Abstract
Objective:
To identify clinical or demographic variables that influence long-term mortality, as well as in-hospital mortality, with a particular focus on the effects of age.
Summary and Background Data:
Cervical spine fractures with or without spinal cord injury (SCI) disproportionately impact the elderly who constitute an increasing percentage of the US population.
Methods:
We analyzed data collected for 10 years at a state-designated level I trauma center to identify variables that influenced in-hospital and long-term mortality among elderly patients with traumatic cervical spine fracture with or without SCI. Acute in-hospital mortality was determined from hospital records and long-term mortality within the study period (2003-2013) was determined from the National Death Index. Univariate and multivariate regression analyses were used to identify factors influencing survival.
Results:
Data from patients (N = 632) with cervical spine fractures were analyzed, the majority (66%) of whom were geriatric (older than age 64). Most patients (62%) had a mild/moderate injury severity score (ISS; median, interquartile range: 6, 5). Patients with SCI had significantly longer lengths of stay (14.1 days), days on a ventilator (3.5 days), and higher ISS (14.9) than patients without SCI (P < .0001 for all). Falls were the leading mechanism of injury for patients older than age 64. Univariate analysis identified that long-term survival decreased significantly for all patients older than age 65 (hazard ratio [HR]: 1.07; P < .0001). Multivariate analysis demonstrated age (HR: 1.08; P < .0001), gender (HR: 1.60; P < .0007), and SCI status (HR: 1.45, P < .02) significantly influenced survival during the study period.
Conclusion:
This study identified age, gender, and SCI status as significant variables for this study population influencing long-term survival among patients with cervical spine fractures. Our results support the growing notion that cervical spine injuries in geriatric patients with trauma may warrant additional research.
Keywords: spine, cervical spine, fracture, geriatric, spinal cord injury, mortality
Introduction
Within the United States, the percentage of people older than 65 years of age is increasing due to improved health care and life expectancy.1 Cervical spine fractures with and without spinal cord injury (SCI) disproportionately impact the elderly, leading to longer hospital lengths of stay, poor functional outcomes, lower quality of life, and increased mortality.2–8 Recent analyses of data from 488, 262 patients in the US National Inpatient Sample found that the number of traumatic cervical fractures has increased from 2005 to 2013, with >57 000 cases in 2013, with Medicare listed as the insurer for 42% of those cases.9
For persons with traumatic spinal cord injuries, the average age at onset has risen to 42.2 years, which is due to a higher incidence among persons older than age 65.10 Many studies have determined that falls have become the most common mechanism of injury (MOI) for cervical spine fracture with or without SCI for patients older than 45 years.3,7,9,10 Among geriatric (>65 years of age) patients with cervical spine fractures with SCI, the in-hospital mortality rates typically range from 7.5% (from 2010 to 2012) to 11% (from 2001 to 2011).7,11 Mortality rates at 1 year from initial injury range from 26% to 100%, depending on the neurological completeness of injury and comorbidities.6,7 Given the increasing age of patients with cervical fractures, the influence of age on their in-hospital mortality is a topic of current investigation. For example, at a regional trauma center, Martin and colleagues found that in-hospital mortality was higher for patients with cervical SCI older than age 75.12
Much less is known about long-term mortality in geriatric patients with cervical spine fracture, with or without SCI. Here, the goal was to use data collected from a large number of patients with cervical spine fracture treated over a 10-year period at a New York State–designated level I trauma center to identify clinical or demographic variables that influence long-term mortality, as well as in-hospital mortality, with a particular focus on the effects of age.
Methods
Study Design and Cohort Characteristics
This retrospective cohort study was approved by the local institutional review board. Inclusion criteria for patients admitted over a 10-year period (January 1, 2003, to December 31, 2013) to the state-designated level I trauma center were ≥18 years of age, International Classification of Diseases, 9th revision (ICD)-9 codes 806, 952, 805.0 to 805.1, corresponding to fracture of the cervical vertebral column with SCI, SCI without evidence of spinal bone injury, and fracture of the cervical vertebral column without SCI. Clinical and demographic data were abstracted retrospectively from a prospectively collected Trauma Registry (“Trauma One,” Version 4.11, Lancet Technology, Boston, Massachusetts) and from medical records. Neurologic level of injury was classified as high (C1-4), low (C5-C7), multiple levels (C1-C7), or unspecified cervical levels as indicated by the available ICD-9 code in the Trauma Registry. Data analyzed included medical diagnoses prior to injury, MOI, hospital length of stay (LOS), ventilator use, Glasgow Coma Scale (GCS) scores, and discharge disposition. We also analyzed injury severity scores (ISS), which were calculated using the AIS-90 system, (TraumaOne; Lancet Technology, Boston, MA, USA) and defined as severe (>15), moderate (9-15), or mild (<9). The GCS scores were defined as severe (≤8), moderate (9-12), or mild (≥13) head injury. Patients with severe traumatic brain injury, indicated by GCS score, were excluded from our analysis, as this would confound our interpretation of the influence of SCI on mortality. Preinjury medical comorbidities were classified by the Charlson Comorbidity Index (CCI) as done previously by Furlan and Fehlings.6,13 Survival after acute hospitalization during the remainder of the study period was determined by data obtained from the US National Death Index (NDI), part of the National Center for Health Statistics.
