Abstract
Background:
Fibular collateral ligament (FCL) tears are challenging to diagnose. Left untreated, FCL tears lead to residual ligament instability and increased joint loading on the medial compartment of the knee. Additionally, when a concomitant anterior cruciate ligament (ACL) reconstruction is performed, increased forces on reconstruction grafts occur, which may lead to premature graft failure. Stress radiographs constitute a reliable and validated technique for the objective assessment of a complete grade III FCL tear.
Purpose:
To evaluate side-to-side difference (SSD) values of lateral compartment gapping on varus stress radiographs in patients with a grade III injury to the FCL. Additionally, to evaluate the reliability and reproducibility of 3 different measurement techniques that used various radiographic reference points.
Study Design:
Cohort study (diagnosis); Level of evidence, 2.
Methods:
Inclusion criteria were patients who sustained an FCL with or without a concomitant ACL injury and underwent a combined FCL + ACL reconstruction between 2010 and 2016. Patients were excluded if they had a complete posterolateral corner injury, open physes, intra-articular fracture, meniscal root tear, other ligament injury, or prior surgery on either knee. All FCL tears were diagnosed with a clinical varus stress examination at 0° and 20° of knee flexion and varus stress radiographs at 20° of knee flexion measured in 3 different locations. The SSD for lateral compartment gapping was obtained from the varus stress radiographs and then statistically compared for interrater and intrarater reliability.
Results:
A total of 98 consecutive patients (50 males, 48 females; 13 isolated FCL injuries, 85 combined ACL + FCL injuries) with mean age 33.6 years (range, 18-69 years) were included. Measurement techniques 1, 2, and 3 had mean ± SD lateral compartment SSDs of 2.4 ± 0.20 mm, 2.2 ± 0.20 mm, and 2.0 ± 0.03 mm, respectively (no significant differences). Interrater reliabilities for the 3 measuring techniques were 0.83, 0.86, and 0.91, respectively, while intrarater reliabilities were 0.99, 0.77, and 0.99, respectively.
Conclusion:
This study demonstrated a lower SSD value of 2.2 mm to be consistent with a grade III FCL tear on clinician-applied varus stress radiographs in the clinical setting. Although all SSD measurement locations had excellent reliability, the method using the midpoint of the lateral tibial plateau was found to be the most reproducible.
Keywords: fibular collateral ligament, varus stress radiographs, posterolateral corner, ACL
Despite a recent increase in awareness, injuries to the fibular collateral ligament (FCL) still pose significant diagnostic challenges to treating physicians, with a significant proportion of these injuries either missed or misdiagnosed on initial evaluation.4,8,14 While a thorough history and physical examination are still paramount, patient pain, guarding, and concomitant cruciate ligament injuries can pose significant challenges in obtaining a definitive diagnosis.4 Animal studies and clinical studies3,4,8,10–15,20 have reported that grade III injuries heal poorly, resulting in knee instability. Persistent varus instability of the knee results in a varus thrust gait with increased forces on the medial compartment of the knee. In the long term, this can result in meniscal injuries and medial compartment osteoarthritis. Varus instability due to a deficient FCL has also been demonstrated to increase forces on the anterior cruciate ligament (ACL) and posterior cruciate ligament (PCL). Therefore, failure to reconstruct the FCL at the same time as the cruciate ligament reconstruction can put undue stress on the graft(s) and lead to graft failure.3,8,13,18,22,23
The utility and validity of varus stress radiographs in diagnosing FCL injuries have been well documented. In 2008, LaPrade et al9 published results from a cadaveric study indicating an increase of 2.7 mm of lateral compartment gapping from the intact state to be consistent with an isolated, grade III tear of the FCL. A difference of 4.0 mm was consistent with a complete posterolateral corner (PLC) injury. While this study has traditionally served as the gold standard for side-to-side difference (SSD) values consistent with a complete FCL tear, more recent literature has reported these values to be 1.99 mm.19 Both of these studies, however, were performed using cadaveric specimens. Factors such as an intact soft tissue envelope and patient relaxation may make the values obtained in the clinical setting different than those found in a cadaveric model. A previously published clinical study suggested an SSD value of 2.0 mm to be predictive of an FCL tear, but this study was performed in healthy volunteers and was done with a “gonylaxometer” and not a clinician-applied load, making its clinical applicability difficult.6
Additionally, the optimal reference point and measurement location for determining displacement and lateral compartment gapping on varus stress radiographs have yet to be defined. Thus, the purposes of this study were to assess the SSD on varus stress radiographs in surgically confirmed FCL injuries and determine the accuracy and reliability of 3 different stress radiograph measurement techniques for defining lateral compartment gapping in patients with complete tears of the FCL. It was hypothesized that the SSD of a clinician-applied varus load would be the same in the clinical setting compared with previous cadaveric models and that there would be no difference in the various radiographic reference points.
