Abstract
The global burden of lung disease is substantial, accounting for an estimated 7.5 million deaths per year, approximately 14% of annual deaths worldwide. The prime illnesses include, in descending order, chronic obstructive pulmonary disease, lung cancer, tuberculosis, acute respiratory infections, asthma, and interstitial lung fibrosis. Key risk factors include smoking, both indoor and outdoor air pollution, and occupational exposures. Although the distribution of both the diseases and the risk factors varies greatly by age, geography, and setting, the greatest burden falls on populations living in low- and middle-income countries. Improvements in these metrics will require major public health interventions to curb smoking; improving air quality both in the community and the household; addressing the ever-present burden of infections, including tuberculosis, flu, and the many agents that cause acute respiratory disease; and identifying and protecting workers from the hazards of exposure to toxic substances. Although research over the years has identified many ways to reduce or prevent the enormous burden of disease, a huge gap exists between what we know and what we can do. This “implementation gap” is the greatest challenge we face in this field today. Research on how best to address and implement the changes needed will require not only biomedical advances to improve treatment but also social, economic, and policy research. We still need to elaborate more effective evidence-based policies and interventions to control tobacco use, address ambient and household air pollution, and improve the prevention and treatment of tuberculosis and acute respiratory infections with vaccines and drugs and reduce exposures to environmental and occupational hazards. Until these efforts receive greater prioritization, the burden of disease is unlikely to diminish a great deal more.
Keywords: global burden of disease, air pollution, smoking, capacity building, implementation research
The Global Burden of Environmental Lung Disease
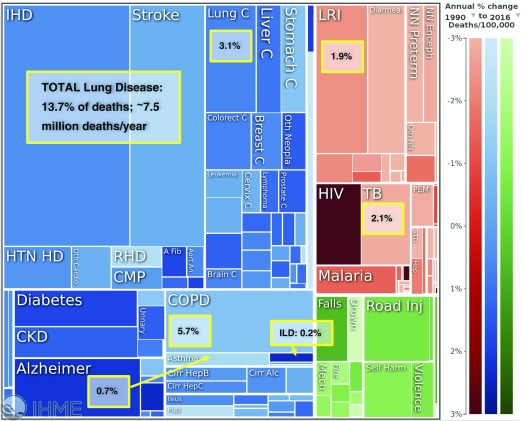
The most recent estimates of the global burden of disease from the Institute of Health Metrics and Evaluation indicate that with the aging of the world’s population, both morbidity and mortality from lung disease will increase substantially in the next few decades, and much of this increase will be concentrated among people in low- and middle-income countries (LMICs). From their massive collation and analysis of data from around the world, the Institute of Health Metrics and Evaluation estimates that approximately 7.5 million people die from lung disease each year, representing 13.5% of deaths from all causes (1). The additional burden of the disability-adjusted life-years is even greater. The Institute of Health Metrics and Evaluation database (2) is easily accessible and allows for deeper examination of the burden of each disease and exposure by time, place, and person for each country. Five major lung diseases are represented, the most common being chronic obstructive pulmonary disease, followed by lung cancer, infectious diseases (tuberculosis and acute respiratory infections, including influenza), asthma, and interstitial lung fibrosis (Figure 1). Most of these noninfectious conditions are related to environmental risks from tobacco, ambient air pollution, household use of solid fuels, and occupational exposures (3). Infections represent the second most common cause of death and morbidity, led by the continuing pandemic of tuberculosis that has emerged as the most important infectious cause of death today, exceeding that of human immunodeficiency virus/acquired immunodeficiency syndrome, seasonal and pandemic flu, and acute respiratory infections.
Figure 1.
