g., “I will stop to think about how my drinking is hurting people around me;” see Supplemental Material 1).
The active group followed an “if-then” format. Participants were asked to pick at least three critical situations where they are tempted to drink and to link them with three appropriate responses that they believe might help reduce drinking by drawing a line between those applicable to them. Following this, they were asked to pick the three linked situations and behaviors that they believed would most helpful to them and write them in sentence form, starting with an “if” in front of the critical situation, and a “then” in front of the response (e.g., “If I am tempted to drink when there are arguments and conflicts, then I will put things around my home that remind me not to drink”).
Consistent with the methods of Armitage and Arden (2012), participants in the control group were asked to check critical situations and responses without connecting or drawing any line between the two. Participants were then asked to pick three of the items they had checked (i.e. critical situations or alternative responses) that they believed would be most helpful to them to help them cut down on drinking and to write in sentence form (e.g., “I will make commitments to myself not to drink”). Note that these control statements were not in the if-then format.
2.1.2.2. Self-reported EMAs
Daily self-reports of previous-day drinking were collected throughout the baseline and intervention period. Participants were compensated $1 that was immediately and electronically transferred to a reloadable debit card (https://greenphire.com/) for providing these daily reports regardless of alcohol consumption during both the baseline and intervention period.
2.1.2.3. Biologic EMAs
During an in-lab session, participants were instructed on how to use the Soberlink breathalyzer device (www.soberlink.net) and selected three daily timepoints for submitting the Soberlink breathalyzer samples over the two-week intervention period, including a morning, afternoon, and evening time point that were spaced at least six hours apart. The 12-hour range of timepoints for breath samples were selected to get an estimation of BrAC throughout the day the corroborate self-reported drinking, while recognizing that drinking may occur outside the scope of breath alcohol detection. This precise fuel cell breathalyzer is compact and photographs the user mid-submission, making it ideal to collect biologic samples while limiting in-person contact during the two-week intervention phase. After each Soberlink submission, the device automatically uploads the breathalyzer results and picture of the user to a centralized, secure website available to research staff. To encourage treatment compliance, participants were compensated $1 for each on-time breathalyzer submissions regardless of BrAC for a maximum of $3 of daily compensation for these samples deposited daily to the participants study debit card.
2.1.2.4. Daily EMIs
Once-daily EMIs were texted to participants at 8 AM throughout the intervention period. The daily EMI was one of the participant’s three selected tailored implementation intention cues (active or control) provided verbatim as the participant wrote the cue during the intervention session. The three selected active or control implementation intention cues were provided one-per-day in randomized order that was assigned at the start of the intervention period.
2.1.3. Post-intervention session
The intervention phase was followed by post-intervention session where participants were compensated $50 for successful return of study materials including the Soberlink device and a study cell phone if used. Participants also completed a brief Treatment Acceptability questionnaire (see supplemental materials).
2.1.4. Follow-up period
Participants were invited back for a one-month follow-up session that could fall anywhere from 3–5 weeks following the completion of the intervention period. During the follow-up session, participants completed a TLFB of daily alcohol consumption since completion of the intervention period (Sobell & Sobell, 1995).
2.2. Statistical Methods
All analyses were done in R version 3.3.2 (R Core Team, 2014). AUDIT scores and demographic characteristics between treatment conditions were compared using two sample t-tests and Chi-square tests for continuous and categorical variables, respectively.