Methods
An institutional review board approved a retrospective review of prospectively collected data from April 2010 to August 2016 for patients who sustained either an isolated FCL or combined ACL/FCL tears that were diagnosed based upon patient history, clinical examination, and bilateral varus stress radiographs. This was further confirmed by examination under anesthesia (EUA) and confirmed during surgery for patients who underwent either an isolated FCL or combined ACL and FCL reconstruction. Exclusion criteria were a complete PLC injury, open physes, concomitant intra-articular fracture, meniscal root tear on the ipsilateral knee, PCL injury, medial collateral ligament injury, prior osteotomy on the ipsilateral knee, or any prior surgery on the contralateral knee. Complete PLC injuries were evaluated by checking for an increase in external rotation on either the dial test at 30° and 90° or the posterolateral drawer test at 90° on clinical examination and the EUA, in addition to arthroscopic confirmation of an intact popliteus tendon. Patient demographic data including age, sex, and injury chronicity were collected. FCL tears were diagnosed preoperatively based on clinical examination and imaging studies (magnetic resonance imaging [MRI] scans and bilateral varus stress radiographs) and were confirmed during surgery. Varus stress examination at 0° and 20° of knee flexion was performed during the preoperative clinical examination (lateral compartment gapping in comparison with the contralateral side, with the knee flexed to 20°, indicated an injury to the FCL) and was verified during the EUA by the senior author (R.F.L.).
All stress radiographs were performed by the senior author in clinic with the patient in the supine position as previously described.9 Each radiograph was independently measured using all 3 techniques by 2 raters (P.W.K., M.E.C.), on 2 separate occasions.
Varus Stress Radiographs
Varus stress radiographs were performed in all patients who had increased lateral compartment gapping on clinical examination preoperatively (Figure 1). Radiographs were performed in the same manner as previously reported by LaPrade et al.9 All patients had bilateral varus stress radiographs with the maximum physician-applied load in clinic. A standard radiographic distance of 46 cm was used, and a 20° foam block was placed under the knee to standardize the knee flexion angle. A maximum clinician-applied varus load was then performed by the senior author by placing one hand on the medial femoral condyle and the other hand on the lateral aspect of the foot.
Figure 1.

Varus stress radiographic technique performed on patient’s right lower extremity. The patient’s knee is placed in 20° of flexion with the use of a polyurethane wedge underneath the knee. A clinician applies a varus load by placing one hand on the medial femoral condyle and the other hand on the lateral aspect of the foot.
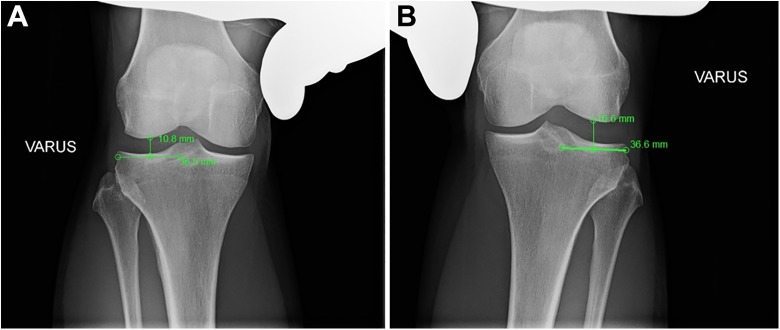
Three different measurement techniques were used to quantify the amount of gapping in the patient cohort. The first measurement technique was performed as defined by LaPrade et al9 by extending a vertical line from the most inferior aspect of the lateral femoral condyle to the corresponding point on the lateral tibial plateau (Figure 2).
