Abstract
Aims: Most previous prospective studies have examined workplace social capital as a resource of the individual. However, literature suggests that social capital is a collective good. In the present study we examined whether a high level of workplace aggregated social capital (WASC) predicts a decreased risk of individual-level long-term sickness absence (LTSA) in Danish private sector employees. Methods: A sample of 2043 employees (aged 18–64 years, 38.5% women) from 260 Danish private-sector companies filled in a questionnaire on workplace social capital and covariates. WASC was calculated by assigning the company-averaged social capital score to all employees of each company. We derived LTSA, defined as sickness absence of more than three weeks, from a national register. We examined if WASC predicted employee LTSA using multilevel survival analyses, while excluding participants with LTSA in the three months preceding baseline. Results: We found no statistically significant association in any of the analyses. The hazard ratio for LTSA in the fully adjusted model was 0.93 (95% CI 0.77–1.13) per one standard deviation increase in WASC. When using WASC as a categorical exposure we found a statistically non-significant tendency towards a decreased risk of LTSA in employees with medium WASC (fully adjusted model: HR 0.78 (95% CI 0.48–1.27)). Post hoc analyses with workplace social capital as a resource of the individual showed similar results. Conclusions: WASC did not predict LTSA in this sample of Danish private-sector employees.
Keywords: Social capital, trust, justice, psychosocial, sick leave, multilevel analysis, occupational health, workplace, private sector, epidemiology
Introduction
Following in particular the work of Bourdieu, Coleman and Putnam [1-3] the concept of ‘social capital’ has gained wide attention within a range of disciplines and from a number of scholars during the last three decades [4]. In public health research, social capital has been defined as ‘resources that are accessed by individuals as a result of their membership of a network or a group’ [5, p. 291]. In this research, key components of social capital are mutual trust, reciprocity, shared norms and networks [4].
Recently, interest in social capital at the workplace has increased, in particular in the Nordic countries. Studies suggest that high workplace social capital may protect or even enhance employee health [6-11]. Healthy norms of behaviour may be easier and more rapidly adopted within workplaces with high social capital, and deviant health-related behaviours may more tightly socially controlled [12]. Further, high workplace social capital may be associated with more emotional support and mutual respect at the workplace and thereby may reduce health-hazardous psychophysiological stress responses [12].
Empirical evidence on the association of workplace social capital and health, however, is weak, as the extant research faces some important limitations. First, the majority of studies are cross-sectional [13]. Most prospective epidemiological evidence on workplace social capital and health comes from one particular cohort study, namely the Finnish Public Sector (FPS) study that has analysed workplace social capital in relation to all-cause mortality [7], self-rated health [8], hypertension [9] and depression [10, 11]. Consequently, evidence on the putative association of workplace social capital and health is disproportionally based on public-sector employees in Finland. Only recently have prospective studies from other countries been added, showing associations of workplace social capital with sickness absence in Danish employees [6] and psychological distress in employees in Japan [14] and Belgium [15].
Second, whereas individual-level social capital, i.e. social capital analysed as a characteristic of the individual, was associated with health endpoints in several studies [6-11, 14, 15], group-level social capital (e.g. mean social capital scores of work units) has been investigated less, and shown in general weaker or no associations with employees’ health [7-11, 15]. This is a reason for concern, as it has been argued that social capital is a group characteristic and not an individual characteristic [5].
Long-term sickness absence (LTSA) has been shown to be a reliable proxy for employees’ health, as it predicts both disability pensioning [16] and mortality [17]. To our knowledge, only two studies so far have examined workplace social capital and risk of LTSA prospectively. The BELSTRESS study [15] found that individual-level but not group-level workplace social capital predicted LTSA in a sample of Belgian public- and private-sector employees. BELSTRESS, however, had only a limited measure of workplace social capital consisting of two single items measuring reciprocity in social support from colleagues and supervisors, respectively [15]. The other study found that individual-level workplace social capital predicted risk of LTSA in a random sample of Danish employees, but that the association was attenuated when adjusting for occupational grade [6]. When stratified by occupational grade, individual-level workplace social capital predicted LTSA among employees of high occupational grade but not among those of low occupational grade. Group-level workplace social capital was not measured in this study [6].