2.2.1. Active implementation intentions compared to control intervention
The effect of implementation intentions on alcohol consumption was evaluated using the daily self-report EMAs as the primary outcome measure. Since alcohol consumption showed many days of zero drinking, a two-step hurdle mixed model was used (Atkins, Baldwin, Zheng, Gallop, & Neighbors, 2013). First, a mixed effects logistic regression was used to model the probability a participant would drink on a given day. Second, a gamma mixed regression was fit to model the number of drinks in a day that a participant consumed given they consumed alcohol. The hurdle mixed model was:
where i is the index of the participant, t is the day in the study, and l and g indicate parameters from the logistic and gamma models, respectively, and p is the proportion of days without drinking. Condition and time point are fixed effects and participant ID is a random effect. One advantage of hurdle models is that they provide a straightforward interpretation as all zero values are modeled solely in the logistic regression component. While the overall fit of hurdle models and zero-inflated models are frequently similar (Madden, 2008), this approach allows for two distributional characteristics to be modeled separately, (1) the probability that an individual will drink or not drink on a given day, and (2) how many drinks an individual will consume if that individual drinks. Note, a zero-inflated poisson regression was not appropriate because on several days and by several participants non-integer values for number of drinks (e.g., 3.5 drinks) were reported. The hurdle model was implemented using the glmmadmb package (Skaug, Nielsen, Magnusson, & Bolker, 2013) which allows for mixed random effects and zero inflation. A binomial distribution was used to model the logistic regression and a Gamma distribution was used with the zero-truncated discrete probability distribution function. Model-adjusted least square means are reported for significant variables in the model.
2.2.2. Correlations between self-report and biologic EMAs
Self-report measurement is subject to uncertain reliability due to participant characteristics. To corroborate the self-report EMAs, the concordance between self-report and biologic EMAs was examined. The reliability of EMAs of daily drinks were verified using Pearson product-moment correlations with the average of the three daily BrAC samples and separately the daily peak daily BrAC sample. Finally, days where participants reported alcohol consumption were separately correlated with the average daily BrAC. An independent-samples t-test of the correlation between self-report and average daily biologic EMAs were then used to compare between treatment conditions to assess for differences in reporting reliability across groups.
2.2.3. Alcohol consumption at one-month follow-up
To look at possible persistence of effects of the intervention on drinking across time points, including at one-month follow- up a mixed model was used. The mixed model adjusted for time point (baseline, intervention, follow-up) and treatment condition (active, control) to assess for changes in average reported drinking (collected using self-reported daily EMAs for baseline and intervention and average daily drinks from the TLFB at follow-up). Overall model effects in addition to model-adjusted means and standard errors are reported.
2.2.4. Treatment acceptability and compliance
Descriptive statistics of treatment acceptability questions are reported for both treatment conditions. Independent samples t-tests were used to compare between treatment groups. The rate of treatment compliance was separately examined as the average percent of self-report and BrAC samples successfully obtained per participant.
3. Results
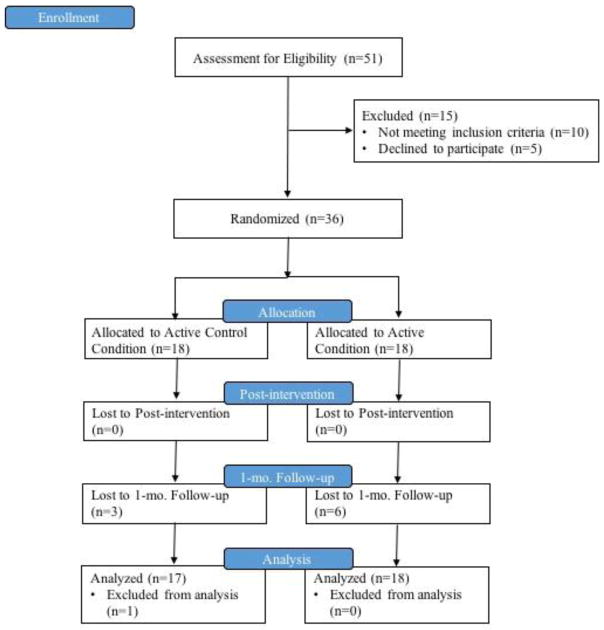
Of the fifteen participants who were screened but not randomized to treatment, two participants did not drink on at least two days during the baseline period, four participants did not return to the lab for the intervention session, four were referred to services because of high alcohol withdrawal scores, and five voluntarily withdrew (see Figure 1). AUDIT scores and demographic characteristics were compared between the treatment conditions (Table 1). Independent samples t-tests indicate that AUDIT score (t(30)=−0.52, p=0.61), age (t(30)=−0.32, p=0.75), education (t(30)=−0.47, p=0.64), and income (t(30)=0.09, p=0.93) did not differ between the treatment and control groups. Similarly, Chi-square test of independence indicates the active and control condition did not significantly differ with regard to gender (X2(1, N=35)=0.69, p=0.41) or race (X2(1, N=35)=0.04, p=0.84).
