Abstract
Purpose of the Study
This study investigated the mechanisms of change underlying an activity-based lifestyle intervention, an occupational therapy program aimed at promoting healthy habits, and routines in older adults. We examined two activity-relevant factors as potential mediators linking the intervention to reduced symptoms of depression: activity frequency and global perceptions of activity significance. Social connections and perceived control were assessed to understand how activity-related factors relate to reduced symptoms of depression.
Design and Methods
The sample consisted of 460 multiethnic community-dwelling older adults aged 60–95 years. Participants were randomly assigned to a 6-month lifestyle redesign intervention (n = 232) or a no-treatment control (n = 228) condition. After the 6-month period, 360 individuals completed post-testing. Latent change score models were used to represent changes from baseline over the experimental interval. Structural equation models were applied to examine the indirect effects of the intervention on reduced depressive symptoms.
Results
The results demonstrated significant indirect effects from intervention receipt to decreased depressive symptoms via increased activity frequency and activity significance. Higher activity frequency was linked to fewer depressive symptoms via heightened social connections, whereas increased activity significance was associated with fewer depressive symptoms via enhanced perceived control.
Implications
The results support basic principles of occupational therapy by highlighting important mediating roles of activity frequency and activity significance in reducing depressive symptoms. Understanding of these change mechanisms can help optimize activity-centered interventions to reduce depressive symptoms.
Keywords: Depression, Intervention, Occupational therapy and/or physical therapy, Frequency and significance of activities, Social connections, Perceived control
Activity-based lifestyle interventions for older adults aim to improve well-being by promoting healthy activity engagement in daily life. These interventions oftentimes include individually tailored supports provided by health care professionals to increase older adults’ ability and motivation to participate in activity. Lifestyle Redesign is one example of an evidence-based, activity-centric intervention that is led by occupational therapists and suitable for community-dwelling elders (Clark et al., 2015; Jackson, Carlson, Mandel, Zemke, & Clark, 1998). In Lifestyle Redesign, therapists review participants’ personal strengths and weaknesses and environmental affordances (e.g., financial status and neighborhood safety); a review which subsequently informs the creation of a customized, feasible, and sustainable activity plan to be carried out in everyday life. Attempts are made to reduce barriers and increase facilitators to successful activity performance. Lifestyle Redesign has been found to improve well-being, including decreased depressive symptoms, with smaller effects in the more distal domain of physical health (Clark et al., 1997; Clark et al., 2012).
Beyond testing intervention effectiveness, studies investigating mechanisms of therapeutic change are called for. Understanding such mechanisms can help integrate interventions targeting the same outcome, clarify the relationship between treatment and diverse outcomes, help optimize therapeutic change, facilitate dissemination from research to practice, help identify moderators of treatment, and provide a better understanding of human functioning beyond the context of therapy (Kazdin, 2007). Yet, there is a dearth of studies testing the active ingredients in treatments related to clinical rehabilitation (Whyte & Hart, 2003). Therefore, the current study aims to identify factors that contribute to Lifestyle Redesign’s positive outcomes in decreasing depressive symptoms.
Linking Lifestyle-Based Interventions to Better Well-Being: Activity Frequency and Activity Significance
Lifestyle Redesign is grounded in theories from occupational therapy, emphasizing that participation in meaningful activities is a vital part of people’s lives (Law, 2002). “Frequency” of performed activities—being active in a general sense—has been theorized to be an important determinant of positive aging outcomes (Lemon, Bengtson, & Peterson, 1972), an expectation commonly borne out in studies of the correlates of older adults’ well-being (e.g., Chao, 2016; Everard, Lach, Fisher, & Baum, 2000; Glass, Leon, Bassuk, & Berkman, 2006; Hong, Hasche, & Bowland, 2009; Menec, 2003). In addition to activity frequency, positive perceptions of activity “significance” is considered as another active ingredient of Lifestyle Redesign. It is crucial to maintain a positive global perception of activity significance, or perceive activities to be important for personal health and wellness (Mallinson et al., 2014). However, in comparison to activity frequency, perceptions of activity significance have received less attention due to lack of appropriate measurement. Although not directly assessed, prior work highlights the value of engaging in activities that are perceived to be meaningful (Clark et al., 2012; Eakman, 2013; Eakman, 2014; Edgelow & Krupa, 2011; Roland & Chappell, 2015; Wright-St Clair, 2012), suggesting that well-being can be dependent on the significance individuals place on the roles of activities in their daily life.
Psychological Mechanisms of Activity Frequency and Significance: Social Connections and Perceived Control
Despite a large number of studies documenting the benefits of activity participation, it is less clear how increasing activity frequency and promoting activity significance are associated with improved well-being. One qualitative study found that engaging in meaningful activities helped maintain older adults’ social connectedness and enhanced their ability to control their daily routines after financial, physical, and personal changes (Jackson, 1996). This finding highlighted the importance of being connected and feeling a sense of control.
One salient characteristic of activity participation is that it commonly help establish or strengthen “social connections” (Menec, 2003). Many activities are coperformed with friends or family members. This social aspect of activity participation has the capacity to heighten well-being or alleviate depression (Fox, 1999). In fact, promoting activities that involve socializing with others is more beneficial, compared to passive and solitary activities, for reducing depressive symptoms (Riebe, Fan, Unützer, & Vannoy, 2012). Because social relationships mediate the effectiveness of a variety of interventions for older adults (Barrera, Toobert, Angell, Glasgow, & Mackinnon, 2006; Dour et al., 2014; Oh & Ell, 2015), increased connectedness with others may at least partially explain how intervention-based activity changes augment psychological well-being.