In this article, we examine the prospective association of group-level social capital (workplace aggregated social capital, WASC) with the risk of LTSA in a sample of Danish private-sector employees. Based on the findings from the previous Danish study on individual-level workplace social capital and risk of LTSA, we hypothesized that WASC would predict risk of LTSA. We further explored whether associations were different for employees of high, medium and low socioeconomic position.
Methods
Study design and sample
This is a prospective cohort study linking survey data on WASC to register information on LTSA with a 52 week follow-up.
We assessed workplace social capital in the Danish National Working Environment Survey (DANES) and LTSA in the Danish Register for Evaluation of Marginalization (DREAM) at the National Labour Market Authority [18]. Briefly, DANES was a national Danish study on working conditions and health. It consisted, among other elements, of a workplace sample, comprising 268 workplaces that we used for the analysis in this article. Detailed descriptions of the DANES study are published elsewhere [19, 20].
Selection of participants
Figure 1 depicts the flowchart for creating the sample. Workplaces were selected based on their unique Central Business Register number (‘Det Centrale Virksomhedsregister (CVR)’ number) via Statistics Denmark. The CVR number relates to the legal unit of the company but not to its physical location. Thus, it is possible that in some cases employees from the same company have worked at different physical locations.
Figure 1.
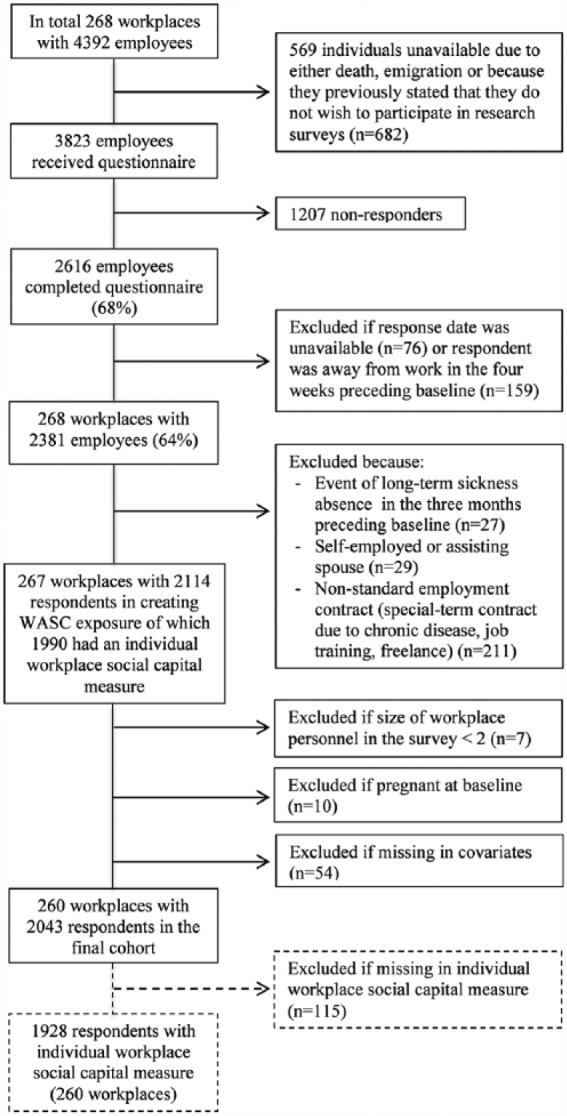
Flowchart of the construction of the study sample.
We stratified the workplaces by the number of employees into three categories: small, medium and large workplaces with 10–99, 100–249 and 250–499 employees, respectively. Workplaces with 500 or more employees were excluded because they could easily be identified and workplaces with less than 10 employees were excluded because they were not available at Statistics Denmark. For each of the three workplace size categories we selected the number of workplaces according to their distribution in Denmark. In total 268 workplaces where identified and within these we randomly selected employees based on their unique personal identification number (CPR number). We selected 12 participants from small workplaces (or all employees if the workplace consisted of 12 employees or less), 24 participants from medium-size workplaces and 60 participants from large workplaces. From October 2008 to March 2009, we sent out questionnaires on working conditions and health to 3823 employees working at these workplaces.
Non-responders first received two reminders and were then invited to participate in a telephone interview. In total, 2616 employees completed the questionnaire (68% response rate) and the final sample consisted of 2043 respondents from 260 workplaces: 191 small, 49 medium and 20 large workplaces with 1048, 537 and 458 employees, respectively (Figure 1 depicts the exclusion process).