Figure 1.
CONSORT diagram.
Flow of participants through the study.
Table 1.
Demographic characteristics by treatment condition
| Active | Control | |
|---|---|---|
| AUDIT | 18.78 (7.42) | 20.00 (6.54) |
| Age | 38.89 (11.58) | 40.24 (12.91) |
| Education (in years) | 12.94 (2.18) | 13.35 (2.85) |
| Gender (% male) | 66.60 | 52.90 |
| Income (monthly) | 1235.50 (1574.90) | 1186.06 (1586.05) |
| Race | ||
| Black | 8 | 7 |
| White | 10 | 10 |
AUDIT total score, age, education and income are shown as mean (standard deviation). Gender is shown as percent of sample that is male. Race is shown as number of individuals reporting as black or white, no individuals reported being from other racial groups.
3.1. Implementation Intentions Compared to Control Intervention
To model the effect of treatment on the number of daily drinks, a hurdle (two-stage) model was implemented. First, a mixed effects logistic regression was used to model if a participant consumed alcohol or not on a given day (Table 2). During the baseline period, participants in the active condition were abstinent on 7.14% of the days while participants in the control condition were abstinent on 16.80% of the days. In comparison, during the intervention period, control participants were abstinent on 24.89% of the days, while participants in the active condition were abstinent on 14.05% of the days. The time point (i.e., baseline or intervention) was significant in the logistic regression model (b=0.68, z=2.02, p=0.04), indicating that during the baseline period participants were more likely to have days where alcohol was consumed than during the intervention period (OR=1.98, 95% CI [1.02,3.84]). Condition was not significant in the logistic regression (b=1.30, z=1.52, p=0.13, ns).
Table 2.
Hurdle regression of primary outcome measures
| b | SE | z | p | |
|---|---|---|---|---|
| Mixed Model Logistic Regression | ||||
| Condition | 1.30 | 0.85 | 1.52 | 0.13 |
| Timepoint | 0.68 | 0.34 | 2.02 | 0.04 |
| Condition x Timepoint | 0.28 | 0.59 | 0.49 | 0.62 |
| Gamma Mixed Model Regression | ||||
| Condition | −0.32 | 0.20 | −1.56 | 0.12 |
| Timepoint | 0.05 | 0.06 | 0.80 | 0.42 |
| Condition x Timepoint | 0.18 | 0.08 | 2.23 | 0.03 |
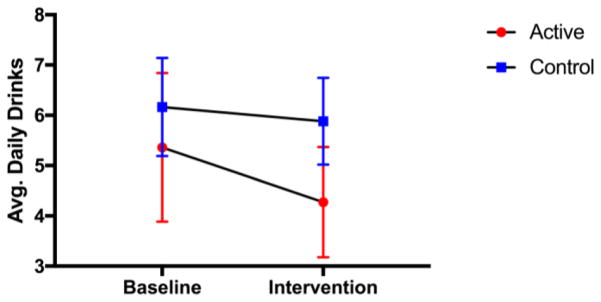
Second, the number of drinks consumed on drinking days was modeled using a Gamma mixed effects regression (R2=.44; Table 2) and a significant interaction was observed between condition and time point (b=0.18, z=2.23, p=0.03). During the baseline period, control participants consumed a model-adjusted average of 6.17 (SE=0.97) drinks per day and active participants consumed an average of 5.36 (SE=1.48) drinks per day. In the intervention period, control participants consumed a model-adjusted average of 5.88 (SE=0.86) drinks per day while active participants consumed an average of 4.27 (SE=1.10) drinks per day (see Figure 2). A Cohen’s d effect size of the contrast between conditions in daily drinking from baseline to intervention period was 0.07 for the control condition and 0.23 for the active condition.
Figure 2.
Change in drinking on days where alcohol was consumed.
Model-adjusted average drinks ± SE from baseline to intervention period by condition on days when drinking occurred.
