Abstract
Ectopic thyroid tissue is very rare, but its prevalence increases in those with thyroid pathology. It typically occurs due to aberrant development of the thyroid gland during its migration to the pretracheal region. In this report, there are two cases of mediastinal ectopic thyroid tissue discussed, which were initially considered to be malignancies. The hospital course, diagnostic workup, including the use of computed tomography and positron emission tomography scans, and the characteristic features of the tissue are examined here. Due to the imaging characteristics, it is important to consider ectopic thyroid tissue as a differential diagnosis for mediastinal masses as encountered in these cases. Asymptomatic ectopic thyroid tissue is usually treated medically; however, patients in both of our cases opted for surgical resection of the masses even after confirmation of the origin of the tissues.
KEY WORDS: Computed tomography, malignancy, mediastinal ectopic thyroid, positron emission tomography-computed tomography
INTRODUCTION
Ectopic thyroid can be described as functional thyroid tissue that is located anywhere other than its anatomic position.[1] The aberrant development of the thyroid gland typically takes place during its migration from the primitive foregut to the pretracheal region. Ectopic thyroid tissue is typically located along the path of thyroid gland descent, but it can rarely be found in the mediastinum, heart, diaphragm, and esophagus. The prevalence of ectopic thyroid tissue is about 1 in 100,000–300,000 people and that increases to 1 in 4000–8000 patients with thyroid pathology.[2,3] The most common variant of ectopic thyroid is the lingual thyroid gland at the base of the tongue, accounting for 47% of ectopic thyroid cases.[2] Mediastinal ectopic thyroid is seen in <1% of all ectopic thyroid cases.[4] In 440 autopsy cases, ectopic thyroid tissue was the only thyroid tissue in 70%–90% of cases.[2] Computed tomography (CT) findings of ectopic thyroid tissue can be influenced by multiple factors including its continuation from cervical thyroid gland, noncontrast attenuation of thyroid tissue compared to that of the surrounding tissue, and areas of focal calcification.[5,6] We describe two cases of ectopic thyroid located in the mediastinum, one with features of malignancy on both CT and positron emission tomography with 2-deoxy-2-[fluorine-18]fluoro-D-glucose integrated with CT (F-18 FDG PET-CT) and the other case displaying possible malignancy on F-18 FDG PET-CT.
CASE REPORTS
Case 1
An elderly male with rib injury was found to have a right hilar mediastinal mass on chest radiograph. CT scan performed at outside hospital demonstrated right paratracheal mass, separate from native thyroid gland. Subsequent mediastinoscopy with biopsy of the mass revealed colloidal thyroid tissue with no evidence of malignancy. F-18 FDG PET-CT was performed, showing right paratracheal mass with peripheral calcification and central hypodensity as well as right hilar calcified lymph node with no abnormal increased metabolic activity [Figures 1 and 2]. Thyroid ultrasound showed enlarged gland with ill-defined nodules bilaterally. Technetium-99m (Tc-99m) pertechnetate scan showed normal uptake signifying nonfunctioning thyroid tissue, but a cold thyroid nodule could not be excluded. The patient was clinically and biologically euthyroid. Fine-needle aspiration of the thyroid nodule confirmed left nontoxic multinodular goiter. A right-sided video-assisted thoracoscopic surgery was subsequently performed to remove the paratracheal mass. Final pathology results confirmed it as benign thyroid nodule with nodular hyperplasia with no signs of malignancy. Subsequent follow-up at 4 and 12 months revealed no evidence for new mass.
Figure 1.
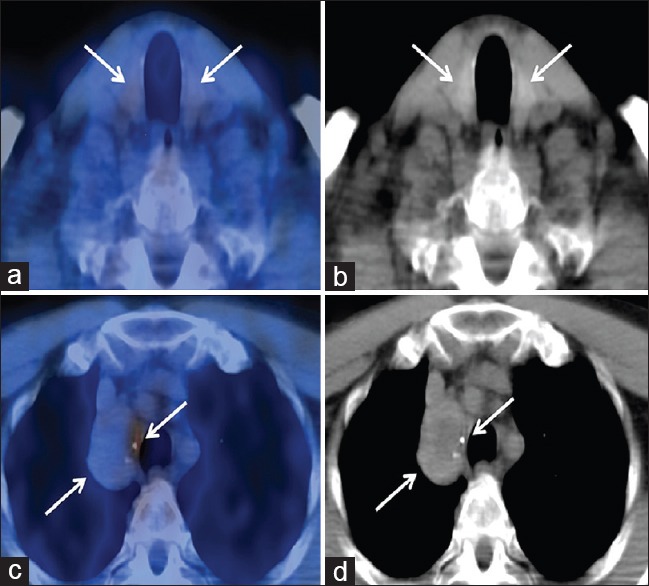
Fused axial positron emission tomography/computed tomography and low-dose computed tomography images of lower neck (a and b) showing nonhypermetabolic orthotopic bilateral thyroid with heterogeneous computed tomography appearance. Fused axial positron emission tomography/computed tomography and low-dose computed tomography images of the upper chest (c and d) demonstrating nonhypermetabolic right paratracheal mass with central hypodensity and peripheral calcifications. Mild uptake at the medial aspect of the mass represents inflammation at biopsy site
Figure 2.