Statistical Analysis
Descriptive statistics and analyses were generated using SAS (Version 9.3, SAS Institute Inc., Cary, North Carolina). To detect associations between categorical variables, data were examined using χ2 or Fisher exact test. For continuous variables, either t tests or Mann-Whitney U tests were used, as appropriate. The Kaplan-Meier product limit method was used to estimate patient survival and the log rank test was used to compare survival between the groups. Factors specified as being clinically important a priori (age, gender, and SCI) along with those factors found to be associated with survival in a univariate screen using Cox regression (P < .05), were included in a multivariate Cox regression in order to examine the joint effects of those factors on survival, to estimate adjusted hazard ratios (HRs) and their corresponding 95% confidence intervals (CIs). A backward selection algorithm was applied in order to arrive at a parsimonious model, removing variables that did not contribute significant information to the model. For descriptive purposes only, survival analysis was performed using data from patients binned by age-group (Figure 1), and Hall-Wellner 95% confidence bands are indicated.14
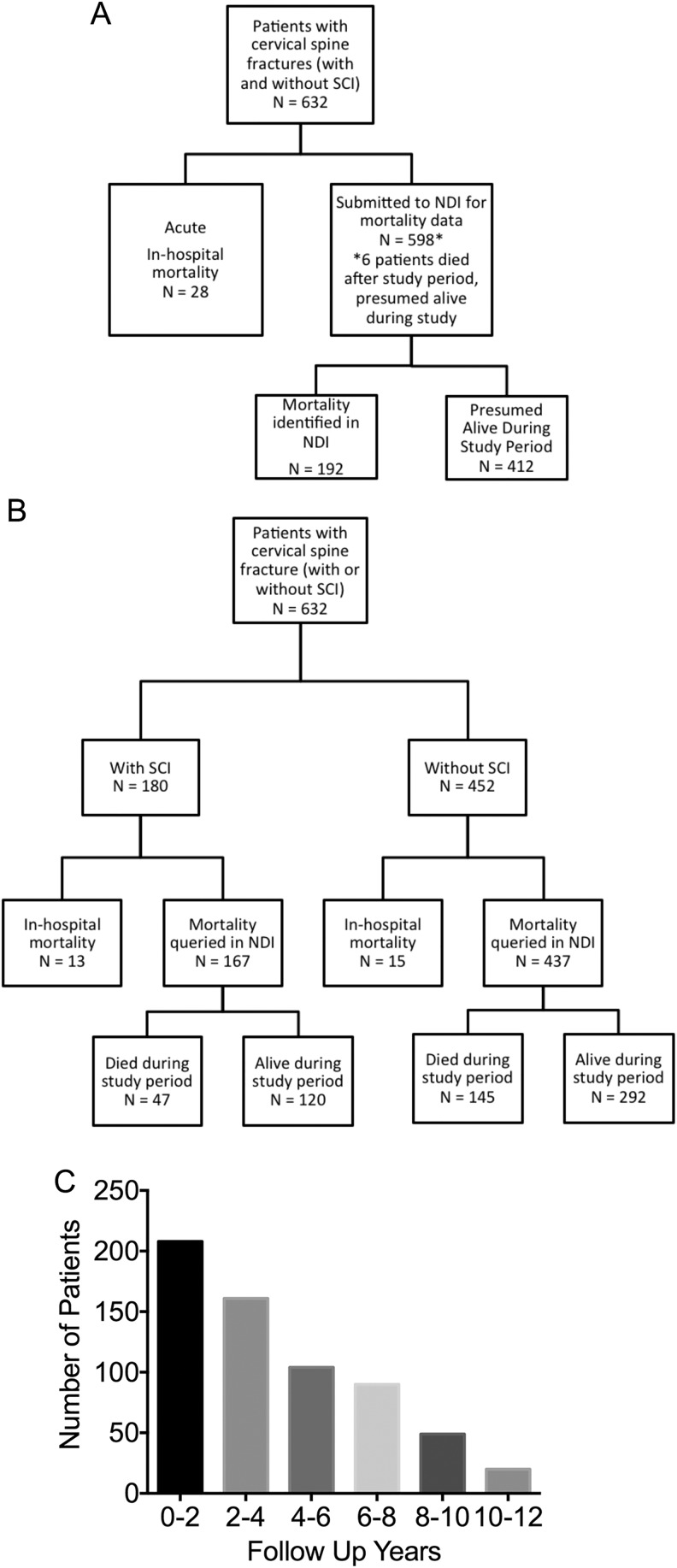
Figure 1.
Consort diagram of the study population. A. Stratification of patients with cervical spine fracture in study cohort. B. Stratification of patients with cervical spine fracture by spinal cord injury status. C. Number of patients whose survival was followed over time by years.
Results
A total of 632 adults meeting eligibility criteria were admitted to our state-designated level I trauma center during the 10-year period of interest (January 1, 2003, to December 31, 2012; Table 1, Figure 1A and B). The number of years of patient follow-up after discharge is shown in Figure 1C.
Table 1.
Clinical and Demographic Characteristics of Study Cohort Stratified by Age-Group.