Measuring WASC
To obtain WASC, we first measured individual-level workplace social capital using five items, covering mutual trust (two items) and justice at work (three items), two core dimensions of social capital in a workplace context [21]. All five items had been documented and psychometrically tested in the Copenhagen Psychosocial Questionnaire, version II (COPSOQ-II) [22]: (i) ‘Can you trust the information that comes from the management?’; (ii) ‘Do the employees withhold information from each other?’; (iii) ‘Is your work recognized and appreciated by the management?’; (iv) ‘Are conflicts resolved in a fair way?’; and (v) ‘Is the work distributed fairly?’.
All items were rated on a five-point scale, ranging from 0 (‘to a very small extent’) to 4 (‘to a very large extent’). Item (ii) was reversely coded. The responses were summed up resulting in individual workplace social capital scores from 0–20 with higher scores indicating higher workplace social capital (Cronbach’s alpha = 0.78). Confirmatory factor analysis (CFI) showed an adequate fit to the data (χ2 = 56.819, df = 5, p < 0.001; RMSEA = 0.072; CFI = 0.981; TLI= 0.963; SRMR = 0.022). Standardized factor loadings were between 0.45 and 0.81. According to the suggested cut-off points by Hu and Bentler both the CFI, TLI and SRMR are acceptable, whereas the RMSEA was slightly above the recommended level of 0.06 [23].
We generated the WASC score by calculating the mean workplace social capital score for each workplace and assigning this score to all employees working in the same workplace. Respondents who had missing social capital items (n = 115) were also assigned the WASC score of their respective workplace.
Measuring LTSA
We measured the first occurrence of LTSA from the day respondents filled in the questionnaire and 52 weeks ahead in the DREAM register, which has been demonstrated as a valid source for research purposes [18]. DREAM has information on all Danish social transfer payments on a weekly basis since July 1991. In 2008, spells of sickness absence of 22 days (since 2012: 31 days) or longer were registered in DREAM and consequently, we used the first occurrence of such a spell as the outcome of this study.
Measuring covariates
As covariates, we recorded sex, age, survey method (postal or web-based self-administered questionnaire versus telephone interview), cohabitation with a partner or spouse, socioeconomic position, self-rated health, chronic disease at baseline, and workplace size.
We measured socioeconomic position using the European Socio-Economic Classification (ESeC) categorized into three subgroups [24]. Self-rated health was measured with a single item: ‘In general, how do you think your health is?’ with responses categorized into ‘good’, ‘medium’ and ‘poor’ health. We classified participants with a chronic disease if they reported any of the following diagnoses: diabetes, ischaemic heart disease, back disorder, or depression/other psychological disorders.
Statistical analyses
Participants were followed from questionnaire response until the onset of LTSA or censoring due to early retirement, retirement pension, maternity leave, emigration, death or end of follow-up, whichever came first. Using multilevel survival models [25] with the Weibull distribution we calculated crude and adjusted hazard ratios (HRs) and 95% confidence intervals (CI) for the prospective association of WASC score at baseline with time to the onset of LTSA or censoring, accounting for the clustering of employees within workplaces.
The statistical models were incrementally adjusted for age, sex and survey method (model I), cohabitation and socioeconomic position (model II), and self-rated health, chronic disease and workplace size (model III). WASC was analysed both as a continuous variable (one standard deviation increment of WASC) and as a categorical variable (WASC score divided into tertiles). Effect modification by socioeconomic position was analysed as departure from multiplicativity.
All analyses were conducted using the ‘mestreg’ command in the statistical software package Stata 14 (StataCorp LP, College Station, Texas, USA). We tested possible violations of the proportional hazard assumption by using Schoenfeld residuals and calculated the fraction of variance in workplace social capital attributable to variation between workplaces by using intra-class correlation (ICC) [25].
Post hoc analyses
We conducted two post hoc analyses with the purpose of investigating the robustness of the results. First, we examined the association of each WASC item separately with risk of LTSA. Second, we replaced WASC with individual-level workplace social capital as the predictor of LTSA.
