Abstract
Objective
To determine the percentage of research projects funded by the National Health and Medical Research Council in the period 2000–2014 that aimed specifically to deliver health benefits to Australians living in rural and remote areas and to estimate the proportion of total funding this represented in 2005–2014.
Design
This is a retrospective analysis of publicly available datasets.
Setting
National Health and Medical Research Council Rural and Remote Health Research 2000–2014.
Outcome measures
‘Australian Rural Health Research’ was defined as: research that focussed on rural or remote Australia; that related to the National Health and Medical Research Council's research categories other than Basic Science; and aimed specifically to improve the health of Australians living in rural and remote areas. Grants meeting the inclusion criteria were grouped according to the National Health and Medical Research Council's categories and potential benefit. Funding totals were aggregated and compared to the total funding and Indigenous funding for the period 2005–2014.
Results
Of the 16 651 National Health and Medical Research Council‐funded projects, 185 (1.1%) that commenced funding during the period 2000–2014 were defined as ‘Australian Rural Health Research’. The funding for Australian Rural Health Research increased from 1.0% of the total in 2005 to 2.4% in 2014. A summary of the funding according to the National Health and Medical Research Council's research categories and potential benefit is presented.
Conclusion
Addressing the health inequality experienced by rural and remote Australians is a stated aim of the Australian Government. While National Health and Medical Research Council funding for rural health research has increased over the past decade, at 2.4% by value, it appears very low given the extent of the health status and health service deficits faced by the 30% who live in rural Australia.
Keywords: health outcomes research, Indigenous health, remote health, research, rural health
What is already known on this subject:
Approximately 30% of Australians live in rural and remote areas.
Rural and remote Australians have poorer health and less access to health professionals and services than their urban counterparts.
Addressing rural health inequality is a key aim of the Australian Government, outlined in policy documents.
The National Health and Medical Research Council provides approximately $800 million of funding to health and medical research annually.
What this study adds:
This article presents an analysis of publicly available databases to determine the proportion of the National Health and Medical Research Council‐funded research that is specifically aimed to deliver health benefits to rural‐ and remote‐living Australians in the period 2000–2014 and the proportion of total funding this represented in the period 2005–2014.
Of the total 16 651 National Health and Medical Research Council grants that commenced funding in the period 2000–2014, 184 (1.1%) were for Australian Rural Health Research, as defined in this article.
In 2005, Australian Rural Health Research represented 1.0% of the total National Health and Medical Research Council funding, excluding Basic Science research, increasing to 2.4% in 2014.
The findings demonstrate that, although increasing, investment in Australian Rural Health Research as defined remains low, given the widely understood and accepted poorer health status and services in rural areas.
Introduction
Approximately 30% of Australians live in rural and remote areas.1, 2, 3 The term ‘rural and remote’ is used to refer to all areas outside major cities, according to the Australian Bureau of Statistics Australian Standard Geographical Classification.3 Australians living in rural and remote areas generally have poorer health than their urban counterparts, with higher rates of chronic disease and lifestyle‐related illnesses, higher mortality rates and lower life expectancy and higher rates of smoking, alcohol misuse and obesity.2 These people also experience disadvantages in relation to their social determinants of health, such as lower levels of education, employment and income than Australians living in major cities.2 Despite their increased burden of illness, people living in rural and remote areas have less access to health professionals and services.3 Health service delivery in rural and remote areas faces complex and unique challenges, including distance, higher costs and workforce shortages.2 Due to this unique combination of factors, research that is specific to the needs of rural communities is required to address rural health disadvantage.
Addressing health inequality for rural and remote Australians is a stated priority of the Australian Government.2 The National Health and Medical Research Council (NHMRC) provides approximately $800 million to health and medical research annually,4 but is not explicitly charged with the task of addressing rural inequity or disadvantage. This article reports an analysis of NHMRC data to quantify NHMRC research funding that is specifically aimed to improve the health of rural and remote Australians.
Methods
This study is a retrospective analysis of the NHMRC dataset, Rural and Remote Health Research 2000–2014.5 Figure 1 outlines the method of analysis.
Figure 1.
