Abstract
Objective
Medical management of obesity can result in significant weight loss and reduce the burden of obesity‐related complications. This report employs a new conceptual model to quantify engagement with obesity care and associated determinants in the US adult population.
Methods
Engagement with obesity care was conceptualized as a cascade comprising 5 successive steps: perceiving oneself as overweight, desiring to lose weight, attempting weight loss, seeking care from a health care professional for obesity, and seeking care from a physician specifically.
Results
Among adults with obesity, 7.3% did not perceive themselves as overweight, 1.5% perceived themselves as overweight but had no desire to lose weight, 29.9% wanted to lose weight but did not try in the last year, 51.3% tried to lose weight but did not consult a health professional, and 6.4% sought help for weight loss from a health professional but not a physician, implying that 96.4% of the population with obesity had an unmet need for obesity care.
Conclusions
This analysis provides new insight into the most common points along the cascade at which disengagement occurs and can inform efforts to improve uptake of obesity‐related health care services.
Introduction
The prevalence of obesity (BMI ≥ 30 kg/m2) in the United States has risen rapidly over the past several decades. Evidence from clinical trials indicates that intensive lifestyle change can lead to weight loss and improved control of obesity‐related comorbidities 1. The US Preventive Services Task Force guidelines call for physicians to screen and refer patients with obesity for intensive multicomponent behavioral interventions 2. Medical management of obesity may also include pharmacotherapy targeting obesity directly or treating within the context of an associated comorbidity 3. Finally, for individuals with severe obesity, or with moderate obesity and an associated comorbidity, weight loss surgery may be indicated.
The US Department of Health and Human Services' Healthy People 2020 initiative set targets for a 10% relative reduction in obesity by 2020 4. However, evidence indicates secular shifts in body weight norms in the US population 5, with declines in the proportion of overweight individuals correctly perceiving themselves as such and in overweight adults trying to lose weight 6. Low motivation to lose weight across the population may result in fewer individuals with obesity consulting a health care professional or physician for obesity, which in turn may contribute to low uptake of obesity‐related medical care. Consistent with this idea, uptake of bariatric surgery remains low at the population level relative to the proportion of individuals who are eligible according to federal guidelines.
In this report, we estimate engagement with obesity care and associated determinants in US adults across a continuum that emphasizes perceptions of weight and motivation to lose weight as important prerequisites to successful long‐term weight management.
Methods
We used data from the 2005 to 2012 National Health and Nutrition Examination Survey (NHANES) (https://www.cdc.gov/nchs/nhanes/index.htm) to examine engagement with obesity care among adults aged 30 to 64 years with BMI ≥ 30.
Engagement with obesity care was conceptualized as a stepwise cascade with 5 nested stages. The stages included (1) perceiving oneself as overweight; (2) wanting to lose weight; (3) trying to lose weight within the past 12 months; (4) seeking the help of a health professional to assist with weight loss, including personal trainers, dietitians, nutritionists, doctors, or other health professionals within the past 12 months; and (5) seeking the help of a physician to lose weight within the past 12 months (Figure 1). For each level of the cascade, only those who indicated engagement with the prior level were considered.
Figure 1.
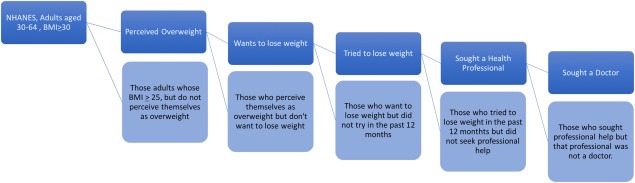
Obesity care cascade criteria: US adults ages 30‐64. Data are from NHANES 2005‐2012. [Color figure can be viewed at http://wileyonlinelibrary.com]
Determinants of engagement were analyzed using multivariable continuation ratio logit regression. Independent variables included demographic characteristics and socioeconomic and health status. In a sensitivity analysis, we constrained variables that demonstrated equality of coefficients across stages, as determined by Wald tests.
Results
Sample characteristics are provided in Supporting Information Table S1. The transition from trying to lose weight to seeking a health professional showed the highest relative disengagement (83.7%), followed by the transitions of seeking a health professional to seeking physician care (63.5%) and the desire to lose weight to attempting to lose weight (32.7%) (Figure 2).
Figure 2.
