Abstract
Introduction:
The incidence of hip fracture is projected to increase in the next 25 years as the world population ages. Hip fracture is often associated with subsequent readmission and mortality. Nevertheless, elderly patients often may not achieve the same level of functional ability as prior to their injury. Several studies have shown that close collaboration between orthopedic surgeons and geriatricians can improve such outcomes and Geriatric Day Hospital (GDH) is one of the examples of collaboration to improve such outcomes. The aim of this descriptive retrospective study is to review the effectiveness of the day rehabilitation program provided by a GDH on functional outcomes, mortality, and readmission rate, among a sample of elderly patients with hip fracture.
Methods:
The medical records of patients from January 1, 2009, to December 31, 2012, were collected and evaluated. Demographic data of the patients and Charlson Comorbidity Index were collected. The Barthel Index, Elderly Mobility Scale, and Mini-Mental State Examination were measured on admission and at discharge of the patients to evaluate both physical and cognitive functions.
Results:
The results showed that the majority of patients benefited from rehabilitation in the GDH. The 12-month mortality rate of patients taking full-course rehabilitation in the GDH was improved. The age of patient was the most important factor influencing the rehabilitation outcomes. Gender was the only risk factor for 12-month mortality and 6-month readmission.
Discussion:
Since patients were selected to attend GDH, there was a bias during the selection of patients. Furthermore, it was difficult to compare patients attended GDH with patients who did not because outcomes of the latter were difficult to be recorded.
Conclusions:
Our study shows that postoperative geriatric hip fracture patients definitely can benefit from rehabilitation service offered by GDH in terms of functional and cognitive outcomes.
Keywords: day rehabilitation program, Geriatric Day Hospital (GDH), geriatric hip fractures, functional outcomes, readmission, mortality
Introduction
The incidence of hip fractures is projected to increase by more than 250% in the next 25 years as the world population ages.1,2 Hip fracture is often associated with subsequent rehospitalization, increased number of hospital stay, and high hospital costs. In United States, Sloan et al3 reported a 167% increase in expense for hospital readmission from 1984 to 1994 for patients with hip fracture. The occurrence of unplanned hospital readmission among elderly adults with hip fracture is a significant concern, as it will further burden our medical system. Apart from readmission, the elderly patients become weaker by the effect of hospitalization and surgery.4 As a result, the patients may not achieve the same level of functional ability as prior to their injury. Approximately one-third of the patients with hip fracture die within the first year after surgery.5,6 Existing literatures suggested that there is a need to improve the efficiency and quality of hip fracture treatment and the model of care. An example of such improvement is the establishment of day rehabilitation program for those patients who received hip fracture surgery. It has been reported that the collaboration between orthopedic surgeons and geriatricians can improve hip fracture patients’ outcomes, which include activities of daily living (ADLs), number of medical complications, readmissions, subsequent mortality, and long-term restitution.7–10 A number of preliminary studies have shown that better outcomes were resulted when elderly patients were treated by a closed collaboration between orthopedic surgeons and geriatricians.11–13
In Hong Kong, there are 14 geriatric day hospitals (GDHs) providing day rehabilitation services and serving different parts of Hong Kong.14 There are geriatricians, physiotherapists, and nurses with geriatric expertise providing care for patients after hip fracture surgery during daytime on weekdays. The services include the following components: conducting initial physical and mental screening and evaluation; providing continuity of care including geriatric care, physiotherapy, and occupational therapy; and early discharge planning. After hip fracture surgery in acute hospital, patients are referred to GDHs for physical therapy. Different patients have different treatment timelines according to the suggestions by physical therapists. They would be discharged once they reach the plateau of their exercise tolerance. Although the day rehabilitation program provided by GDH has been launched for decades, there is still lack of evidence showing such service is effective in improving the eventual outcomes of the patients after hip fracture surgery. Furthermore, as the number of geriatric hip fracture is increasing dramatically in recent years, the resource implication for the rehabilitation is expected to significantly increase burden to our social economic system in the coming years. It is time to justify the efficiency of day rehabilitation service with balance of the clinical outcome and social resource implicated being taken into account.
The aim of this descriptive retrospective study is to review the effectiveness of the day rehabilitation program provided by GDH on functional outcomes, mortality, and readmission rate, among a sample of elderly patients with hip fracture.
Materials and Methods
Patients
Some patients after hip fracture surgery in one of the acute hospitals are transferred to a GDH in Hong Kong for further rehabilitation after discharge. Medical records of the patients attending this GDH from January 1, 2009, to December 31, 2012, were collected for this retrospective study. Patients aged 60 or above who received hip surgery due to low-energy traumatic (defined as fall from standing height) hip fracture and had attended full course of rehabilitation in this GDH were included in this study. The hip fracture should be isolated, including femoral neck, intertrochanteric, and subtrochanteric fractures. Patients having pathological fractures, periprosthetic fractures, multiple fractures, totally bedridden, or more than 14 days’ surgery lag time were excluded. A total of 253 patients were recruited in the study. The study was approved by the institutional review board of the institution.
