Recently, primary prevention with statins was liberalized in the USA and UK but restricted in many comparable European countries. Supported by risk-benefit and cost-effectiveness analyses, the 2013 ACC/AHA (American College of Cardiology/American Heart Association)1 and 2014 UK-NICE (National Institute for Health and Care Excellence)2 risk assessment and prevention guidelines lowered the risk threshold above which primary prevention with statins should be considered. In contrast, the 2016 update of the European guidelines on cardiovascular disease prevention in clinical practice,3 issued jointly by the European Society of Cardiology (ESC) and nine other societies, continued a conservative position on statin use in primary prevention by preserving the high-risk decision threshold introduced in 2003: 5% 10-year risk for fatal atherosclerotic cardiovascular disease (ASCVD) estimated by SCORE (Systematic Coronary Risk Evaluation).4
Unfounded high-risk threshold preserved since 1994
The 5% high-risk threshold introduced by the SCORE-based 2003 ESC prevention guidelines4 was chosen because 5% 10-year risk for fatal ASCVD was considered to equate with 20% 10-year risk for fatal and non-fatal coronary heart disease (CHD) arbitrarily defined as high-risk under previous ESC guidelines. No rationale was provided for choosing ≥20% 10-year CHD risk as high risk when introduced in 1994,5 neither for preserving it as ≥5% 10-year risk for fatal ASCVD.4
Hence, except for UK and possibly a few other European countries, the most important threshold for initiating primary prevention with statins has not been revised in Europe for more than 20 years, during which time long-awaited generic and inexpensive statins became available, and their efficacy and safety convincingly documented. Considering that the prevalence and treatment costs of ASCVD remain high, such a development would normally favour a more widespread use of statins in primary prevention. However, because SCORE depends solely on the ultimate cause of death, in countries with declining ASCVD mortality it is becoming harder and harder to qualify for SCORE-based statin therapy, even though this treatment is contributing to the lower mortality. This and other limitations of SCORE are discussed in this view-point.
SCORE derived from old cohorts
The SCORE model, introduced by the 2003 ESC guidelines, was developed retrospectively from data originating from 12 European cohorts undergoing baseline examination in 1967–1991.6 Only traditional risk factors were generally available and uniformly defined to allow inclusion in the SCORE model. For this reason, diabetes could not be included as predictor, and patients with known diabetes were not excluded from the pooled derivation cohort.6 Only subjects with a previous history of heart attack were excluded. The predicted outcome was fatal ASCVD defined by a wide range of atherosclerosis-related ICD-9 codes.
The predictors included in SCORE (age, sex, smoking, systolic blood pressure, and total cholesterol), the applicable age range (40–65 years), and the predicted outcome (fatal ASCVD) were chosen by necessity, limited by data available from these decades-old cohorts.4,6,7 Non-fatal endpoints were not generally available and not uniformly defined to allow inclusion in the predicted outcome, and reliable risk estimates could not be provided for people older than 65. Hence, in contrast to most other cardiovascular risk models,1,2,7 it was decided to disregard all non-fatal events and only focus on the prediction of fatal ASCVD in people 40–65 years of age. Further, focusing only on fatal events was considered necessary to facilitate the development and update of country-specific recalibrated versions of SCORE based on routinely collected national mortality information.4,6,7 However, the reliability of such information obtained directly from death certificates may be questioned.8 Further, the proposed recalibration approach assumes that it is possible to extrapolate from cross-sectional 1-year (annual) ASCVD mortality rates in the total population to the future 10-year risk for fatal ASCVD in the healthy sub-population.4,6,7,9 This assumption remains unsubstantiated as discussed below.
The SCORE prevention paradox
The purpose of primary prevention is to prevent the development of symptomatic disease. Thereafter, secondary prevention takes over. Therefore, to make sense, a risk score created for use in primary prevention of ASCVD should focus on the prevention of a first ASCVD event. SCORE is focusing on the last event rather than the first event, and only events leading to death count.