Figure 2.
Varus stress radiographs resulting from measurement technique 1. This measurement technique was performed by extending a vertical line from the most inferior aspect of the lateral femoral condyle to the corresponding point on the lateral tibial plateau. (A) Measurement technique 1 demonstrated on an uninjured right knee. (B) Measurement technique 1 demonstrated on a left knee with a combined anterior cruciate ligament and fibular collateral ligament injury, resulting in a 2.2-mm side-to-side difference.
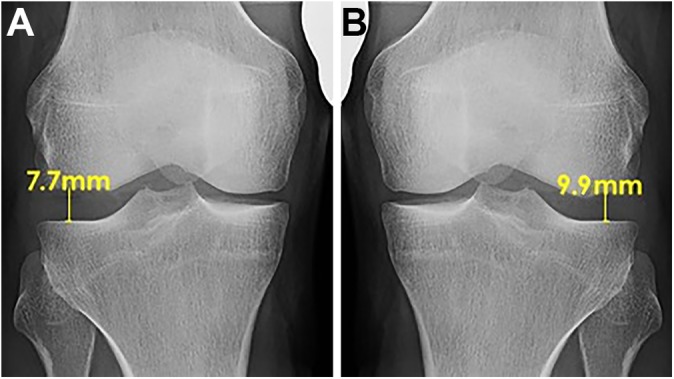
The second measurement technique was performed by identifying the most distal aspect of the popliteal sulcus and drawing a vertical line down to the corresponding point on the lateral tibial plateau (Figure 3).
Figure 3.
Varus stress radiographs resulting from measurement technique 2. This measurement technique was performed by identifying the most distal aspect of the popliteal sulcus and drawing a vertical line down to the corresponding point on the lateral tibial plateau. (A) Measurement technique 2 demonstrated on an uninjured right knee. (B) Measurement technique 2 demonstrated on a left knee with a combined anterior cruciate ligament and fibular collateral ligament injury, resulting in a 2-mm side-to-side difference.
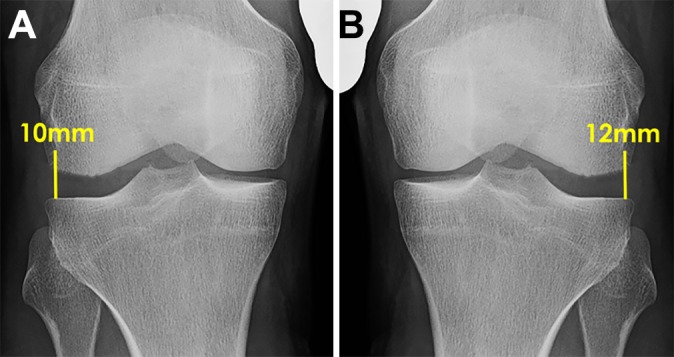
The third measurement technique was performed by first measuring the distance from the most lateral aspect of the lateral tibial plateau to the lateral tibial eminence. The midpoint of this line was identified by measuring half the distance of the length of the line. A line from the midpoint was then drawn to the corresponding point on the femoral condyle (Figure 4).
Figure 4.
Varus stress radiographs resulting from measurement technique 3. This measurement technique was performed by measuring the distance from the most lateral aspect of the lateral tibial plateau to the lateral tibial eminence. The midpoint of this line was identified by measuring half the distance of the length of the line. A line from the midpoint was then drawn to the corresponding point on the femoral condyle. (A) Measurement technique 3 demonstrated on an uninjured right knee. (B) Measurement technique 3 demonstrated on a left knee with a combined anterior cruciate ligament and fibular collateral ligament injury, resulting in a 5.8-mm side-to-side difference.