Another important dimension of activity participation is its ability to heighten an individual’s sense of “perceived control,” which can be defined as belief that one’s own efforts can bring about personally desired outcomes (Wallston, Wallston, Smith, & Dobbin, 1987). Higher perceived control is associated with better mental health outcomes (Dracup et al., 2003; Moser & Dracup, 1995; Schulz & Decker, 1985; Turk, Okifuji, & Scharff, 1995), and such efficacy beliefs can be enhanced by activity participation over time (Salanova, Llorens, & Schaufeli, 2011). Therefore, heightened sense of control may also partially explain how intervention-based activity changes relate to reduced depressive symptoms.
Mediation Model of Activity-Centered Lifestyle Intervention
In the current study, we applied a latent change score model to test patterns of mediation within a large-scale randomized controlled trial of Lifestyle Redesign, the Well Elderly 2 study. In a prior intention-to-treat (ITT) analysis, this intervention was shown to improve a variety of self-rated outcomes, including depression, a key indicator of well-being. Although Lifestyle Redesign was intended to improve overall well-being and not to treat clinical depression, depressive symptoms were examined as the intervention’s well-being outcome to study mechanisms of change. We hypothesized that the beneficial effects of this intervention on depressive symptoms are mediated by activity frequency and activity significance. We also hypothesized that social connections and perceived control mediate the association between the two activity-related factors and decreased depressive symptoms.
Design and Methods
Participants and Procedures
Details of the sample and study procedures can be found in Clark and colleagues (2012) and Jackson and colleagues (2009). In brief, the sample consisted of a multiethnic group of 460 participants ranging in age from 60 to 95 years. Participants were residents or visitors of senior housing facilities, community centers, or retirement communities in the Los Angeles metropolitan area. Individuals without signs of psychosis and who were able to complete the study assessment battery were included in the study. Participants were recruited in two waves at nine community sites. A block sizes of 4 was used within each wave and site to randomly assign participants to the 6-month Lifestyle Redesign intervention (n = 232) or no-treatment control (n = 228) condition. After 6 months, participants randomized to the control condition received the intervention. The analyses reported here include only data collected during the first 6 months of the study. See Table 1 for demographic information across groups. At baseline, there were no significant differences in demographic characteristics. After the 6-month period, a total of 360 participants completed post-testing, with 187 from the intervention group and 173 from the control group. Drop-out rates did not differ by conditions, and there were no significant differences in sample characteristics between completers and those who dropped out.
Table 1.
Demographic Information at Baseline
| Demographic variables | Intervention (n = 232) | Control (n = 228) | Total (n = 460) |
|---|---|---|---|
| Sex, n (%) | |||
| Male | 70 (30.2%) | 87 (38.2%) | 157 (34.1%) |
| Female | 162 (69.8%) | 141 (61.8%) | 303 (65.9%) |
| Age, M (SD) | 74.8 (7.8) | 74.9 (7.6) | 74.9 (7.7) |
| Race, n (%) | |||
| White | 85 (36.6%) | 87 (38.2%) | 172 (37.4%) |
| Black/African | 78 (33.6%) | 71 (31.1%) | 149 (32.4) |
| American | |||
| Hispanic or Latino | 49 (21.1%) | 43 (18.9%) | 92 (20%) |
| Other | 20 (8.6%) | 25 (11%) | 45 (9.8%) |
| Education, n (%) | |||
| Less than high school | 72 (31%) | 64 (28.1%) | 136 (29.6%) |
| High school | 45 (19.4%) | 44 (19.3%) | 89 (19.3%) |
| Some college | 77 (33.2%) | 81 (35.5%) | 158 (34.3%) |
| 4-year college or more | 38 (16.4%) | 39 (17.1%) | 77 (16.7%) |
| Monthly income, n (%) | |||
| <$1,000 | 123 (53.0%) | 117 (51.3%) | 240 (52.2%) |
| $1,000–$1,999 | 51 (22%) | 56 (24.6%) | 107 (23.3%) |
| >$2,000 | 55 (23.7%) | 47 (20.6%) | 102 (22.1%) |
The Lifestyle Redesign intervention includes didactic presentation, peer exchanges, direct experience, and personal reflection to enable participants to explore activity as it relates to healthy habit formation, routines, and overall wellness. It is a manualized program led by occupational therapists who are trained in the administration of the intervention prior to providing treatment. Weekly small (8–10 participants) group sessions and up to 10 individual sessions were held. On average, individuals in the treatment group participated in 12.11 group sessions (SD = 7.53) and 2.42 individual sessions (SD = 2.49). Modules included Introduction to the Power of Activity; Aging, Health, and Activity; Transportation; Safety; Social Relationships; Cultural Awareness; Finances; and Integrative Summary: Lifestyle Redesign Journal. In addition, participants engaged in monthly community outings as a means of gaining direct experience with the intervention content.
Measures
Participants were assessed at baseline (all measures) and 6 months (all measures except for demographic information) using the following instruments.
Demographic Information
Demographic information was collected on participants’ age, gender, ethnicity, education, and income.
Depression
The Center for Epidemiologic Studies Depression Scale (CESD; Radloff, 1977) was used to assess the frequency with which individuals experienced depressive symptoms during the past week. Participants self-rated 20 items such as depressed mood, somatic symptoms, and feelings of hopelessness on a scale from 0 (rarely/none of the time) to 3 (most/all of the time). A summary score, ranging from 0 to 60, was calculated by summing all items, with higher scores indicating more depressive symptoms. Cronbach’s α in this sample was .90.
