Suzuki T, Inokuchi R, Hanaoka K, Suka M, Yanagisawa H. Dexmedetomidine use during epiduroscopy reduces fentanyl use and postoperative nausea and vomiting: A single-center retrospective study. SAGE Open Medicine. 2018. DOI: 10.1177/2050312118756804
The author would like to report some statistical errors in the text as well as in Tables 1 & 2 and likes replace Figure 2 in the above article.
Under the heading Results in Abstract, the values in the last line have been changed as follows:
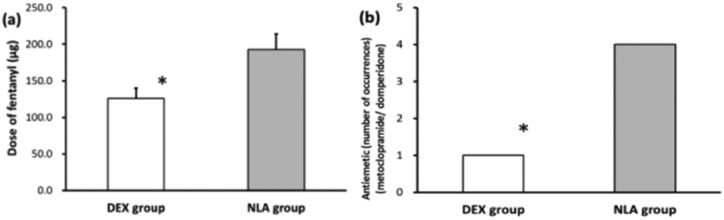
We identified 45 patients (31 and 14 in the DEX and NLA groups, respectively) with a mean age of 69.0 years. The two groups had comparable characteristics, such as age, sex, body mass index, the American Society of Anesthesiologists Physical Status, analgesics used in the clinic, comorbidities, history of smoking, and the duration of anesthesia. The DEX group received a significantly lower fentanyl dose during surgery (126 ± 14 vs. 193 ± 21 µg, mean ± standard deviation, P = 0.014) and exhibited a significantly lower incidence of PONV (1 vs. 4, P = 0.027) than the NLA group.
Under the Introduction, comma has been replaced with hyphen in the second paragraph as follows:
Minimally invasive epiduroscopy may be an effective treatment for such conditions;11 therefore, the number of epiduroscopy procedures performed is currently increasing worldwide.12, 13 This procedure consists of observation, washing, irrigation, lysis of the adhesion in the epidural space under direct visual observation, and direct drug administration to the affected part of the spinal canal.12–14 However, anesthesia is required to alleviate pain during the lysis of the adhesions in the epidural space.15 Thus, monitored anesthesia care (MAC) should be used to provide anesthesia during epiduroscopy.16–18
Under the sub-heading “Statistical analysis”, Chi-square tests has been replaced with Fisher’s exact tests as follows:
The statistical analysis was designed to compare the DEX and NLA groups. Continuous parameters were expressed as means ± standard deviations (SD) and independent t-tests were conducted to compare the groups. Categorical variables were expressed as frequencies and percentages, and Fisher’s exact tests were conducted to compare the groups. All the analyses were performed using STATA 13.1 software (Stata Corporation, College Station, TX, USA). The threshold for significance was set at P < 0.05.
The values in Table 1 and 2 have been changed as follows:
Table 1.
Comparison of patient characteristics, American Society of Anesthesiologists (ASA) physical status classification system, comorbidities, and analgesic agents between the DEX and NLA groups.
| Variables | DEX group | NLA group | P-value |
|---|---|---|---|
| Number enrolled | 31 | 14 | |
| Age (years, mean ± SD) | 68.5 ± 1.83 | 70.1 ± 2.76 | 0.631 |
| Male/Female (%) | 12/19 (38.7/61.3) | 8/6 (57.1/42.9) | 0.249 |
| BMI (kg/m2, mean ± SD) | 23.4 ± 0.47 | 22.7 ± 0.70 | 0.426 |
| Tobacco | 0.525 | ||
| No (never smoked) | 16 | 9 | |
| Yes (former/ current smoker) | 15 | 5 | |
| ASA physical status | 0.552 | ||
| Class 1 | 3 | 3 | |
| Class 2 | 24 | 10 | |
| Class 3 | 4 | 1 | |
| Diagnosis (%) | |||
| Spinal stenosis | 29 (93.6) | 11 (78.6) | 0.166 |
| Disc herniation | 5 (16.1) | 3 (21.4) | 0.689 |
| Spondylolisthesis | 2 (14.3) | 2 (6.5) | 0.578 |
| Other | 6 (19.4) | 2 (14.3) | 1 |
| Comorbidities (%) | |||
| Hypertension | 18 (58.1) | 8 (57.1) | 1 |
| Diabetes mellitus | 2 (6.5) | 1 (7.1) | 1 |
| Dyslipidemia | 14 (45.2) | 5 (35.7) | 0.746 |
| Malignancy | 4 (12.9) | 3 (21.4) | 0.659 |
| Cardiovascular disease | 3 (9.7) | 1 (7.1) | 1 |
| Asthma | 4 (12.9) | 1 (7.1) | 1 |
| Urological disease | 4 (12.9) | 2 (14.3) | 1 |
| Thyroid disease | 1 (3.2) | 1 (7.1) | 0.530 |
| Brain disease | 5 (16.1) | 1 (7.1) | 0.648 |
| Peripheral nerve disease | 2 (6.5) | 1 (7.1) | 1 |
| Dementia | 1 (3.2) | 1 (7.1) | 0.530 |
| Depression | 2 (6.5) | 0 | 1 |
| Analgesic agents used in clinic (%) | |||
| NSAIDs | 12 (38.7) | 7 (50.0) | 0.528 |
| Narcotics | 5 (16.1) | 2 (14.3) | 1 |
| Pregabalin | 14 (45.2) | 5 (35.7) | 0.746 |
| Adjuvant remedy | 22 (71.0) | 12 (85.7) | 0.458 |
| Other | 24 (77.4) | 13 (92.3) | 0.402 |
ASA, The American Society of Anesthesiologists; DEX group, dexmedetomidine plus fentanyl; NLA group, droperidol plus fentanyl; BMI, body-mass index; NSAIDs, Nonsteroidal Anti-inflammatory Drugs; SD, standard deviation.
Table 2.
Comparison of intraoperative drugs between the DEX and NLA groups.
| DEX group n = 31 |
NLA group n = 14 |
P-value | |
|---|---|---|---|
| Nicardipine | 6 | 5 | 0.277 |
| Diltiazem | 1 | 0 | 1 |
| Landiolol | 0 | 2 | 0.092 |
| Lidocaine | 0 | 1 | 0.311 |
| Atropine | 5 | 1 | 0.648 |
| Phenylephrine | 0 | 1 | 0.311 |
| Ephedrine | 1 | 0 | 1 |
DEX group, dexmedetomidine plus fentanyl; NLA group, droperidol plus fentanyl; SD, standard deviation.
Under the heading Main Results, the values have been changed as follows:
A comparison of the incidence of PONV and the dose of fentanyl during surgery between the DEX and NLA groups is shown in Figure 2. The presence or absence of PONV was determined based on the history of receiving an antiemetic (metoclopramide or domperidone), which was noted in significantly fewer patients in the DEX group than in the NLA group (1 vs. 4, P = 0.027). A significantly lower dose of the anesthetic fentanyl was used during surgery in the DEX group than in the NLA group (126 ± 14 vs. 193 ± 21 µg, respectively, mean ± SD, P = 0.014). Significant intergroup differences were not observed in the use of other intraoperative drugs during surgery (Table 2).
Figure 2 has been changed as follows: