Abstract
It is a well-known fact that inner ear diseases are often caused by microcirculatory disorders, and the recent literature is oriented towards investigations into the relationship between the cardiovascular system and cochleovestibular illness with related classical symptoms: tinnitus, hearing loss, and vertigo or instability. These symptoms, and particularly the vertigo, may be the alarm signal of microcirculatory disorders of the labyrinth or vertebrobasilar circulation so as to represent a possible symptom of posterior circulation stroke. The treatment aimed at correcting the haemodynamic and metabolic imbalance, generated by the cochleovestibular microcirculatory disorders, with drugs that act on the vessel wall being very useful, both alone and in combination with other treatment protocols. This is a multicenter retrospective observational study conducted in 40 neurootological laboratories with 873 patients with cardiovascular risk factors suffering from tinnitus, instability or peripheral vertigo alone or in combination with one another treated for the first time with mesoglycan. The data collected showed that the treatment with mesoglycan, irrespective of the type of vascular risk factor, is not only well tolerated but also significantly and objectively improves the cochleovestibular symptoms and the quality of life of patients suffering from tinnitus, peripheral vertigo and instability.
Keywords: dizziness, mesoglycan, tinnitus, vascular disease, vertigo
Introduction
The inner ear diseases are often caused by microcirculatory disorders.1 The anatomical structure of the inner ear is a terminal system closely dependent on the cochlear perfusion pressure. The mean arterial pressure reduction may cause a state of hypoxia in the inner ear and the related endothelial damage2 can lead to metabolic damage in the cochlear cells and thus to the classical cochleovestibular symptoms: tinnitus, hearing loss, and vertigo or instability. Tinnitus may be a disabling symptom3 and in the adult and senile population reaches a prevalence of 15%.4 It has often been microcirculatory disorders of the inner ear.5 Peripheral vertigo and dizziness may be the possible symptoms of posterior circulation stroke6 and affect7 33% of the general population,8 and the most frequent causes in the adult are benign paroxysmal positional vertigo (BPPV), migraine-associated vertigo, vestibular neuritis, endolymphatic hydrops and vascular disorders.9 From the evidence in the literature, it is clear that a treatment aimed at correcting the haemodynamic and metabolic imbalances at the origin of the cochleovestibular microcirculatory disorder with drugs that act on the circulating blood and the vessel wall being very useful, both alone and in combination with other treatment protocols.7 The drug that presents these characteristics is mesoglycan, essential constituents of the endothelium and the vessel walls with an antithrombotic function. This work comes from the GliCoVer2 study, an Italian multicenter retrospective observational study conducted in 40 neurootological laboratories, to assess the clinical efficacy and safety of administering mesoglycan orally to patients suffering from tinnitus, vertigo and/or instability.
Materials and methods
It is a retrospective observational study with no control group. The population studied was patients with cardiovascular risk factors suffering from tinnitus, instability or peripheral vertigo alone or in combination with one another treated for the first time with mesoglycan. Patients suffering from gastric ulcer, haemorrhagic diathesis, under oral anticoagulant therapy (OAT) and women who are or may be pregnant were excluded. Moreover, we excluded patients with dizziness caused by Meniére disease or started after sudden deafness. Informed consent was obtained from each participant after a full explanation of the study in accordance with the Declaration of Helsinki. All patients had been treated with two oral doses of 50 mg of mesoglycan per day for 90 days. The patients had also been reassessed after 30 (visit 2), 60 (visit 3) and 90 days (final visit).
All patients at each visit had been subjected to pure tone audiometry. At the first visit, demographical data were collected together with information about the presence of vascular risk factors and the presence of tinnitus, instability, including occasional or recurrent true spinning vertigo, and light-headedness was recorded together with the time for which every symptom had been suffered. All patients at each visit were subjected to Romberg’s test, which was considered pathological when, within 60 s, patients with their eyes closed could not maintain an upright position or increased the distance between their feet or arms, or opened their eyes. Patients with tinnitus filled in the Tinnitus Handicap Inventory (THI), which measures the impact of tinnitus on the patient’s daily life and is used to assess the result of treatments. The test is made up of three scales: functional (12 questions), emotional (8 questions) and catastrophic (5 questions), which concern physical functioning, the psychological impact, despair and loss of control. The total score ranges from 0 (no problem) to 100 (maximum impact on quality of life). Patients with vertigo or instability filled in the validated Italian version of the Dizziness Handicap Inventory (DHI), which measures the impact of vertigo on the patient’s quality of life. The test consists of 25 questions summed up on three scales: functional (9 questions), emotional (9 questions) and physical (7 questions). Finally, at each visit, the subjective perception of the gravity of the symptoms was assessed. Tinnitus, vertigo and instability were classified into four categories: ‘None’, ‘Mild’, ‘Moderate’ and ‘Severe’. The assessment was made both by the doctor and by the patient with a view to comparing any improvement, worsening or lack of a clinical change without the patient’s emotional state interfering with the overall assessment. The results were analysed using the statistics software SPSS version 19.0. To describe the categorical data, the frequencies were calculated, while for the continuous variables, the means and standard deviations were calculated. The differences between categorical data were calculated using the chi-square test and for the continuous variables using Student’s t-test. The variations in the continuous variables between visits were determined using the paired-sample t-test. The statistical tests were considered to be significant if less than 0.05.
