Abstract
Rationale: Bronchoscopy is commonly used for the diagnosis of suspicious pulmonary nodules discovered on computed tomographic (CT) imaging of the chest. Procedural CT imaging for bronchoscopy planning is often completed weeks to months before the date of a scheduled bronchoscopy, which may not allow discovery of a decrease in nodule size or resolution before the bronchoscopic procedure.
Objectives: To determine whether same-day CT imaging of the chest discovers partial or total resolution of some lung nodules and thereby reduces unnecessary bronchoscopic procedures.
Methods: We performed a prospective case series study of patients undergoing navigational bronchoscopy using a new technology requiring same-day preprocedural CT imaging at one university teaching hospital. Patients scheduled to undergo bronchoscopy who were found to have partial or complete resolution of their lesion on the same-day CT exam leading to the cancellation of their procedure were identified and further characterized.
Measurements and Main Results: From January 2015 to June 2016, 116 patients were scheduled for navigational bronchoscopy for the diagnosis of a pulmonary lesion. Of the 116 patients scheduled, 8 (6.9%) had a decrease in size or resolution of their lesion, leading to the cancellation of their procedure. The number needed to screen to prevent one unnecessary procedure was 15. For cancelled cases, the average time from initial CT prompting referral for bronchoscopy to the day of procedure scan was 53 days.
Conclusions: Time from initial imaging to day of procedure is variable, occasionally allowing enough time for lesions to resolve, thereby obviating the need for biopsy. Same-day imaging may decrease unnecessary procedural risk.
Keywords: pulmonary nodule, pulmonary mass, nodule resolution, bronchoscopy
The National Lung Screening Trial found a 20% reduction in lung cancer–related deaths in patients screened with annual low-dose computed tomographic (CT) chest scanning (1). This trial subsequently led to the endorsement of lung cancer screening by the United States Preventive Services Task Force as well as Medicare coverage for low-dose CT scans (2). A total of 10 million CT scans of the chest are performed in the United States annually, with this number predicted to increase due to the recent National Lung Screening Trial findings (3). Due to this increased vigilance for lung cancer screening, an increase in diagnostic procedures is likely to follow.
The percentage of all lung nodules resolving on interval imaging at 1–3 years has been studied, with a resolution rate cited anywhere from 40 to 80% in the radiology literature (4–6). These studies examined all nodules, including low-risk cases (small size, rounded non–irregular/spiculated borders, no smoking history, no prior malignancy) being managed conservatively with serial imaging, likely accounting for the high percentage of nodule resolution. Current American College of Chest Physician guidelines on nodule management recommend that patients with nodules that fall into an intermediate- to higher-risk category who are surgical candidates may undergo definitive testing before surgical resection (7). In addition, the guidelines also state that, in patients with peripheral lung lesions difficult to reach with conventional bronchoscopy, electromagnetic navigation bronchoscopy (ENB) is recommended if the equipment and the expertise are available (7) or a CT-guided transthoracic biopsy if ENB is unavailable.
ENB uses a three-dimensional bronchial tree constructed from a prior CT scan of the chest to map an endobronchial route to the target lesion (8). An electromagnetic field is then paired to the virtual bronchial tree, allowing intraoperative navigational assistance. The earlier-generation ENB technologies (Superdimension, Minneapolis, MN) used previous scans completed at the time of diagnosis. However, these scans were often performed weeks to months before the patient was referred to a specialist and scheduled for their procedure.