3.2. Correlations between Self-report and Biologic EMAs
Pearson product-moment correlations between the average and the peak daily BrAC and daily self-reports of previous day drinks during the intervention period showed a positive significant correlation (r=0.33, p<0.001; r=0.23, p<0.001, respectively). A similar correlation was observed when only considering average BrAC on days where drinking was reported as well (r=0.25, p<0.001). The correlations between self-reported drinks and BrAC were not significantly different between conditions (t(30)=−1.29, p=0.21).
3.3. Alcohol Consumption at One-month Follow-up
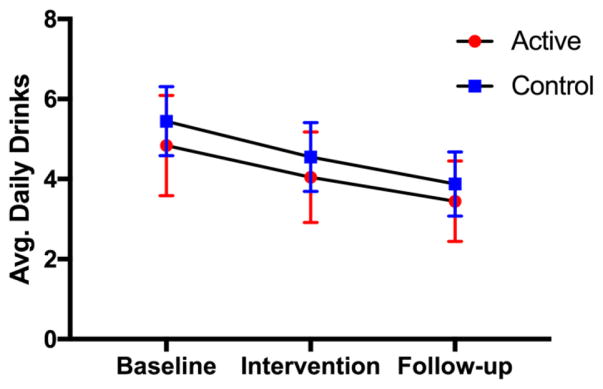
Alcohol consumption during the one-month following the intervention period was collected using the TLFB from the end of the intervention period to the one-month follow- up session. Average drinks across time points (baseline, intervention, and follow-up) were evaluated for persistence of reductions in alcohol consumption beyond the intervention period. Due to attrition, only 27 (active = 12, control = 15) of the 35 participants from the previous analyses completed the follow-up session (attrition rate=22.86%). The mixed regression modeled average drinks across fixed effects of time point and treatment conditions as well as random effects of participant. The overall model was significant (F(2,24)=12.77, p<0.001, R2=0.52). The average drinks during the one-month follow-up period were significantly less than average drinks during the baseline period (b=−0.34, z=−2.79, p<0.01); however, no significant difference was observed between the baseline and intervention periods (b=−0.18, z=−1.73, p=0.08, ns) or between treatment conditions (b=−0.12, z=−0.57, p=0.57, ns). Model-adjusted alcohol consumption by condition (active, control) and time point (baseline, intervention, follow-up) are shown in Figure 3.
Figure 3.
Alcohol consumption by treatment condition across all time points.
Model-adjusted average drinks by time point and condition. Note: Only participants that completed all time points (n=27) were included in this analysis and figure.
3.4. Treatment Acceptability and Compliance
Average responses to questions about treatment acceptability (see Supplemental Materials 2) are provided in Table 3. No significant differences were detected between treatment conditions using independent samples t-test for any of the adherence questions (test statistics are also reported in Table 3). Overall satisfaction with the study was rated as 3.18 on a 1 to 4 point scale across groups which corresponded to the treatment being satisfactory, easy, and convenient.
Table 3.
Treatment acceptability questions and average responses by condition
| Questions | Active | Control | t | p |
|---|---|---|---|---|
| How satisfied are you with the ability of this treatment to help you reduce your alcohol use? | 2.78 (0.94) | 2.59 (1.18) | 0.52 | 0.60 |
| How difficult is it to adhere to the scheduled requirements? | 3.11 (0.90) | 3.00 (1.12) | 0.32 | 0.75 |
| How convenient is it to use the SOBERLINK device? | 3.44 (0.78) | 3.82 (0.39) | 1.82 | 0.08 |
| How convenient is it to use a cell phone to communicate with us? | 3.67 (0.77) | 3.76 (0.56) | 0.43 | 0.67 |
| How convenient is it to use the debit card system to receive payments? | 3.61 (0.98) | 3.88 (0.33) | 1.11 | 0.28 |
| Taking all things into account, how satisfied are you with this treatment? | 3.17 (0.92) | 3.18 (0.95) | 0.03 | 0.98 |
Average responses and standard deviations are reported for each condition in addition to t-value and p-values. Treatment acceptability questions were rated by participants after completion of the intervention session on a scale from 1 to 4 where 1 = very [dissatisfied, difficult, inconvenient] and 4 = very [satisfied, easy, convenient].