Results
The study was conducted on 873 patients coming from 40 laboratories in 12 regions of Italy. A total of 761 patients came to the second visit, data were collected at the third visit on 682 patients, and the study was completed at the fourth visit attended by 671 patients. Of the patients who failed to complete the study, 124 were lost to follow-up, 28 discontinued it due to inefficacy of the treatment, 19 due to the cost of the drug, 6 due to side effects and 25 for other reasons. The average age of the total population at the initial visit was 57.6 years, and the proportion of men and women was similar (48.8% and 51.2%, respectively). The risk factor reported most frequently was hypertension (48.8%), followed by smoking (36.4%) and dyslipidaemia (25.2%). Familial migraine diathesis was reported by 9.6% of the patients. In the 671 patients who came to the final visit, the proportions of the variables were very similar, except for their level of education, which was slightly higher. At the initial visit, 363 patients reported tinnitus, 36 vertigo, 96 instability as isolated symptoms, while the other patients reported various combinations of these symptoms. In most cases, the onset of tinnitus had occurred during the previous 6 months, while instability had occurred during the previous month. The result of the treatment, assessed by the patient and the doctor, showed that 48.4% of the patients reported an improvement at visit 2, 65.8% at visit 3 and 80.0% at the final visit after 90 days. The percentages were very similar in the doctors’ assessments, that is, 50.1%, 68.6% and 84.0%, respectively. For vertigo, at the final visit, 100% of the patients reported an improvement, as did 91% of patients with vertigo associated with instability. Lower percentages of improvement were reported by patients with tinnitus both alone and in combination with vertigo (67.7% and 70%, respectively). The severity of the vertigo and instability improved significantly in the follow-up as it did for tinnitus, for which the improvement was, however, less marked. In fact, at the end of the study, while patients with severe vertigo and instability reported that the symptoms had disappeared altogether, 3.9% of the patients with tinnitus continued to assess them as severe at the last visit. In addition, over 2.2% of the patients with vertigo and 3.8% of patients with instability assessed their disease as moderate. As far as the duration of the symptoms is concerned, according to the patients’ assessment, 87.5% of patients with tinnitus for 1 month or less, 79.8% of those with tinnitus for 2–3 months, 71.3% for 4–5 months and 67.7% for 6 months (P = 0.021) had improved. For vertigo, 96.0% of the patients who had been suffering from it for 1 month or less reported an improvement, compared to 86.1% of those who had been suffering from it for 6 months or more (P = 0.039). For instability, the proportion of patients reporting an improvement varied from 93.3% to 79.3% for symptoms with a duration of 1 month or less compared to 6 months (P = 0.093).
No significant relationship was observed between the presence of risk factors and the result of the treatment, except for limited physical activity. With regard to the audiometry, the values improved significantly from the initial visit to the final visit for all frequencies measured. For the tinnitus hearing test, the mean threshold for the right ear dropped on average from 38.4 (standard deviation (SD), 24.1) to 35.1 dB (SD, 24.3; P < 0.001) and for the left ear from 40.9 (SD, 24.7) to 37.3 (23.5; P = 0.001). As far as Romberg’s test is concerned, at the initial visit, the test was negative in 36.4% of cases, while 21.5% opened their eyes, 30.8% moved their feet apart and 11.2% raised their arms. At the final visit, these percentages changed to 90.4%, 5.2%, 3.5% and 0.9%, respectively, thus showing a highly significant improvement (P < 0.001; Figure 1).
Figure 1.
