Abstract
Animals were experimentally infected with Brucella melitensis via aerosol. B. melitensis was cultured from the saliva and vaginal vault of infected animals, corresponding to bacterial dissemination in other target tissues. This is the first report of bacterial dissemination to these mucosal surfaces in a non-human primate model of brucellosis.
Keywords: aerosol exposure, Brucella melitensis, mucosal dissemination, rhesus macaque
1 | INTRODUCTION
Brucella melitensis is a Gram-negative, coccobacillus, zoonotic pathogen with worldwide distribution that can cause disease in multiple species.1 The primary natural route of human infection is through consumption of unpasteurized/raw dairy products. Goats and sheep are the preferred hosts for B. melitensis,2 and zoonotic transmission can occur through contact with infected animals and fluid transfer from mucous membranes, particularly during the birthing process.3,4 Inhalation poses an additional risk of infection; brucellosis among abattoir workers is attributed to this route of exposure.5–7 B. melitensis has been identified as a biological threat agent that holds the potential to be purposefully disseminated as an aerosol.8 Human brucellosis can be a debilitating and chronic disease characterized by fever, fatigue, depression, hepatosplenomegaly, arthritis, endocarditis, and genital infections.
Experimental brucellosis in the non-human primate causes progressive systemic infection affecting the spleen and liver.9,10 Physiological changes include characteristic pronounced undulating fever, mild to moderate anorexia, and transient tachycardia. The pathophysiologic changes noted in the rhesus macaque model are analogous to those of human brucellosis,10 making the rhesus an ideal candidate for vaccine efficacy studies.
2 | MATERIALS AND METHODS
2.1 | Humane care guidelines
The Institutional Animal Care and Use Committee (IACUC) of Tulane National Primate Research Center (TNPRC; assurance # A4499-01) reviewed and approved all animal studies. The TNPRC is fully accredited by AAALAC, International (AAALAC # 000594).
2.2 | Animals and Infection
A subset of TNPRC-bred Indian rhesus macaques (Macaca mulatta; male and female; 3.7–7.0 kg; 2.7–8.4 years of age) involved in a larger brucellosis vaccine study and exposed by inhalation to small-particle B. melitensis (str. 16M) using a head-only exposure system under high containment laboratory conditions11 were sampled for this study. Samples were obtained from the same four to five animals at each time point as available from the larger study. Animals received an inhaled dose of B. melitensis consistent with induction of disease (6.2E+06±1.2E+05 CFU/animal).10,12
Animals were biosampled under anesthesia at +15 days PI for saliva, liver, inguinal lymph node, and bronchoalveolar lavage fluid. Saliva samples were obtained prior to bronchoalveolar lavage by placing Weck-Cel sponges (Beaver-Visitec, Waltham, MA, USA) in the cheek pouches for at least 5 minutes. Liver biopsies were collected laparoscopically from the margins of the hepatic lobes using clamshell-type biopsy forceps. Bronchoalveolar lavage was performed using 40 mL of sterile saline.
Swabs of the vaginal vault were collected under anesthesia immediately prior to euthanasia at +45 days PI. Tissue samples including lung, spleen, liver, and bronchial lymph node were aseptically collected from the same sites in each animal during complete necropsy.
Samples were plated onto tryptic soy agar to determine the total CFU/organ. Serial dilutions were performed, and aliquots were plated. Brucella CFU were enumerated and colonies morphologically confirmed prior to recordation after 3 days of growth. Descriptive statistical analyses were performed using GraphPad Prism software (version 6.0, GraphPad Software, La Jolla, CA, USA).