Data Collection
Demographic data of the patients, including age, gender, premorbid walking status, smoking status, use of bisphosphonates, length of stay in acute hospital, and Charlson Comorbidity Index (CCI) were collected. Charlson Comorbidity Index is the most extensively studied comorbidity index and widely used.15 The Barthel Index (BI), Elderly Mobility Scale (EMS), and Mini-Mental State Examination (MMSE) were measured on admission and at discharge of the patients to evaluate both physical and cognitive functions. The rehabilitation effectiveness (RE) has been used to evaluate the rehabilitative impact as early as 1987 by Heinemann and Shah in 1990.16,17 Rehabilitation effectiveness was defined as the percentage of potential functional improvement actually achieved, so as to take the potential maximal functional improvement into account. In this study, the outcome was evaluated by RE in terms of BI, EMS, and MMSE and calculated as follows:
In additional to that, cumulative readmission (3 and 6 months after discharge), cumulative mortality (1, 6, and 12 months after discharge), and refracture within 2 years of patients were also recorded to evaluated outcomes.
Statistical Analyses
Statistical analyses were carried out using Statistical package for Social Science software version 17.0. Independent t test was used for continuous variables, and χ2 test was performed for categorical variables. Statistical significance was set as P < .05.
Linear regression was used to determine those risk factors for poor RE in terms of BI, EMS, and MMSE. Binary logistic regression was used to determine risk factors for mortality, refracture, and readmission. The covariates that were controlled during multivariate analysis included gender, age, smoking status, use of bisphosphonates, length of stay, CCI, BI on admission, EMS on admission, MMSE on admission, and premorbid ambulatory status.
Results
During the observed period from January 1, 2009, to December 31, 2012, 317 elderly patients attended the GDH for rehabilitation. Among these patients, 253 met the inclusion criteria and were included. Most patients were female (75.9%). Majority of the recruited patients were between 80 and 89 years. Only 47 (18.6%) patients were smoker or ex-smoker, and 34 (13.4%) patients had been taking bisphosphonates. Two hundred one (80.4%) patients stayed in acute hospital no more than 7 days, whereas 49 (19.6%) patients stayed in acute hospital for more than 7 days. The mean CCI was 2.6. Most of the patients walked with aid before injury. The detailed demographic profile of the study population is shown in Table 1.
Table 1.
Demographic Profile of Study Population.
| Demographic Variable | All (N = 253), n (%) |
|---|---|
| Gender | |
| Male | 61 (24.1%) |
| Female | 192 (75.9%) |
| Age (years) | |
| 60-69 | 8 (3.2%) |
| 70-79 | 71 (28.1%) |
| 80-89 | 140 (55.3%) |
| 90-99 | 33 (13.0%) |
| ≥100 | 1 (0.4%) |
| Premorbid ambulation status | |
| Walking without aid | 94 (37.2%) |
| Walking with aid | 159 (62.8%) |
| Smoking status | |
| Nonsmoker | 206 (81.4%) |
| Smoker or ex-smoker | 47 (18.6%) |
| Use of bisphosphonates | |
| Not used | 219 (86.6%) |
| Used | 34 (13.4%) |
| BI on admission | |
| 61-100 (slightly dependent or independent) | 214 (84.6%) |
| 41-60 (moderately dependent) | 19 (7.5%) |
| 0-40 (severely dependent) | 20 (7.9%) |
| EMS on admission | |
| 15-20 (independent) | 83 (32.7%) |
| 10-14 (moderately dependent) | 97 (38.3%) |
| 0-9 (severely dependent) | 73 (28.9%) |
| MMSE on admission | |
| 27-30 (normal) | 22 (8.7%) |
| 21-26 (slight) | 70 (27.7%) |
| 10-20 (moderate) | 140 (55.3%) |
| 0-9 (severe) | 21 (8.3%) |
| Charlson Comorbidity Index, mean (SD) | 2.4 (2.6) |
Abbreviations: BI, Barthel Index; EMS, Elderly Mobility Score; MMSE, Mini-Mental State Examination; SD, standard deviation.
The mean scores of BI, EMS, and MMSE on admission were 80.5, 12.1, and 17.8, respectively. Most of the patients showed improvement in physical and cognitive function after rehabilitation in GDH (mean score increased on discharge; P < .000). The mean RE is also shown in Table 2. Those patients with maximum scores on admission were excluded when calculating the RE.
Table 2.
Mean of RE, Physical, and Cognitive Measures Before and After Rehabilitation in GDH.
| Time Points for Evaluating Patients’ Outcomes | BI | EMS | MMSE |
|---|---|---|---|
| Mean score on admission, mean (SD) | 80.5 (19.8) | 12.1 (4.6) | 17.8 (6.2) |
| Mean score at discharge, mean (SD) | 83.2 (20.2) | 13.8 (4.9) | 19.1 (6.6) |
| P value | .000 | .000 | .000 |
| Mean RE (%), mean (SD) | 22.5 (66.6), n = 233 | 27.1 (32.9), n = (240) | 12.3 (35.4), n = (251) |
Abbreviations: BI, Barthel Index; EMS, Elderly Mobility Score; GDH, Geriatric Day Hospital; MMSE, Mini-Mental State Examination; RE, rehabilitation effectiveness; SD, standard deviation.