To assess for compliance to the EMA schedules, the percent of successfully obtained self-report measurements and BrAC measurements were evaluated. The average percent of daily self-reports submitted was 97.75%. The average percent of breath alcohol samples submitted was 85.44% per participant and no significant difference in missingness was detected between the three daily breath alcohol sample timepoints (F(1,103)=0.61, p=0.43, ns). The EMA compliance rates are likely due, at least in part, to participants receiving $1 incentives for each submitted EMA that were electronically uploaded to participant debit cards for near-immediate access to the incentives. The higher percentage of successfully obtained self-report measures may be because participants had a longer window of time to provide a report of previous day drinking whereas breath samples had to be submitted within the prescribed hour window.
4. Discussion
This initial examination of an implementation intention treatment for alcohol use disorders capitalizes on technology to achieve frequent assessments of alcohol use and deliver intervention prompts repeatedly throughout treatment. The frequent EMAs of daily drinking provide the unique ability to distinguish between days of abstinence and days with drinking in order to identify more precisely the drinking processes influenced by implementation intentions. As such, two components of alcohol use were considered: (1) the decision to drink or not to drink on a given day was investigated using the mixed model logistic regression and (2) the amount of alcohol consumed on days when drinking was reported was evaluated using the mixed model Gamma regression.
While no significant difference was observed between conditions in the number of drinking days, participants in the active group reduced alcohol consumption more than the control group on drinking days during the intervention period. The active implementation intention treatment was associated with a significant reduction in alcohol consumption when drinking was reported. The model-adjusted average reduction in alcohol consumption from baseline to intervention was 1.09 drinks per day in the active implementation intention treatment condition compared to an average reduction of 0.29 drinks per days in the control condition (see Figure 1). The active implementation intention treatment was associated with a threefold reduction in alcohol consumed on drinking days compared to the control condition and is more than two times the reduction in daily alcohol consumption (0.5 drinks per day) observed in a previous, non-EMA or EMI, implementation intention study (Armitage & Arden, 2012). Furthermore, the difference in the reduction between active and control conditions exceed those observed in a meta-analysis of brief alcohol interventions (Bertholet, Daeppen, Wietlisbach, Fleming, & Burnand, 2005) with the current study showing a reduction of 5.6 drinks per week more in the active condition than the control compared to 4 drinks a week in the meta-analysis.
In addition to reductions in consumption on drinking days in the active condition, both conditions were abstinent more during the intervention period than the baseline period. The overall increase in abstinent days compared to baseline may be due to all participants: (1) being asked to try not to drink during the intervention period, (2) completing worksheets with critical situations and responses related to drinking (see Supplementary Materials 1), (3) being prompted for daily self-report and thrice daily biologic EMAs of drinking, and (4) receiving daily EMIs of (active or control) tailored cues.
The use of technologically-advanced methods to assess, intervene on, and incentivize participant behavior are a strength of the current study. The EMAs and EMIs were used throughout the study and the correlation between self-report and BrAC EMAs indicates a positive and significant concordance between the self-report and biologic assessment measures. The use of EMAs and EMIs to remotely assess and intervene on drinking behavior reduces participant burden by avoiding the need for frequent office visits while the collection of EMAs using the Soberlink devices also reduces experimenter burden by automating the collection process. The use of technology to increase ease of frequent (self-report and biologic) assessment of drinking, in addition to the near-immediate incentivization for providing these measurements likely contributed to the EMA compliance rates.
Participants that completed the follow-up session showed a significant reduction in alcohol consumption that was maintained across both conditions compared to baseline consumption (see Figure 3). One limitation of the follow- up assessment, unlike the baseline and intervention drinking assessments, was that follow-up data was collected using the TLFB as opposed to daily EMAs. Prior studies show that the TLFB is associated with slight underreporting of use in alcohol users compared to EMAs (Carney et al., 1998; Dulin et al., 2017; Searles et al., 2000) and thus the difference in measurement procedures may account, in part, for the observed reduction in alcohol consumption. This possibility is further supported by the the TLFB observations being collected a month following treatment which would typically be associated with a diminishing of treatment effects. Furthermore, 23% of participants did not return for the follow- up session perhaps leading to even greater uncertainty of the follow-up drinking assessments.