| Study Population | Age Groups, years | N (%) | |||
|---|---|---|---|---|---|
| <65 | 65-84 | ≥85 | Total | ||
| Number of cases | 212 (34) | 253 (40) | 167 (26) | 632 (100) | |
| Age range, years | 18-101 (min-max) | ||||
| Gender (% of category) | Male | 134 (63) | 123 (49) | 63 (38) | 320 (51) |
| Female | 78 (37) | 130 (51) | 104 (62) | 312 (49) | |
| Race (% of category) | White | 157 (74) | 211 (84) | 157 (94) | 525 (83) |
| Non-white | 55 (26) | 41 (16) | 10 (6) | 106 (17) | |
| Injury (% of category) | Fracture with SCI | 88 (42) | 70 (28) | 22 (13) | 180 (28.5) |
| Fracture without SCI | 124 (58) | 183 (72) | 145 (87) | 452 (71.5) | |
| Mechanism of injury (% of category) | Fall | 86 (41) | 210 (83) | 155 (93) | 451 (71) |
| MVA | 98 (46) | 41 (16) | 12 (7) | 151 (24) | |
| Violence | 5 (2) | 0 (0) | 0 (0) | 5 (0.8) | |
| Sports | 19 (9) | 2 (1) | 0 (0) | 21 (3.3) | |
| Other | 4 (1.9) | 0 (0) | 0 (0) | 4 (0.6) | |
| Cervical level of injury (% of category) | C1-C4 | 79 (37.6) | 166 (66) | 131 (76.6) | 376 (59) |
| C5- C7 | 95 (45.2) | 56 (22) | 21 (12.3) | 172 (27) | |
| C1-C7 (multiple levels) | 15 (7.1) | 16 (6.4) | 9 (5.3) | 40 (6) | |
| Unspecified cervical levels | 21 (10) | 13 (5.2) | 10 (5.8) | 44 (7) | |
| ISS (% of category) | Mild/moderate (0-14) | 170 (80) | 215 (85) | 155 (93) | 540 (85) |
| Severe (> −15) | 42 (20) | 37 (15) | 12 (7) | 91 (15) | |
| GCS (≤8 were excluded) | Mean ± SEM | 14.8 ± 0.1 | 14.6 ± 0.1 | 14 .8 ± 0.1 | 14.7 ± 0.1 |
| Hospital LOS, days | Mean ± SEM | 10.5 ± 1.3 | 10.8 ± 0.7 | 8.8 ± 0.9 | 10.1 ± 0.6 |
| Days on ventilator | Mean ± SEM | 1.7 ± 0.5 | 1.8 ± 0.4 | 0.6 ± 0.3 | 1.4 ± 0.2 |
| Charlson Comorbidity Index (CCI), % of category | 0-2 | 205 (97) | 239 (94) | 152 (91) | 596 (94) |
| >3 | 7 (3) | 14 (0.1) | 15 (9) | 36 (6) | |
| Insurance, % of category | Medicare | 8 (4) | 196 (77) | 155 (93) | 359 (57) |
| Commercial | 158 (75) | 53 (21) | 11 (7) | 222 (35) | |
| Self-Pay | 46 (22) | 4 (2) | 1 (1) | 51 (8) | |
| Discharge disposition, % of category | Home | 164 (77) | 118 (47) | 42 (25) | 324 (51) |
| Rehabilitation | 46 (22) | 125 (49) | 109 (65) | 279 (44) | |
| Mortality, % of category | Acute in-hospital | 3 (1.4) | 10 (4) | 15 (9) | 28 (4) |
Abbreviations: GCS, Glasgow Coma Scale; ISS, injury severity scores; LOS, length of stay; MVA, motor vehicle accident; SCI, spinal cord injury; SEM, standard error of the mean.
The median age of all patients was 77 (range 18-101) years, and 66% were at least 65 years of age. Almost equal percentages of males (51%) and females (49%) were included in the study. The majority (83%) of patients included were white. The majority (71%) of patients had cervical spine fractures without SCI, and a minority (28.5%) had cervical spine fractures with SCI. Falls were the most common MOI (71% of all patients), followed by motor vehicle accident (MVA). Most (59%) patients had a cervical spine fracture at levels C1 to C4 (Table 1). The ISS was mild/moderate for 85% of all patients, and per exclusion criteria, the average GCS was 14.7 ± 0.01 (mean ± standard error of the mean [SEM]). Ventilator support was used in less than 2% of all patients. As done by Furlan and Fehlings, we used the CCI to compare major comorbidity burden across age-groups.6,13 Most (94%) patients had a CCI of 0 to 2. Consistent with the age of the study population, 92% of patients had their medical expenses paid either by Medicare or by commercial insurance (Table 1). Approximately half of all patients were discharged home. Acute in-hospital mortality was 4% across all patients (Table 1).
To investigate potential correlations between age and other clinical and demographic variables in this cohort, we compared patients by age-group at the time of cervical spine fracture: (1) younger than 65 years, (2) 65 to 84 years, or (3) at least 85 years. We determined 34% were younger than 65 years, 40% were 65 to 84 years, and 26% of patients were at least 85 years (Table 1). As expected, the percentage of injuries due to falls increased with age: 41% in persons younger than 65 years, 83% in persons 65 to 84 years, and 93% in persons at least 85 years. The MVA was the next most common MOI, which declined with age-group. In each age-group, a minority of patients had cervical fractures with SCI. Consistent with observation that the frequency of falls increases with age and falls incur low-velocity injuries, the percentage of patients with SCI declined with age: 42% in persons younger than 65 years, 28% in persons 65 to 85 years, and 13% in persons ≥85 years (Table 1; P = .0001 χ2). Conversely, the proportion of patients with mild/moderate ISS scores increased with age: 80% in persons younger than 65 years, 85% in persons 65 to 84 years, and 93% in persons at least 85 years (Table 1, P = .0024 χ2).