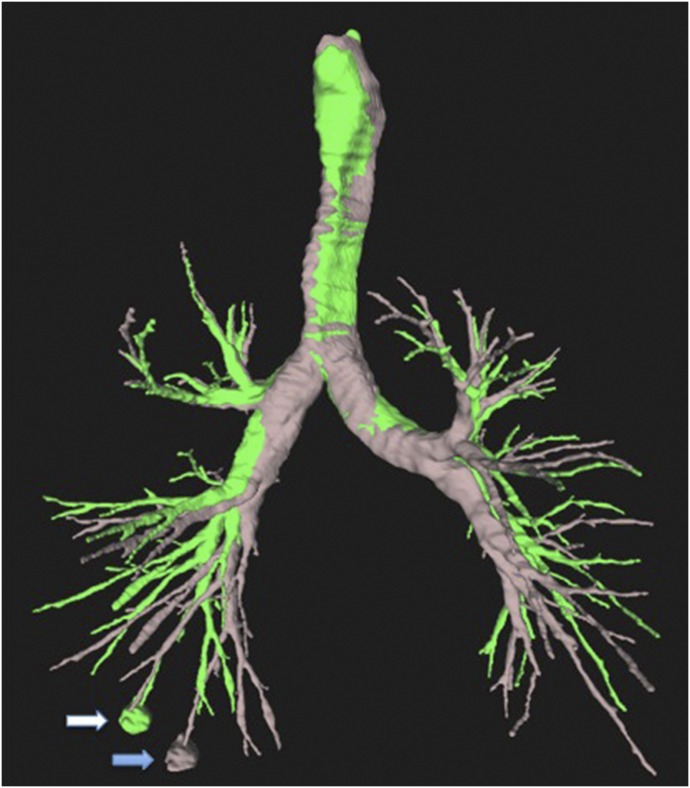
A newer ENB platform (Veran Medical Technologies, St. Louis, MO) allowing both ENB and electromagnetic-guided transthoracic needle aspiration has attempted to decrease diagnostic error by obtaining a repeat CT scan on the same day as the procedure. The rationale for the same-day procedural CT scan is to use the ENB platform technology to pair both an expiratory and inspiratory CT scan to allow the software to build a virtual airway model, which localizes the nodule and compensates for respiratory variation (Figure 1) (9). Prior CT studies have shown that there is significant nodule movement between inspiration and expiration (Figure 2), which may adversely affect diagnostic yields (10).
Figure 1.
Computed tomographic (CT) reconstruction of a right lower lobe pulmonary nodule (arrows) revealing 32 mm of movement between inspiration (blue arrow) and expiration (white arrow).
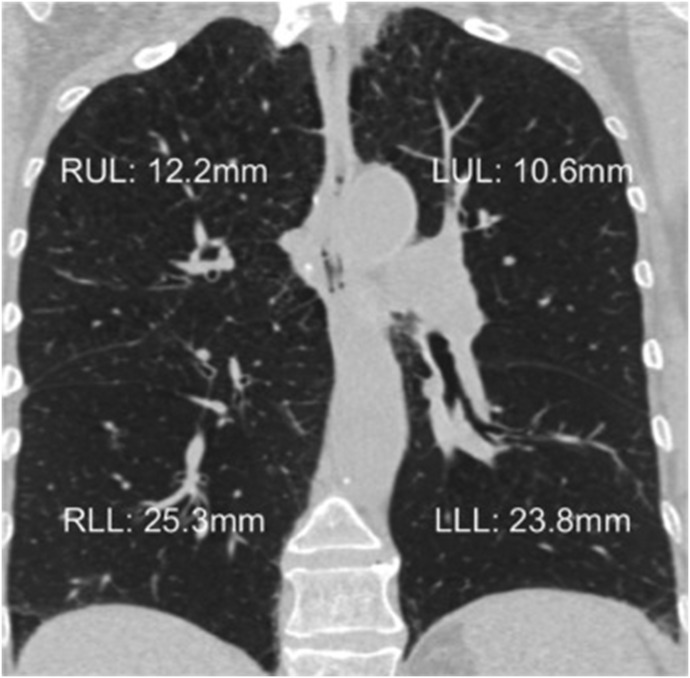
Figure 2.
Average nodule movement per lobe. LLL = left lower lobe; LUL = left upper lobe; RLL = right lower lobe; RUL = right upper lobe. Reprinted by permission from Reference 10.
Intermediate- to high-risk pulmonary nodules that have been referred for a bronchoscopic tissue diagnosis have a rate of resolution that is not well described in the literature. In a study by Zhao and colleagues (11), 750 patients underwent CT surveillance for pulmonary nodules. A total of 964 nodules with at least one noncalcified, solid, indeterminate, intraparenchymal nodule at baseline were included and were re-examined at a 3-month follow-up CT examination, revealing a 7.7% nodule resolution rate.
In addition to nodule resolution on same-day imaging, there is also a potential to identify disease progression that may alter the diagnostic plan of care. We theorized that repeat imaging on the day of a bronchoscopic procedure may uncover a previously unreported percentage of intermediate- to high-risk nodules that have decreased in size or resolved. These nodules would no longer need a biopsy, thereby preventing unnecessary procedures and improving patient safety.