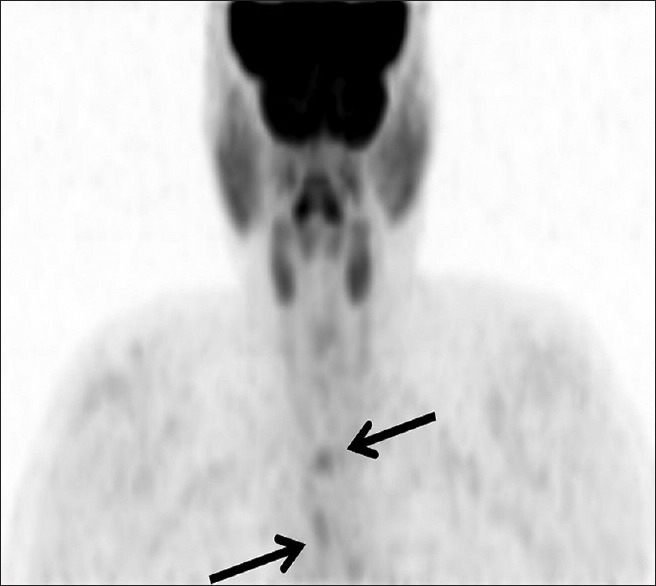
Maximal intensity projection positron emission tomography image showing no uptake in orthotopic or ectopic thyroid tissues with the two foci corresponding to inflammatory uptake from previous mediastinoscopy (superior) and biopsy site of the ectopic thyroid (inferior)
Case 2
An elderly female with a history of chronic obstructive pulmonary disease was admitted to the intensive care unit for headache, shortness of breath, and somnolence for 1 day. CT angiography with contrast showed an anterior mediastinal heterogeneous highly enhancing soft-tissue mass with central calcification was noted, which was considered to be neoplastic likely representing thymic carcinoma. A second smaller more superior anterior mediastinal soft-tissue lesion was also noted. Subsequent F-18 FDG PET-CT showed mildly increased activity in the anterior mediastinal mass with calcifications [Figure 3]. The smaller mediastinal mass anterior to the brachiocephalic vein demonstrated uptake slightly below blood pool [Figure 3]. The findings were initially concerning for germ cell tumor, thymic carcinoma, or thymic neuroendocrine tumor. Subsequently, partial upper sternotomy and anterior mediastinal mass resection were performed. Final pathology findings confirmed it as two nodular foci of thyroidal tissue displaying nodular hyperplasia. The ectopic thyroid foci and surrounding thymic tissue were negative for neoplasia or other significant pathologic changes. A 4-month follow-up chest CT with IV contrast did not show any recurrence of the lesion, hematoma, or seroma.
Figure 3.
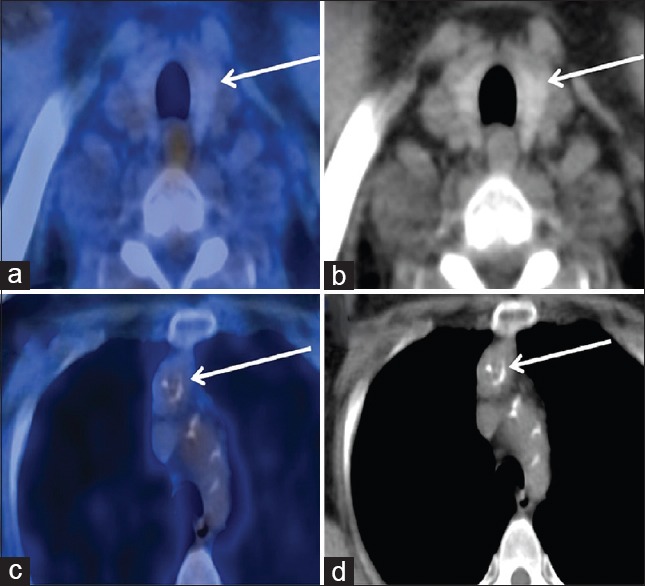
Fused axial positron emission tomography/computed tomography of the neck (a) and noncontrast computed tomography (b) of the neck showing normal appearing thyroid gland with physiological uptake. Fused axial positron emission tomography/computed tomography of the chest (c) and noncontrast computed tomography (d) of the chest showing a mildly active heterogeneous anterior mediastinal mass with calcifications abutting the posterior aspect of the left brachiocephalic vein and aortic arch. This was confirmed as ectopic thyroid on biopsy
DISCUSSION
Ectopic thyroid tissue is identical to orthotopic thyroid tissue with exception of the inherent anatomic bilobed shape.[7] Ectopic thyroid tissue is formed due to aberrant migration of the thyroid gland as it descends from primitive foregut to the pretracheal region in the neck.[1] Intrathoracic ectopic thyroid tissue occurs very rarely and is typically located in the anterosuperior aspect of the mediastinum.[4] Furthermore, primary intrathoracic goiter can be described as thyroid tissue lacking the connection with the cervical thyroid, receiving its blood supply from intrathoracic vasculature.[8] However, this condition originates from true ectopic thyroid tissue in <1% of cases. Intrathoracic goiter is often secondary from extension of the cervical portion of the thyroid gland.[4]