SCORE differs in two important ways from other common ASCVD risk models, including the 2013 ACC/AHA Pooled Cohort Equations (PCE)1 and the 2014 UK-NICE QRISK2.2 First, SCORE predicts the risk of dying from ASCVD (mortality), disregarding non-fatal events (morbidity). Second, SCORE does not predict the natural history of ASCVD but the end result after using all available means to keep patients with ASCVD alive. Today, because of effective secondary prevention, the great majority of those who develop ASCVD survive with chronic ASCVD without dying from it, and such cases do not count as SCORE events worth preventing. It is indeed a paradox for a risk score intended for primary prevention that it depends simply and solely on the risk of dying from the disease in question. More specifically, the more statins reduce the risk of dying from ASCVD in patients with diabetes or known ASCVD (secondary prevention), the harder it becomes to qualify for SCORE-based statin therapy to prevent a first ASCVD event (primary prevention). Recent data indicate that the mortality from ASCVD is now so low in many European countries that SCORE-based statin therapy soon might be history in these countries despite high ASCVD morbidity and treatment costs.10
SCORE not applicable beyond age 65
The burden of ASCVD increases with age, including higher incidence, case-fatality, longer-term mortality, and prevalence. In a contemporary European population of apparently healthy people, only 18% (62/339) of all fatal ASCVD events occurred in the target population for SCORE-based risk assessment (age 40–65 years).10 Thus, the restricted age range in which SCORE is applicable and risk charts are available constitute a major limitation of SCORE. Somewhat misleading, it is possible to enter age up to 100 years in the online risk calculator, HeartScore (www.heartscore.org), but the age-dependent risk is truncated at age 65, leading to systematic underestimation of risk beyond this age if the SCORE function is well-calibrated to the target population.
The ESC guidelines on cardiovascular disease prevention provide only limited guidance on primary prevention with statins in people who just because of aging (>65 years) is no longer eligible for SCORE-based risk assessment.
Two standard versions of SCORE
When treatment decisions are based on absolute risk, the risk equations used to estimate risk need to be well calibrated to the target population. Because background risk for fatal ASCVD differs across Europe, the 2003 ESC guidelines4 provided two standard versions of SCORE that are still used for risk assessment3: one intended for countries with low cardiovascular mortality (low-risk SCORE version), the other intended for countries with high cardiovascular mortality (high-risk SCORE version). Because of declining ASCVD mortality, many more European countries are now classified as low-risk countries (n = 24) than in 2003 (n = 8), and even the low-risk SCORE version overestimates 10-year risk for fatal ASCVD in several of these countries today (see Supplementary material online). The 2016 ESC guidelines3 arbitrarily defined low-risk countries as those with 2012 cardiovascular mortality rates <225 in men and <175 in women per 100 000, age-adjusted to the WHO World Standard Population (Figure 1).11 The rationale for the chosen cut-points was not provided, neither for using this unusual age adjustment for a risk score intended for Europeans 40–65 years of age.
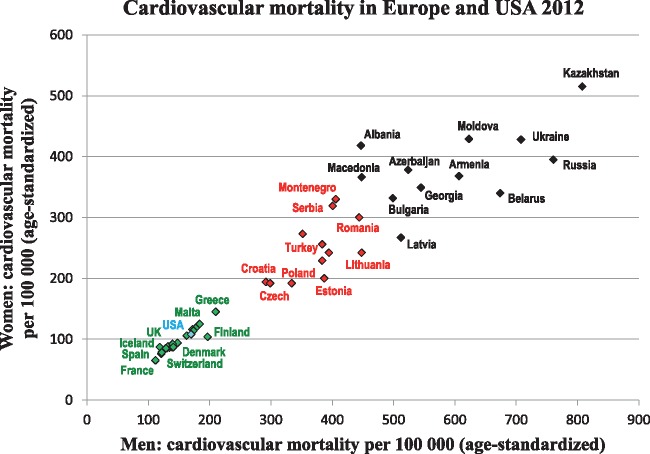
Figure 1.
Cardiovascular mortality in men and women. The ESC guidelines3 arbitrarily classify countries in low-risk, high-risk, and very-high-risk based on national cardiovascular mortality rates age-adjusted to the WHO World Standard Population.11 For clarity, only some countries are named on the figure (all countries, see Supplementary material online). Green indicates low-risk, red high-risk, and black very-high-risk countries.
The European country with the lowest age-adjusted cardiovascular mortality is France (86 per 100 000), the highest is Kazakhstan (636 per 100 000).11 Considering the most prevalent form of ASCVD, the cross European difference is even more striking: CHD mortality is >15 times higher in Ukraine than France (337 vs. 21 per 100 000).12 Thus, it seems to be an understatement that ‘Very-high-risk countries present levels of risk that are more than double that of low-risk countries’.3 Obviously, with only two standard versions of SCORE available for general use, most European countries are inevitably using a miscalibrated SCORE model unless a country-specific recalibrated version of SCORE is available. Thus, how to recalibrate SCORE to the target population is critically important.