Importantly, participants rated the study design, the use of cell phones for study communication, the use of the Soberlink device for breath alcohol samples, and the use of the debit card system to remit payments above three on a scale from one to four (see Table 3). No significant differences in participant acceptability were observed between the active and control treatment groups. This finding is consistent with the study’s intention to provide largely comparable experiences for both active and control participants. Similarities in participant experiences included the daily (active or control) EMI cues which may have made participants more reflective about their drinking practices regardless of condition and the experimenter request at the start of the intervention period for participants to reduce alcohol use during the intervention period. In fact, the one difference in participant experience between conditions was linking the critical situations and alternative responses into if-then statements and then receiving those linked statements as cues. The similarity in participant experiences across conditions may, in part, explain the increase in the number of abstinent days compared to baseline in both conditions.
Finally, several weaknesses of the current study warrant mentioning. This was a proof-of-concept pilot study using biologic and self-report EMAs and daily EMIs to examine interventions and as a test of an implementation intention intervention to reduce alcohol use. As such, the sample size is small and some analyses do not include adequate sample size to confidently speak to the relationship with drinking behaviors. This pilot trial was not registered with clinicaltrials.com. Another weakness is the lack of intent-to-treat analysis of the one-month follow-up drinking assessment. The follow- up drinking may be underestimated both because this time point was collected using the TLFB measure and also because nearly a quarter of participants did not return for this follow-up session. Finally, some participants may have underreported drinking because of perceived social desirability of less drinking. Future studies may wish to continue to assess drinking using EMAs following the intervention period to better capture persistence in intervention effects.
The current report provides evidence of the moderate efficacy of implementation intentions to reduce alcohol consumption on drinking days. In addition, this study exemplifies the merits of using novel technology to collect frequent biologic assessments and daily self-reports of drinking in conjunction in daily intervention prompts. Future, larger scale studies using EMAs and EMIs will help to move the field of planning-based interventions forward as established strategies to reduce health risk behaviors.
Supplementary Material
Highlights.
Effective interventions to decrease alcohol consumption are needed.
Implementation intentions reduce amount of drinking on drinking days.
Largely remote interventions reduce patient burden.
Ecological momentary assessments increase reliability of measurement.
Ecological momentary interventions may increase impact of interventions.
Acknowledgments
Role of Funding Sources
Funding for this study was provided by an NIAAA Grant R01-AA021529 awarded to WKB and R21-AA022727 and R21-AA023605 awarded to MNK. LNM’s time was funded by NIAAA Grant F31-AA024368. NIAAA has no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or decision to submit this paper for publication.
The authors wish to thank the staff members at the Addiction Recovery Research Center for their help working with participants. The authors also wish to thank all of the voluntary participants at the Addiction Recovery Research Center for contributing to the better understanding of addiction and novel treatments.
Footnotes
Contributors
LNM, LMP, MNK, and WKB designed the study and wrote the protocol. LNM and LMP conducted literature searches and provided summaries of previous research studies. LNM and ANT conducted the statistical analysis. LNM and LMP wrote the first draft of the manuscript and all authors contributed to and have approved the final manuscript.