3 | RESULTS
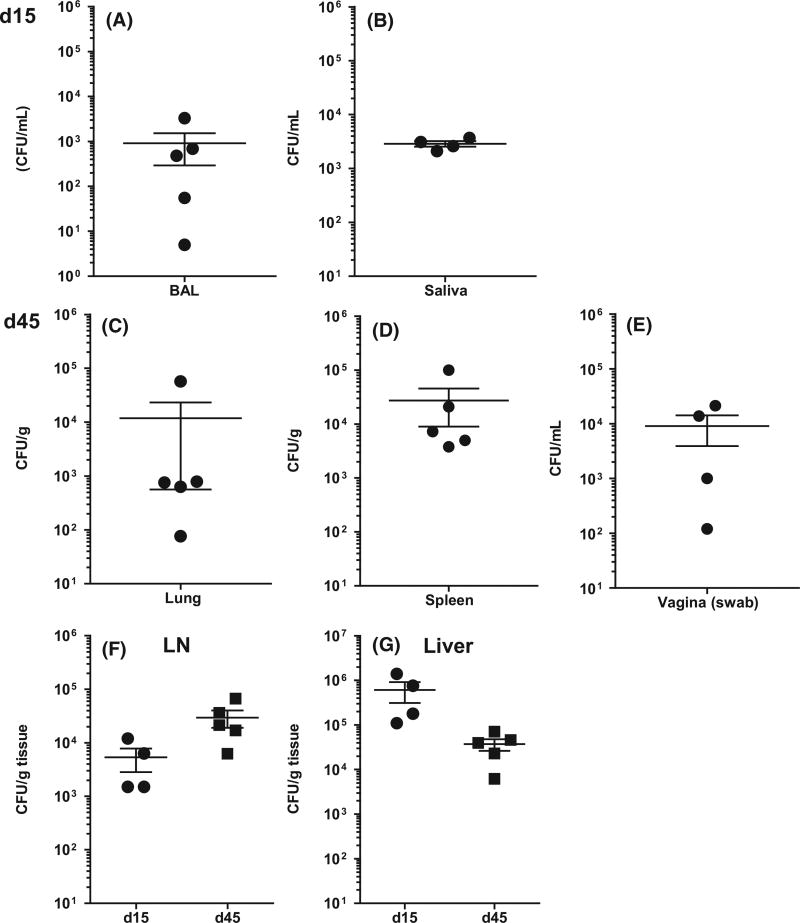
All animals developed positive brucellosis card test results following infection. Samples were analyzed at +15 days PI revealed bacterial dissemination to all tissues, and fluids were analyzed at that time point (Figure 1A,B,F,G). Subsequent sampling at the time of necropsy (+45 days PI) revealed B. melitensis in samples from the vaginal vault as well as within homogenized lung, spleen, lymph node, and liver tissues (Figure 1C–G). The greatest number of CFUs was obtained from liver biopsy samples at +15 days PI, and hepatic bacterial load remained high at necropsy. Lymph node burden increased between +15 and +45 days time points. CFU totals from BAL fluid (+15 days PI) and lung (+45 days PI) were varied, but culture of saliva showed consistent shedding of B. melitensis among sampled animals at +15 days PI.
FIGURE 1.
Colony-forming units (CFUs) per gram of tissue or per milliliter of fluid were determined for samples collected from rhesus macaques at 15 (A, B, F, G) and 45 (C–G) days post-infection with Brucella melitensis. Brucella organisms were identified in mucosal samples from the mouth and vagina as well as from known target tissues such as liver, lymph node, and spleen
4 | DISCUSSION
This is the first evidence of B. melitensis in mucosal secretions in a macaque model of brucellosis. Brucella species are known to be transmissible through mucosal surfaces. PCR/culture-positive vaginal samples have been obtained from dogs13 and goats,14 and contact with birthing fluids or aborted fetuses from these species is a common route of zoonotic transmission. Human-to-human transmission of Brucella species is considered rare, but sexual transmission has occasionally been reported. Male to female sexual transmission has been shown to occur,15,16 and an early report indicated that Brucella was present in female vaginal secretions,17 suggesting that transmission from females to males is also a potential concern.
Brucella melitensis disseminates throughout the body following aerosol inoculation. Not only can the disease cause pathology in multiple organs, causing variations in clinical presentation, but culturable organisms can also be found in many of these tissues or their secretions, enhancing the risk of transmission of Brucella from one animal to another. The greatest bacterial burden in this subset of B. melitensis-infected animals was noted in the liver during the acute phase of infection at +15 days PI; CFU decreased approximately one log entering the chronic phase at +45 days PI. In contrast, the number of bacteria cultured from lymph node samples increased as infection progressed. The presence of B. melitensis in lung, liver, spleen, and lymph node at necropsy is consistent with previously reported findings,10 although in those studies spleen was reported to have the highest bacterial load at +56 days PI, with bacterial burden decreasing in all tissues over time past +28 days PI. Unique to this study were the discoveries of culturable Brucella in the vaginal secretions and saliva of rhesus macaques at levels up to 104 CFU. The presence of B. melitensis in the saliva of the macaques sampled here contrasts the findings of a 7-day study of Brucella suis in rhesus macaques in which no Brucella DNA was found in buccal swab samples and it was concluded that Brucella does not remain in the mouth.9 Our results indicate that viable Brucella organisms can be obtained from the oral cavity for at least +15 days following infection. This report of culturable B. melitensis in vaginal secretions of rhesus macaques supports previous findings in other species17,18 and further advances the appropriateness of this model for human brucellosis pathogenesis and vaccine efficacy studies.
Acknowledgments
Funding information
This work was performed at Tulane National Primate Research Center, Covington, Louisiana, USA.
This research was supported by NIH 5 U54 AI057156 and by the TNPRC base grant (NIH, P51-OD11104).