Recalibration of SCORE based on cross-sectional data
Natural history studies in contemporary cohorts with appropriate follow-up for clinical events are the gold standard for the development, updating and recalibration of risk scores intended for primary prevention of ASCVD.13 Realizing that such cohort studies are not available in many European countries, the 2003 ESC guidelines introduced an alternative cohort-independent recalibration approach relying solely on cross-sectional risk factors and mortality information without follow-up.4,6,7,9 Since then, SCORE has been recalibrated in many countries across Europe based on national cause-specific mortality rates from a single year (see Supplementary material online). However, since the national ASCVD mortality rate includes everyone, also high-risk patients who do not qualify for SCORE-based risk assessment (patients with known ASCVD, diabetes, familial hypercholesterolemia, kidney disease or statin use), this unusual recalibration approach most likely leads to overestimation of risk in the healthy subpopulation where SCORE is going to be used, as exemplified below using data from Denmark.
The Danish experience
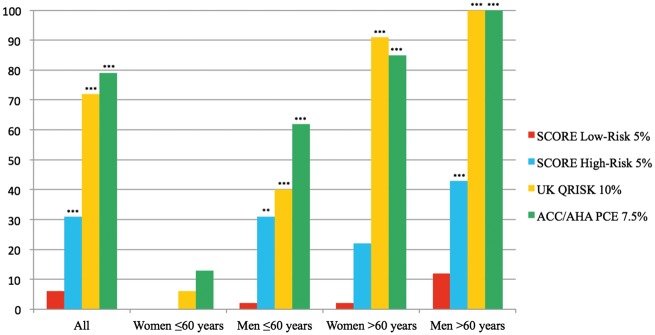
In 2003, Denmark, Norway, and Finland were arbitrarily chosen to represent European high-risk countries, and the high-risk version of SCORE was developed from cohorts in these countries.6 However, already 1 year later, a recalibrated version of SCORE was recommended in Denmark because the high-risk SCORE version was found to overestimate risk.14 Less than 10 years later, because of still declining cardiovascular mortality, Denmark was declared a low-risk country and recommended to use the low-risk SCORE version instead of the high-risk SCORE version,15 which is the standard way to improve the calibration of SCORE to the target population. Evaluated in consecutive real-world patients with a first myocardial infarction (MI),16 eligibility for SCORE-based statin therapy before MI (detection rate) dropped from 30% to 6% just by using the better calibrated low-risk SCORE version—far below detection rates seen with the 2013 ACC/AHA and 2014 UK-NICE guidelines (Figure 2).
Figure 2.
Proportion (%) of patients with first myocardial infarction who would have qualified for risk-based statin therapy before the event. The guideline-recommended risk thresholds for primary prevention with statins are shown next to the bar diagram. QRISK is recommended by 2014 UK-NICE2, PCE (pooled cohort equations) by 2013 ACC/AHA1. Adapted from Mortensen et al.16 Data were compared by Kruskal–Wallis one-way ANOVA with Dunn’s post-hoc test for multiple comparisons (SCORE low-risk as control group). *** indicates P < 0.0001 and ** indicates P < 0.01.
More recently, an updated country-specific version of SCORE was provided,17 developed using the guideline-recommended cross-sectional recalibration approach, which confirmed that Denmark is a low-risk country as defined by the ESC guidelines. However, when tested prospectively in a contemporary, population-based cohort of healthy Danes 40–65 years of age (target population for SCORE-based risk assessment), the low-risk SCORE version overestimated risk for fatal ASCVD substantially (∼5 times).10 Even worse, using a well-calibrated SCORE-like risk function, none of those who died of ASCVD during follow-up qualified for SCORE-based statin therapy.10 These surprising results indicate that (1) the guideline-recommended cross-sectional recalibration approach is unreliable, and (2) primary prevention with statins will soon be history in many so-called ‘low-risk’ European countries if SCORE is recalibrated according to the gold standard (prospective and contemporary cohort study with follow-up). This development is thought-provoking, considering that the prevalence of ASCVD remains high and even tends to be increasing,18 and is in stark contrast to the expanded indication for primary prevention with statins in the recent American and British guidelines.1,2
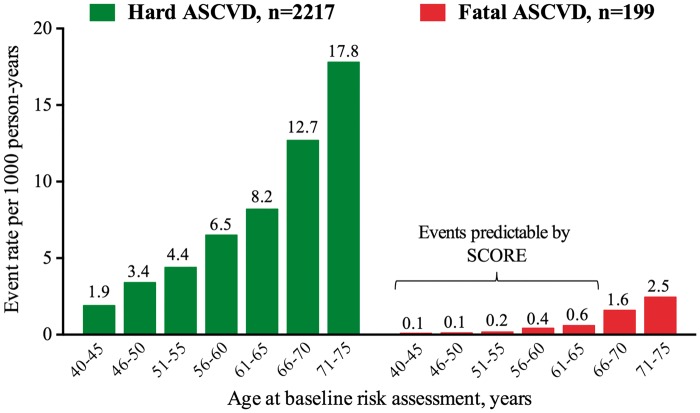
These observations in a large contemporary cohort of healthy people revealed another limitation of the mortality-based SCORE model: there were too few fatal ASCVD events during follow-up to allow for reliable sex-specific recalibration of SCORE in the target population. Among 30.824 apparently healthy Danes aged 40–65 years at baseline risk assessment, only 62 of 767 (8%) ASCVD events observed during 6.8 years of follow-up were fatal.10 More recently, similar results were obtained in an expanded study population (Figure 3).19 Obviously, getting enough fatal events will not pose a problem in the cross-sectional recalibration approach relying on national mortality data.