Conflict of Interest
WKB declares HealthSim LLC and NotifiUS LLC as organizations that I have interest in as a principal. All other authors declare that they have no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5. Arlington: American Psychiatric Publishing; 2013. Retrieved from http://www.lswo2014.org/StanMcCrackenDSMV.pdf. [Google Scholar]
- Armitage CJ. Efficacy of a brief worksite intervention to reduce smoking: the roles of behavioral and implementation intentions. Journal of Occupational Health Psychology. 2007;12(4):376–390. doi: 10.1037/1076-8998.12.4.376. [DOI] [PubMed] [Google Scholar]
- Armitage CJ. A volitional help sheet to encourage smoking cessation: a randomized exploratory trial. Health Psychology: Official Journal of the Division of Health Psychology, American Psychological Association. 2008;27(5):557–566. doi: 10.1037/0278-6133.27.5.557. [DOI] [PubMed] [Google Scholar]
- Armitage CJ. Effectiveness of experimenter-provided and self-generated implementation intentions to reduce alcohol consumption in a sample of the general population: A randomized exploratory trial. Health Psychology: Official Journal of the Division of Health Psychology, American Psychological Association. 2009a;28(5):545–553. doi: 10.1037/a0015984. [DOI] [PubMed] [Google Scholar]
- Armitage CJ. Is there utility in the transtheoretical model? British Journal of Health Psychology. 2009b;14(2):195–210. doi: 10.1348/135910708X368991. [DOI] [PubMed] [Google Scholar]
- Armitage CJ. Evidence That Implementation Intentions Can Overcome the Effects of Smoking Habits. Health Psychology: Official Journal of the Division of Health Psychology, American Psychological Association. 2016 doi: 10.1037/hea0000344. https://doi.org/10.1037/hea0000344. [DOI] [PubMed]
- Armitage CJ, Arden MA. A volitional help sheet to reduce alcohol consumption in the general population: a field experiment. Prevention Science: The Official Journal of the Society for Prevention Research. 2012;13(6):635–643. doi: 10.1007/s11121-012-0291-4. [DOI] [PubMed] [Google Scholar]
- Atkins DC, Baldwin SA, Zheng C, Gallop RJ, Neighbors C. A tutorial on count regression and zero-altered count models for longitudinal substance use data. Psychology of Addictive Behaviors: Journal of the Society of Psychologists in Addictive Behaviors. 2013;27(1):166–177. doi: 10.1037/a0029508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bertholet N, Daeppen JB, Wietlisbach V, Fleming M, Burnand B. Reduction of alcohol consumption by brief alcohol intervention in primary care: systematic review and meta-analysis. Archives of Internal Medicine. 2005;165(9):986–995. doi: 10.1001/archinte.165.9.986. [DOI] [PubMed] [Google Scholar]
- Carney MA, Tennen H, Affleck G, Del Boca FK, Kranzler HR. Levels and patterns of alcohol consumption using timeline follow-back, daily diaries and real-time” electronic interviews. Journal of Studies on Alcohol. 1998;59(4):447–454. doi: 10.15288/jsa.1998.59.447. [DOI] [PubMed] [Google Scholar]
- Cohn AM, Hunter-Reel D, Hagman BT, Mitchell J. Promoting behavior change from alcohol use through mobile technology: the future of ecological momentary assessment. Alcoholism, Clinical and Experimental Research. 2011;35(12):2209–2215. doi: 10.1111/j.1530-0277.2011.01571.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Vet E, Oenema A, Brug J. More or better: Do the number and specificity of implementation intentions matter in increasing physical activity? Psychology of Sport and Exercise. 2011;12(4):471–477. [Google Scholar]
- Dulin PL, Alvarado CE, Fitterling JM, Gonzalez VM. Comparisons of alcohol consumption by timeline follow back vs. smartphone-based daily interviews. Addiction Research & Theory. 2017;25(3):195–200. doi: 10.1080/16066359.2016.1239081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frane JW. A method of biased coin randomization, its implementation, and its validation. Drug Information Journal. 1998;32(2):423–432. [Google Scholar]
- Gollwitzer PM, Sheeran P. Implementation Intentions and Goal Achievement: A Meta- analysis of Effects and Processes. Advances in Experimental Social Psychology. 2006;38:69–119. [Google Scholar]