Bivariate analysis was used to study the relationship between RE and various variables. On the other hand, it revealed any significant factors for RE determined by BI, EMS, and MMSE (Table 3). It showed that older age (>90) was the significant factor influencing improvement in BI (P < .05), while premorbid ambulatory status was the significant factor influencing that of EMS (P < .05). Barthel Index and EMS on admission were all important factors related to the improvement of BI and EMS. Mini-Mental State Examination can reflect the cognitive status of patients. In our study, there was no single important factor related to the improvement in MMSE, including MMSE on admission. Smoking status, use of bisphosphonates, length of stay, and CCI did not have any relationship on the RE in terms of BI, EMS, and MMSE. In the subsequent multivariate analysis, only older age (>90) was the independent predictor factor of poor RE of BI, while poor BI and EMS performance on admission were independent predictor factors of poor RE of EMS.
Table 3.
Bivariate Analysis of RE and Various Variables.
| Demographic Variable | Mean RE by BI (%); n | P Value (Compared With Mean of First Group) | Mean RE by EMS (%); n | P Value (Compared With Mean of First Group) | Mean RE by MMSE (%); n | P Value (Compared With Mean of First Group) |
|---|---|---|---|---|---|---|
| Gender | ||||||
| Male | 30.2 (46.1); 54 | – | 25.8 (32.8); 59 | – | 16.1 (30.3); 59 | – |
| Female | 20.2 (71.6); 179 | .334 | 27.5 (33.0); 181 | .719 | 11.2 (36.8); 192 | .346 |
| Age | ||||||
| 60-74 | 55.0 (39.1); 23 | – | 25.1 (36.2); 24 | – | 19.2 (72.7); 27 | – |
| 75-89 | 20.9 (68.3); 176 | .061 | 29.5 (33.8); 182 | .923 | 12.4 (29.2); 190 | .953 |
| ≥90 | 8.6 (67.1); 34 | .029a | 15.7 (22.5); 34 | .603 | 6.4 (18.8); 34 | .763 |
| Premorbid ambulation status | ||||||
| Walk without aid | 32.9 (56.6); 77 | – | 33.8 (37.9); 84 | – | 14.3 (44.5); 92 | – |
| Walk with aid | 17.4 (70.6); 156 | .095 | 23.5 (29.4); 156 | .033a | 11.2 (28.8); 159 | .505 |
| Charlson Comorbidity Index | ||||||
| 0 | 28.2 (77.9); 49 | – | 28.1 (30.9); 52 | – | 13.0 (35.1); 57 | – |
| 1-2 | 24.3 (53.1); 100 | 1.0 | 29.3 (34.5); 104 | 1.0 | 9.7 (40.0); 107 | 1.0 |
| >2 | 17.0 (74.0); 84 | 1.0 | 23.8 (32.2); 84 | 1.0 | 15.1 (29.5); 87 | 1.0 |
| Smoking status | ||||||
| Nonsmoker | 24.1 (57.6); 187 | .569 | 26.5 (32.3); 197 | .571 | 11.4 (37.0); 204 | .386 |
| Smoker or ex-smoker | 15.7 (95.3); 46 | 29.7 (35.9); 43 | 16.4 (27.3); 47 | |||
| Use of bisphosphonate | ||||||
| Bisphosphonates not used | 19.5 (69.8); 200 | .096 | 26.2 (32.2); 208 | .281 | 11.1 (36.4); 217 | .152 |
| Bisphosphonates used | 40.3 (38.0); 33 | 33.0 (37.0); 32 | 20.4 (26.5); 34 | |||
| Length of stay | ||||||
| ≤7 days | 22.0 (72.6); 201 | .849 | 27.3 (32.2) | .407 | 12.4 (36.3) | .874 |
| >7 days | 24.1 (36.6); 49 | 22.8 (33.2) | 11.5 (28.6) | |||
| BI on admission | ||||||
| 61-100 | 25.6 (71.9); 194 | – | 30.4 (34.0); 201 | – | 12.7 (37.6); 212 | – |
| 41-60 | 6.8 (27.9); 19 | .078 | 9.3 (17.5); 19 | .000a | 14.3 (23.0); 19 | 1.0 |
| 0-40 | 6.8 (15.5); 20 | .009a | 10.8 (21.2); 20 | .003a | 7.0 (14.3); 20 | 1.0 |
| EMS on admission | ||||||
| 15-20 | 48.6 (62.5); 66 | – | 39.6 (41.9); 70 | – | 17.4 (50.3); 81 | – |
| 10-14 | 12.6 (84.6); 94 | .007a | 28.6 (28.7); 97 | .171 | 13.6 (21.3); 97 | .893 |
| 0-9 | 11.5 (66.6); 73 | .000a | 13.1 (21.4); 73 | .000a | 5.0 (28.9); 73 | .171 |
| MMSE on admission | ||||||
| 27-30 | 36.2 (92.9); 15 | – | 30.2 (45.3); 19 | – | 0.8 (87.3); 20 | – |
| 21-26 | 34.8 (72.8); 62 | 1.000 | 37.5 (34.4); 64 | .988 | 21.2 (39.7); 70 | .904 |
| 10-20 | 16.9 (64.6); 135 | .971 | 24.0 (30.2); 136 | .994 | 10.8 (18.3); 140 | .997 |
| 0-9 | 11.9 (19.0); 21 | .913 | 12.9 (24.3); 21 | .623 | 12.3 (35.4); 21 | 1.0 |
Abbreviations: BI, Barthel Index; EMS, Elderly Mobility Score; MMSE, Mini-Mental State Examination; RE, rehabilitation effectiveness.