Within each age-group, we next determined the number of comorbidities reflected by CCI scores as done previously.6 Most patients had 0 to 2 comorbid conditions categorized by the CCI, and the CCI was not statistically significant by age-group (P = .59, χ2): 97% in patients younger than age 65 years, 94% in patients 65 to 84 years, and 91% in patients ≥85 years old. Hospital LOS (10.1 ± 0.6 days, mean ± SEM), and the number of days on ventilator (1.4 ± 0.2 days, mean ± SEM) were similar among persons in all age-groups (Table 1). Discharge dispositions for patients were either home (with or without services) or to a rehabilitation facility. For patients younger than age 65 years, 77% were discharged home and 22% were discharged to a rehabilitation unit (1.4% died in hospital). For persons 65 to 85 years old, 47% were discharged home and 49% to rehabilitation unit or facility (4% died in hospital). For patients ≥85 years of age, 25% were discharged home and 65% to rehabilitation unit or facility (9% died in hospital). Among persons younger than 65 years old, 91% survived during study period. For persons aged 65 to 84 years old, 56% survived during the study period. For persons ≥85 years old, 30% survived during study period (Table 1).
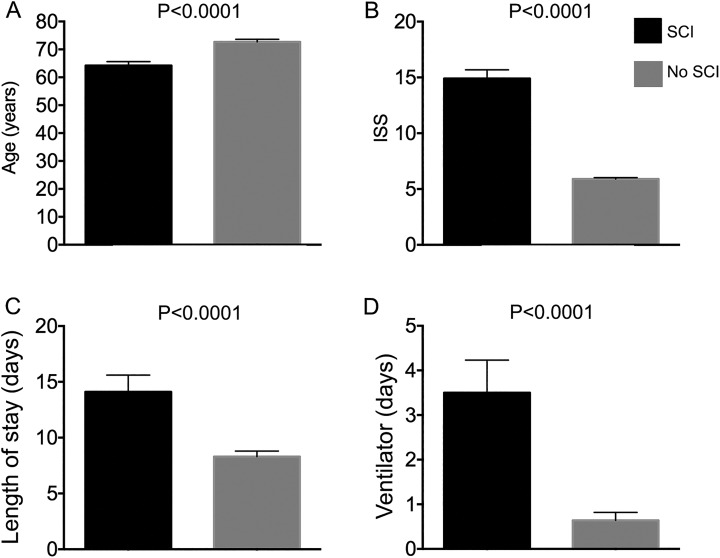
In order to explore correlations of SCI with other clinical and demographic variables, data were next stratified by SCI status (Table 2). As mentioned earlier, 28.5% of patients with cervical spine fractures had a SCI, and the percentage ranged from 20.5% to 54% for any given year of the study. Males accounted for 62% of patients with cervical spine fractures with SCI and 46% without SCI. At the time of hospital admission, the mean age of patients without SCI was older than with SCI (P < .0001; Figure 2A). Falls was the most common MOI for patients with or without SCI as expected. Also as expected, ISS was significantly higher in patients with versus without SCI (14.9 vs. 5.9, P < .0001; Figure 2B) as was hospital LOS (14.1 vs 8.3, P < .0001; Figure 2C) and days with ventilator assistance (3.5 vs 0.64, P < .0001; Figure 2D). The GCS and CCI scores did not differ significantly by SCI status. The primary discharge disposition for patients both with and without SCI was home (49% vs 53%) followed by rehabilitation.
Table 2.
Clinical and Demographic Characteristics of Study Cohort Stratified by SCI Status.
| Characteristics | Fracture With SCI | Fracture Without SCI |
|---|---|---|
| N (% of total) | 180 (28.5%) | 452 (71.5%) |
| Males, n (% of column variable) | 111 (62) | 209 (46) |
| Mechanism of injury, n (% of column variable) | ||
| Fall | 118 (66) | 333 (74) |
| MVA | 52 (29) | 99 (22) |
| Violence | 8 (4) | 13 (3) |
| Sports | 0 (0) | 5 (1) |
| Other | 2 (1) | 2 (0.4) |
| Level of injury, n (% of column variable) | ||
| C1-C4 | 80 (45) | 290 (64) |
| C5-C7 | 67 (37) | 115 (26) |
| C1-C7 or multiple cervical levels | 26 (14) | 10 (2) |
| Unspecified cervical levels | 7 (4) | 37 (8) |
| Glasgow Coma Scale (GCS), mean ± SEM | 14.3 ± 0.2 | 14.9 ± 0.3 |
| Charlson Comorbidity Index (CCI), N (% of column variable) | ||
| 0-2 | 171 (95) | 425 (94) |
| ≥3 | 9 (5) | 27 (6) |
| Acute hospital length of stay (LOS) | days (range), 8 (2-198) | days (range), 5 (1-123) |
| Discharge disposition, n (% of column variable) | ||
| Home | 88 (49) | 237 (53) |
| Rehabilitation | 79 (44) | 200 (44) |
| Acute in-hospital death | 13 (7) | 15 (3) |
Abbreviations: MVA, motor vehicle accident; SEM, standard error of the mean.
Figure 2.
Clinical features of patients with and without spinal cord injury. A, Age at acute hospitalization admission. B, Injury severity score (ISS) at acute hospitalization admission. C, Length of stay during acute hospitalization. D, Days on ventilator during acute hospitalization.
Acute in-hospital mortality was less than 10% for all patients: 7% for SCI and 3% for without SCI (Tables 1–2). As expected, the percentage of patients with in-hospital mortality increased with age: 0.47% in persons younger than 65 years, 1.58% in persons 65 to 85 years, and 2.37% in persons ≥85 years (Tables 1 and 3). Of patients with in-hospital mortality, 64% were male, and the most common MOI was falls (Table 3). As expected, in-hospital mortality was higher for the group with severe ISS scores (Table 3).
Table 3.