Methods
This was a prospective case series, with all consecutive patients scheduled for ENB bronchoscopy at the Johns Hopkins Hospital (Baltimore, MD) from January 2015 to June 2016 included in the study. Included patients were scheduled for an ENB with or without mediastinal staging using endobronchial ultrasound–guided transbronchial needle aspiration. All ENBs performed used the Veran navigational platform (Veran Medical Technologies), which requires an inspiratory and expiratory CT scan on the day of the procedure. If the lesion decreased in size or resolved, leading to the cancellation of the procedure, the patient was then included in the case series. If the procedure was cancelled due to any other reason, the patient was not included. The study was approved by the Institutional Review Board at the Johns Hopkins Hospital (NA_00084376).
Patients included in the study had demographic information collected, including age, sex, smoking history, prior medical history, and prior malignancies. The dates of the scans were recorded, and images of their lesions from the initial diagnostic CT scan, as well as the day-of-procedure scan, were obtained for comparison. A number needed to screen analysis was performed using a theoretical comparison group, where no same-day imaging was performed and 100% of patients underwent their scheduled procedure.
Results
During the 18-month study period, 116 patients were scheduled for ENB bronchoscopy at the Johns Hopkins Hospital for the diagnosis of a pulmonary nodule or mass. Of the 116 patients scheduled during the study period, 8 patients (6.9%) had a decrease in the size of their lesion, leading to the cancellation of the scheduled procedure. Compared with a theoretical group, where 100% of patients received their bronchoscopy, the cohort in this series, where 93.4% of patients underwent the procedure, an absolute risk reduction of 6.9% was calculated, with a number needed to screen of 15.
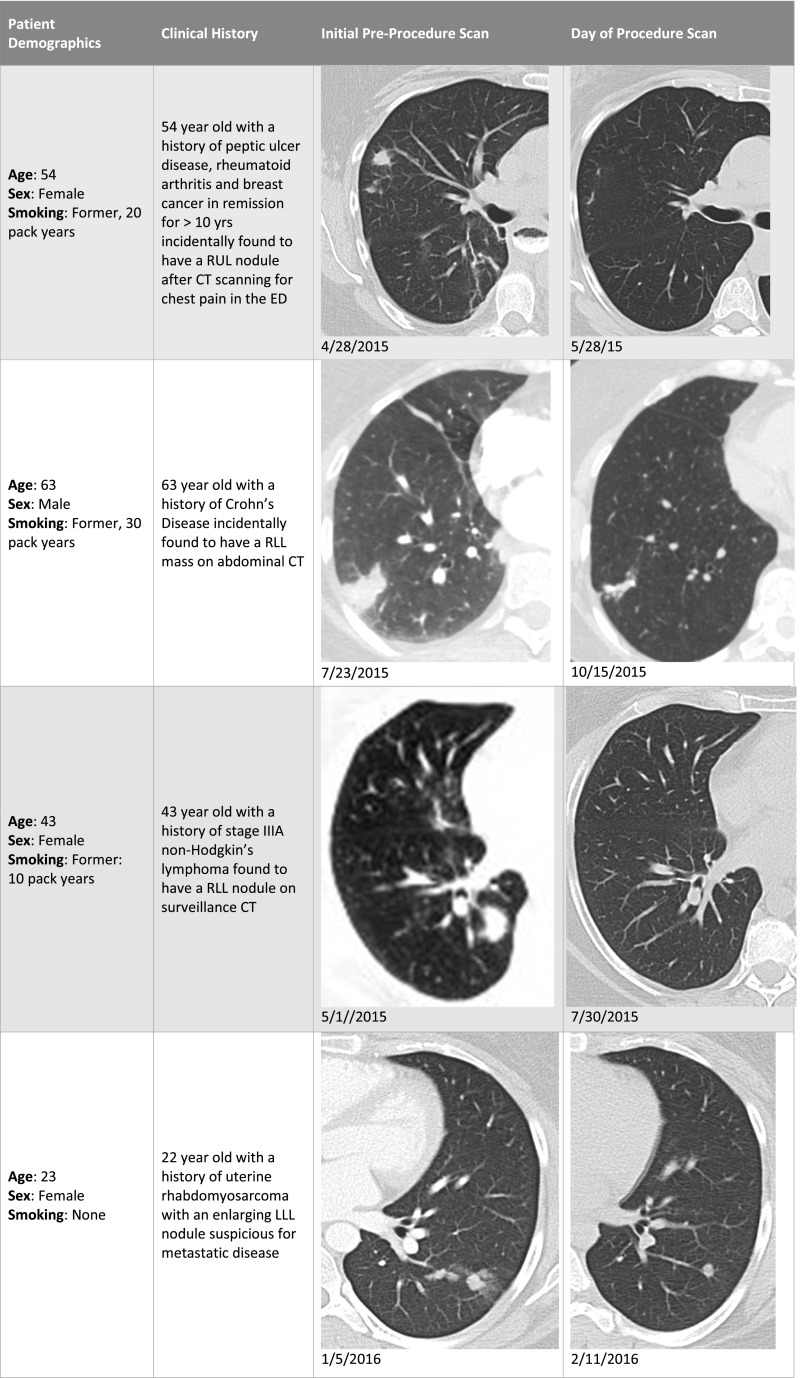
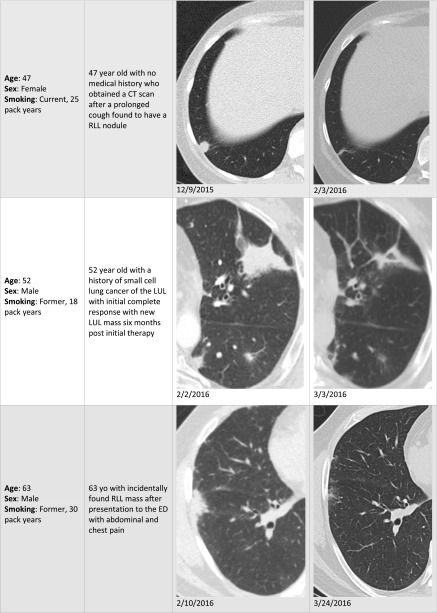