aSignificant difference (P < .05).
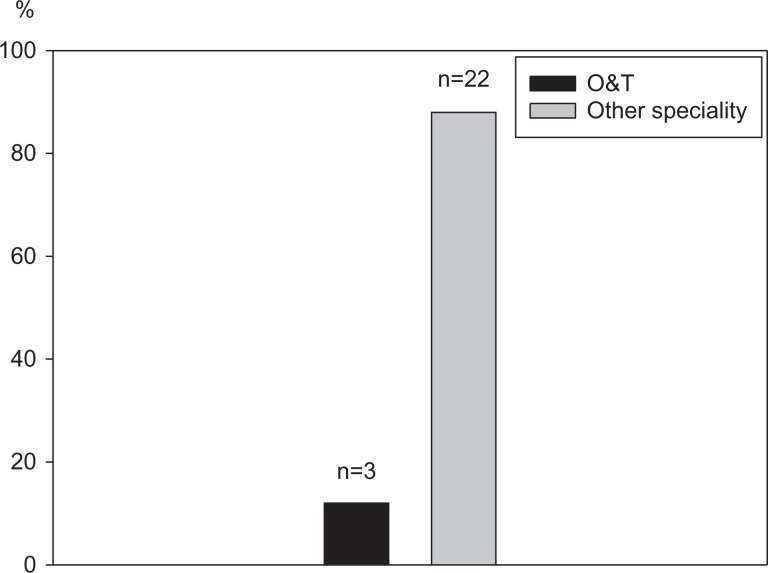
The outcomes of patients were evaluated by readmission, refracture, and mortality. As shown in Table 4, there were readmissions of 15 (5.9%) and 25 (9.9%) within 3 and 6 months after discharge, respectively. Only 3 (12%) of these patients were readmitted to orthopedics and traumatology specialty, while 22 (82%) of these patients were readmitted to other specialties (Figure 1). Fifteen (5.9%) patients underwent refracture within 2 years. No patients died within 6 months and 12 (4.7%) patients died within 12 months.
Table 4.
Outcomes of Patients Discharged From GDH.
| Outcomes | n (%) |
|---|---|
| Readmission | |
| Cumulative within 3 months | 15 (5.9%) |
| Cumulative within 6 months | 25 (9.9%) |
| Readmission specialty | |
| O&T | 3 (12%) |
| Other specialty | 22 (88%) |
| Refracture within 2 years | 15 (5.9%) |
| Mortality | |
| Within 3 months | 0 (0%) |
| Within 6 months | 0 (0%) |
| Within 1 year | 12 (4.7%) |
Abbreviations: GDH, Geriatric Day Hospital; O&T, orthopedics and traumatology.
Figure 1.
Readmission specialties of patients’ readmission within 6 months. O&T indicates orthopedics and traumatology.
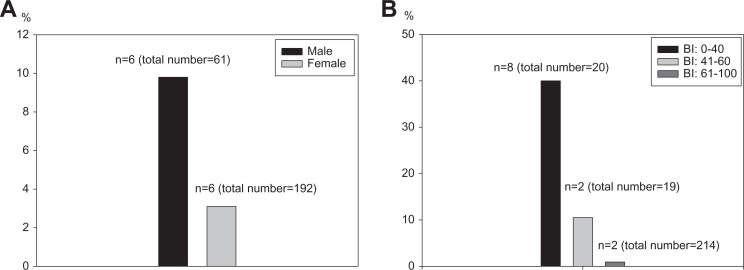
Bivariate analysis indicated no risk factors for readmission and refracture within 2 years (Table 5). On the other hand, males, poor BI performance on admission, and poor EMS performance on admission were risk factors for cumulative 12-month mortality.
Table 5.