Data visualization. 2015 Global Burden of Disease: 50 million deaths. Highlighting the contribution of lung disease. The “Compare” tool illustrating the most current estimates of mortality in the Global Burden of Diseases database. Each box depicts by size the proportion of deaths by cause. Blue boxes are noncommunicable diseases. Orange boxes indicate infectious diseases. Green boxes are trauma- and injury-related deaths. The proportion of these that are lung diseases are marked in yellow boxes with approximate percentages of the total deaths indicated. The Compare tool and other data visualization tools that the Institute of Health Metrics and Evaluation produces can be found in Reference 23. Figure reproduced from Reference 25 (https://vizhub.healthdata.org/gbd-compare/) under Creative Commons Attribution-NonCommerical-NoDerivatives 4.0 International License (https://creativecommons.org/licenses/by-nc-nd/4.0/). We have added labels framed in yellow to the Institute of Health Metrics and Evaluation figure, identifying lung diseases of environmental origin. Aort An = aortic aneurysm; A Fib = atrial fibrilation; C = cancer; Cirr = cirrhosis; Cirr Alc = alcoholic cirrhosis; CKD = chronic kidney disease; CMP = cardiopathy and myocarditis; COPD = chronic obstructive pulmonary disease; Enceph = encephalopathy; Hep = hepatitis; HIV = human immunodeficiency virus; HTN HD = hypertensive heart disease; IHD = ischemic heart disease; ILD = interstitial lung disease; Inj = injury; LRI = lower respiratory infections; Mech = mechanical; Neopla = neoplasms; NN = neonatal disorders; Oth = other; PEM = protein-energy malnutrition; PUD = peptic ulcer disease; RHD = rheumatic heart disease; STD = sexually transmitted diseases (non HIV); TB = tuberculosis.
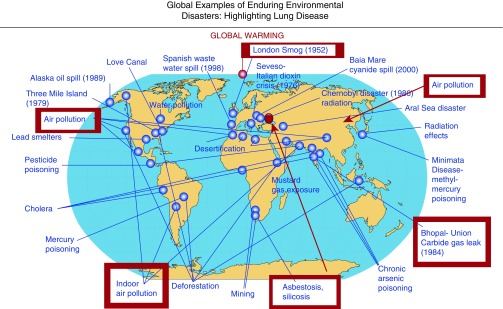
Environmental lung diseases are like global infectious diseases, in that much of what we have learned about exposures and their consequences has come from focal extreme events. Investigations around the world by astute researchers able to investigate these events have assessed their consequences, identified their causes, and proposed public health interventions (Figure 2). The Great London Smog of 1952 that left more than 12,000 people dead (4) resulted from burning sulfurous coal for cooking and heating at the time of a thermal inversion and led to the switch in London from coal to the use of alternative fuels. A more recent “natural experiment,” courtesy of a mandated cessation of vehicle and manufacturing activity during the Beijing Olympics of 2008, provided an international group of researchers the opportunity to identify a new group of biomarkers of cardiorespiratory responses to changes in air quality (5). Research by Sir Richard Doll and others (6) linking cigarette smoking with lung cancer and heart disease, and estimating that one-third of people who smoke will die of their disease, has led to public health interventions and the first global agreement designed to curb the habit. Years of research by Kirk Smith and others has recently brought to the fore an understanding that exposure to high levels of air pollution in the home, principally fine particles (<2.5 μm in aerodynamic diameter) from combustion of solid fuels such as wood and charcoal, causes almost 3 million deaths per year around the world (3, 7). Household air pollution has been prioritized as a new public health target, and much of this burden is due to respiratory disease. Finally, foci of occupational diseases from mining (e.g., asbestosis, silicosis), agriculture (e.g., byssinosis, hantavirus pulmonary syndrome), and electronic waste extraction (e.g., lung cancer and acute lung damage) are more common in LMICs than in the United States and, in some cases, are increasing in prevalence (3).
Figure 2.
Illustrative map of the world indicating locations of historically important environmental disasters with major health consequences. Red boxes flag events both acute and chronic with important lung disease effects. Inspired by Anthony Fauci’s map (24) of infectious disease outbreaks around the world.
Of course, widespread and severe respiratory infections, such as tuberculosis and influenza, should make clinicians appreciate the critical need to take a detailed environmental, occupational, and travel history. This information is essential to identify the underlying cause of disease in a patient presenting with respiratory illness and to provide care of both a common epidemic (e.g., flu) or endemic disease (e.g., respiratory syncytial virus). Finally, we cannot ignore the fact that although pneumonia in infants is much less common or deadly in the United States today, it is still the single greatest mortality threat to children younger than 2 years of age in the developing world (1) and frequently linked to air pollution and secondhand tobacco smoke.
Some Examples of Ongoing Research Activities to Address These Burdens and the Associated Risks
The Fogarty International Center at the National Institutes of Health hosts several programs that have supported research to advance our understanding of lung disease in LMICs and identify novel modes of diagnosis, treatment, and prevention. Three of these programs that link researchers in the United States with those in LMICs have proven particularly useful to advance our understanding of lung disease while training the next generation of lung researchers.