Clinical and Demographic Characteristics of Patients With Acute In-Hospital Mortality.
| Age-groups, years | N (% age-group, % total) |
|---|---|
| <65 | 3, (1.42, 0.47) |
| 65-84 | 10 (4, 1.58) |
| ≥ 85 | 15 (9, 2.37) |
| Total | 28 |
| Gender | N (% died, % total) |
| Male | 18 (64.3, 2.85) |
| MOI | N (% of MOI, % total) |
| Fall | 24 (5.32, 3.8) |
| MVA | 4 (2.65, 0.63) |
| Other | 0 |
| ISS | N (% of ISS group, % total) |
| Mild/moderate (0-14) | 19, (3.5, 3) |
| Severe (> 15) | 9, (9.9, 1.4) |
| SCI status | N (% of group, % of total) |
| SCI | 13 (7, 2) |
| No SCI | 15 (3, 2.4) |
Abbreviations: MOI, mechanism of injury; MVA, motor vehicle accident; ISS, injury severity scores; SCI, spinal cord injury.
To determine whether there were differences in survival between patients with cervical spine fracture with or without SCI after acute hospitalization but during the study period, the NDI was searched for data from the 95.5% of patients (n = 604) who survived acute hospitalization. Most (68%) patients were alive during the entire study period, while a record of death for 32% of patients was identified in the NDI data (Figure 1A). Within the study period, 65% of patients with cervical spine fractures without SCI survived as did 67% of patients with cervical spine fractures with SCI (Figure 1B). The average follow-up beyond acute hospitalization in the study was 63.56 months ± 1.554 (mean ± SEM) or 5.29 years (Figure 1C). We examined the age distribution of participants during the course of the study and found that from its initiation to completion, the percentage of total patients with cervical spine fractures (with or without SCI) rose from 5.38 to 12.97% (Table 4).
Table 4.
Number of Patients in Cohort Admitted Each Study Year Stratified by Age-Group.
| Age-Groups | ||||||
|---|---|---|---|---|---|---|
| Study Population | Years | <65 (% of total) | 65-84 (% of total) | ≥85 (% of total) | N ≥ 65 for year (% of year N) | N for year (% of total N = 632) |
| Study year | 2003 | 16 (2.5) | 12 (1.9) | 6 (0.95) | 18 (53) | 34 (5.38) |
| 2004 | 23 (3.6) | 15 (2.4) | 8 (1.3) | 23 (50) | 46 (7.28) | |
| 2005 | 14 (2.2) | 17 (2.7) | 10 (1.6) | 27 (66) | 41 (6.49) | |
| 2006 | 19 (3.0) | 20 (3.2) | 9 (1.42) | 29 (60) | 48 (7.59) | |
| 2007 | 23 (3.6) | 35 (5.5) | 16 (2.5) | 51 (69) | 74 (11.71) | |
| 2008 | 20 (3.2) | 26 (4.1) | 17 (2.69) | 43 (69) | 63 (9.97) | |
| 2009 | 13 (2.0) | 37 (5.8) | 24 (3.8) | 61 (82) | 74 (11.7) | |
| 2010 | 24 (3.8) | 34 (5.4) | 24 (3.8) | 58 (71) | 82 (12.97) | |
| 2011 | 33 (5.2) | 28 (4.4) | 27 (4.2) | 55 (63) | 88 (13.92) | |
| 2012 | 27 (4.3) | 29 (4.6) | 26 (4.1) | 55 (67) | 82 (12.97) | |
| Total | 212 (34) | 253 (40) | 167 (26) | 420 (66) | 632 | |
For the remaining study period beyond acute hospitalization, we performed a univariate screen of the influence of individual clinical and demographic variables on survival. Specifically, we screened for effects of age, gender, SCI status, race, medical insurance provider, and MOI (Table 5). The most significant variables influencing mortality in the univariate model were age (HR: 1.07, 95% CI = 1.06-1.08), race (white, HR: 2.07, CI = 1.32-3.25), Medicare/commercial insurance(HR: 1.32, CI = 2.87-17.0), and MOI falls (HR: 17.49, CI = 2.45-124.8; Table 5). Significant factors were then included in a multivariate regression analysis to test their joint effects on survival. Age (as a continuous variable; HR: 1.08, CI = 1.06-1.09), gender (male; HR: 1.60, CI = 1.22-2.10), or SCI (HR: 1.45, CI =1.06-1.97) were significant predictors of mortality (Table 5, right).
Table 5.
Significant Variables Influencing Survival.
| Univariate Model | Multivariate Model | ||||||
|---|---|---|---|---|---|---|---|
| Variables | Unadjusted Hazard Ratio | 95% CI | P | Variables | Adjusted Hazard Ratio | 95% CI | P |
| Age | 1.07 | 1.06-1.08 | <.0001 | Age | 1.08 | 1.06-1.09 | <.0001 |
| Male | 1.06 | 0.81-1.38 | .668 | Male | 1.60 | 1.22-2.10 | .0007 |
| SCI | 0.86 | 0.64-1.16 | .327 | SCI | 1.45 | 1.06-1.97 | .02 |
| Race: white | 2.07 | 1.32-3.25 | .0015 | ||||
| Insurance: commercial | 1.32 | 0.51-3.39 | .568 | ||||
| Insurance: Medicare | 6.99 | 2.87-17.0 | <.0001 | ||||
| MOI: fall | 17.49 | 2.45-124.8 | .0043 | ||||
| MOI: MVA | 5.34 | 0.725-39.4 | .1001 | ||||
| ISS severe (>15) | 0.90 | 0.608-1.33 | .60 | ||||
Abbreviations: CI, confidence interval; MOI, mechanism of injury; MVA, motor vehicle accident; ISS, injury severity scores; SCI, spinal cord injury.