The SSD was then calculated by comparing the injured and uninjured knees. Digital radiographs were measured by use of OrthoCase Software (Merge Healthcare).
Statistical Analysis
Interrater and intrarater agreement was assessed for radiographic measurements by use of a 2-way random-effects model to calculate the intraclass correlation coefficient (ICC). Each radiograph was independently measured using all 3 techniques by 2 raters (P.W.K., M.E.C.) on 2 separate occasions using OrthoCase Software. The ICC values were interpreted as follows: ICC ≤0.40 = poor agreement; ICC 0.40-0.75 = fair to good agreement; ICC ≥0.75 = excellent agreement.7 All continuous demographic and radiographic variables were reasonably normally distributed.
Results
One hundred consecutive patients who had undergone either isolated FCL reconstruction or combined ACL and FCL reconstructions were identified following a retrospective chart review of patients from the years 2010 to 2016. Of these 100 patients, 98 (13 isolated FCL injuries, 85 combined ACL/FCL injuries) had preoperative varus stress radiographs. Sixty-two patients were treated acutely, while 36 patients were treated more than 6 weeks from the initial injury. No significant differences were found between the acute and chronic groups with respect to SSD in varus gapping. Patient demographics are reported in Table 1. Interrater reliabilities for measuring techniques 1, 2, and 3 were 0.83, 0.86, and 0.91, respectively. Intrarater reliabilities for the 3 measuring techniques were 0.99, 0.77, and 0.99, respectively. The means, ranges, SDs, and standard error of each measurement technique are reported in Table 2.
TABLE 1.
Demographic Information for Patients With FCL Tears and Preoperative Varus Stress Radiographsa
| Total patients, n | 98 |
| Patients with isolated FCL injuries, n | 13 |
| Patients with combined ACL/FCL injuries, n | 85 |
| Age, y (range) | 33.6 (18-69) |
| Males, n | 50 |
| Females, n | 48 |
| Body mass index (range) | 24.6 (18-34) |
| Acute injury, n | 62 |
| Chronic injury, n | 36 |
aACL, anterior cruciate ligament; FCL, fibular collateral ligament.
TABLE 2.
Summary of Side-to-Side Differences in Varus Gapping in Patients With Combined Anterior Cruciate Ligament and Fibular Collateral Ligament Injuriesa
| Mean (Range) | Standard Deviation | Standard Error | |
|---|---|---|---|
| Technique 1 | 2.2 (0-4.9) | 0.20 | 0.091 |
| Technique 2 | 2.4 (0-11.3) | 0.20 | 0.143 |
| Technique 3 | 2.0 (0-4.9) | 0.03 | 0.090 |
| Overall | 2.2 (0-11.3) | 0.20 | 0.064 |
aAll values are expressed as millimeters. Technique 1 was performed by extending a vertical line from the most inferior aspect of the lateral femoral condyle to the corresponding point on the lateral tibial plateau. Technique 2 was performed by identifying the most distal aspect of the popliteal sulcus and drawing a vertical line down to the corresponding point on the lateral tibial plateau. Technique 3 was performed by measuring the distance from the most lateral aspect of the lateral tibial plateau to the lateral tibial eminence.
Discussion
The most important finding of this study was that the amount of SSD in lateral compartment gapping in patients with a grade III FCL injury was lower than the amount of lateral compartment gapping seen in sectioning studies of the same knee in cadaveric models. Furthermore, this study demonstrated 3 reliable and reproducible techniques for clinicians to use to accurately evaluate patients with suspected FCL injuries.