Tobacco-related Disease
Smoking is the single most common and specific cause of mortality and morbidity from lung disease leading to lung cancer and chronic obstructive pulmonary disease and is a cofactor that aggravates the severity of many other conditions, such as tuberculosis and asbestosis (3). Yet despite this clear association, our efforts to control tobacco have been slow in coming. The Framework Convention for Tobacco Control has been a landmark agreement on this topic and has accelerated relevant policies around the world. However, despite successes through implementing high taxes on tobacco products, labeling packages with hazard warnings, removing public advertising, and creating smoke-free zones in public spaces to limit secondhand smoke, the global epidemic remains and has great potential to increase, particularly among women in LMICs (8).
At the Fogarty International Center, we have partnered with the National Cancer Institute to support investigators to conduct research examining the economics of tobacco control in LMICs. The results of this research and training have laid the groundwork for some countries to institute a ban on smoking in public places, assessed the hazards of smoking from a water pipe (9), and gathered country-specific evidence to help policy makers make more informed decisions on the relative cost and benefit of different control activities. The Second Disease Control Priorities Project hosted at Fogarty with the World Bank, the World Health Organization, and the Population Reference Bureau identified the control of tobacco use through taxation as the most cost-beneficial intervention available to a country to address its burden of noncommunicable diseases (10). In many LMICs, smoking has not yet caught on, especially among woman and rural dwellers, so a major concern for the global community is how to keep these nonsmokers, especially the adolescents and young adults of today, from succumbing to the sophisticated advertising of the tobacco companies tomorrow. Smoking in people with asbestos-related disease, tuberculosis, asthma, and chronic obstructive pulmonary disease is an additive risk, making the disease more severe. The evaluation of new policies, such as the stringent control measures enacted in Australia limiting the number of brands that a company can sell or covering a package completely with demonstrative photos of people with extreme smoking-related diseases, may identify more productive routes to inform purchasers of the risks of tobacco products and the consequences of this most deadly, costly, and addictive habit. Research on antinicotine vaccines, nicotine patches, and e-cigarettes are topics being investigated as biomedical solutions to what remains a major preventable public health problem today. However, the future control of tobacco in the United States may come from studying the impact of the aggressive antismoking campaigns in Australia and the new tax policies in China (11), and there is a need for implementation research to understand if, when, and how such policies can be most effective.
Household Air Pollution
In 2010, the Global Alliance for Clean Cookstoves was launched by then Secretary of State Hilary Clinton as a global program to reduce death and disability among people exposed to high levels of pollutants from burning solid fuels (e.g., wood, charcoal, straw, dung) using traditional, low-efficiency cookstoves. The World Health Organization and Institute of Health Metrics and Evaluation have estimated that household air pollution is associated with an estimated 3 to 4 million deaths per year among the ∼3 billion people cooking and heating with these fuels. Their vision has been to improve health from acute respiratory infections, chronic obstructive pulmonary disease, lung cancer, and other diseases from chronic exposure by decreasing levels of indoor air pollutants, principally fine particulate matter (particulate matter with an aerodynamic diameter < 2.5 μm) and carbon monoxide (12). The Global Alliance for Clean Cookstoves originally focused on efforts to introduce new, more efficient, solid fuel cookstoves to 100 million families by 2020, because this offered the greatest opportunity for scale. However, subsequent research by Kirk Smith and many others in Guatemala, India, Malawi, and elsewhere has shown that these more efficient stoves could not decrease levels of household air pollution enough to improve health (13). The goals of the Global Alliance for Clean Cookstoves have since evolved to provide greater emphasis on scaling up cleaner fuels, primarily liquefied petroleum gas, but in some settings, biogas, ethanol, electric, or solar stoves (14). The World Health Organization has developed new Indoor Air Quality Guidelines that are, for the most part, unattainable without near-exclusive use of these cleaner fuels (15).