Discussion
Nationally, the elderly population is increasing, and by 2050, the number of people older than 65 years of age is projected to double.1 Risk factors for mortality among elderly patients with cervical spine fracture (with or without SCI) are of increasing interest.4,15,16 Falls are the most common MOI for persons with SCI and for persons with cervical spine fractures.7–9,17 Trauma resulting from a fall, although a low-velocity MOI, may cause serious injuries in the elderly individuals because of frailty, decreased bone mineral density, and frequent comorbidities.15,18,19 In the case of a trauma that results in a SCI, elderly patients have less functional recovery.6 Many studies have shown previously that age among patients with trauma was associated with increased mortality, which was also related to injury level, severity, and other factors.12,20
Here, we retrospectively analyzed data from 632 cervical spine fracture patients, with 212 who were <65 years old, 253 patients who were 65 to 84 years, and 167 who were older than 85 years (Tables 1, 3, and 4). The study site was located in New York state, where 85.5% of counties exceed the national percentage of population 65 years and over, and 80.6% of counties exceed the national percentage of population 85 years and older.21 In the 2010 US Census, the local county reported 16.7% of residents older than 65 years of age, which is slightly higher than the national average of 15.1%.1,21 It is therefore not surprising that within this study, the percentage of patients aged 65 years and older increased from 5.38% in 2003 to 12.97% in 2012 (Table 4). While acute in-hospitalization mortality in this and other studies is relatively low, it is increasingly of interest to understand what variables may correlate with long-term outcomes in elderly trauma patients.
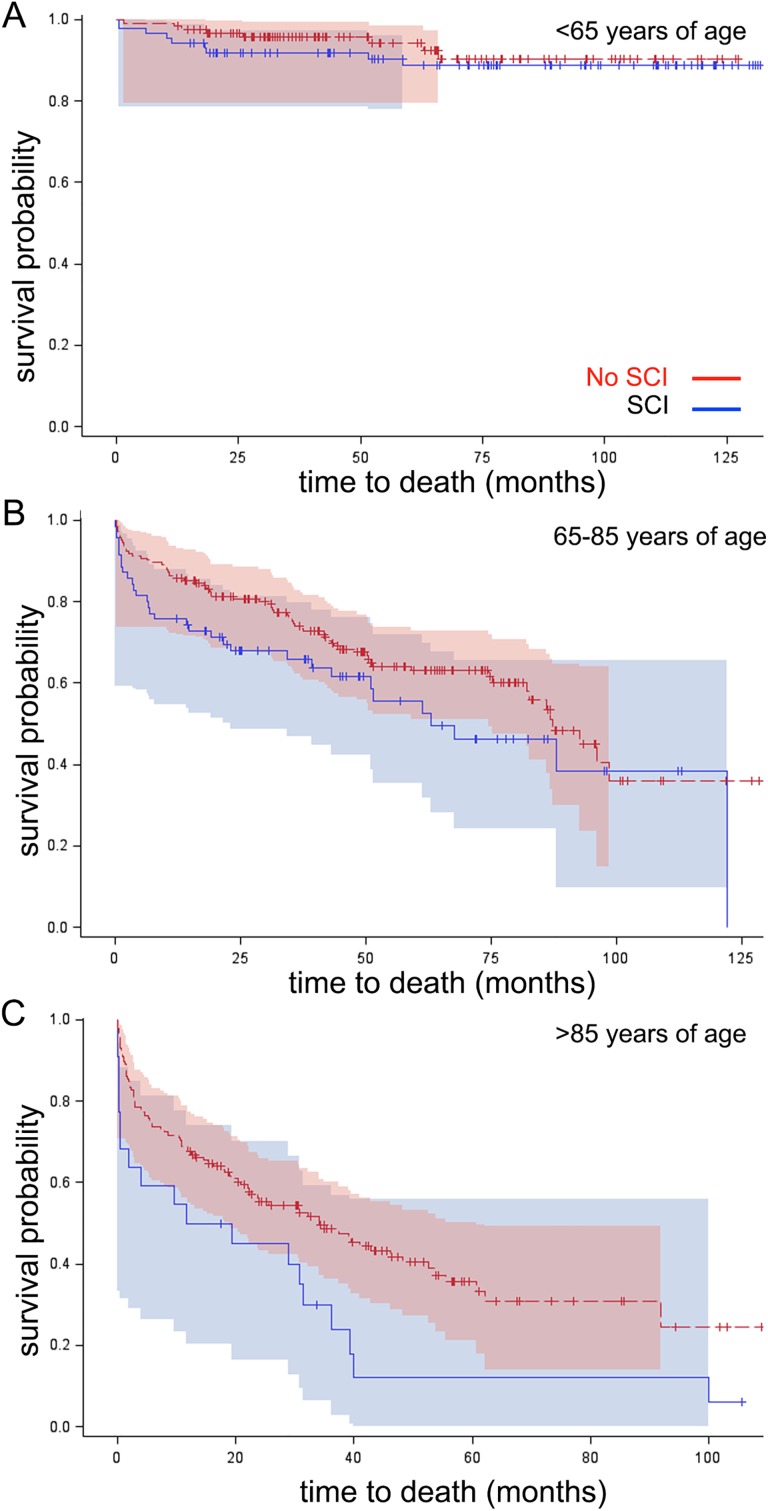
Overall, we had an almost equal gender distribution, while patients with SCI were predominantly male which is consistent with data from that National Spinal Cord Injury Statistical Database.22 In agreement with previous studies, falls constituted the most common etiology of injury among all patients, and consistent with this MOI, the majority of injuries occurred at the C1 to C4 levels (Table 2). The ISS and GCS were mostly mild to moderate also consistent with falls being the most common MOI.11 The consistently low ISS scores limit the value of ISS as a predictor of mortality in this study population. The number of comorbidities as indicated by CCI did not increase with age in our study cohort, but the number was generally low for all participants, consistent with a large study of Medicare patients, where most patients also had a CCI of 0 to 2 (Table 1).23 Recent studies with large samples in the United States and United Kingdom have demonstrated that a change in CCI over time may be a better predictor of long-term mortality than a single baseline measurement as done here.24,25 There are also efforts to improve the predictive power of CCI by refining it or using it in a combinatorial scoring system that incorporates the Elixhauser system.23 In this study, patients with SCI were younger, had higher ISS scores, greater hospital lengths of stay, and greater number of days on a ventilator (Figure 3). In-hospital mortality increased by age-group was higher among males, patients with SCI, and severe ISS (Table 1 and 3). Age-group was not a significant factor influencing mortality when treated as a categorical variable (Figure 3) as found in a neighboring county.19 However, in a univariate screen for factors influencing mortality during the study period, age as a continuous variable, race (white), insurance (Medicare), and MOI (fall) were significant variables influencing long-term survival (Table 5). We recognize that older people are more likely to have Medicare and to sustain their cervical spine fracture as a result of a fall. In a multivariate analysis, age, gender, and SCI status were significant variables influencing long-term survival in patients with cervical spine fracture (Table 5).