Risk Factors for Poor Outcomes (Cumulative Readmission Within 3 Months and 6 Months, Refracture Within 2 Years, and Cumulative Mortality Within 1 Year).
| Risk Factors | Readmission Within 3 Months (n = 15) | P Value (Compared With Mean of First Group) | Readmission Within 6 Months (n = 25) | P Value (Compared With Mean of First Group) | Refracture Within 2 Years | P Value (Compared With Mean of First Group) | Cumulative Mortality Within 1 Year | P Value (Compared With Mean of First Group) |
|---|---|---|---|---|---|---|---|---|
| Gender | ||||||||
| Male (61) | 4 (6.6%) | .811 | 8 (13.1%) | .331 | 3 (4.9%) | .701 | 6 (9.8%) | .032 a |
| Female (192) | 11 (5.7%) | 17 (8.6%) | 12 (6.25%) | 6 (3.1%) | ||||
| Age | ||||||||
| 60-74 (28) | 0 (0%) | .225 | 1 (3.6%) | .458 | 0 (0%) | .146 | 0 (0%) | .129 |
| 75-89 (191) | 14 (7.3%) | 21 (11.0%) | 11 (5.8%) | 12 (6.3%) | ||||
| ≥90 (34) | 1 (2.9%) | 3 (8.8%) | 4 (11.8%) | 0 (0%) | ||||
| Premorbid ambulation status | ||||||||
| Walk without aid (94) | 5 (5.3%) | .752 | 8 (8.5%) | .574 | 5 (5.3%) | .752 | 3 (3.2%) | .372 |
| Walk with aid (159) | 10 (6.3%) | 17 (10.7%) | 10 (6.3%) | 9 (5.7%) | ||||
| Charlson Comorbidity Index | ||||||||
| 0 (57) | 1 (1.8%) | .283 | 2 (3.5%) | .186 | 4 (7.0%) | .734 | 1 (1.8%) | .052 |
| 1-2 (109) | 7 (6.4%) | 13 (11.9%) | 5 (4.6%) | 3 (2.8%) | ||||
| >2 (87) | 7 (8.0%) | 10 (11.5%) | 6 (6.9%) | 8 (9.2%) | ||||
| Smoking status | ||||||||
| Nonsmoker (206) | 12 (5.8%) | .884 | 18 (8.7%) | .202 | 13 (6.3%) | .590 | 10 (4.9%) | .862 |
| Smoker or ex-smoker (47) | 3 (6.4%) | 7 (14.9%) | 2 (4.3%) | 2 (4.3%) | ||||
| Use of bisphosphonate | ||||||||
| Bisphosphonates not used (219) | 12 (5.5%) | .442 | 20 (9.1%) | .311 | 12 (5.6%) | .442 | 10 (4.6%) | .737 |
| Bisphosphonates used (34) | 3 (8.8%) | 5 (14.7%) | 3 (8.8%) | 2 (5.9%) | ||||
| Length of stay | ||||||||
| ≤7 days (201) | 11 (5.5%) | .477 | 18 (9.0%) | .265 | 13 (6.5%) | .227 | 8 (4.0%) | .512 |
| >7 days (49) | 4 (8.2%) | 7 (14.3%) | 1 (2.0%) | 3 (6.1%) | ||||
| BI on admission | ||||||||
| 61-100 (214) | 14 (6.5%) | .503 | 20 (9.3%) | .244 | 12 (5.6%) | .723 | 2 (0.9%) | .000 a |
| 41-60 (19) | 0 (0%) | 1 (5.3%) | 1 (5.3%) | 2 (10.5%) | ||||
| 0-40 (20) | 1 (5%) | 4 (20%) | 2 (10%) | 8 (40%) | ||||
| EMS on admission | ||||||||
| 15-20 (83) | 2 (2.4%) | .236 | 3 (3.6%) | .064 | 5 (6.0%) | .207 | 1 (1.2%) | .046 a |
| 10-14 (97) | 8 (8.2%) | 13 (13.4%) | 3 (3.1%) | 4 (4.1%) | ||||
| 0-9 (73) | 5 (6.8%) | 9 (12.3%) | 7 (9.6%) | 7 (9.6%) | ||||
| MMSE on admission | ||||||||
| 27-30 (22) | 0 (0%) | .224 | 1 (4.5%) | .151 | 0 (0%) | .302 | 0 (0%) | .062 |
| 21-26 (70) | 2 (2.9%) | 3 (4.3%) | 6 (8.6%) | 1 (1.4%) | ||||
| 10-20 (140) | 12 (8.6%) | 19 (13.6%) | 9 (6.4%) | 8 (5.7%) | ||||
| 0-9 (21) | 1 (4.8%) | 2 (9.5%) | 0 (0%) | 3 (14.3%) | ||||
Abbreviations: BI, Barthel Index; EMS, Elderly Mobility Score; MMSE, Mini-Mental State Examination; RE, rehabilitation effectiveness.
aSignificant difference (P < .05).
Multivariate analysis was also performed (Table 6). Similarly, no risk factors for readmission and refracture were found in this study. The risk factors for 12-month mortality were male and poor BI performance on admission (Figure 2).
Table 6.