Six National Institutes of Health components (U.S. National Heart, Lung, and Blood Institute; National Cancer Institute; National Institute of Environmental Health Sciences; Eunice Kennedy Shriver National Institute of Child Health and Human Development; John E. Fogarty International Center; and the National Institutes of Health Common Fund) have partnered with the Bill and Melinda Gates Foundation and the Global Alliance for Clean Cookstoves to support an interventional trial to provide proof of principle that the introduction of liquefied petroleum gas–based stoves into homes that currently rely on solid fuels can in fact achieve significant reductions in incidence of severe pneumonia, low birth weight, and indicators for hypertension, chronic obstructive pulmonary disease, and lung cancer (16). The studies are being launched in four countries (Peru, Rwanda, Guatemala, and India) where the governments are actively grappling with the regulations, infrastructure, and financial barriers to scaling up clean fuel access. In parallel, Fogarty is leading a Clean Cooking Implementation Science Network to accelerate the science of adoption and scale-up of cleaner technologies in low-income settings (17). In many countries around the world, the policy environment for clean energy is changing. In India, a massive program of subsidies and vouchers is in place to provide up to 50 million homes below the poverty line access to liquefied petroleum gas (18). In Ghana, the government has set a goal of providing half of its people with liquefied petroleum gas by 2020 (19). In Ecuador, reduction of subsidies for liquefied petroleum gas combined with rural electrification is encouraging people to move to even cleaner-fuel, high-efficiency induction stoves for cooking (20). The results of these efforts will, it is hoped, provide the evidence needed to provide direction for scaling up these interventions.
Capacity Building for Respiratory Disease Research
A key challenge in addressing lung health and environmental lung diseases has been the paucity of investigators in the United States and in LMIC settings capable of conducting research on hazardous exposures, from toxins to infections, and arriving at strategies for their control and treatment. For more than a decade, the Fogarty International Center, along with the National Institute of Environmental Health Sciences and the U.S. Centers for Disease Control and Prevention’s National Institute on Occupational Health Sciences, has supported capacity building for environmental and occupational health researchers around the world (21). We have recently expanded this effort with additional partners and focused on the development of networked institutional centers for training and research on environmental hazards, including lung disease risk factors. By building research capacity in LMICs, collaborations between U.S. and foreign scientists have helped us understand the risks of disease that we would have difficulty addressing at home. These seven networked centers provide a platform for global research on lung diseases associated with ambient air pollution, household air pollution, electronic waste extraction, pesticide inhalation, mining, and other exposures in Africa, Asia, and Latin America, and all welcome collaborators (22). As our understanding of the global burden of lung disease is better appreciated, the need for more international partnerships to understand the exposure context, etiology and pathogenesis, genetic risk factors, behavior, and policy environment will lead to more effective ways to consider their prevention, treatment, and ultimate control.
Conclusions
The community of lung researchers “owns” a substantial portion of the global burden of disease that impacts low- and middle-income countries more profoundly than anywhere. We have learned a great deal about these conditions and their underlying risk factors but have been only modestly effective in securing gains in the control of the most common conditions. Future opportunities to partner in research with foreign investigators on the science that underlies well-designed policies to control and prevent the most common conditions will be essential to improve lung health around the world.
Supplementary Material
Footnotes
The views expressed in this article do not represent official views of the National Institutes of Health or the U.S. Government.
Publication of this article falls on the 50th anniversary of the Fogarty International Center.
Author Contributions: R.I.G. developed the lecture with contributions from J.P.R. R.I.G. delivered the lecture. Both authors contributed to background research, concept development, and drafting of the manuscript.
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.GBD 2013 Mortality and Causes of Death Collaborators. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;385:117–171. doi: 10.1016/S0140-6736(14)61682-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Institute for Health Metrics and Evaluation. GBD data visualizations [accessed 2018 Feb 14] Available from: http://www.healthdata.org/gbd/data-visualizations.