Results
Study sample characteristics and distribution of WASC
Table I shows the characteristics of the study participants at baseline. WASC scores ranged from 7.5 to 19.0 with a mean of 12.9 (SD 1.6). Mean age was 43 years (SD 11.6) and the majority of the sample was men (61.5%) and working-class employees (43.6%). About 5% reported poor self-rated health and 29% had a chronic disease at baseline. The mean number of participating employees nested within the same workplace was 8 (range: 2–47). The amount of variation in workplace social capital explained by workplaces was 8.8% (data not shown in table).
Table I.
Study participants’ characteristics at baseline: 2043 Danish employees nested within 260 private workplaces.
| N | % | Mean | SD | |
|---|---|---|---|---|
| WASC1 | 12.88 | 1.56 | ||
| WASC range: 7.5–19.0 | ||||
| Age | 43.29 | 11.55 | ||
| Age range: 18–64 years | ||||
| Sex | ||||
| Women | 787 | 38.52 | ||
| Men | 1256 | 61.48 | ||
| Method | ||||
| Post/web | 1647 | 80.62 | ||
| Telephone interviews | 396 | 19.38 | ||
| Cohabitation | ||||
| Yes | 1594 | 78.02 | ||
| No | 449 | 21.98 | ||
| Socioeconomic position | ||||
| Salariat | 676 | 33.09 | ||
| Intermediate | 476 | 23.30 | ||
| Working class | 891 | 43.61 | ||
| Self-rated health | ||||
| Good | 1161 | 56.83 | ||
| Medium | 775 | 37.93 | ||
| Poor | 107 | 5.24 | ||
| Chronic disease | ||||
| Yes | 596 | 29.17 | ||
| No | 1,447 | 70.83 | ||
| Workplace size | ||||
| Small | 1048 | 51.30 | ||
| Medium | 537 | 26.28 | ||
| Large | 458 | 22.42 |
N = number of participants 1) WASC = Workplace Aggregated Social Capital.
When we compared non-responders and responders, we found that non-responders were more likely to be men and more likely to be of younger age compared to responders (data not shown in table).
WASC and the onset of LTSA
During the one-year follow-up period, 107 (5.2%) of the 2043 participants had an episode of LTSA and 74 (3.6%) were censored due to early retirement (n = 34, 46.0%), maternity leave (n = 24, 32.4%), old age pension (n = 12, 16.2%) or emigration (n = 4, 5.4%). Mean time to the onset of LTSA among those who had an event during follow-up was 23.1 weeks (SD 14.3).
Table II presents the crude and adjusted HR for the prospective association of WASC at baseline and the onset of LTSA. In the crude analysis, the HR for a one standard deviation increase in WASC was 0.86, indicating that higher WASC was associated with a reduced risk of LTSA. However, the 95% CI included unity (0.71–1.04), thus the result was not statistically significant. Adjustments for covariates incrementally attenuated the estimate with an HR of 0.93 (95% CI = 0.77–1.13) in the most adjusted model.
Table II.
Workplace aggregated social capital (WASC) at baseline and the onset of long-term sickness absence (LTSA) during the one-year follow-up: 2043 Danish employees nested within 260 private workplaces.
| Predictor | N | Cases | Crude |
Model I |
Model II |
Model III |
||||
|---|---|---|---|---|---|---|---|---|---|---|
| HR | (95%CI) | HR | (95%CI) | HR | (95%CI) | HR | (95%CI) | |||
| WASC continuous1) | 2043 | 107 | 0.86 | (0.71–1.04) | 0.84 | (0.70–1.02) | 0.89 | (0.74–1.07) | 0.93 | (0.77–1.13) |
| WASC categorical2) | ||||||||||
| Low | 633 | 41 | 1 | (reference) | 1 | (reference) | 1 | (reference) | 1 | (reference) |
| Medium | 655 | 29 | 0.69 | (0.42–1.14) | 0.70 | (0.43–1.14) | 0.76 | (0.47–1.29) | 0.78 | (0.48–1.27) |
| High | 648 | 37 | 0.90 | (0.57–1.43) | 0.88 | (0.55–1.39) | 0.98 | (0.62–1.54) | 1.10 | (0.69–1.74) |
Hazard ratios (HRs) using multilevel Cox proportional hazard analysis: 1) One standard deviation (SD) increment; 2) categorized as tertiles.