Risk Factors for Outcomes of Patients Discharged From GDH.a
| Dependent | Variable | OR (95% CI) | P |
|---|---|---|---|
| Cumulative mortality within 12 months | BI on admission | 30.5 | .028 * |
| Sex | 13.5 | .029 * |
Abbreviations: CCI, Charlson Comorbidity Index; CI, confidence interval; EMS, Elderly Mobility Scale; GDH, Geriatric Day Hospital; OR, odds ratio.
aDependents were set as cumulative readmission within 3 and 6 months, refracture within 2 years, and cumulative mortality within 1 year. Controlling factors include gender, age, smoking status, use of bisphosphonates, CCI, BI on admission, EMS on admission, MMSE on admission, and premorbid ambulatory status.
*Significant difference because P value < 0.05.
Figure 2.
Twelve-month mortalities of patients with different genders (A) and BI performance on admission (B). BI indicates Barthel Index.
Discussion
Elderly patients have a higher risk in experiencing functional decline after hospitalization. Córcoles-Jiménez et al showed that 20% of patients remain in a situation of dependence after discharge.18 The implementation of GDH is to allow elderly patients receive rehabilitation and comprehensive geriatric assessment without hospitalization. On the other hand, it can provide services in a multidisciplinary approach similar to institution but without additional costs. Hui et al reported that the cost of day hospital treatment in Hong Kong was found to be much cheaper than an equivalent period of inpatient rehabilitation.19 The difference in costing was mainly due to the manpower allocation. In GDH, more allied health but less nursing manpower was recruited and it only opened in daytime. The current study demonstrated that most of geriatric hip fracture patients benefited after rehabilitation in GDH in terms of physical outcomes (BI and EMS; P < .000) and cognitive outcomes (MMSE; P < .000).
There were few published studies on postoperative hip fracture rehabilitation using RE. Recently, Tan et al reported that the mean RE of postoperative hip fracture rehabilitation in a community hospital was 40.4 (26.3).20 From our study, the mean RE by BI was 22.5 (66.6). One possibility relative low percentage is that our study had slightly older patients (>50% between 80 and 89 years). On the other hand, most of our patients had higher BI on admission (>50% between 61 and 100).
In bivariate analysis, older age patients and poor functional scores (both BI and EMS) on admission were associated with poor outcome on RE by BI. On the other hand, premorbid ambulatory status and poor functional scores (both BI and EMS) on admission were associated with poor outcome on RE by EMS. Elderly Mobility Scale is mainly used for assessment of patients’ ambulatory status and it is significantly more likely to detect improvement in mobility than the BI, and the magnitude of detected improvement is significantly greater using EMS.21 However, BI is a measurement of patients’ ADLs, not only mobility but also the level of independence. We hypothesized that patients with localized diseases affecting walking ability might have poor EMS, but overall ADLs might not be affected. Similarly, age is one of significant predictors of ADL independence among older adults.22 Comorbidities, gender, and cognitive status on admission were not associated with the outcomes on RE (P > .05), and these findings were similar to other studies.23–27 In multivariate analysis (Table 7), advanced age is the only independent predictor of poorer RE by BI in our study. Previous studies also have showed older age is usually associated with poor functional recovery after a hip fracture.27–29
Table 7.
Multivariate Analysis of RE.
| Variables | RE of BI | RE of EMS | RE of MMSE | |||
|---|---|---|---|---|---|---|
| β Coefficient | P Value | β Coefficient | P Value | β Coefficient | P Value | |
| Gender | 15.723 | .192 | −7.705 | .177 | 3.091 | .626 |
| Age (old [≥90] vs young [<90]) | −25.238 | .009* | −5.326 | .238 | −2.253 | .650 |
| Premorbid ambulation status (without aid vs with aid) | −10.325 | .289 | −4.245 | .359 | .133 | .979 |
| CCI (high vs low) | −2.328 | .700 | 1.048 | .716 | 2.560 | .421 |
| Smoking status | −21.989 | .077 | 4.069 | .502 | .058 | .993 |
| Use of bisphosphonate | 21.773 | .077 | 5.890 | .328 | 9.058 | .173 |
| Length of stay | 2.203 | .842 | −3.554 | .503 | −2.891 | .617 |
| BI on admission (low vs high) | −3.511 | .660 | −8.033 | .025* | 4.207 | .293 |
| EMS on admission (low vs high) | −12.595 | .073 | −8.821 | .010* | −8.084 | .433 |
| MMSE on admission (low vs high) | −0.757 | .915 | −0.645 | .848 | 0.639 | .864 |
Abbreviations: BI, Barthel Index; CCI, Charlson Comorbidity Index; EMS, Elderly Mobility Score; MMSE, Mini-Mental State Examination; RE, rehabilitation effectiveness.
*Significant difference because P value < 0.05.