There were four females and four males with an average age of 49.6 years. The average time from initial CT prompting referral for bronchoscopy to the day of procedure scan for those cancelled was 53 days. The average time from initial CT prompting referral for bronchoscopy to the day of procedure scan for those who underwent a bronchoscopy was 50 days. The patient demographics, medical history, and imaging for seven of the patients who had their cases cancelled due to a decrease in the size of their lesion are summarized in Figure 3.
Figure 3.
Demographics, clinical summary, and imaging for cancelled bronchoscopic cases. Definition of abbreviations: CT = computed tomography; ED = emergency department; LLL = left lower lobe; LUL = left upper lobe; RUL = right upper lobe; RLL = right lower lobe.
Of note, two other cases were cancelled during this time period due to reasons unrelated to findings from a same-day CT scan. One patient presented to the endoscopy suite with hypotension and was subsequently found to have a hemodynamically significant pericardial effusion on bedside point-of-care ultrasound. The patient was admitted and taken for pericardiocentesis, with cytopathology revealing a malignant effusion. The second patient’s case was cancelled and rescheduled due to logistics with transportation after anesthesia. As neither patient underwent a day-of-procedure CT, with their cases being cancelled due to circumstances unrelated to findings on a CT scan, they were not included in the analysis.
Discussion
With the introduction of ENB, there has been an increase in the use of bronchoscopy for the diagnosis of pulmonary nodules (8). ENB technologies require a CT scan of the chest completed before the procedure to construct a virtual airway and route to the lesion. The time gap between initial CT imaging and a diagnostic procedure for pulmonary lesions has not been studied. A prior study showed a 7.7% nodule resolution rate in patients undergoing screening (11), but there has been no published literature to date specifically investigating the impact of interval CT imaging during procedural planning. In our experience, this time can vary significantly, sometimes spanning several months. The reasons for this delay are likely multifactorial, including referral times to a specialist, scheduling of the procedure, as well as patient compliance and availability.