When using WASC as a categorical instead of a continuous variable, we did not find any statistically significant associations. There was a tendency for a curvilinear association, with the highest risk of LTSA among those with low or high WASC and the lowest risk among those with medium WASC in all models. However, none of the results were statistically significant (Table II).
Among the covariates, higher age, female sex, living alone, poor self-rated health and chronic disease at baseline predicted risk of LTSA in the fully adjusted model (results available on request from the first author). The association of WASC and LTSA was not modified by socioeconomic position (p = 0.31, results not shown in table).
Schoenfeld residuals tests showed that the proportional hazard assumption was fulfilled in all analyses.
Post hoc analyses
None of the five WASC items showed statistically significant associations with LTSA when analysed separately (data not shown). Analyses of individual-level workplace social capital instead of WASC were also statistically non-significant. The HR of LTSA for a 1 SD increase of individual-level workplace social capital was 0.85 (95% CI = 0.70–1.03) in the crude analysis and 0.94 (95% CI = 0.77–1.14) in the fully adjusted analysis. When individual-level workplace social capital was used as a categorical variable, the HRs for medium and high workplace social capital were 0.62 (95% CI = 0.38–1.01) and 0.67 (95% CI = 0.42–1.08), respectively, in the crude analyses. In the adjusted analyses, the HRs were 0.72 (95% CI = 0.44–1.17) and 0.85 (95% CI = 0.52–1.40), respectively.
Discussion
The DANES study could not confirm that higher workplace social capital, measured as a characteristic of the workplace, was associated with a decreased risk of LTSA. Neither WASC nor individual-level workplace social capital significantly predicted risk of LTSA.
Comparisons with previous studies
To our knowledge, the only other prospective study to date examining WASC as a risk factor of LTSA was conducted in the BELSTRESS study, which also did not find an association between WASC and LTSA [15]. In addition, analyses from the FPS study failed to show associations between WASC hypertension [9] and depression[10, 11]. The association of WASC with risk of low self-rated health, though, approached statistical significance in FPS [8] and there was a suggestive, albeit not statistically significant, association of co-worker assessed workplace social capital with all-cause mortality [7]. Importantly, individual-level workplace social capital predicted health endpoints in FPS, and LTSA in BELSTRESS, whereas in DANES neither WASC nor individual-level workplace social capital predicted LTSA.
Possible reasons for these conflicting results might be differences in the study sample (public sector in FPS, public and private sector in BELSTRESS, private sector in DANES) and the definition, number and size of workplaces. The term workplace referred to 32 large companies or public administrations in BELSTRESS, 260 various-sized companies in DANES and more than 1500 smaller work units in FPS. Thus, the aggregation level of workplace social capital differed between the studies, and it is unknown which level would have been the most appropriate.
Further, all three studies used different questions to assess workplace social capital. BELSTRESS was limited to items on social support from colleagues and supervisors, whereas DANES combined items on trust and justice, two core dimensions of workplace social capital [21]. However, FPS probably had the most comprehensive approach by combining items on trust, justice, collaboration, social support and cohesion [26].
Variation in workplace social capital explained by the workplace
In our study, the workplaces accounted for only about 9% of the variation in the individual workplace social capital scores. This is much lower than the 21 to 22% explained variation reported in FPS [8, 26]. A possible explanation is that in our study a workplace was defined broadly at the company level, not allowing us to differentiate between different work units or work groups within the same workplace. In contrast, FPS aggregated data at a more detailed work-unit level.
Strengths and limitations
Strengths of the study are the prospective design and the assessment of social capital as resources of social entities (i.e. workplaces) that are in concordance with the conceptualization of social capital [5]. Further, by using the well-validated DREAM register for assessing LTSA [18] we omitted loss-to-follow-up and recall bias in the assessment of LTSA and were able to adjust for LTSA prior baseline. Covariates, such as higher age, female sex, living alone, poor self-rated health and chronic disease at baseline predicted risk of LTSA in accordance with prior studies [27], indicating that the absence of association between WASC and LTSA was not due to measurement errors in the assessment of LTSA. Finally, we consider the use of a random sample of private-sector employees as a strength as the majority of prospective analyses on workplace social capital and health was conducted in FPS, which is limited to the public sector [7-11, 26, 28].