Frequency of Activity
A variation of the Meaningful Activity Participation Assessment-Frequency (MAPA-f; Eakman, Carlson, & Clark, 2010) was used to measure how frequently participants engaged in meaningful activities in the past few months. Participants were presented with 29 different activities, such as “socializing with family,” “personal finances,” or “shopping,” and were asked to indicate the amount of time spent on each activity on a scale from 1 (not at all) to 7 (everyday). Higher scores reflected greater levels of activity. The MAPA has sufficient internal consistency and test–retest reliability (Eakman et al., 2010). Cronbach’s α in this sample was .81.
Global Perception of Activity Significance
The Activity Significance and Perception of Engagement assessment (ASPEn; Mallinson et al., 2014) was used to measure individuals’ perception of the extent to which their everyday activities contribute to their health and wellness. Sample items include, “overall, how much do you think your activities contribute to your mental health”? and “overall, are your activities personally fulfilling for you”? Each of 13 items is rated on a scale ranging from 1 (not at all) to 4 (a great deal), and a scoring algorithm is used to calculate an overall score for perceived significance. Cronbach’s α was .91 in a previous study using the same dataset (Mallinson et al., 2014).
Social Connections
The Lubben Social Network Scale (LSNS; Lubben, 1988) was used to assess level of social integration and connections. This 10-item scale included items such as “how many relatives do you see or hear from at least once a month”? and “when you have an important decision to make do you have someone you can talk to about”? Most questions were asked on a 6-point scale, with the anchors differing depending on the question. The total score was used to reflect the level of social connections, with higher scores indicating higher levels of connections. Cronbach’s α in this sample was .73.
Perceived Control
Perceived control was measured using an 8-item instrument found to be unidimensional, reliable, and valid in previous studies (Eizenman, Nesselroade, Featherman, & Rowe, 1997). Examples of items include “I can do just about anything I really set my mind to,” and “Maintaining my level of health depends strongly on my own efforts.” Each item was rated on a 4-point scale from 1 (disagree strongly) to 4 (agree strongly), with higher scores evidencing more perceived control. Cronbach’s α in this sample was .66.
Analyses
Descriptive statistics were calculated using SPSS (version 21). Analysis involving latent change models were completed using Mplus (version 7.31).
Latent Change Score Model
A latent change score model was used to model changes from baseline in variables included in the model (depression, activity frequency, activity significance, social connections, and perceived control). Specifically, the latent change variable (∆X) was defined as the part of the time 2 (i.e., 6-month post-test) variable that is not identical to the time 1 (i.e., baseline) variable (McArdle, 2009). The paths from time 1 variables to time 2 variables and latent change to time 2 variables were fixed at 1, so that latent change scores were similar to the results obtained by subtracting time 1 from time 2 (X[2] = 1*X[1] + 1*∆X). Covariances between time 1 variables and the latent change scores (σ1∆) were estimated. Means of time 1 variables (μ1) and latent change scores (μ∆) were also estimated.
Model Testing
To test model fit and interpret parameter estimates, maximum likelihood estimation with robust standard errors was used to accommodate nonnormal data as well as handle missing data. We assessed model fit by using multiple goodness-of-fit indices, including chi-square fit statistics, Root Mean Square Error of Approximation (RMSEA), Standardized Root Mean Square Residual (SRMR), Comparative Fit Indices (CFI), and Tucker–Lewis Indices (TLI). Chi-square fit statistics tend to be overly conservative, so a significant chi-square statistic was not in itself considered sufficient to reject a given model. Adequate model fit is indicated by RMSEA values up to .08, SMSR values up to .08, or CFI and TLI values above .90 (Wang & Wang, 2012).
Indirect Effects
To assess whether specific indirect effects were significant, the bias-corrected bootstrapping method was employed, allowing for empirical, nonparametric approximations of the sampling distributions of the indirect effects by repeatedly sampling the dataset multiple times (Preacher & Hayes, 2008). Bootstrapping provides empirical standard errors, minimizing the effect of skew and heteroskedasticity. Results were presented based on 1,000 bootstrapping samples. This produced point estimates and 95% confidence intervals (CIs) for the indirect effects. An indirect effect was deemed significant if the 95% CI did not include zero. A pairwise contrast was used to compare the magnitude of specific indirect effects (Preacher & Hayes, 2008).
Results
Descriptive Statistics
Table 2 presents descriptive statistics of baseline and postintervention by treatment group, and effect sizes based on independent samples t-tests. No excessive skewness or kurtosis was found. The covariance matrix is presented in Supplementary Appendix Table A1.
Table 2.
Baseline and Postintervention Descriptive Statistics by Treatment Group
| Variable name | Intervention groupMean (SD) | Control groupMean (SD) | Independent samples t-tests | |||
|---|---|---|---|---|---|---|
| Baseline (n = 232) | Post (n = 187) | Baseline (n = 228) | Post (n = 173) | p | Effect sizes (Cohen’s d) | |
| DEP | 14.32 (10.89) | 12.47 (9.68) | 13.13 (10.91) | 13.53 (11.17) | * | .22 |
| AF | 76.00 (21.64) | 81.58 (21.95) | 77.15 (23.29) | 76.61 (23.37) | *** | .44 |
| AS | 65.86 (13.72) | 68.32 (12.62) | 65.11 (12.76) | 64.26 (13.38) | * | .23 |
| PC | 23.66 (3.43) | 23.88 (3.35) | 23.60 (3.34) | 23.49 (3.09) | NS | |
| SC | 26.14 (8.80) | 26.77 (8.63) | 26.50 (9.78) | 26.45 (9.33) | NS | |
Notes: DEP = depression; AF = activity frequency; AS = perception of activity significance; PC = perceived control; SC = social connections; NS = nonsignificant. Independent samples t-tests were conducted to compare intervention group differences in changes from baseline to follow-up of the aforementioned variables.