- 3.GBD 2015 Risk Factors Collaborators. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1659–1724. doi: 10.1016/S0140-6736(16)31679-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bell ML, Davis DL, Fletcher T. A retrospective assessment of mortality from the London smog episode of 1952: the role of influenza and pollution. Environ Health Perspect. 2004;112:6–8. doi: 10.1289/ehp.6539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhang J, Zhu T, Kipen H, Wang G, Huang W, Rich D, et al. HEI Health Review Committee. Cardiorespiratory biomarker responses in healthy young adults to drastic air quality changes surrounding the 2008 Beijing Olympics. Res Rep Health Eff Inst. 2013;174:5–174. [PMC free article] [PubMed] [Google Scholar]
- 6.Doll R, Hill AB. Lung cancer and other causes of death in relation to smoking; a second report on the mortality of British doctors. BMJ. 1956;2:1071–1081. doi: 10.1136/bmj.2.5001.1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Smith KR, Bruce N, Balakrishnan K, Adair-Rohani H, Balmes J, Chafe Z, et al. HAP CRA Risk Expert Group. Millions dead: how do we know and what does it mean? Methods used in the comparative risk assessment of household air pollution. Annu Rev Public Health. 2014;35:185–206. doi: 10.1146/annurev-publhealth-032013-182356. [DOI] [PubMed] [Google Scholar]
- 8.GBD 2015 Tobacco Collaborators. Smoking prevalence and attributable disease burden in 195 countries and territories, 1990-2015: a systematic analysis from the Global Burden of Disease Study 2015. Lancet. 2017;389:1885–1906. doi: 10.1016/S0140-6736(17)30819-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Maziak W, Ward KD, Afifi Soweid RA, Eissenberg T. Tobacco smoking using a waterpipe: a re-emerging strain in a global epidemic. Tob Control. 2004;13:327–333. doi: 10.1136/tc.2004.008169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Laxminarayan R, Mills AJ, Breman JG, Measham AR, Alleyne G, Claeson M, et al. Advancement of global health: key messages from the Disease Control Priorities Project. Lancet. 2006;367:1193–1208. doi: 10.1016/S0140-6736(06)68440-7. [DOI] [PubMed] [Google Scholar]
- 11.Hu TW, Zhang X, Zheng R. China has raised the tax on cigarettes: what’s next? Tob Control. 2016;25:609–611. doi: 10.1136/tobaccocontrol-2015-052534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Global Alliance for Clean Cookstoves [accessed 2018 Feb 14]. Available from http://cleancookstoves.org/about/our-mission/
- 13.Smith KR, Sagar A. Making the clean available: escaping India’s chulha trap. Energy Policy. 2014;75:410–414. [Google Scholar]
- 14.Global Alliance for Clean Cookstoves. Technology and fuels overview [accessed 2018 Feb 14] Available from: http://cleancookstoves.org/technology-and-fuels/fuels/index.html.
- 15.World Health Organization. WHO indoor air quality guidelines: household fuel combustion. 2014 [accessed 2018 Feb 14]. Available from: http://www.who.int/indoorair/guidelines/hhfc/HHFC_guidelines.pdf. [PubMed]
- 16.National Institutes of Health. Household Air Pollution Investigation Network (HAPIN) [accessed 2018 Feb 14] Available from: https://commonfund.nih.gov/globalhealth/HAPINresources.
- 17.Rosenthal J, Balakrishnan K, Bruce N, Chambers D, Graham J, Jack D, et al. Implementation science to accelerate clean cooking for public health. Environ Health Perspect. 2017;125:A3–A7. doi: 10.1289/EHP1018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Smith KR, Sagar AD. LPG subsidy: analysing the ‘give it up’ scheme. Economic Times: The Times of India; 2016.
- 19.Ghana News Agency. Government expands LPG programme to rural areas; 2015 [accessed 2018 Feb 14] Available from: http://www.ghananewsagency.org/social/government-expands-lpg-programme-to-rural-areas--87037.
- 20.Martínez-Gómez J, Ibarra D, Villacis S, Cuji P, Cruz PR. Analysis of LPG, electric and induction cookers during cooking typical Ecuadorian dishes into the national efficient cooking program. Food Policy. 2016;59:88–102. [Google Scholar]
- 21.Rosenthal J, Jessup C, Felknor S, Humble M, Bader F, Bridbord K. International environmental and occupational health: from individual scientists to networked science Hubs. Am J Ind Med. 2012;55:1069–1077. doi: 10.1002/ajim.22130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.National Institutes of Health, Fogarty International Center. US and Canada partner to invest $21 million for environmental and occupational health research hubs in developing countries; 2015 [accessed 2018 Feb 14] Available from: https://www.fic.nih.gov/News/GlobalHealthMatters/november-december-2015/Pages/2015-environmental-occupational-health-research-hubs.aspx.
- 23.Institute for Health Metrics and Evaluation. Data visualizations [accessed 2018 Feb 14] Available from: http://www.healthdata.org/results/data-visualizations.
- 24.Paules CI, Eisinger RW, Marston HD, Fauci AS. What recent history has taught us about responding to emerging infectious disease threats. Ann Intern Med. 2017;11:805–811. doi: 10.7326/M17-2496. [DOI] [PubMed] [Google Scholar]
- 25.Institute for Health Metrics and Evaluation (IHME) GBDCompareDataVisualization. Seattle, WA: IHME, University of Washington, 2016 [accessed 2018 Feb 14]. Available from http://vizhub.healthdata.org/gbd-compare.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.