A major weakness of the study is the low amount of variance in WASC that was explained by workplace. Thus, our assessment of exposure was imprecise and we cannot rule out that this might have been a reason for not detecting an association between WASC and LTSA. Further, it is a limitation that workplace social capital and potential confounders were only assessed at baseline. Repeated measurements would have yielded more precise measurements and enabled us to investigate the effect of changes in WASC on risk of LTSA. Additionally, we had no information regarding participants’ potential changes of workplace. This might have caused an underestimation of the association as it is possible that some employees changed to another workplace because social capital was low at their current workplace, and were misclassified as exposed to low social capital despite this change.
The response rate in the study sample was moderate (68%) with a lower response rate among men and younger employees. Thus, we cannot claim that our sample was representative of the private-sector workforce in Denmark. Further, our analyses were limited to LTSA and our results cannot be generalized to short-term sickness absence.
We measured workplace social capital based on an index of five items representing trust and justice. Following that no unambiguous conceptualization of social capital or workplace social capital exists, the scale in this study reflects one attempt to measure and capture workplace social capital. It cannot be ruled out that different measurements of the concept, for example a recently introduced measure that distinguishes between bonding, bridging and linking workplace social capital [29], may have yielded different results.
Conclusions and perspectives
We found no evidence that higher workplace social capital, measured as a resource of the workplace or of the individual, decreased the risk of LTSA among employees from the Danish private sector. We suggest that future studies on workplace social capital and health and sickness absence aggregate individual responses on small work units or formal and informal work teams within the workplace to get more accurate measures of workplace social capital as a collective resource.
Footnotes
Conflict of interest: The authors declare that there is no conflict of interest.
Funding: This work was supported by grants from the Danish Working Environment Research Fund (grant numbers: 9-2011-13 and 10-2016-03). The funding sources had no further influence on the study design; in the collection, analyses, interpretation of data; in the writing of the paper, or in the decision to submit the paper for publication. According to Danish law, questionnaire and register based studies do not need approval by ethical and scientific committees [30].
References
- [1]. Bourdieu P. The forms of capital. In: Richardson J. (ed) Handbook of theory and research for the sociology of education. New York: Greenwood Press, 1986, pp.241–58. [Google Scholar]
- [2]. Coleman JS. Social capital. Foundations of social theory. USA: The Belknap Press of Havard University Press, 1990, pp.300–24. [Google Scholar]
- [3]. Putnam RD. Bowling alone: The collapse and revival of American community. New York: Simon & Schuster Paperbacks, 2000. [Google Scholar]
- [4]. Islam MK, Merlo J, Kawachi I, et al. Social capital and health: Does egalitarianism matter? A literature review. Int J Equity Health 2006;5:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5]. Kawachi I, Berkman LF. Social capital, social cohesion, and health. In: Berkman LF, Kawachi I, Glymour MM. (eds) Social Epidemiology. 2nd ed. New York: Oxford University Press, 2000, pp.290–319. [Google Scholar]
- [6]. Rugulies R, Hasle P, Pejtersen JH, et al. Workplace social capital and risk of long-term sickness absence. Are associations modified by occupational grade? Eur J Public Health 2016;26:328–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7]. Oksanen T, Kivimäki M, Kawachi I, et al. Workplace social capital and all-cause mortality: A prospective cohort study of 28 043 public-sector employees in Finland. Am J Public Health 2011;101:1742–1748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8]. Oksanen T, Kouvonen A, Kivimäki M, et al. Social capital at work as a predictor of employee health: Multilevel evidence from work units in Finland. Soc Sci Med 2008;66:637–649. [DOI] [PubMed] [Google Scholar]
- [9]. Oksanen T, Kawachi I, Jokela M, et al. Workplace social capital and risk of chronic and severe hypertension: A cohort study. J Hypertens 2012;30:1129–1136. [DOI] [PubMed] [Google Scholar]