- Guillaumie L, Godin G, Manderscheid JC, Spitz E, Muller L. The impact of self-efficacy and implementation intentions-based interventions on fruit and vegetable intake among adults. Psychology & Health. 2012;27(1):30–50. doi: 10.1080/08870446.2010.541910. [DOI] [PubMed] [Google Scholar]
- Heather N, Gold R, Rollnick S. Readiness to change questionnaire: User’s manual. National Drug and Alcohol Research Centre, University of New South Wales Kensington; Australia: 1991. [Google Scholar]
- Heron KE, Smyth JM. Ecological momentary interventions: incorporating mobile technology into psychosocial and health behaviour treatments. British Journal of Health Psychology. 2010;15(Pt 1):1–39. doi: 10.1348/135910709X466063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koffarnus MN, Kablinger AS, Swallow AE, Bickel WK. Remote Alcohol Monitoring To Facilitate Abstinence Reinforcement: Preliminary Data. Alcoholism, Clinical and Experimental Research. 2015;39:204A. doi: 10.1111/acer.13891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madden D. Sample selection versus two-part models revisited: the case of female smoking and drinking. Journal of Health Economics. 2008;27(2):300–307. doi: 10.1016/j.jhealeco.2007.07.001. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Alterman AI, Cacciola J, Metzger D, O’Brien CP. A New Measure of Substance Abuse Treatment Initial Studies of the Treatment Services Review. The Journal of Nervous and Mental Disease. 1992;180(2):101–110. doi: 10.1097/00005053-199202000-00007. [DOI] [PubMed] [Google Scholar]
- Norman P, Wrona-Clarke A. Combining self-affirmation and implementation intentions to reduce heavy episodic drinking in university students. Psychology of Addictive Behaviors: Journal of the Society of Psychologists in Addictive Behaviors. 2016;30(4):434–441. doi: 10.1037/adb0000144. [DOI] [PubMed] [Google Scholar]
- Pittman B, Gueorguieva R, Krupitsky E, Rudenko AA, Flannery BA, Krystal JH. Multidimensionality of the Alcohol Withdrawal Symptom Checklist: A Factor Analysis of the Alcohol Withdrawal Symptom Checklist and CIWA-Ar. Alcoholism, Clinical and Experimental Research. 2007;31(4):612–618. doi: 10.1111/j.1530-0277.2007.00345.x. [DOI] [PubMed] [Google Scholar]
- R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing; Vienna, Austria: 2014. 2013. [Google Scholar]
- Rehm J, Mathers C, Popova S, Thavorncharoensap M, Teerawattananon Y, Patra J. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. The Lancet. 2009;373(9682):2223–2233. doi: 10.1016/S0140-6736(09)60746-7. [DOI] [PubMed] [Google Scholar]
- Rehm J, Room R, Graham K, Monteiro M, Gmel G, Sempos CT. The relationship of average volume of alcohol consumption and patterns of drinking to burden of disease: an overview. Addiction. 2003;98(9):1209–1228. doi: 10.1046/j.1360-0443.2003.00467.x. [DOI] [PubMed] [Google Scholar]
- Riordan BC, Conner TS, Flett JAM, Scarf D. A Brief Orientation Week Ecological Momentary Intervention to Reduce University Student Alcohol Consumption. Journal of Studies on Alcohol and Drugs. 2015;76(4):525–529. doi: 10.15288/jsad.2015.76.525. [DOI] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption--II. Addiction. 1993;88(6):791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, de La Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption-II. Addiction. 1993;88(6):791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Searles JS, Helzer JE, Walter DE. Comparison of drinking patterns measured by daily reports and timeline follow back. Psychology of Addictive Behaviors: Journal of the Society of Psychologists in Addictive Behaviors. 2000;14(3):277–286. doi: 10.1037//0893-164x.14.3.277. [DOI] [PubMed] [Google Scholar]
- Skaug H, Nielsen A, Magnusson A, Bolker B. Glmmadmb package (0.6. 7.1 edn) 2013 See Http://glmmadmb.R-Forge.R-Project.Org.
- Sobell LC, Sobell MB. Alcohol timeline followback users’ manual. Toronto, Canada: Addiction Research Foundation; 1995. [Google Scholar]
- Sullivan HW, Rothman AJ. When planning is needed: Implementation intentions and attainment of approach versus avoidance health goals. Health Psychology: Official Journal of the Division of Health Psychology, American Psychological Association. 2008;27(4):438–444. doi: 10.1037/0278-6133.27.4.438. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.