The eight patients included in this case series went almost 2 months (53 d) on average between their initial CT scan and the day of their diagnostic procedure. There was no significant difference between the group that underwent a bronchoscopy (50 d) and those cancelled (53 d). As the time from the CT scan to the actual procedure date may vary, it is reasonable to consider that these lesions may decrease in size enough to warrant a change in management.
The possibility of discovering a percentage of shrinking lesions allowing cancellation of a biopsy must be weighed with the need for repeat CT imaging, radiation exposure, cost, and patient convenience. Besides cancellation of biopsies due to resolution/improvement, same-day CT imaging may also reveal a small percentage of patients with disease progression warranting a different and more appropriate biopsy to appropriately stage their disease. Examples of this include discovery of a new pleural effusion or hepatic lesion on a same-day CT, which would likely change the diagnostic plan from a bronchoscopy to a thoracentesis or liver biopsy, respectively, to diagnose and stage simultaneously.
The Veran ENB system recommends use of a chest CT obtained the morning of bronchoscopy to optimize virtual planning and nodule targeting by compensating for nodule movement, as discussed previously here. This approach allowed us to investigate the number of patients needed to screen to prevent one unnecessary procedure without unwarranted CT exposure to patients. Our case series shows a procedural cancellation rate of 6.9%, with a number needed to screen of 15 patients.
The most obvious risk associated with repeat CT imaging is the increased radiation exposure to the patient. An average low-dose screening CT scan of the chest exposes a patient to 1.5 mSv of radiation, whereas a high-resolution noncontrast CT of the chest exposes the patient to 10 mSv (12). Patients in our study who received inspiratory and expiratory CT scans, which require an extra series and average a higher dose, had a mean exposure of 9.485 mSv. These doses are not negligible, but one-time doses at this range are generally considered to be low risk for contributing to the future development of a malignancy. However, patients receiving serial imaging with a higher cumulative dose of radiation are at a higher life-long risk of developing radiation exposure–related malignancies (13, 14). These cumulative risks may currently be underestimated, as the rate of CT scans in the United States has tripled since the 1990s, and the estimated rate of medical radiation–related malignancy is predicted to rise due to this increase in CT use (3). However, one point to consider is that most of the published data described here is in children with longer life expectancies, who will then have a higher life-long cumulative risk of medical radiation–induced malignancy. The population in our study was generally older, with a shorter life expectancy, possibly negating the higher life-long imaging-related cancer risk.
Other drawbacks of obtaining same-day CT imaging include increased healthcare expense, as a noncontrast CT scan of the chest costs approximately $300 (15). However, this slight increase in cost may be negligible if the repeat CT scan leads to cancelation of an unnecessary procedure with its associated risks, including procedural and anesthetic complications. An additional benefit is the potential for improved cost effectiveness, but this is beyond the scope of this case series.
This case series highlights an important point for patients having invasive diagnostic testing after findings from an imaging study. If there is a significant delay from the initial imaging, practitioners should consider repeat studies before proceeding with the scheduled procedure. The optimal time that should be allowed to pass is difficult to ascertain, and is a limitation of this small case series. However, future, larger studies may be able to answer this interesting question, allowing physicians to determine when repeat imaging to provide optimal diagnostic precision is necessary, taking into account the effects of increased radiation exposure.
Conclusions
We report the first case series of resolving pulmonary lesions seen on chest CT exams obtained on the day of the procedure resulting in cancellation of the scheduled bronchoscopy. Overall, the decision to obtain same-day imaging should be an individualized process based on the biopsy technique used, patient risk factors, life expectancy, characteristics of the lesion, and duration of time that has passed since initial imaging. Larger studies are needed before further recommendations on timing of CT scans before procedural interventions can be made.
Footnotes
Author Contributions: R.W.S.—study design, data collection, drafting of the manuscript; H.J.L.—study design, data collection, editing of the manuscript; D.F.-K. and S.A.A.—study design, editing of manuscript; A.D.L.—data collection, editing of manuscript; C.M.M. and J.T.—drafting and editing of manuscript; L.B.Y.—study design, drafting and editing of the manuscript.