- [10]. Oksanen T, Kouvonen A, Vahtera J, et al. Prospective study of workplace social capital and depression: Are vertical and horizontal components equally important? J Epidemiol Community Health 2010;64:684–689. [DOI] [PubMed] [Google Scholar]
- [11]. Kouvonen A, Oksanen T, Vahtera J, et al. Low workplace social capital as a predictor of depression: The Finnish Public Sector study. Am J Epidemiol 2008;167:1143–1151. [DOI] [PubMed] [Google Scholar]
- [12]. Kawachi I, Kennedy BP, Glass R. Social capital and self-rated health: A contextual analysis. Am J Public Health 1999;89:1187–1193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13]. Murayama H, Fujiwara Y, Kawachi I. Social capital and health: A review of prospective multilevel studies. J Epidemiol 2012;22:179–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14]. Tsuboya T, Tsutsumi A, Kawachi I. Change in psychological distress following change in workplace social capital: Results from the panel surveys of the J-HOPE study. Occup Environ Med. 2015;72:188–194. [DOI] [PubMed] [Google Scholar]
- [15]. De Clercq B, Clays E, Janssens H, et al. Health behaviours as a mechanism in the prospective relation between workplace reciprocity and absenteeism: A bridge too far? PLoS One 2015;10:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16]. Lund T, Kivimäki M, Labriola M, et al. Using administrative sickness absence data as a marker of future disability pension: The prospective DREAM study of Danish private sector employees. Occup Environ Med 2008;65:28–31. [DOI] [PubMed] [Google Scholar]
- [17]. Kivimäki M, Head J, Ferrie JE, et al. Sickness absence as a global measure of health: Evidence from mortality in the Whitehall II prospective cohort study. BMJ 2003;327:364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18]. Burr H, Pedersen J, Hansen JV. Work environment as predictor of long-term sickness absence: Linkage of self-reported DWECS data with the DREAM register. Scand J Public Health 2011;39:147–152. [DOI] [PubMed] [Google Scholar]
- 19]. Bjorner JB, Burr H, Feveile H, et al. Ændringer i det danske arbejdsmiljø fra 2005–2008 [Changes in the Danish working environment from 2005–2008]. Copenhagen: Det Nationale Forskningscenter for Arbejdsmiljø [National Research Centre for the Working Environment], 2010. [Google Scholar]
- [20]. Thorsen SV, Jensen PH, Bjorner JB. Psychosocial work environment and retirement age: A prospective study of 1876 senior employees. Int Arch Occup Environ Health 2016;89:891–900. [DOI] [PubMed] [Google Scholar]
- [21]. Olesen KG, Thoft E, Hasle P, et al. Virksomhedens sociale kapital – Hvidbog [Organisational social capital – White paper]. Copenhagen: Arbejdsmiljørådet [The Working Environment Council], 2008. [Google Scholar]
- 22]. Pejtersen JH, Kristensen TS, Borg V, et al. The second version of the Copenhagen Psychosocial Questionnaire. Scand J Public Health 2010;38:8–24. [DOI] [PubMed] [Google Scholar]
- [23]. Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Equ Modeling 1999;6:1–55. [Google Scholar]
- 24]. Harrison E, Rose D. The European Socio-Economic Classification (ESeC) – User guide. Colchester, UK: Institute for Social and Economic Research, University of Essex, 2006, pp.1–22. [Google Scholar]
- [25]. Gelman A, Hill J. Data analysis using regression and multilevel/hierarchical models. New York: Cambridge University Press, 2006. [Google Scholar]
- [26]. Kouvonen A, Kivimäki M, Vahtera J, et al. Psychometric evaluation of a short measure of social capital at work. BMC Public Health 2006;6:251–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27]. Allebeck P, Mastekaasa A. Chapter 5. Risk factors for sick leave – General studies. Scand J Public Health Suppl 2004;63:49–108. [DOI] [PubMed] [Google Scholar]
- [28]. Väänänen A, Kouvonen A, Kivimäki M, et al. Workplace social capital and co-occurrence of lifestyle risk factors: The Finnish Public Sector study. Occup Environ Med 2009;66:432–437. [DOI] [PubMed] [Google Scholar]
- [29]. Borg V, Cayuelas N, Clausen T. Udvikling af en ny metode til undersøgelse af social kapital på arbejdspladsen – Dokumentationsrapport [Developing a new method for examination of social capital at the workplace. A documentation report]. Copenhagen: Det Nationale Forskningscenter for Arbejdsmiljø [National Research Centre for the Working Environment], 2014. [Google Scholar]
- [30]. Den Centrale Videnskabsetiske Komité [The Danish National Committee on Biomedical Research]. Act on Research Ethics Review of Health Research Projects [Internet]. Copenhagen: Den Centrale Videnskabsetiske Komité, http://www.nvk.dk/english/act-on-research (2013, accessed 14 July 2017). [Google Scholar]