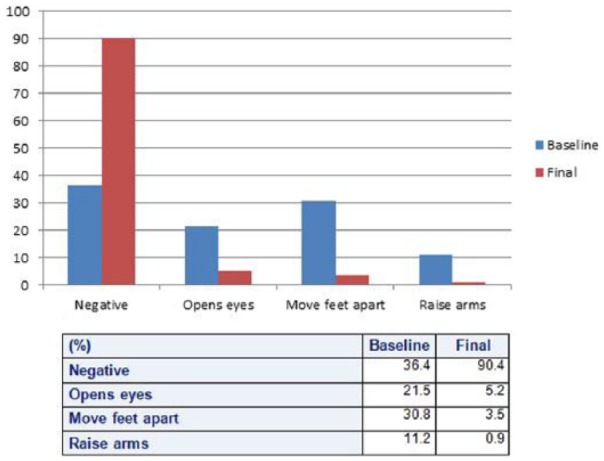
Trend of the percentage values of Romberg’s test.
Figure 2 shows the trend of the average values of the three scales of the THI at the various visits. A gradual reduction of the average values is observed, with significant differences (P < 0.001) between the first and fourth visit in all cases. Similar results were observed in the trend of mean values of the three scales of the DHI (Figure 3). Also in this case, the average scores dropped significantly between the first and last visits (P < 0.001).
Figure 2.
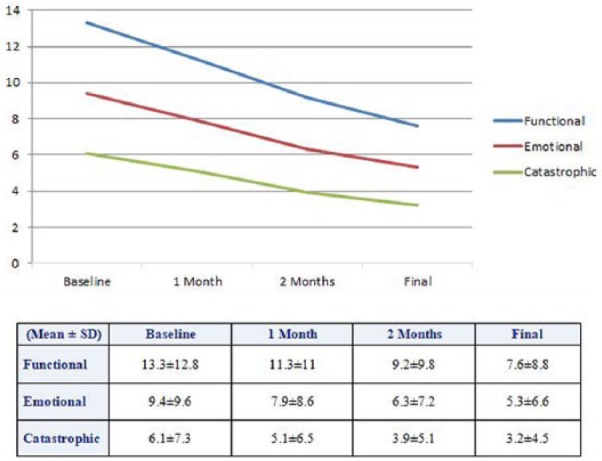
Trend of the mean values on the three Tinnitus Handicap Inventory (THI) scales.
Figure 3.
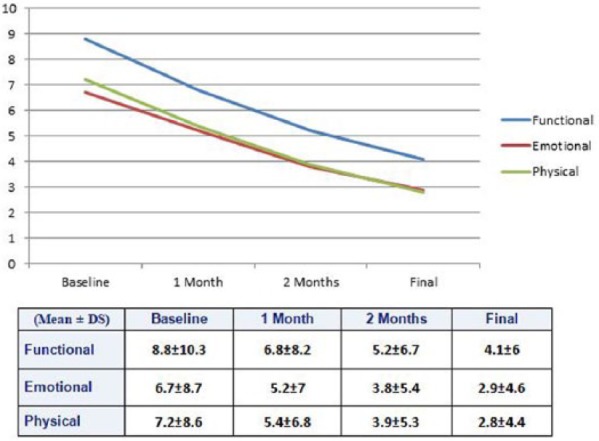
Trend of the mean values on the three Dizziness Handicap Inventory (DHI) scales.
Discussion and conclusion
Peripheral vertigo and tinnitus are easy to diagnose, but their origin is often difficult to recognize and this leads to excessive use of diagnostic instruments or the use of inappropriate treatment. Previous studies with subjective data and with short follow-up have revealed that mesoglycan is more effective than flunarizine in reducing the prevalence, the frequency and the intensity of tinnitus.10–12 The purpose of our study was to establish with objective data and with longer follow-up, whether, in patients with vascular risk factors, the treatment with mesoglycan improves tinnitus, vertigo and/or instability. The mesoglycan improves the microcirculatory haemodynamic and oxygen diffusion13 with direct effect on vestibular receptor producing improvement of the vertigo and instability. We found that mesoglycan improves significantly and inversely proportional to the times of onset of both tinnitus and instability. Probably if the onset of tinnitus is more recent, there is no sufficient time to consolidate in the amygdala-hippocampus circuit and therefore, if the mesoglycan is used at an early stage in the case of cochlear ischaemia, can reduce or even prevent the chronicization of the symptom, simply by increasing the cochlear blood flow. The pure tone audiometry and Romberg’s test at 90 days had improved both significantly. This suggests that the mesoglycan restores the microcirculation with a direct effect on the functionality of the cochlear receptor. The THI and DHI showed a gradual and significant improvement in symptoms during the treatment objectively, demonstrating the usefulness of treatment with mesoglycan in controlling tinnitus and instability. We can state that in patients with vascular risk factors suffering from tinnitus, vertigo and instability, the treatment with mesoglycan, irrespective of the type of vascular risk factor, is not only well tolerated but also significantly and objectively improves the cochleovestibular symptoms and the quality of life of patients.