*p < .05. **p < .01. ***p < .001.
Model Testing and Indirect Effects
All changes from baseline to follow-up were modeled using the latent change score model. For all models, endogenous variables were regressed on covariates, including age, gender, and ethnicity. Attendance rate was not associated with the outcomes of interest and therefore not included as a covariate.
Intervention Effect on Depression
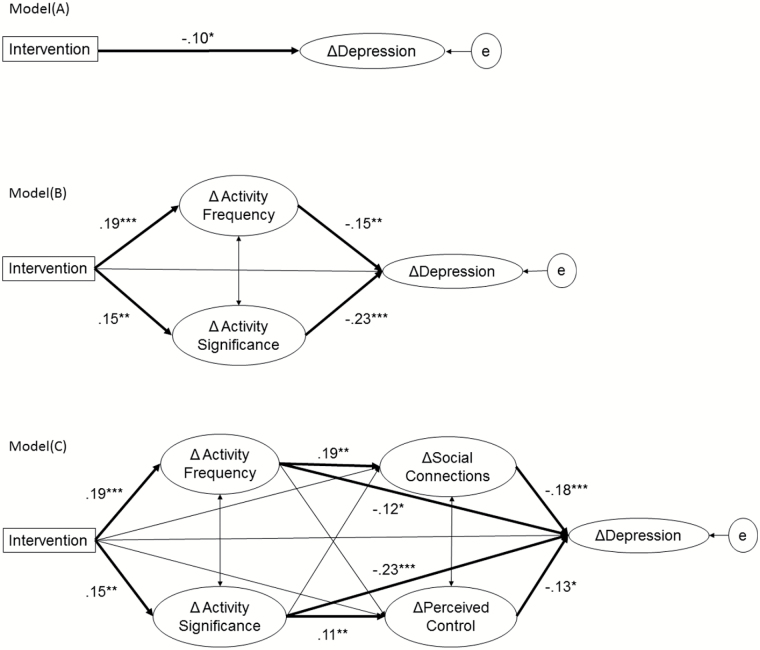
To examine the intervention effect on depression, ∆depression was regressed on intervention group. Model fit was acceptable, χ2 (6) = 18.42, p < .01, CLI = .94, TLI = .93, RMSEA = .07, and SRMR = .04, indicating that receipt of the intervention was associated with a significant decrease in depressive symptoms, compared with the control group (β = −.10, p < .05). See Figure 1 (Model A) for a visual presentation of the model and results.
Figure 1.
Models of mechanisms of change. (A) Model A: intervention effects on change in depressive symptoms, (B) Model B: changes in activity frequency and activity significance as mediators, (C) Model C: psychological mediators of the changes in activity frequency and significance. Paths containing the following were omitted in the figure to increase figure legibility: baseline covariates (age, gender, and ethnicity) and baseline and follow-up variables for the major variables (activity frequency, activity significance, social connections, perceived control, and depression). Significant paths were presented by bold lines and standardized coefficients (*p < .05, **p < .01, and ***p < .001).
Indirect Effects via Increased Activity Engagement and Positive Perceptions of Activity Significance
To test mechanisms of change, ∆activity frequency and ∆activity significance were included as mediators simultaneously. ∆Depression was regressed on intervention group, ∆activity frequency, and ∆activity significance. ∆Activity frequency and ∆activity significance were regressed on intervention group. Covariance between the two mediators was estimated.
Model fit was excellent, χ2 (24) = 55.42, p < .001, CLI = .96, TLI = .95, RMSEA = .05, and SRMR = .04. Results showed that intervention led to increased activity frequency (β = .19, p < .001), which predicted decrease in depressive symptoms (β = −.15, p < .01). The intervention also led to a more positive perception of activity significance (β = .15, p < .001), which also predicted decreases in depressive symptoms (β = −.23, p < .001). See Figure 1 (Model B) for a visual presentation of the model and results.
Analyses of indirect effects showed that the intervention reduced depressive symptoms by increasing activity frequency (B = −.50, 95% CI [−1.16, −.16]) as well as positive perceptions of activity significance (B = −.58, 95% CI [−1.15, −.23]). Pairwise contrasts between the two indirect effects indicated that there was no significant difference in their magnitude (B = .08, 95% [−.56, .70]). In summary, increases in both activity frequency and positive perceptions of activity significance mediated the intervention effects on reduced depressive symptoms.
Underlying Psychological Variables
To further examine the psychological mechanisms of why activity frequency and activity significance appear to decrease depressive symptoms, we added two additional mediators: ∆social connections and ∆perceived control. In addition to intervention group, ∆activity frequency, and ∆activity significance, ∆depression was also regressed on ∆social connections and ∆perceived control. These two psychological mediators were regressed on intervention group, ∆activity frequency, and ∆activity significance. Covariance was estimated for the two activity mediators and the two psychological mediators.
The model fit the data well, χ2 (50)= 114.21, p < .001, CLI = .95, TLI = .93, RMSEA = .05, and SRMR = .05. The intervention predicted an increase in activity frequency (β = .19, p < .001), which further predicted an increase in social connections (β = .19, p < .01) and a decrease in depressive symptoms (β = −.12, p < .05), but not an increase in perceived control. The intervention also predicted a more positive perception of activity significance (β = .15, p < .01), which further predicted an increase in perceived control (β = .11, p < .01) and decrease in depressive symptoms (β = −.23, p < .001), but not an increase in social connections. Decreased depressive symptoms were also predicted by increased social connections (β = −.18, p < .001) and increased perceived control (β = −.13, p < .05). See Figure 1 (Model C) for a visual presentation of the model and results.