The need for an accurate and reproducible method for diagnosing FCL tears is important. Timely identification of these injuries is essential because a missed or delayed diagnosis has been shown to result in inferior outcomes, especially in the setting of cruciate ligament reconstruction.3,21 While varus laxity and increased heel height on physical examination are both suggestive of an FCL tear,2 these findings are subjective and are far from definitive. Although MRI is nearly universally ordered, recent studies have questioned the utility of this modality, with some studies reporting a sensitivity of only 58% for diagnosing FCL tears on MRI.1
Varus stress radiographs provide reliable, dynamic, and objective data and represent an important tool in the clinician’s armamentarium for diagnosing FCL tears. Although the validity and accuracy of varus stress radiographs in a cadaveric model have been previously reported, our results suggest a slightly lower threshold value required for diagnosing FCL tears in the clinical setting. Based on the accepted measurement technique by LaPrade et al,9 an SSD of 2.7 mm was considered consistent with a grade III tear of the FCL. The results from our study, however, suggest a slightly lower SSD value of 2.2 mm to be indicative of a complete FCL injury.9 However, since 2.2 mm is a mean SSD value, using this measurement as a threshold for a grade III injury will result in some complete FCL tears being missed.
Our results appear similar to the results of more recent literature by McDonald et al19 that also support a lower threshold of 1.99 mm for diagnosing a complete grade III tear of the FCL. Several factors may be responsible for the discrepancy seen in our results compared with the cadaveric model. First, an intact soft tissue envelope may add to the overall resistance encountered during varus stress examination. Additionally, patient guarding with varus stress testing may have led to the decrease in lateral compartment gapping seen in our study.16,17,19,20 Second, LaPrade et al9 evaluated lateral compartment gapping after sectioning of each cadaver’s FCL. In the present study, lateral compartment gapping was compared between each patient’s injured and uninjured knee; this method may be more clinically applicable. A patient’s uninjured knee may be a more accurate control than a nonsectioned cadaveric knee because the patient’s inherent laxity is accounted for.
Although Jacobsen6 evaluated SSD values in a clinical as opposed to a cadaveric setting, several important differences exist compared with our current investigation. First, our study used a clinician-applied load for varus stress, while the Jacobsen study was based on a specialized, pneumatic apparatus called a “gonylaxometer.” The gonylaxometer applied a roughly 9-kg adduction force through the patients’ constrained feet, indirectly applying a varus force through the knee. Although the results from the gonylaxometer were highly reproducible, the results from the clinician-applied load in our study are more applicable to patient care. Second, all participants in the Jacobsen study were healthy volunteers, while the SSD values obtained from our study used patients with a known injury to the FCL (confirmed clinically and radiographically). Additionally, radiograph acquisition and interpretation in the previous study may have been subject to slight magnification error because the images were hard copies and were not on a digital PACS system. Despite these differences, the Jacobsen study came to nearly the same conclusion as our current study—that lateral compartment gapping on varus stress radiographs of greater than 2.0 mm appears diagnostic of an injury to the FCL.
Although Gwathmey et al5 reported on absolute values for lateral compartment gapping for complete PLC injuries in the clinical setting, the authors did not comment on the SSD value seen in patients with an FCL tear. In their study of 27 patients with MRI evidence of PLC injury, the range of lateral compartment gapping was between 7.5 and 36.5 mm. Even more concerning was the SD of 5.6 mm, more than double the value considered positive for diagnosing an FCL tear.
According to our results, technique number 3, using the midpoint of the lateral tibial plateau, resulted in the most reproducible measurement method, with an interrater reliability of 0.91 and an SD of only 0.03 mm. Although the traditional LaPrade technique,9 as measured from the distal-most aspect of the lateral femoral condyle to the corresponding lateral tibial plateau, performed within the excellent range with an ICC of 0.83 and SD of 0.20 mm, it was the least reproducible technique of all 3 measurement methods trialed. Identification of the midpoint of the lateral tibial plateau seemed to be resistant to changes in knee position during radiograph acquisition.