Glicover Investigators
Giampiero Neri (CH), Claudio Petrolo (CZ), Vincenzo Stufano (BA), Massimo Degli Innocenti (Prato-FI), Angelo Chiantelli (Viareggio), Saverio Capobianco (SS), Marco Vinci (NU), Fabio Brocchetti (SV), Alberto Tombolini (Sanremo), Giacomo Caligo (GE), Paolo Marcolin (NA), Guglielmo Severino (Angri), Alfonso Scarpa (Nocera Inferiore-SA), Generoso Riccardi (Nola-NA), Mario Mandara (Pompei-NA), Mario Gamerra (Gragnano-NA), Vincenzo Marcelli (Agropoli-SA), Fiorenza G. D’Agostino (Sarno-SA), Renzo Cremonesi (AN), Gino Latini (Pesaro), Giovanni Serafini (Termoli-CB), Francesco Berni Canani (PE), Piero Fanizzi (BA), Paolo Luperto (BR), Federico Ummarino (Lucera-FG), Giuseppe Leo (San Severo-FG), Luigi Mazzotta (Casarano-LE), Angelo Scaringi (Cerignola-FG), Mauro Carboni (Orvieto), Piergiorgio Volpini (Branca), Giuseppe Morgante (VT), Ines Canciello (NA), Salvatore Mazzone (NA), Marco Angelillo (NA), Luigi Califano (BN), Roberto Falciglia (EN), Luigi Cutrera (RG), Angelo Anastasi (AG), Carlo Gianformaggio (Marsala), Giuseppe Monteleone (PA)
Acknowledgments
Any underlying research materials related to this paper (e.g. data, samples or models) can be accessed by sending a mail to giampiero.neri@unich.it
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship and/or publication of this article.
References
- 1. Guidetti G. (2005) La vertigine vascolare. Il razionale della diagnosi e della terapia. Otoneurologia 2000 21: 3–56. [Google Scholar]
- 2. Nakashima T, Naganawa S, Sone M, et al. (2003) Disorders of cochlear blood flow. Brain Research: Brain Research Reviews 43(1): 17–28. [DOI] [PubMed] [Google Scholar]
- 3. Newman CW, Sandridge SA, Jacobson GP. (2014) Assessing outcomes of tinnitus intervention. Journal of the American Academy of Audiology 25: 76–105. [DOI] [PubMed] [Google Scholar]
- 4. Martines F, Bentivegna D, Di Piazza F, et al. (2010) Investigation of tinnitus patients in Italy: Clinical and audiological characteristics. International Journal of Otolaryngology 2010: 265861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Baguley D, McFerran D, Hall D. (2013) Tinnitus. The Lancet 382: 1600–1607. [DOI] [PubMed] [Google Scholar]
- 6. Baloh RW. (1995) Vertebrobasilar insufficiency and stroke. Otolaryngology: Head and Neck Surgery 112(1): 114–117. [DOI] [PubMed] [Google Scholar]
- 7. Neri G, De Stefano A, Baffa C, et al. (2009) Treatment of central and sensorineural tinnitus with orally administered Melatonin and Sulodexide: Personal experience from a randomized controlled study. Acta Otorhinolaryngologica Italica 29: 86–91. [PMC free article] [PubMed] [Google Scholar]
- 8. Karatas M. (2008) Central vertigo and dizziness: Epidemiology, differential diagnosis, and common causes. The Neurologist 14: 355–364. [DOI] [PubMed] [Google Scholar]
- 9. Fields WS, Weibel J. (1964) Effects of vascular disorders on the vestibular system. In: Fields WS, Alford BR. (eds) Neurological Aspects of Auditory and Vestibular Disorders. Springfield, IL: Thomas, pp. 1–365. [Google Scholar]
- 10. Galioto GB, Mevio E. (1988) Mesoglycan in the treatment of vascular labyrinth disorders. La Nuova Clinica Otorinolaringologica 40: 223–225 (in Italian). [Google Scholar]
- 11. Bottazzi GM, Franzetti A. e Investigatori GliCoVer (2015) Il trattamento dell’acufene di origine vascolare con il mesoglicano. Argomenti di Acta Otorhinolaryngologica Italica 9(1): 1–6. [Google Scholar]
- 12. Oron Y, Elgart K, Marom T, et al. (2014) Cardiovascular risk factors as causes for hearing impairment. Audiology and Neurotology 19: 256–260. [DOI] [PubMed] [Google Scholar]
- 13. Caimi G, Romandini S, Lo Presi R, et al. (1992) Effect of mesoglycan on macrorheologic and microrheologic parameters. Current Therapeutic Research 52: 412–418. [Google Scholar]