Figure 3.
ASCVD events predictable by SCORE. In a large contemporary European cohort of apparently healthy individuals aged 40–75 years at baseline examination (Copenhagen General Population Study, n = 44 889), fatal ASCVD as defined by SCORE constituted only 9% of the hard ASCVD events (fatal coronary heart disease and stroke plus non-fatal myocardial infarction and stroke) observed over ≥5 years of follow-up. Relatively few of the fatal ASCVD events occurred in the target population for SCORE-based risk assessment (age 40–65 years). In the overall population, only 18% of all fatal ASCVD events occurred among those aged 40–65 years at baseline10. This is too few fatal events to allow for reliable sex-specific recalibration of SCORE in the target population. Adapted from Mortensen et al.19 ASCVD = atherosclerotic cardiovascular disease.
Conclusion
Inherent limitations of the mortality-based SCORE model are discussed, including the SCORE prevention paradox (if a drug can keep patients alive, there is no need to use it in primary prevention), restricted age range (not applicable beyond 65 years), unreliable cross-sectional recalibration approach, and too few fatal events to allow for reliable sex-specific recalibration of SCORE in the intended target population. It may indeed be questioned whether it is possible to update the SCORE model to meet current needs in primary ASCVD prevention. With the conservative position taken by the 2016 ESC guidelines, SCORE-based statin therapy is soon going to be phased out in European countries with low and/or declining ASCVD mortality despite high morbidity and treatment costs.
New approaches are needed to guide primary prevention with statins that do not rely solely on traditional natural history studies, taking the burden of both fatal and non-fatal ASCVD into account, and providing guidance on statin therapy also in the elderly population. Risk-based treatment thresholds should be supported by transparent risk-benefit and cost-effectiveness analyses.
Supplementary material
Supplementary material is available at European Heart Journal online.
Conflict of interest: none declared.
Supplementary Material
References
- 1. Stone NJ, Robinson JG, Lichtenstein AH, Bairey Merz CN, Blum CB, Eckel RH, Goldberg AC, Gordon D, Levy D, Lloyd-Jones DM, McBride P, Schwartz JS, Shero ST, Smith SC, Watson K, Wilson PWF.. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults. J Am Coll Cardiol 2014;63:2889–1934. [DOI] [PubMed] [Google Scholar]
- 2.National Institute for Health and Care Excellence (NICE) Clinical Guideline CG181: Lipid modification—Cardiovascular risk assessment and the modification of blood lipids for the primary and secondary prevention of cardiovascular disease. National Clinical Guideline Centre, July 2014. http://www.nice.org.uk/Guidance/cg181 (12 November 2016). [PubMed]
- 3. Piepoli MF, Hoes AW, Agewall S, Albus C, Brotons C, Catapano AL, Cooney MT, Corrà U, Cosyns B, Deaton C, Graham I, Hall MS, Hobbs FD, Løchen ML, Löllgen H, Marques-Vidal P, Perk J, Prescott E, Redon J, Richter DJ, Sattar N, Smulders Y, Tiberi M, van der Worp HB, van Dis I, Verschuren WM.. 2016 European Guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J 2016;37:2315–2381.27222591 [Google Scholar]
- 4. De Backer G, Ambrosioni E, Borch-Johnsen K, Brotons C, Cifkova R, Dallongeville J, Ebrahim S, Faergeman O, Graham I, Mancia G, Manger Cats V, Orth-Gomér K, Perk J, Pyörälä K, Rodicio JL, Sans S, Sansoy V, Sechtem U, Silber S, Thomsen T, Wood D.. European guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J 2003;24:1601–1610. [DOI] [PubMed] [Google Scholar]
- 5. Pyörälä K, De Backer G, Graham I, Poole-Wilson P, Wood D.. Prevention of coronary heart disease in clinical practice: recommendations of the Task Force of the European Society of Cardiology, European Atherosclerosis Society and European Society of Hypertension. Eur Heart J 1994;15:1300–1331. [DOI] [PubMed] [Google Scholar]