The 1-year mortality of the current study was 4.7% (n = 12), which was much lower than the average 1-year mortality rate in Hong Kong (around 25%).30,31 This further confirmed the effectiveness of rehabilitation in GDH. Male patients showed higher risks of death (odds ratio [OR] = 4.5; P = .04) and readmission at 6 months (OR = 4.2; P = .041). This finding was similar to other studies.30,31 Ekstrom et al reported that men with hip fracture usually has a poorer comorbidity before surgery and has higher mortality than women.32 The readmission rates at 6 months were 10.3% (n = 26). The rate of readmission at 6 months was 10.3%, which was lower than the figures in other published hip rehabilitation literature.1,8
Limitations
There are some limitations in this study. Firstly, those patients attending GDH for rehabilitation were selected by doctors in acute hospital. As a result, there was a bias during the selection of patients. Secondly, in order to prove the effectiveness of day program provided by GDH, it was much better to compare patients with and without attending GDH; however, there were no data about patients who did not attend GDH. Another issue was that readmission specialties were recorded, while exact diseases for readmission were not. The numbers of patients died within 12 months (n = 12) and rehospitalized within 6 months (n = 26) were small, which was an evidence for the effectiveness of GDH. However, the relatively small sample size of death and rehospitalization would deteriorate the accuracy of statistical analysis for mortality and rehospitalization risk factors. The RE method showed some deficiency in evaluating patients with decreased functions after rehabilitation. The RE value could be smaller than −100%, which made the variation extremely large.
Future Plan
All GDHs in Hong Kong should be recruited for future study in order to see whether each GDH is cost-effective in geriatric hip fracture rehabilitation. On the other hand, the data generated can help setting up a standard protocol for geriatric hip fracture rehabilitation in all GDH in order to maximize the effectiveness of rehabilitation in GDHs with limited resources, thereby decrease the burden to our social economic system.
Conclusion
Our study showed that postoperative geriatric hip fracture patients definitely could benefit from rehabilitation service offered by one of our GDH in Hong Kong in terms of functional and cognitive outcomes. According to our study, age was the most important factor in determining the functional outcomes after rehabilitation. The current study showed the preadmission cognitive status did not affect the functional outcomes at discharge. Gender was the only risk factor for 12-month mortality and 6-month readmission.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was supported by a grant from the Health and Medical Research Fund, Hong Kong, No 12133551.
References
- 1. Ottenbacher KJ, Smith PM, Illig SB, Peek MK, Fiedler RC, Granger CV. Hospital readmission of persons with hip fracture following medical rehabilitation. Arch Gerontol Geriatr. 2003;36(1):15–22. [DOI] [PubMed] [Google Scholar]
- 2. French DD, Bass E, Bradham DD, Campbell RR, Rubenstein LZ. Rehospitalization after hip fracture: predictors and prognosis from a national veterans study. J Am Geriatr Soc. 2008;56(4):705–710. [DOI] [PubMed] [Google Scholar]
- 3. Sloan FA, Taylor DH, Jr, Picone G. Costs and outcomes of hip fracture and stroke, 1984 to 1994. Am J Public Health. 1999. June;89(6):935–937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Buecking B, Eschbach D, Koutras C, et al. Readmission to level 2 unit after hip fracture surgery-risk factor for reasons and outcome. Injury. 2013;44(12):1919–1925. [DOI] [PubMed] [Google Scholar]
- 5. Roche JJ, Wenn RT, Sahota O, Moran CG. Effect of comorbidities and postoperative complications on mortality after hip fracture in elderly people: prospective observational cohort study. BMJ. 2005;331(7529):1374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Brauer CA, Coca-Perraillon M, Cutler DM, Rosen AB. Incidence and mortality of hip fractures in the United States. JAMA. 2009;302(14):1573–1579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Deschodt M, Braes T, Broos P, et al. Effect of an inpatient geriatric consultation team on functional outcome, mortality, institutionalization, and readmission rate in older adults with hip fracture: a controlled trial. J Am Geriatr Soc. 2011;59(7):1299–1308. [DOI] [PubMed] [Google Scholar]