Analyses of indirect effects between intervention and ∆depression were conducted. Results showed that an indirect effect via ∆activity frequency was significant (B = −.40, 95% CI [−.95, −.09]). There was also a significant indirect effect from intervention, ∆activity frequency, and ∆social connections to ∆depression, B = −.12, 95% CI [−.29, −.03]. In contrast, there was no indirect effect of intervention, ∆activity frequency, or ∆perceived control to ∆depression. Pairwise contrasts of the two indirect effects showed that the strength of association was significantly larger for indirect effects via ∆social connections than for those via ∆perceived control (B = −.14, 95% [−.34, −.05]).
Indirect effects via ∆activity significance were also present (B = −.57, 95% CI [−1.13, −.21]), along with a significant indirect effect of intervention, ∆activity significance, and ∆perceived control to ∆depression, B = −.04, 95% CI [−.11, −.01]. In contrast, no indirect effect was observed for intervention, ∆activity significance, or ∆social connections to ∆depression. Despite one indirect effect being significant and the other not, a pairwise contrast showed that the magnitude of the indirect effects did not differ significantly (B = −.03, 95% [−.13, .03]). Therefore, for ∆activity significance, we cannot conclude that ∆perceived control was a stronger “downstream mediator” than ∆social connections.
Nevertheless, these findings demonstrated different psychological mechanisms behind these two aspects of activities. ∆Activity frequency predicted ∆depressive symptoms partially via ∆social connections but not via increased perceived control. In contrast, ∆perceived control partially mediated the association between ∆activity significance and ∆depressive symptoms, although the magnitude of mediation was not significantly larger than that for increased social connections.
Post Hoc Analyses on Activity Frequency
Post hoc analyses were conducted to identify specific activities that increased in frequency following intervention, compared to the control group. Independent samples t-tests showed that participants in the intervention group increased the frequency of socializing with family [t(357) = −2.11, p < .05], socializing with friends [t(357) = −2.39, p < .05], helping others [t(357) = −3.29, p < .01], taking or teaching classes [t(348.22) = −2.77, p < .01], creative activities [t(357) = −3.32, p < .01], talking on the telephone [t(357) = −2.28, p < .05], and shopping [t(357) = −2.15, p < .05]. These activities generally involve interactions with others, which is consistent with the finding that increased social connections partially mediated the effects of increased activity frequency on reduced depressive symptoms.
Implications
In this study, we investigated the mechanisms of change for an activity-based lifestyle intervention. Consistent with our hypotheses, the intervention reduced older adults’ depressive symptoms through increasing activity frequency and promoting positive perceptions of activity significance. This result is consistent with the occupational therapy discipline’s emphasis on the health-promoting value of professionally guided daily activity (Clark et al., 1997; Law, 2002). Our findings also dovetail with behavioral theories of depression which posit that behavioral activation disrupts maladaptive behavioral cycles (Cuijpers, van Straten, & Warmerdam, 2007). Also of note, our results bolster the case for a “causal” role of the intervention in affecting older adults’ mental well-being, as differences in activity changes emanated from an intervention that was experimentally manipulated. However, given that activity was systematically facilitated, caution is warranted in generalizing these results to older adults’ naturally occurring, self-generated activity efforts.
Our findings also suggest that activity frequency and activity significance likely function independently. Assessing both mediators simultaneously helped determine the magnitude of specific indirect effects via one mediator, conditional on the presence of the other. Further, when analyzing the psychological mechanisms behind the two activity-related factors, our findings showed distinctive mechanisms for activity frequency and activity significance. These findings echo prior research emphasizing the need to evaluate and target global perception of activity significance, in addition to activity frequency (Mallinson et al., 2014; Carlson, Kuo, Chou, & Clark, 2013).
The association between increased activity frequency and reduced depressive symptoms was partially mediated by increased social connections, which was a salient characteristic of the specific activities that increased in frequency following the intervention. This finding underscores the notion that activities can maintain and foster social connectedness (Bauman, Merom, Bull, Buchner, & Singh, 2016; Riebe et al., 2012). This study focused on structural aspects of social support, the size and strength of social networks, and frequency of social contacts. Past studies have indicated that functional social support, or the perception of the adequacy of available support, predicts positive physical and mental health outcomes more consistently than structural social support (Barth, Schneider, & von Kanel, 2010; Murrell, Norris, & Chipley, 1992). Therefore, future studies would benefit from understanding whether functional social support also mediates the association between increased activity frequency and reduced depressive symptoms.
The association between increased activity significance and reduced depressive symptoms was partially mediated by increased perceived control. Enhancing older adults’ appreciation for the role of activities can reduce feelings of helplessness, as older adults develop a stronger sense that they have the ability to influence their well-being. Individuals with a stronger sense of control may have a more positive outlook and perceive fewer barriers to becoming active (Ayotte, Margrett, & Hicks-Patrick, 2010), eventually resulting in behavioral changes that promote well-being (Lachman, 2006). In this study, increased perceived control and increased activity frequency were not associated. This may be because perceived control is linked with self-generated increased activity frequency but not with increased activity frequency emanating from direct support and systematic facilitation. Nevertheless, our findings indicate that promoting a positive perception of activity significance can foster a stronger sense of control over one’s daily routines and health, which may help older adults maintain an active lifestyle on their own following intervention.
It is important to note that social connections and perceived control only partially explained associations between the two activity-related factors and reduced symptoms of depression. There may be additional pathways through which these activity factors promote better mental health. Future studies should examine other mechanisms explaining the benefits of activity participation, such as physiological and functional changes (Fox, 1999).