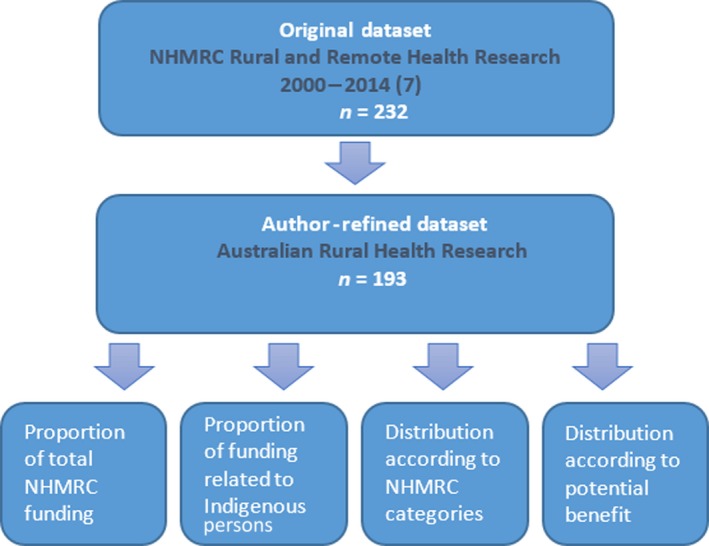
Overview of data analysis method.
Identifying ‘Australian Rural Health Research’
Two of the authors independently analysed the NHMRC dataset, Rural and Remote Health Research 2000–2014,5 to determine the proportion of grants in this dataset that specifically aimed to deliver benefits to people living in rural and remote Australia. The NHMRC defined as ‘rural’ all research activities where the description or keywords included the words ‘rural’, remote’, ‘regional’, ‘country’ or ‘isolated’.5 The dataset therefore included some international studies and some Australian studies that used one or more of the keywords in different contexts; that is, ‘remote sensing’. To overcome these discrepancies, the authors developed a mutually verified system to describe whether research specifically benefitted Australians living in rural or remote areas. The authors’ definition of ‘Australian Rural Health Research (ARHR)’ was: research that focussed on rural or remote Australia; that related to any of the NHMRC research categories other than Basic Science (on the grounds that Basic Science outcomes would benefit all Australians); and aimed to improve the health of Australians living in rural and remote areas. Projects meeting the definition were combined to form an ARHR dataset that was used for the remaining analysis.
Australian Rural Health Research as a proportion of National Health and Medical Research Council funding
To assess the proportion of ARHR funding, compared with total NHMRC funding across all schemes, a simple aggregation of the number and value of annual grant payments made to ARHR between 2005 and 2014 was undertaken. A comparison was then made with the number and value of all NHMRC annual grant payments made between 2005 and 2014 drawn from the NHMRC datasets ‘The Last Ten Years 2005–2014’ and ‘All grants 2000–2015’.6
Research benefitting Aboriginal and Torres Strait Islander people
To better understand the contribution of ARHR in improving the health of Indigenous communities, the authors calculated the proportion of the refined dataset that represented targeted benefit for Aboriginal or Torres Strait Islander people. This was compared with the NHMRC's Aboriginal and Torres Strait Islander Health Research 2000–2014 dataset8 to determine the proportion of rural health funding related to Indigenous health and the proportion of Indigenous health research funding specifically benefitting the 65% of Indigenous people who live in rural and remote Australia.9
Australian Rural Health Research according to National Health and Medical Research Council categories and potential research benefits
The authors classified the identified ARHR funding according to the following NHMRC‐defined categories: Clinical Medicine and Science; Health Services Research; and Public Health. A further classification system was then developed to describe the potential benefits of ARHR:
Improve the delivery of services (including clinical, public health, prevention or health promotion).
Improve treatments or procedures for people living in rural or remote Australia.
Address health determinants (e.g. social determinants, smoking and obesity).
Improve health through other mechanisms.
Results
Identifying Rural Health Research
In total, 232 individual grants were classified by the NHMRC as relating to rural health and received grant payments at some stage of the period 2000–2014. Of these, 39 were excluded from the analysis. Of these 39, 12 were grants for international research, while a further 23 were deemed not to be relevant in improving the health of Australians living in rural and remote areas (e.g. five were related to ‘remote sensing’). Four grants were categorised by the NHMRC as Basic Science and these were excluded as per the definition above.
Thus, a total of 193 projects that received funding in the period 2000–2014 and which met the adopted definition of ARHR were included in this study. Of these, 184 commenced funding in this period, equating to 1.1% of the total (16 651) whose funding commenced in this period.