References
- 1.Ozturk O, Akcam Z, Sahin U, Bircan A, Akkaya A, Yayli G. A rare agent of pneumonia: Brucella melitensis. Tuberkuloz ve toraks. 2008;56:443–447. [PubMed] [Google Scholar]
- 2.Marin CM, Jimenez de Bagues MP, Barberan M, Blasco JM. Comparison of two selective media for the isolation of Brucella melitensis from naturally infected sheep and goats. Vet Rec. 1996;138:409–411. doi: 10.1136/vr.138.17.409. [DOI] [PubMed] [Google Scholar]
- 3.Blasco JM, Molina-Flores B. Control and eradication of Brucella melitensis infection in sheep and goats. Vet Clin N Am-Food A. 2011;27:95–104. doi: 10.1016/j.cvfa.2010.10.003. [DOI] [PubMed] [Google Scholar]
- 4.Mustafa AA, Roberts RM, Corbel MJ. Isolation of Brucella melitensis from sheep in Syria. Vet Rec. 1985;117:277. doi: 10.1136/vr.117.11.277. [DOI] [PubMed] [Google Scholar]
- 5.Staszkiewicz J, Lewis CM, Colville J, Zervos M, Band J. Outbreak of Brucella melitensis among microbiology laboratory workers in a community hospital. J Clin Microbiol. 1991;29:287–290. doi: 10.1128/jcm.29.2.287-290.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sam IC, Karunakaran R, Kamarulzaman A, et al. A large exposure to Brucella melitensis in a diagnostic laboratory. J Hosp Infect. 2012;80:321–325. doi: 10.1016/j.jhin.2011.12.004. [DOI] [PubMed] [Google Scholar]
- 7.Ilhan Z, Aksakal A, Ekin IH, Gulhan T, Solmaz H, Erdenlig S. Comparison of culture and PCR for the detection of Brucella melitensis in blood and lymphoid tissues of serologically positive and negative slaughtered sheep. Lett Appl Microbiol. 2008;46:301–306. doi: 10.1111/j.1472-765X.2007.02309.x. [DOI] [PubMed] [Google Scholar]
- 8.Smither SJ, Perkins SD, Davies C, Stagg AJ, Nelson M, Atkins HS. Development and characterization of mouse models of infection with aerosolized Brucella melitensis and Brucella suis. Clin Vaccine Immunol. 2009;16:779–783. doi: 10.1128/CVI.00029-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yingst SL, Huzella LM, Chuvala L, Wolcott M. A rhesus macaque (Macaca mulatta) model of aerosol-exposure brucellosis (Brucella suis): pathology and diagnostic implications. J Med Microbiol. 2010;59:724–730. doi: 10.1099/jmm.0.017285-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Henning LN, Miller SM, Pak DH, et al. Pathophysiology of the rhesus macaque model for inhalational brucellosis. Infect Immun. 2012;80:298–310. doi: 10.1128/IAI.05878-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hartings JM, Roy CJ. The automated bioaerosol exposure system: preclinical platform development and a respiratory dosimetry application with nonhuman primates. J Pharmacol Toxicol. 2004;49:39–55. doi: 10.1016/j.vascn.2003.07.001. [DOI] [PubMed] [Google Scholar]
- 12.Lee KM, Chiu KB, Sansing HA, et al. Aerosol-induced brucellosis increases TLR-2 expression and increased complexity in the microanatomy of astroglia in rhesus macaques. Front Cell Infect Microbiol. 2013;3:86. doi: 10.3389/fcimb.2013.00086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Keid LB, Soares RM, Vasconcellos SA, et al. A polymerase chain reaction for detection of Brucella canis in vaginal swabs of naturally infected bitches. Theriogenology. 2007;68:1260–1270. doi: 10.1016/j.theriogenology.2007.08.021. [DOI] [PubMed] [Google Scholar]
- 14.Ebrahimi A, Milan JS, Mahzoonieh MR, Khaksar K. Shedding Rates and Seroprevalence of Brucella melitensis in Lactating Goats of Shahrekord. Iran. Jundishapur J Microbiol. 2014;7:e9394. doi: 10.5812/jjm.9394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Meltzer E, Sidi Y, Smolen G, Banai M, Bardenstein S, Schwartz E. Sexually transmitted brucellosis in humans. Clin Infect Dis. 2010;51:e12–e15. doi: 10.1086/653608. [DOI] [PubMed] [Google Scholar]
- 16.Kato Y1, Masuda G, Itoda I, Imamura A, Ajisawa A, Negishi M. Brucellosis in a returned traveler and his wife: probable person-to-person transmission of Brucella melitensis. J Travel Med. 2007;14:343–345. doi: 10.1111/j.1708-8305.2007.00139.x. [DOI] [PubMed] [Google Scholar]
- 17.Williams E. The Mediterannean Fever Commission-its origins and achievements. In: Young EJ, Corbel MJ, editors. Brucellosis—clinical and Laboratory Aspects. Boca Raton, FL: CRC Press; 1989. pp. 11–24. [Google Scholar]
- 18.Tittarelli M, Di Ventura M, De Massis F, et al. The persistence of Brucella melitensis in experimentally infected ewes through three reproductive cycles. J Vet Med, Series B. 2005;52:403–409. doi: 10.1111/j.1439-0450.2005.00885.x. [DOI] [PubMed] [Google Scholar]