In an effort to increase generalizability of the results, we recruited an ethnically diverse sample of community-dwelling older adults, with non-Hispanic Whites a minority. The ethnic groups were not large enough, however, to allow for separate analysis, and so we included ethnic categories as covariates, along with other covariates (age and gender), to adjust for their effects on changes in depressive symptoms and other mediators in the model simultaneously.
Clinical Implications
Our findings provide empirical support for the guiding principles of occupational therapy and more broadly to activity-centered interventions. Although there are numerous theoretical discussions about why such interventions work, there has been little supportive evidence. More studies that directly test the mechanisms of change are an important next step in attempting to understand why and how interventions work, ultimately providing new insights on how to optimize treatment across settings and populations.
Our study outcomes support the continued development of interventions that target activity changes as a route to improved well-being among older adults. In connection with this effort, clinicians may specifically attend to a proposed activity’s potential to foster social contact. Clinicians may also enhance participants’ sense of control by encouraging them to reflect on how activities shape their health and well-being. Further, clinicians across disciplines should consider other methods, in addition to targeting frequency and significance of activities, to enhance social connections and perceived control. For example, connections with others can also be fostered through teaching social skills and sense of control can be enhanced through cognitive restructuring.
Along these lines, it would be useful to assess change mechanisms in other interventions that focus on activity participation. For example, behavioral activation in psychology also involves assisting patients to engage in pleasurable activities (Cuijpers et al., 2007; Kanter et al., 2010). Approaches to increasing activity participation may vary, but mechanisms of change may be similar. The notion that different types of interventions contain similar active ingredients highlights the potential value of integrating key strategies used in different treatment approaches. Such effort to integrate services can bring parsimony and increase effectiveness for different types of interventions targeting the same outcome. This also raises an important question of how services across disciplines strive to achieve comparable goals and complement each other while maintaining their unique contributions.
Limitations
One important study limitation is that only two measurement time points were included in the analysis. This precludes identification of the sequence of temporal effects, such that it is not possible to document that changes in activity (or in social contact and perceived control) occurred prior to improvements in depression. Therefore, alternate explanations such as those based on reverse causation cannot be ruled out. For example, the intervention may have first reduced depression, which in turn produced beneficial changes in activity.
A second limitation is the unknown extent to which the results generalize to other elder populations or treatment settings. In the current study, the participants were multiethnic community-dwellers within a large metropolitan environment that included opportunities to engage in a wide range of activities, both at senior centers and in public settings such as parks and museums. Although the nexus among intervention, activity, and improved health is thought to be robust, further research should be undertaken to determine the extent to which these mediation routes hold for groups such as nursing home residents or older adults in rural environments.
Although the effect size for increased activity frequency postintervention was moderate, effect sizes for changes in depressive symptoms and perceptions of activity significance were small. The small effect sizes may in part be due to our approach of ITT analysis, in which treatment effects tend to be more conservative (Gupta, 2011). In addition, given that our intervention was designed to improve well-being for all older adults, we recruited a group of relatively healthy and nonclinically depressed elders. This may have led to relatively smaller decreases in depressive symptoms due to floor effects. However, the exploration of process variables is important to understanding change processes, irrespective of the effect size magnitude.
Conclusions
Empirical tests of therapeutic change mechanisms underlying activity-based lifestyle interventions have been extremely limited. Our study showed that an occupational therapy-based lifestyle intervention reduced depressive symptoms by facilitating activity frequency and promoting activity significance. We also showed two possible avenues in which activity frequency and activity significance may be beneficial. First, the intervention led to increased activity frequency, which predicted fewer depressive symptoms through increased social connections. Second, the intervention increased the perceived significance of activities, which in turn reduced depressive symptoms through the pathway of increased perceived control. Our findings not only provide evidence for the theoretical underpinnings of lifestyle-based interventions, but also suggest ways in which clinicians can optimize therapeutic changes.
Supplementary Material
Supplementary data are available at The Gerontologist online.
Funding
The work was supported by the National Institute on Aging (R01 AG021108 to F. C.) and the K12 Rehabilitation Research Career Development Program (K12 HD055929 to S. S. N).