- 6. Conroy RM, Pyörälä K, Fitzgerald AP, Sans S, Menotti A, De Backer G, De Bacquer D, Ducimetière P, Jousilahti P, Keil U, Njølstad I, Oganov RG, Thomsen T, Tunstall-Pedoe H, Tverdal A, Wedel H, Whincup P, Wilhelmsen L, Graham IM.. Estimation of ten-year risk of fatal cardiovascular disease in Europe: the SCORE project. Eur Heart J 2003;24:987–1003. [DOI] [PubMed] [Google Scholar]
- 7. Cooney MT, Dudina AL, Graham IM.. Value and limitations of existing scores for the assessment of cardiovascular risk: a review for clinicians. J Am Coll Cardiol 2009;54:1209–1227. [DOI] [PubMed] [Google Scholar]
- 8. Lloyd-Jones DM, Martin DO, Larson MG, Levy D.. Accuracy of death certificates for coding coronary heart disease as the cause of death. Ann Intern Med 1998;129:1020–1026. [DOI] [PubMed] [Google Scholar]
- 9. De Bacquer D, De Backer G.. Predictive ability of the SCORE Belgium risk chart for cardiovascular mortality. Int J Cardiol 2010;143:385–390. [DOI] [PubMed] [Google Scholar]
- 10. Mortensen MB, Afzal S, Nordestgaard BG, Falk E.. The high-density lipoprotein-adjusted SCORE model worsens SCORE-based risk classification in a contemporary population of 30,824 Europeans: the Copenhagen General Population Study. Eur Heart J 2015;36:2446–2453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. World Health Organisation. WHO Global Health Repository. Cardiovascular diseases, deaths per 100 000. Data by country. http://apps.who.int/gho/data/node.main.A865CARDIOVASCULAR?lang=en (24 October 2016).
- 12. World Health Organization Mortality Database. http://www.who.int/healthinfo/mortality_data/en/ (24 October 2016).
- 13. D'Agostino RB Sr, Grundy S, Sullivan LM, Wilson P.. CHD Risk Prediction Group. Validation of the Framingham coronary heart disease prediction scores: results of a multiple ethnic groups investigation. JAMA 2001;286:180–187. [DOI] [PubMed] [Google Scholar]
- 14. Thomsen T, Christensen B, Hildebrandt P, Iversen HK, Larsen ML, Sillesen H, Snorgaard O, Videbæk L, Clinical guidelines on cardiovascular disease prevention in Denmark. Danish. Danish Society of Cardiology 2004. file:///C:/Users/efal/Downloads/klinise%20retningslinier%20for%20cvp%202004.pdf (12 November 2016).
- 15. Perk J, De Backer G, Gohlke H, Graham I, Reiner Z, Verschuren M, Albus C, Benlian P, Boysen G, Cifkova R, Deaton C, Ebrahim S, Fisher M, Germano G, Hobbs R, Hoes A, Karadeniz S, Mezzani A, Prescott E, Ryden L, Scherer M, Syvänne M, Scholte Op Reimer WJM, Vrints C, Wood D, Zamorano JL, Zannad F.. European Guidelines on cardiovascular disease prevention in clinical practice (version 2012). Eur Heart J 2012;33:1635–1701. [DOI] [PubMed] [Google Scholar]
- 16. Mortensen MB, Falk E.. Real-life evaluation of European and American high-risk strategies for primary prevention of cardiovascular disease in patients with first myocardial infarction. BMJ Open 2014;4:e005991.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.2015 National Treatment Guidelines on Heart Disease Prevention. Danish Society of Cardiology 2015. Danish. Updated version available at: http://nbv.cardio.dk/forebyggelse (12 November 2016).
- 18. Koch MB, Davidsen M, Andersen LV, Juel K, Jensen GB.. Increasing prevalence despite decreasing incidence of ischaemic heart disease and myocardial infarction. A national register based perspective in Denmark, 1980-2009. Eur J Prev Cardiol 2015;22:189–195. [DOI] [PubMed] [Google Scholar]
- 19. Mortensen MB, Nordestgaard BG, Afzal S, Falk E.. ACC/AHA guidelines superior to ESC/EAS guidelines for primary prevention with statins in non-diabetic Europeans: the Copenhagen General Population Study. Eur Heart J 2017;38:586–594. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.