Figure 3.
Survival of patients with and without SCI stratified by age group for descriptive purposes, data was binned according to age group, as designated in the figure. Kaplan-Meier curves analyzed by Cox regression show survival probability in months. Shaded regions indicate 95% Hall-Wellner confidence bands. A. Patients younger than age 65. Logrank p=0.4239. B. Patients age 65-85. Logrank p=0.0980. C. Patients older than age 85. Logrank p=0.01113.
There were several strengths to this study: the large number of patients older than 64 (n = 420) years and over than 85 (n = 167) years, the comparisons of patients with cervical spine fractures with and without SCI, and the incorporation of long-term (∼5 years of follow-up) mortality data from the NDI. Despite these strengths, the study had several limitations. A limitation of this study, which is inherent in all longitudinal trauma registry studies, is that data on comorbidities, which are not the main focus of trauma registry registries, may be underestimated. We did not include an analysis of imaging, types of nonsurgical or surgical procedures, or time to surgery, all of which are important factors in traumatic SCI.26–28 For example, a study from the Rick Hansen Spinal Cord Injury Registry in Canada found that patients older than 65 years were less likely to receive acute surgery, and patients older than 70 years experienced a significant delay in time to surgery.29 Rehabilitation (duration, intensity, and type) may also have influenced long-term mortality. We did not have access to consistent data on functional outcomes as indicated by American Spinal Injury Association (ASIA) scale grade or Functional Independence Measure (FIM) scores or to incidence of pneumonia or other infections during hospitalization, which may be related to functional outcomes and mortality.30,31 We also did not have data readily available for transfusion of packed red cells, which has been incorporated into the Geriatric Trauma Outcome Score (GTOS) recently developed.27 However, data thus far have not shown that the GTOS is useful for predicting long-term mortality.32 Data available for discharge status was limited and did not distinguish between home with or without services or between different types of rehabilitation settings. In addition, for the period beyond acute hospitalization, data were not available for causes of death. Despite these limitations, the present study includes a very large number of geriatric trauma patients and highlights the association of increasing age with increased mortality for persons with cervical spine fractures, both with and without SCI. Future prospective studies are needed to ascertain whether treatment algorithms or resource allocation should be stratified by age among patients with traumatic cervical spine fractures.
Footnotes
Authors’ Note: Matthew Bank, Cristina Sison, Adam Stein and Ona Bloom are also affiliated to Zucker School of Medicine at Hofstra Northwell, Hempstead, NY, USA.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: Funding for this study was provided by the New York State Empire Clinical Research Program and by the New York State Spinal Cord Injury Research Board (grants to OB).