Supplementary Material
References
- Ayotte B. J. Margrett J. A., & Hicks-Patrick J (2010). Physical activity in middle-aged and young-old adults the roles of self-efficacy, barriers, outcome expectancies, self-regulatory behaviors and social support. Journal of Health Psychology, 15, 173–185. doi:10.1177/1359105309342283 [DOI] [PubMed] [Google Scholar]
- Barrera M. Jr. Toobert D. J. Angell K. L. Glasgow R. E., & Mackinnon D. P (2006). Social support and social-ecological resources as mediators of lifestyle intervention effects for type 2 diabetes. Journal of Health Psychology, 11, 483–495. doi:10.1177/1359105306063321 [DOI] [PubMed] [Google Scholar]
- Barth J. Schneider S., & von Känel R (2010). Lack of social support in the etiology and the prognosis of coronary heart disease: A systematic review and meta-analysis. Psychosomatic Medicine, 72, 229–238. doi:10.1097/PSY.0b013e3181d01611 [DOI] [PubMed] [Google Scholar]
- Bauman A. Merom D. Bull F. C. Buchner D. M., & Singh M. A. F (2016). Updating the evidence for physical activity: Summative reviews of the epidemiological evidence, prevalence, and interventions to promote “Active Aging”. The Gerontologist, 56, S268–S280. doi:10.1093/geront/gnw031 [DOI] [PubMed] [Google Scholar]
- Carlson M. Kuo A. Chou C. P., & Clark F (2013). Relationship of global self-evaluation of activity to psychosocial and health-related aging outcomes. OTJR: Occupation, Participation & Health, 33, 180–189. doi:10.3928/15394492-20130712-01 [Google Scholar]
- Chao S. F. (2016). Changes in leisure activities and dimensions of depressive symptoms in later life: A 12-year follow-up. The Gerontologist, 56, 397–407. doi:10.1093/geront/gnu052 [DOI] [PubMed] [Google Scholar]
- Clark F. Azen S. P. Zemke R. Jackson J. Carlson M. Mandel D., … Lipson L (1997). Occupational therapy for independent-living older adults: A randomized controlled trial. Journal of the American Medical Association, 278, 1321–1326. doi:10.1001/jama.1997.03550160041036 [PubMed] [Google Scholar]
- Clark F. Blanchard J. Sleight A. Cogan A. Floríndez L. Gleason S., … Vigen C (2015). Lifestyle redesign: The intervention tested in the USC well elderly studies (2nd ed). Bethesda, MD: AOTA Press. [Google Scholar]
- Clark F. Jackson J. Carlson M. Chou C. P. Cherry B. J. Jordan-Marsh M., … Azen S. P (2012). Effectiveness of a lifestyle intervention in promoting the well-being of independently living older people: Results of the Well Elderly 2 Randomised Controlled Trial. Journal of Epidemiology & Community Health, 66, 782–790. doi:10.1136/jech.2009.099754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuijpers P. van Straten A., & Warmerdam L (2007). Behavioral activation treatments of depression: A meta-analysis. Clinical Psychology Review, 27, 318–326. doi:10.1016/j.cpr.2006.11.001 [DOI] [PubMed] [Google Scholar]
- Dour H. J. Wiley J. F. Roy-Byrne P. Stein M. B. Sullivan G. Sherbourne C. D., … Craske M. G (2014). Perceived social support mediates anxiety and depressive symptom changes following primary care intervention. Depression and Anxiety, 31, 436–442. doi:10.1002/da.22216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dracup K. Westlake C. Erickson V. S. Moser D. K. Caldwell M. L., & Hamilton M. A (2003). Perceived control reduces emotional stress in patients with heart failure. The Journal of Heart and Lung Transplantation, 22, 90–93. doi:10.1016/S1053-2498(02)00454-0 [DOI] [PubMed] [Google Scholar]
- Eakman A. M. (2013). Relationships between meaningful activity, basic psychological needs, and meaning in life: Test of the meaningful activity and life meaning model. OTJR: Occupation, Participation and Health, 33, 100–109. doi:10.3928/15394492-20130222-02 [DOI] [PubMed] [Google Scholar]
- Eakman A. M. (2014). A prospective longitudinal study testing relationships between meaningful activities, basic psychological needs fulfillment, and meaning in life. OTJR: Occupation, Participation and Health, 34, 93–105. doi:10.3928/15394492-20140211-01 [DOI] [PubMed] [Google Scholar]
- Eakman A. M. Carlson M. E., & Clark F. A (2010). Factor structure, reliability, and convergent validity of the Engagement in Meaningful Activities Survey for older adults. OTJR: Occupation, Participation & Health, 30, 111–121. doi:10.3928/15394492-20090518-01 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edgelow M., & Krupa T (2011). Randomized controlled pilot study of an occupational time-use intervention for people with serious mental illness. The American Journal of Occupational Therapy, 65, 267–276. doi:10.5014/ajot.2011.001313 [DOI] [PubMed] [Google Scholar]
- Eizenman D. R. Nesselroade J. R. Featherman D. L., & Rowe J. W (1997). Intraindividual variability in perceived control in an older sample: The MacArthur successful aging studies. Psychology and Aging, 12, 489–502. doi:10.1037/0882-7974.12.3.489 [DOI] [PubMed] [Google Scholar]
- Everard K. M. Lach H. W. Fisher E. B., & Baum M. C (2000). Relationship of activity and social support to the functional health of older adults. The Journals of Gerontology: Series B – Psychological Sciences & Social Sciences, 55, S208–212. doi:10.1093/geronb/55.4.S208 [DOI] [PubMed] [Google Scholar]
- Fox K. R. (1999). The influence of physical activity on mental well-being. Public Health Nutrition, 2, 411–418. doi:10.1017/S1368980099000567 [DOI] [PubMed] [Google Scholar]
- Glass T. A. De Leon C. F. Bassuk S. S., & Berkman L. F (2006). Social engagement and depressive symptoms in late life: Longitudinal findings. Journal of Aging and Health, 18, 604–628. doi:10.1177/0898264306291017 [DOI] [PubMed] [Google Scholar]
- Gupta S. K. (2011). Intention-to-treat concept: A review. Perspectives in Clinical Research, 2, 109. doi:10.4103/2229–3485.83221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hong S. I. Hasche L., & Bowland S (2009). Structural relationships between social activities and longitudinal trajectories of depression among older adults. The Gerontologist, 49, 1–11. doi:10.1093/geront/gnp006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson J. (1996). Living a meaningful existence in old age. In Zemke R., Clark F. (Eds.), Occupational science: The evolving discipline (pp. 339–361). Philadelphia: F. A. Davis. [Google Scholar]