Australian Rural Health Research as a proportion of National Health and Medical Research Council funding
From 2005 to 2014, the number of ARHR projects receiving NHMRC funding each year increased from just under 30 to just under 70. During this period, the total number of projects funded each year by the NHMRC increased from around 3000 to around 4500 per year. Of these, around 1500 and 2100 were classified as Basic Science, respectively. Following the exclusion of NHMRC Basic Science projects from the analysis, ARHR represented approximately 2.0% of NHMRC grants, increasing to approximately 2.7% in 2012, 2013 and 2014.
The amount of NHMRC funding received by ARHR each year increased from around $2 million in 2005 to around $11 million by 2014 (a total of $69 million for the decade). However, during this period, total NHMRC funding doubled from around $400 million to around $800 million, while funding for research, excluding Basic Science, increased from just over $200 million to around $450 million. This means that the share of total NHMRC research money going to ARHR increased from 0.5% in 2005 to 1.4% in 2014; or, if Basic Science is excluded, it increased from 1.0% to 2.4%.
Research benefitting Aboriginal and Torres Strait Islander people
The NHMRC estimates that in the period 2005–2014, it invested $365 million in total in Indigenous health research,8 which represented 5.5% of its total funding. This included $39 million on ARHR specifically aimed to benefit Aboriginal and Torres Strait Islander people living in rural and remote Australia. This $39 million represented 55% of the total amount allocated to ARHR as defined.
Australian Rural Health Research funding in National Health and Medical Research Council categories
Grants classified by the NHMRC as ‘Public Health’ received 58% of ARHR funding, those classified as ‘Health Services’ received 31% and those classified as ‘Clinical Medicine and Science’ received 10%. Figure 2 shows the percentage of NHMRC's ARHR funding, classified according to NHMRC funding categories for general and Indigenous health research.
Figure 2.
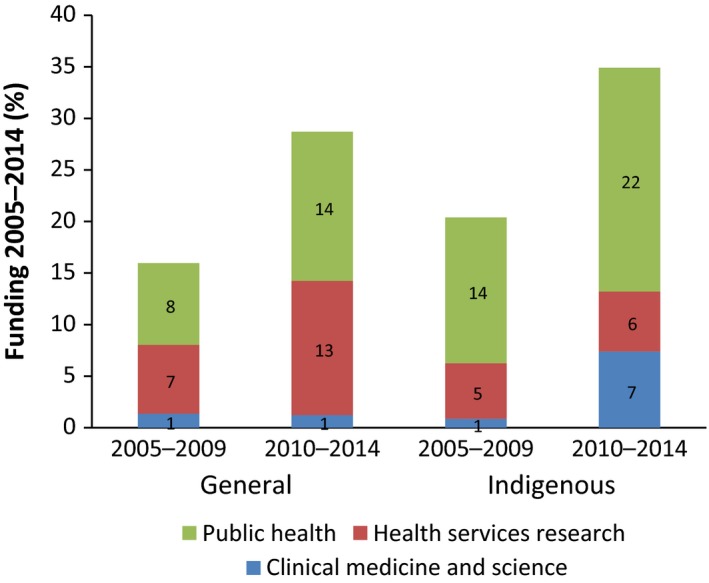
Australian Rural Health Research funding 2005–2014 allocated to National Health and Medical Research Council categories.
Australian Rural Health Research according to potential research benefits
Categorisation based on this assessment of the potential benefits of research provides another perspective. Of the total number of ARHR activities funded between 2005 and 2014, 27% were likely to address health determinants, 52% were likely to improve health service delivery, 24% were likely to lead to better procedures and 22% addressed rural health in other ways. Figure 3 shows the percentage of NHMRC’s ARHR funding classified according to the authors’ categories of potential research benefit for general and Indigenous health research.
Figure 3.