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Aberle DR, Adams AM, Berg CD, Black WC, Clapp JD, Fagerstrom RM, Gareen IF, Gatsonis C, Marcus PM, Sicks JD National Lung Screening Trial Research Team. Reduced lung-cancer mortality with low-dose computed tomographic screening. 2011;365:395–409. doi: 10.1056/NEJMoa1102873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Moyer VA U.S. Preventive Services Task Force. Screening for lung cancer: U.S. Preventive Services Task Force recommendation statement. 2014;160:330–338. doi: 10.7326/M13-2771. [DOI] [PubMed] [Google Scholar]
- 3.Berrington de González A, Mahesh M, Kim KP, Bhargavan M, Lewis R, Mettler F, Land C. Projected cancer risks from computed tomographic scans performed in the United States in 2007. 2009;169:2071–2077. doi: 10.1001/archinternmed.2009.440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Diederich S, Hansen J, Wormanns D. Resolving small pulmonary nodules: CT features. 2005;15:2064–2069. doi: 10.1007/s00330-005-2836-4. [DOI] [PubMed] [Google Scholar]
- 5.Felix L, Serra-Tosio G, Lantuejoul S, Timsit JF, Moro-Sibilot D, Brambilla C, Ferretti GR. CT characteristics of resolving ground-glass opacities in a lung cancer screening programme. 2011;77:410–416. doi: 10.1016/j.ejrad.2009.09.008. [DOI] [PubMed] [Google Scholar]
- 6.Silva M, Sverzellati N, Manna C, Negrini G, Marchiano A, Zompatori M, Rossi C, Pastorino U. Long-term surveillance of ground-glass nodules: evidence from the MILD trial. 2012;7:1541–1546. doi: 10.1097/JTO.0b013e3182641bba. [DOI] [PubMed] [Google Scholar]
- 7.Rivera MP, Mehta AC, Wahidi MM. Establishing the diagnosis of lung cancer: diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. 2013;143(5 suppl):e142S–e165S. doi: 10.1378/chest.12-2353. [DOI] [PubMed] [Google Scholar]
- 8.Arias S, Yarmus L, Argento AC. Navigational transbronchial needle aspiration, percutaneous needle aspiration and its future. 2015;7:S317–S328. doi: 10.3978/j.issn.2072-1439.2015.11.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yarmus LB, Arias S, Feller-Kopman D, Semaan R, Wang KP, Frimpong B, Oakjones Burgess K, Thompson R, Chen A, Ortiz R, et al. Electromagnetic navigation transthoracic needle aspiration for the diagnosis of pulmonary nodules: a safety and feasibility pilot study. 2016;8:186–194. doi: 10.3978/j.issn.2072-1439.2016.01.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen A, Pastis N, Furukawa B, Silvestri GA. The effect of respiratory motion on pulmonary nodule location during electromagnetic navigation bronchoscopy. 2015;147:1275–1281. doi: 10.1378/chest.14-1425. [DOI] [PubMed] [Google Scholar]
- 11.Zhao YR, Heuvelmans MA, Dorrius MD, van Ooijen PM, Wang Y, de Bock GH, Oudkerk M, Vliegenthart R. Features of resolving and nonresolving indeterminate pulmonary nodules at follow-up CT: the NELSON study. 2014;270:872–879. doi: 10.1148/radiol.13130332. [DOI] [PubMed] [Google Scholar]
- 12.Smith-Bindman R, Lipson J, Marcus R, Kim KP, Mahesh M, Gould R, Berrington de González A, Miglioretti DL. Radiation dose associated with common computed tomography examinations and the associated lifetime attributable risk of cancer. 2009;169:2078–2086. doi: 10.1001/archinternmed.2009.427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ron E. Cancer risks from medical radiation. 2003;85:47–59. doi: 10.1097/00004032-200307000-00011. [DOI] [PubMed] [Google Scholar]
- 14.Linet MS, Kim KP, Rajaraman P. Children’s exposure to diagnostic medical radiation and cancer risk: epidemiologic and dosimetric considerations. 2009;39:S4–S26. doi: 10.1007/s00247-008-1026-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Black WC, Gareen IF, Soneji SS, Sicks JD, Keeler EB, Aberle DR, Naeim A, Church TR, Silvestri GA, Gorelick J, et al. National Lung Screening Trial Research Team. Cost-effectiveness of CT screening in the National Lung Screening Trial. 2014;371:1793–1802. doi: 10.1056/NEJMoa1312547. [DOI] [PMC free article] [PubMed] [Google Scholar]