- 8. Gregersen M, Morch MM, Hougaard K, Damsgaard EM. Geriatric intervention in elderly patients with hip fracture in an orthopedic ward. J Inj Violence Res. 2012;4(2):45–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gregersen M, Zintchouk D, Borris LC, Damsgaard EM. A geriatric multidisciplinary and tailor-made hospital-at-home method in nursing home residents with hip fracture. Geriatr Orthop Surg Rehabil. 2011;2(4):148–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Texeira A, Trinquart L, Raphael M, Bastianic T, Chatellier G, Holstein J. Outcomes in older patients after surgical treatment for hip fracture: a new approach to characterise the link between readmissions and the surgical stay. Age Ageing. 2009;38(5):584–589. [DOI] [PubMed] [Google Scholar]
- 11. Dy CJ, Dossous PM, Ton QV, Hollenberg JP, Lorich DG, Lane JM. The medical orthopaedic trauma service: an innovative multidisciplinary team model that decreased in-hospital complications in patients with hip fractures. J Orthop Trauma. 2012;26(6):379–383. [DOI] [PubMed] [Google Scholar]
- 12. Friedman SM, Mendelson DA, Bingham KW, Kates SL. Impact of a comanaged Geriatric Fracture Center on short-term hip fracture outcomes. Arch Intern Med. 2009;169(18):1712–1717. [DOI] [PubMed] [Google Scholar]
- 13. Kates SL, Mendelson DA, Friedman SM. The value of an organized fracture program for the elderly: early results. J Orthop Trauma. 2011;25(4):233–237. [DOI] [PubMed] [Google Scholar]
- 14. Luk JK, Chan CF. Rehabilitation outcomes of older patients at 6 months follow up after discharged from a geriatric day hospital (GDH). Arch Gerontol Geriatr. 2011;52(3):327–330. [DOI] [PubMed] [Google Scholar]
- 15. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic co-morbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. [DOI] [PubMed] [Google Scholar]
- 16. Shah S, Vanclay F, Cooper B. Efficiency, effectiveness, and duration of stroke rehabilitation. Stroke. 1990;21(2):241–246. [DOI] [PubMed] [Google Scholar]
- 17. Heinemann A, Roth EJ, Cichowski K, Betts HB. Multivariate analysis of improvement and outcome following stroke rehabilitation. Arch Neurol. 1987;44(11):1167–1172. [DOI] [PubMed] [Google Scholar]
- 18. Córcoles-Jiménez MP, Ruiz-García MV, Saiz-Vinuesa MD, et al. Hospitalisation as a risk for functional decline in older adults. Enferm Clin. 2016;26(2):121–128. [DOI] [PubMed] [Google Scholar]
- 19. Hui E, Woo J, Or KH, Chu LW, Wong KH. A geriatric day hospital in Hong Kong: an analysis of activities and costs. Disabil Rehabil. 1995;17(8):418–423. [DOI] [PubMed] [Google Scholar]
- 20. Tan AK, Taiju R, Menon EB, Koh GC. Postoperated hip fracture rehabilitation effectiveness and efficiency in a community hospital. Ann Acad Med Singapore. 2014;43(4):209–215. [PubMed] [Google Scholar]
- 21. Spilg EG, Martin BJ, Mitchell SL, Aitchison TC. A comparison of mobility assessments in a geriatric day hospital. Clin Rehabil. 2001;15(3):296–300. [DOI] [PubMed] [Google Scholar]
- 22. Chen SW, Chippendale T. Factors associated with IADL independence: implications for OT practice. Scand J Occup Ther. 2017;24(2):109–115. [DOI] [PubMed] [Google Scholar]
- 23. Lieberman D. Rehabilitation following hip fracture surgery: a comparative study of females and males. Disabil Rehabil. 2004;26(2):85–90. [DOI] [PubMed] [Google Scholar]
- 24. Hawkes WG, Wehren L, Orwig D, Hebel JR, Magaziner J. Gender differences in functioning after hip fracture. J Gerontol A Biol Sci Med Sci. 2006;61(5):495–499. [DOI] [PubMed] [Google Scholar]
- 25. Endo Y, Aharonoff GB, Zuckerman JD, Egol KA, Koval KJ. Gender differences in patients with hip fracture: a greater risk of morbidity and mortality in men. J Orthop Trauma. 2005;19(5):29–35. [DOI] [PubMed] [Google Scholar]
- 26. Luk JK, Chan CF, Chan FH, Chu LW. Rehabilitation outcomes of older Chinese patients with different cognitive function in a geriatric day hospital. Arch Gerontol Geriatr. 2011;53(2):e144–e148. [DOI] [PubMed] [Google Scholar]
- 27. Vergara I, Vrotsou K, Orive M, Gonzalez N, Garcia S, Quintana JM. Factors related to functional prognosis in elderly patients after accidental hip fracture: a prospective cohort study. BMC Geriatr. 2014;14:124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Cobeu JC, Cobey JH, Conant L. Indicators of recovery from fractures if the hip. Clin Orthop Relat Res. 1976;(117):258–262. [PubMed] [Google Scholar]
- 29. Magaziner J, Simonsick EM, Kashner TM. Predictors of functional recovery one year following hospital discharge for hip fracture: a prospective study. J Gerontol. 1990;45(3):M101–M107. [DOI] [PubMed] [Google Scholar]
- 30. Chau PH, Wong M, Lee A, Ling M, Woo J. Trends in hip fracture incidence and mortality in Chinese population from Hong Kong 2001-09. Age Ageing. 2013;42(2):229–233. [DOI] [PubMed] [Google Scholar]
- 31. Cheung MY, Ho AW, Wong SH. Operative outcome of Hong Kong centenarians with hip fracture. Hong Kong Med J. 2017;23(1):63–66. [DOI] [PubMed] [Google Scholar]
- 32. Ekstrom W, Samuelsson B, Ponzer S, Cederholm T, Thorngre KG, Hedstrom M. Sex effects on short-term complications after hip fracture: a prospective cohort study. Clin Interv Aging. 2015;10:1259–1266. [DOI] [PMC free article] [PubMed] [Google Scholar]