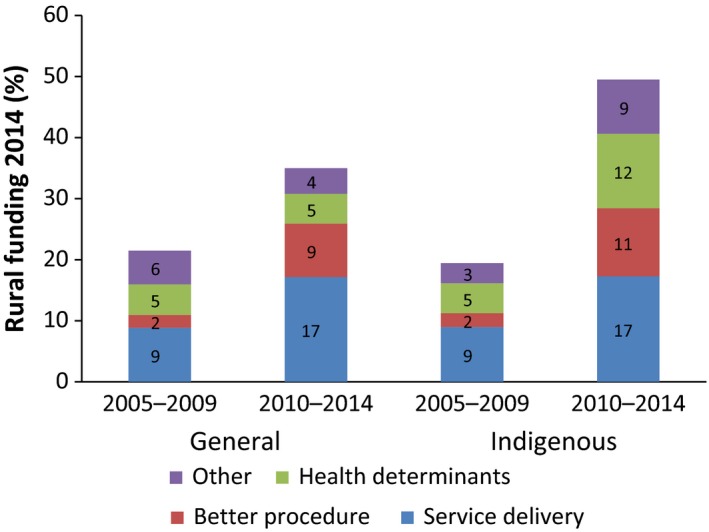
Australian Rural Health Research funding 2005–2014 allocated to potential areas of benefit.Note: Some projects were classified under more than one category, in which case, the full funding amount was allocated to each category and consequently the sum of the percentages (125%) exceeds 100%. As each project could be allocated to more than one category, it is not possible to make absolute comparisons between years or between general and Indigenous rural research.
Discussion
It was found that NHMRC funding for health research that specifically aimed to deliver health benefits to people who live in rural or remote Australia increased between 2005 and 2014 but still represented only 2.4% of total NHMRC research funding not categorised as Basic Science research in 2014.
The authors believe that, based on the significant challenges and deficits in health and health services experienced by people in rural areas, that rural health ought to be a priority for NHMRC funding.
A desirable precedent has been set by the prioritisation given by the NHMRC to Aboriginal and Torres Strait Islander health to help address the persistent and well‐documented disadvantages faced by these Australians.
Research that addresses particular health disadvantages is important, not only in a social justice sense but also to moderate the growing cost of chronic diseases and their treatments. While the poorer health outcomes of Australians living in rural and remote areas (including the majority of Aboriginal and Torres Strait Islander people who live there)10 are partially a consequence of social and environmental determinants, they also reflect lower levels of access to public and private health services and the efficiency and appropriateness of services.11 Research is needed to improve rural and remote social determinants and to develop and evaluate services that are fit for purpose and designed in ways that enable optimal clinical supervision and quality control, sometimes in challenging circumstances.12
The proposed higher priority on rural issues should not in any way reduce the emphasis given by the NHMRC to the health of Aboriginal and Torres Strait Islander people. Indeed, the significant proportion of rural research that is about Indigenous health is appropriate and very welcome. High‐quality, rurally focussed and located research helps to build the rural health sector's capacity and has been demonstrated to bring positive health service and cost outcomes.13, 14 Research that improves rural service delivery and that addresses the underlying causes of poor health can make a critical contribution to the reduction of rural health inequality, a key aim of the Australian Government.
The NHMRC is Australia's premier science and health research body and NHMRC‐funded projects bring strong intellectual capital to address local issues and also hold status as important projects developing new evidence. Therefore, NHMRC funding will increase the focus on rural and remote health research as an important research and policy area.
Limitations of the study
The publicly available NHMRC datasets used for the study provide information on the number of funded activities for 2000–2014 and on the value of grants for the period 2005–2014.
Categorisation as an ARHR project first relies on NHMRC categorisation based on keywords. It is possible that NHMRC‐funded projects which benefit people living in rural or remote Australia, but whose description does not include any of these keywords, will not have been included, which would result in an undercount by this study of ARHR projects and funding.
The main limitation of the study is its focus on a particular subset of research activities defined, arbitrarily, by criteria selected by the authors. Clearly, NHMRC funding in other (non‐rural) categories is likely to benefit people living in rural areas. The focus on research that aimed specifically to benefit rural‐ and remote‐living Australians might be seen as a proxy for the extent to which the specific circumstances and specific needs of rural people are driving broad, diffuse national health agendas. The evidence from this study suggests that such specific recognition has had only a weak influence on the agendas set, at least in relation to research.
The benefits of health research constitute a public good that should flow equitably to all Australians, irrespective of their location. With research assets, as with infrastructure and clinical services, some positive discrimination is needed to balance the natural challenges of space, time and place.
Acknowledgements
The authors acknowledge Sarah Robin, Research Officer at University Centre for Rural Health North Coast, for her assistance with research and editing the manuscript.