Our study is not without its limitations, including all of the weaknesses inherent in a retrospective study. Both reviewers were nonblinded and were aware that the patient cohort had sustained an FCL injury. Additionally, a majority of the patients included in our study had sustained a combined FCL and ACL injury; only 13 of the 98 patients examined had an isolated FCL tear. Although a concomitant ACL tear could theoretically increase lateral compartment gapping because of the loss of a secondary varus stabilizer, recent literature has shown that the effect of an ACL tear on the SSD is minimal clinically.19 Unlike the cadaveric model, where the effect of individual structures could be evaluated through sequential sectioning, isolated FCL tears in a clinical setting were rare and more commonly occurred in the setting of a concomitant cruciate ligament injury. The inclusion of patients with combined FCL and ACL tears was required in order to increase patient numbers and achieve adequate power.
Conclusion
This study demonstrated a lower SSD value of 2.2 mm to be consistent with a grade III FCL tear on clinician-applied varus stress radiographs in the clinical setting. Although all SSD measurement locations had excellent reliability, the method using the midpoint of the lateral tibial plateau was found to be the most reproducible. Further research is necessary to fully define the optimal measurement technique and corresponding threshold values for diagnosing FCL tears.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: This research was sponsored by the Steadman Philippon Research Institute. P.W.K. has received educational support from Smith & Nephew and research support from DJO. M.T.P. is a consultant for Arthrex and the Joint Restoration Foundation (Allosource) and receives royalties from Arthrex and SLACK Inc. R.F.L. is a consultant for Arthrex, Ossur, and Smith & Nephew; receives royalties from Arthrex and Smith & Nephew; and receives research support from Arthrex, Smith & Nephew, Ossur, and Linvatec.
Ethical approval for this study was obtained from the Vail Valley Medical Center Institutional Review Board (protocol No. 2002-03).
References
- 1. Bonadio MB, Helito CP, Gury LA, Demange MK, Pécora JR, Angelini FJ. Correlation between magnetic resonance imaging and physical exam in assessment of injuries to posterolateral corner of the knee. Acta Ortop Bras. 2014;22(3):124–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Cinque ME, Geeslin AG, Chahla J, et al. The heel height test: a novel tool for the detection of combined anterior cruciate ligament and fibular collateral ligament tears. Arthroscopy. 2017;33(12):2177–2181. [DOI] [PubMed] [Google Scholar]
- 3. Geeslin AG, LaPrade RF. Outcomes of treatment of acute grade-III isolated and combined posterolateral knee injuries: a prospective case series and surgical technique. J Bone Joint Surg Am. 2011;93(18):1672–1683. [DOI] [PubMed] [Google Scholar]
- 4. Geeslin AG, Moulton SG, LaPrade RF. A systematic review of the outcomes of posterolateral corner knee injuries, part 1: surgical treatment of acute injuries. Am J Sports Med. 2016;44(5):1336–1342. [DOI] [PubMed] [Google Scholar]
- 5. Gwathmey FW, Jr, Tompkins MA, Gaskin CM, Miller MD. Can stress radiography of the knee help characterize posterolateral corner injury? Clin Orthop Relat Res. 2012;470(3):768–773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Jacobsen K. Stress radiographical measurement of the anteroposterior, medial and lateral stability of the knee joint. Acta Orthop Scand. 1976;47(3):335–344. [DOI] [PubMed] [Google Scholar]
- 7. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–174. [PubMed] [Google Scholar]