- Jackson J. Carlson M. Mandel D. Zemke R., & Clark F (1998). Occupation in lifestyle redesign: The Well Elderly Study Occupational Therapy Program. American Journal of Occupational Therapy, 52, 326–336. doi:10.5014/ajot.52.5.326 [DOI] [PubMed] [Google Scholar]
- Jackson J. Mandel D. Blanchard J. Carlson M. Cherry B. Azen S., … Clark F (2009). Confronting challenges in intervention research with ethnically diverse older adults: the USC Well Elderly II Trial. Clinical Trials, 6, 90–101. doi:10.1177/1740774508101191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanter J. W. Manos R. C. Bowe W. M. Baruch D. E. Busch A. M., & Rusch L. C (2010). What is behavioral activation? A review of the empirical literature. Clinical Psychology Review, 30, 608–620. doi:10.1016/j.cpr.2010.04.001 [DOI] [PubMed] [Google Scholar]
- Kazdin A. E. (2007). Mediators and mechanisms of change in psychotherapy research. Annual Review of Clinical Psychology, 3, 1–27. doi:10.1146/annurev.clinpsy.3.022806.091432 [DOI] [PubMed] [Google Scholar]
- Lachman M. E. (2006). Perceived control over aging-related declines adaptive beliefs and behaviors. Current Directions in Psychological Science, 15, 282–286. doi: 10.1111/j.1467-8721.2006.00453.x [Google Scholar]
- Law M. (2002). Participation in the occupations of everyday life. American Journal of Occupational Therapy, 56, 640–649. doi:10.5014/ajot.56.6.640 [DOI] [PubMed] [Google Scholar]
- Lemon B. W. Bengtson V. L., & Peterson J. A (1972). An exploration of the Activity Theory of Aging: Activity types and life satisfaction among in-movers to a retirement community. Journal of Gerontology, 27, 511–523. doi: 10.1093/geronj/27.4.511 [DOI] [PubMed] [Google Scholar]
- Lubben J. E. (1988). Assessing social networks among elderly populations. Family & Community Health: The Journal of Health Promotion & Maintenance, 11, 42–52. doi:10.1097/00003727-198811000-00008. [Google Scholar]
- Mallinson T. Schepens Niemiec S. L. Carlson M. Leland N. Vigen C. Blanchard J., & Clark F (2014). Development and validation of the activity significance personal evaluation (ASPEn) scale. Australian Occupational Therapy Journal, 61, 384–393. doi:10.1111/1440–1630.12155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McArdle J. J. (2009). Latent variable modeling of differences and changes with longitudinal data. Annual Review of Psychology, 60, 577–605. doi:10.1146/annurev.psych.60.110707.163612 [DOI] [PubMed] [Google Scholar]
- Menec V. H. (2003). The relation between everyday activities and successful aging: A 6-year longitudinal study. The Journals of Gerontology: Series B – Psychological Sciences & Social Sciences, 58, S74–S82. doi:10.1093/geronb/58.2.S74 [DOI] [PubMed] [Google Scholar]
- Moser D. K., & Dracup K (1995). Psychosocial recovery from a cardiac event: The influence of perceived control. Heart & Lung, 24, 273–280. doi:10.1016/S0147-9563(05)80070–6 [DOI] [PubMed] [Google Scholar]
- Murrell S. A. Norris F. H., & Chipley Q. T (1992). Functional versus structural social support, desirable events, and positive affect in older adults. Psychology and Aging, 7, 562. doi:10.1037/0882-7974.7.4.562 [DOI] [PubMed] [Google Scholar]
- Oh H., & Ell K (2015). Social support, a mediator in collaborative depression care for cancer patients. Research on Social Work Practice, 25, 229–239. doi:10.1177/1049731514525240 [Google Scholar]
- Preacher K. J., & Hayes A. F (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods, 40, 879–891. doi:10.3758/BRM.40.3.879 [DOI] [PubMed] [Google Scholar]
- Radloff L. S. (1977). The CES-D scale a self-report depression scale for research in the general population. Applied Psychological Measurement, 1, 385–401. doi:10.1177/014662167700100306 [Google Scholar]
- Riebe G. Fan M. Y. Unutzer J., & Vannoy S (2012). Activity scheduling as a core component of effective care management for late-life depression. International Journal of Geriatric Psychiatry, 27, 1298–1304. doi:10.1002/gps.3784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roland K. P., & Chappell N. L (2015). Meaningful activity for persons with dementia: Family caregiver perspectives. American Journal of Alzheimer’s Disease & Other Dementias, 30, 559–568. doi:10.1177/1533317515576389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salanova M. Llorens S., & Schaufeli W. B (2011). “Yes, I can, I feel good, and I just do it!” On gain cycles and spirals of efficacy beliefs, affect, and engagement. Applied Psychology, 60, 255–285. [Google Scholar]
- Schulz R., & Decker S (1985). Long-term adjustment to physical disability: The role of social support, perceived control, and self-blame. Journal of Personality and Social Psychology, 48, 1162–1172. [DOI] [PubMed] [Google Scholar]
- Turk D. C. Okifuji A., & Scharff L (1995). Chronic pain and depression: Role of perceived impact and perceived control in different age cohorts. Pain, 61, 93–101. [DOI] [PubMed] [Google Scholar]
- Wallston K. A. Wallston B. S. Smith S., & Dobbin C (1987). Perceived control and health. Current Psychological Research & Reviews, 6, 5. doi:10.1007/BF02686633 [Google Scholar]
- Wang J., & Wang X (2012). Structural equation modeling: Applications using Mplus. Chichester, UK: John Wiley & Sons. [Google Scholar]
- Whyte J., & Hart T (2003). It’s more than a black box; it’s a Russian doll: Defining rehabilitation treatments. American Journal of Physical Medicine & Rehabilitation, 82, 639–652. doi:10.1097/01.PHM.0000078200.61840.2D [DOI] [PubMed] [Google Scholar]
- Wright-St Clair V. (2012). Being occupied with what matters in advanced age. Journal of Occupational Science, 19, 44–53. doi:10.1080/14427591.2011.639135 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.