Disclosure: The authors declare that they have no competing interests.
References
- 1. Australian Bureau of Statistics . Australian Social Trends March 2011: health outside major cities. Catalogue No. 4102.0. Canberra: Commonwealth of Australia, 2011. [Cited 7 July 2017]. Available from URL: http://www.abs.gov.au/AUSSTATS/abs@.nsf/Lookup/4102.0Main+Features30Mar+2011 [Google Scholar]
- 2. Australian Health Ministers Advisory Council (AHMAC) Rural Health Standing Committee . National Strategic Framework for Rural and Remote Health. Canberra: Commonwealth of Australia, 2012. [Cited 7 July 2017]. Available from URL: http://www.health.gov.au/internet/main/publishing.nsf/Content/national-strategic-framework-rural-remote-health [Google Scholar]
- 3. National Rural Health Alliance . The Little Book of Rural Health Numbers. Canberra: NRHA, 2015. [Cited 7 July 2017]. Available from URL: http://ruralhealth.org.au/book/little-book-rural-health-numbers [Google Scholar]
- 4. National Health and Medical Research Council . Research funding statistics and data. Canberra: NHMRC, 2015. [Cited 12 July 2015]. Available from URL: https://www.nhmrc.gov.au/grants-funding/research-funding-statistics-and-data [Google Scholar]
- 5. National Health and Medical Research Council . Rural and Remote Health Research 2000–2014. Canberra: NHMRC, 2015. [Cited 12 July 2015]. Available From URL: https://www.nhmrc.gov.au/_files_nhmrc/file/grants/dataset/2015/rural_remote_health%20research_%202000-2014.xlsx [Google Scholar]
- 6. National Health and Medical Research Council . The Last Ten Years 2005–2014. Canberra: NHMRC, 2015. [Cited 12 July 2015]. Available from URL: https://www.nhmrc.gov.au/grants-funding/research-funding-statistics-and-data [Google Scholar]
- 7. National Health and Medical Research Council . All grants 2000–2015. Canberra: NHMRC, 2016. [Cited 12 May 2016]. Available from URL: https://www.nhmrc.gov.au/grants-funding/research-funding-statistics-and-data [Google Scholar]
- 8. National Health and Medical Research Council . Aboriginal and Torres Strait Islander Health Research 2000–2014. Canberra: NHMRC, 2015. [Cited 12 July 2015]. Available from URL: https://www.nhmrc.gov.au/_files_nhmrc/file/grants/dataset/2015/aboriginal_torres_strait_islander_health_research_2000-2014.xlsx [Google Scholar]
- 9. Australian Bureau of Statistics . 3238.0.55.001 – Estimates of Aboriginal and Torres Strait Islander Australians, June 2011. Canberra: ABS, 2015. [Cited 7 July 2017]. Available from URL: http://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/3238.0.55.001June%202011?OpenDocument [Google Scholar]
- 10. Commonwealth of Australia . Aboriginal and Torres Strait Islander Health Performance Framework 2014 Report. Canberra: Australian Bureau of Statistics, 2015. [Cited 7 July 2017]. Available from URL: https://www.pmc.gov.au/sites/default/files/publications/Aboriginal_and_Torres_Strait_Islander_HPF_2014%20-%20edited%2016%20June2015.pdf [Google Scholar]
- 11. National Rural Health Alliance . A snapshot of poverty in rural and remote Australia, October 2013. Canberra: NRHA, 2015. [Cited 12 July 2015]. Available from: http://www.ruralhealth.org.au/document/snapshot-poverty-rural-and-regional-australia [Google Scholar]
- 12. Bar‐Zeev S, Kruske S, Barclay L, Bar‐Zeev N, Carapetis J, Kildea S. Use of health services by remote dwelling Aboriginal infants in tropical northern Australia: a retrospective cohort study. BMC Pediatrics 2012; 12: 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Cunningham FC, Ferguson‐Hill S, Matthews V, Bailie R. Leveraging quality improvement through use of the Systems Assessment Tool in Indigenous primary health care services: a mixed methods study. BMC Health Services Research 2016; 16: 583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Bailie R, Matthews V, Brands J, Schierhout G. A systems‐based partnership learning model for strengthening primary healthcare. Implementation Science 2013; 8: 143. [DOI] [PMC free article] [PubMed] [Google Scholar]