- 8. Laprade RF, Griffith CJ, Coobs BR, Geeslin AG, Johansen S, Engebretsen L. Improving outcomes for posterolateral knee injuries. J Orthop Res. 2014;32(4):485–491. [DOI] [PubMed] [Google Scholar]
- 9. LaPrade RF, Heikes C, Bakker AJ, Jakobsen RB. The reproducibility and repeatability of varus stress radiographs in the assessment of isolated fibular collateral ligament and grade-III posterolateral knee injuries: an in vitro biomechanical study. J Bone Joint Surg Am. 2008;90(10):2069–2076. [DOI] [PubMed] [Google Scholar]
- 10. LaPrade RF, Johansen S, Agel J, Risberg MA, Moksnes H, Engebretsen L. Outcomes of an anatomic posterolateral knee reconstruction. J Bone Joint Surg Am. 2010;92(1):16–22. [DOI] [PubMed] [Google Scholar]
- 11. LaPrade RF, Johansen S, Wentorf FA, Engebretsen L, Esterberg JL, Tso A. An analysis of an anatomical posterolateral knee reconstruction: an in vitro biomechanical study and development of a surgical technique. Am J Sports Med. 2004;32(6):1405–1414. [DOI] [PubMed] [Google Scholar]
- 12. LaPrade RF, Ly TV, Wentorf FA, Engebretsen L. The posterolateral attachments of the knee: a qualitative and quantitative morphologic analysis of the fibular collateral ligament, popliteus tendon, popliteofibular ligament, and lateral gastrocnemius tendon. Am J Sports Med. 2003;31(6):854–860. [DOI] [PubMed] [Google Scholar]
- 13. LaPrade RF, Muench C, Wentorf F, Lewis JL. The effect of injury to the posterolateral structures of the knee on force in a posterior cruciate ligament graft: a biomechanical study. Am J Sports Med. 2002;30(2):233–238. [DOI] [PubMed] [Google Scholar]
- 14. LaPrade RF, Resig S, Wentorf F, Lewis JL. The effects of grade III posterolateral knee complex injuries on anterior cruciate ligament graft force: a biomechanical analysis. Am J Sports Med. 1999;27(4):469–475. [DOI] [PubMed] [Google Scholar]
- 15. LaPrade RF, Terry GC. Injuries to the posterolateral aspect of the knee: association of anatomic injury patterns with clinical instability. Am J Sports Med. 1997;25(4):433–438. [DOI] [PubMed] [Google Scholar]
- 16. LaPrade RF, Wentorf F. Diagnosis and treatment of posterolateral knee injuries. Clin Orthop Relat Res. 2002;(402):110–121. [DOI] [PubMed] [Google Scholar]
- 17. LaPrade RF, Wentorf FA, Crum JA. Assessment of healing of grade III posterolateral corner injuries: an in vivo model. J Orthop Res. 2004;22(5):970–975. [DOI] [PubMed] [Google Scholar]
- 18. Levy BA, Dajani KA, Morgan JA, Shah JP, Dahm DL, Stuart MJ. Repair versus reconstruction of the fibular collateral ligament and posterolateral corner in the multiligament-injured knee. Am J Sports Med. 2010;38(4):804–809. [DOI] [PubMed] [Google Scholar]
- 19. McDonald LS, Waltz RA, Carney JR, et al. Validation of varus stress radiographs for anterior cruciate ligament and posterolateral corner knee injuries: a biomechanical study. Knee. 2016;23(6):1064–1068. [DOI] [PubMed] [Google Scholar]
- 20. Moulton SG, Geeslin AG, LaPrade RF. A systematic review of the outcomes of posterolateral corner knee injuries, part 2: surgical treatment of chronic injuries. Am J Sports Med. 2015;44(6):1616–1623. [DOI] [PubMed] [Google Scholar]
- 21. Noyes FR, Jetter AW, Grood ES, Harms SP, Gardner EJ, Levy MS. Anterior cruciate ligament function in providing rotational stability assessed by medial and lateral tibiofemoral compartment translations and subluxations. Am J Sports Med. 2015;43(3):683–692. [DOI] [PubMed] [Google Scholar]
- 22. Ranawat A, Baker CL III, Henry S, Harner CD. Posterolateral corner injury of the knee: evaluation and management. J Am Acad Orthop Surg. 2008;16(9):506–518. [PubMed] [Google Scholar]
- 23. Veltri DM, Deng XH, Torzilli PA, Warren RF, Maynard MJ. The role of the cruciate and posterolateral ligaments in stability of the knee: a biomechanical study. Am J Sports Med. 1995;23(4):436–443. [DOI] [PubMed] [Google Scholar]