References
- 1. Ortman JM, Velkoff VA, Hogan H. An Aging Nation: The Older Population in the United States. Washington, DC: US Census Bureau; 2014. [Google Scholar]
- 2. Chen Y, Tang Y, Allen V, DeVivo MJ. Aging and spinal cord injury: external causes of injury and implications for prevention. Top Spinal Cord Inj Rehabil. 2015;21(3):218–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Chen Y, Tang Y, Vogel LC, Devivo MJ. Causes of spinal cord injury. Top Spinal Cord Inj Rehabil. 2013;19(1):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Daneshvar P, Roffey DM, Brikeet YA, Tsai EC, Bailey CS, Wai EK. Spinal cord injuries related to cervical spine fractures in elderly patients: factors affecting mortality. Spine J. 2013;13(8):862–866. [DOI] [PubMed] [Google Scholar]
- 5. Devivo MJ. Epidemiology of traumatic spinal cord injury: trends and future implications. Spinal Cord. 2012;50(5):365–372. [DOI] [PubMed] [Google Scholar]
- 6. Furlan JC, Fehlings MG. The impact of age on mortality, impairment, and disability among adults with acute traumatic spinal cord injury. J Neurotrauma. 2009;26(10):1707–1717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Jain NB, Ayers GD, Peterson EN, et al. Traumatic spinal cord injury in the United States, 1993-2012. JAMA. 2015;313(22):2236–2243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Golob JF, Claridge JA, Yowler JJ, Como JJ, Reerless JR. Isolated cervical spine fractures in the elderly: a deadliy injury. J Trauma. 2007;64(2):311–315. [DOI] [PubMed] [Google Scholar]
- 9. Passias PG, Poorman GW, Segreto FA, et al. Traumatic fractures of the cervical spine: analysis of changes in incidence, cause, concurrent injuries, and complications among 488,262 patients from 2005 to 2013. World Neurosurg. 2018;110:e427–e437. [DOI] [PubMed] [Google Scholar]
- 10. Chen Y, He Y, DeVivo MJ. Changing demographics and injury profile of new traumatic spinal cord injuries in the United States, 1972-2014. Arch Phys Med Rehabil. 2016;97(10):1610–1619. [DOI] [PubMed] [Google Scholar]
- 11. Poole LM, Le P, Drake RM, Helmer SD, Haan JM. Analysis of patients >/=65 with predominant cervical spine fractures: issues of disposition and dysphagia. J Emerg Trauma Shock. 2017;10(1):13–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Martin ND, Marks JA, Donohue J, Giordano C, Cohen MJ, Weinstein MS. The mortality inflection point for age and acute cervical spinal cord injury. J Trauma. 2011;71(2):380–385;discussion 385-386. [DOI] [PubMed] [Google Scholar]
- 13. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. [DOI] [PubMed] [Google Scholar]
- 14. Hall W, Wellner J. Confidence bands for a survival curve from censored data. Biometrika. 1980;67:133–143. [Google Scholar]
- 15. van Middendorp JJ, Albert TJ, Veth RP, Hosman AJ. Methodological systematic review: mortality in elderly patients with cervical spine injury: a critical appraisal of the reporting of baseline characteristics, follow-up, cause of death, and analysis of risk factors. Spine (Phila Pa 1976). 2010;35(10):1079–1087. [DOI] [PubMed] [Google Scholar]
- 16. Groah SL, Charlifue S, Tate D, et al. Spinal cord injury and aging: challenges and recommendations for future research. Am J Phys Med Rehabil. 2012;91(1):80–93. [DOI] [PubMed] [Google Scholar]
- 17. Chen Y, Tang Y, Allen V, Devivo MJ. Falls-induced spinal cord inury: external causes and implications for prevention. J Spinal Cord Med. 2016;39(1):24–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Bergeron E, Clement J, Lavoie A, et al. A simple fall in the elderly: not so simple. J Trauma. 2006;60(2):268–273. [DOI] [PubMed] [Google Scholar]
- 19. Jawa RS, Singer AJ, Rutigliano DN, et al. Spinal fractures in older adult patients admitted after low-level falls: 10-year incidence and Outcomes. J Am Geriatr Soc. 2016. [DOI] [PubMed] [Google Scholar]
- 20. Caterino JM, Valasek T, Werman HA. Identification of an age cutoff for increased mortality in patients with elderly trauma. Am J Emerg Med. 2010;28(2):151–158. [DOI] [PubMed] [Google Scholar]
- 21. Census U. QuickFacts Nassau County, New York. V2015 2010.
- 22. Center NSCIS. Facts and Figures at a Glance. Birmingham, AL: University of Alabama at Birmingham; 2017. [Google Scholar]
- 23. Gagne JJ, Glynn RJ, Avorn J, Levin R, Schneeweiss S. A combined comorbidity score predicted mortality in elderly patients better than existing scores. J Clin Epidemiol. 2011;64(7):749–759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Fraccaro P, Kontopantelis E, Sperrin M, et al. Predicting mortality from change-over-time in the Charlson Comorbidity Index: a retrospective cohort study in a data-intensive UK health system. Medicine (Baltimore). 2016;95(43):e4973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Wang CY, Baldwin LM, Saver BG, et al. The contribution of longitudinal comorbidity measurements to survival analysis. Med Care. 2009;47(7):813–821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Dvorak MF, Noonan VK, Fallah N, et al. The influence of time from injury to surgery on motor recovery and length of hospital stay in acute traumatic spinal cord injury: an observational Canadian cohort study. J Neurotrauma. 2015;32(9):645–654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Madni TD, Ekeh AP, Brakenridge SC, et al. A comparison of prognosis calculators for geriatric trauma: a prognostic assessment of life and limitations after trauma in the elderly consortium study. J Trauma Acute Care Surg. 2017;83(1):90–96. [DOI] [PubMed] [Google Scholar]
- 28. Delcourt T, Begue T, Saintyves G, Mebtouche N, Cottin P. Management of upper cervical spine fractures in elderly patients: current trends and outcomes. Injury. 2015;46(suppl 1):S24–S27. [DOI] [PubMed] [Google Scholar]
- 29. Ahn H, Bailey CS, Rivers CS, et al. Effect of older age on treatment decisions and outcomes among patients with traumatic spinal cord injury. CMAJ. 2015;187(12):873–880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Failli V, Kopp MA, Gericke C, et al. Functional neurological recovery after spinal cord injury is impaired in patients with infections. Brain. 2012;135(pt 11):3238–3250. [DOI] [PubMed] [Google Scholar]
- 31. Ferrera PC, Bartfield JM, D’Andrea CC. Outcomes of admitted geriatric trauma victims. Am J Emerg Med. 2000;18(5):575–580. [DOI] [PubMed] [Google Scholar]
- 32. Ahl R, Phelan HA, Dogan S, Cao Y, Cook AC, Mohseni S. Predicting in-hospital and 1-year mortality in geriatric trauma patients using Geriatric Trauma Outcome Score. J Am Coll Surg. 2017;224(3):264–269. [DOI] [PubMed] [Google Scholar]