Contrast-enhanced CT of ectopic thyroid tissue demonstrates intensely enhancing mass, whereas non-contrast CT of the same tissue shows increased attenuation due to the iodine content localization.[4,5,6,7] Calcifications are also commonly seen on chest CT.[5,6] Ectopic thyroid tissue is mildly hyperintense on T2-weighted MR imaging but tends to have similar intensity as musculature on T1-weighted MR images.[7] Scintigraphy scan using I-123, I-131, or Tc-99m is the most useful diagnostic tool in localizing ectopic thyroid tissue; however, absent iodine content can be due to necrosis or carcinoma and does not exclude the presence of malignancy in ectopic tissue.[8] F18-FDG PET scan of normal thyroid tissue will display low uptake, but hypermetabolic conditions such as carcinoma, multinodular goiter, and nodular hyperplasia will show local or diffuse uptake.[4] Kim reported PET/CT findings in a case of ectopic thyroid, demonstrating diffuse high metabolic uptake within the mass.[4] This is different from our study where we did not find significantly increased uptake; however, the activity was above blood pool. This emphasizes the heterogeneity of findings on PET/CT for ectopic thyroid tissue, further making it a diagnostic dilemma. Hence, it is important to consider it as one of the potential differential diagnoses in patients with thyroid disorders.
Other differentials for ectopic mediastinal mass include metastatic thyroid disease, lymphomas, neurogenic tumors, and thymic and mesenchymal tumors.[9] Clinically, mediastinal ectopic thyroid tissue is generally euthyroid and asymptomatic. However, it can present with airway compression, dry cough, dyspnea, and hemoptysis, thus necessitating operative intervention.[2] Surgical treatment for symptomatic mediastinal ectopic thyroid generally involves thoracotomy or sternotomy with use of radioiodine ablation in recurring cases.[2] Asymptomatic cases generally require regular follow-up to detect any interval changes.[4]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Hillman T. Pediatric Otolaryngology. 4th ed. Philadelphia: Saunders; 2002. p. 1738. [Google Scholar]
- 2.Noussios G, Anagnostis P, Goulis DG, Lappas D, Natsis K. Ectopic thyroid tissue: Anatomical, clinical, and surgical implications of a rare entity. Eur J Endocrinol. 2011;165:375–82. doi: 10.1530/EJE-11-0461. [DOI] [PubMed] [Google Scholar]
- 3.Di Benedetto V. Ectopic thyroid gland in the submandibular region simulating a thyroglossal duct cyst: A case report. J Pediatr Surg. 1997;32:1745–6. doi: 10.1016/s0022-3468(97)90522-4. [DOI] [PubMed] [Google Scholar]
- 4.Kim SY. A case of right paratracheal ectopic thyroid, mimicking metastasis on CT and 18F-FDG PET CT. Open J Med Imaging. 2013;3:82. [Google Scholar]
- 5.Glazer GM, Axel L, Moss AA. CT diagnosis of mediastinal thyroid. Am J Roentgenol. 1982;138:495–8. doi: 10.2214/ajr.138.3.495. [DOI] [PubMed] [Google Scholar]
- 6.Bashist B, Ellis K, Gold RP. Computed tomography of intrathoracic goiters. AJR Am J Roentgenol. 1983;140:455–60. doi: 10.2214/ajr.140.3.455. [DOI] [PubMed] [Google Scholar]
- 7.Zander DA, Smoker WR. Imaging of ectopic thyroid tissue and thyroglossal duct cysts. Radiographics. 2014;34:37–50. doi: 10.1148/rg.341135055. [DOI] [PubMed] [Google Scholar]
- 8.Foroulis CN, Rammos KS, Sileli MN, Papakonstantinou C. Primary intrathoracic goiter: A rare and potentially serious entity. Thyroid. 2009;19:213–8. doi: 10.1089/thy.2008.0222. [DOI] [PubMed] [Google Scholar]
- 9.Guimarães MJ, Valente CM, Santos L, Baganha MF. Ectopic thyroid in the anterior mediastinum. J Bras Pneumol. 2009;35:383–7. doi: 10.1590/s1806-37132009000400013. [DOI] [PubMed] [Google Scholar]