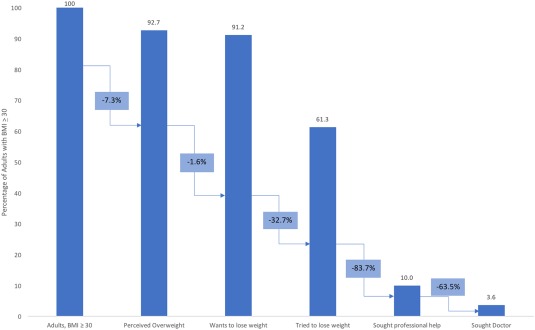
Obesity care cascade: US adults ages 30‐64. Data are from NHANES 2005‐2012. Of those adults who had obesity at examination (BMI ≥ 30), 92.7% perceived their body mass as overweight. Of those who held the perception of being overweight, 98.4% reported wanting to lose weight. Only 61.3% of those who wanted to lose weight tried losing weight over the last 12 months. Of those adults with obesity who met the prior criteria, only 16.3% sought a health professional for help to lose weight, with 36.5% of these individuals seeking a doctor. [Color figure can be viewed at http://wileyonlinelibrary.com]
Cascades were stratified on gender, race/ethnicity, and obesity class (Supporting Information Figures S1‐S8). Men showed more pronounced drop‐offs than women. Race/ethnicity‐specific cascades showed differences in perception of weight and the desire to lose weight, with non‐Hispanic whites engaging more with these initial steps of the cascade. Populations with class II and class III obesity demonstrated greater engagement across all steps of the cascade than individuals with class I obesity.
Table 1 shows the determinants of engagement across the cascade. Those with a higher BMI at examination, greater education, and diabetes were more likely to hold an accurate perception of overweight status. In contrast, those with greater BMI at age 25, males, non‐Hispanic blacks, and more recent NHANES survey years showed decreased odds of correct weight perception. Every 5‐unit increase in current BMI related to a 194% increase in the odds of correct overweight perception (odds ratio [OR]: 2.94; 95% CI: 2.17‐3.99). However, for every 5‐unit increase in BMI at age 25, there was a 27% decrease in the odds (OR: 0.73; 95% CI: 0.63‐0.84). When overweight perception for more recent survey years was compared to that of NHANES 2005‐2006, we observed decreased odds of accuracy (OR2007‐2008: 0.53; OR2009‐2010: 0.60; OR2011‐2012: 0.54).
Table 1.
Factors associated with obesity care cascade engagement, US adults ages 30‐64
| Perceived as having overweight | Wants to lose weight | Tried to lose weight | Sought health professional | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| AOR | 95% CI | P | AOR | 95% CI | P | AOR | 95% CI | P | AOR | 95% CI | P | |
| BMI at examination a, b | 2.94 | 2.17‐3.99 | 0.000 | 2.20 | 1.39‐3.51 | 0.001 | 1.12 | 1.03‐1.23 | 0.010 | 1.06 | 0.93‐1.20 | 0.403 |
| BMI at 25 a, c | 0.73 | 0.63‐0.84 | 0.000 | 0.68 | 0.50‐0.91 | 0.011 | 1.13 | 1.05‐1.23 | 0.003 | 0.97 | 0.86‐1.10 | 0.655 |
| Age d | 0.95 | 0.80‐1.12 | 0.530 | 0.74 | 0.50‐1.10 | 0.140 | 0.94 | 0.85‐1.05 | 0.286 | 0.78 | 0.64‐0.95 | 0.014 |
| Male | 0.44 | 0.34‐0.57 | 0.000 | 0.76 | 0.48‐1.19 | 0.227 | 0.59 | 0.49‐0.72 | 0.000 | 0.61 | 0.45‐0.81 | 0.001 |
| Insurance e | 1.24 | 0.87‐1.77 | 0.221 | 1.64 | 0.88‐3.04 | 0.117 | 1.25 | 1.03‐1.52 | 0.027 | 2.15 | 1.36‐3.40 | 0.001 |
| Education | ||||||||||||
| Less than high school | 1.00 | — | — | 1.00 | — | — | 1.00 | — | — | 1.00 | — | — |
| High school or equivalent f | 2.52 | 1.73‐3.67 | 0.000 | 1.01 | 0.42‐2.41 | 0.989 | 1.12 | 0.87‐1.44 | 0.385 | 1.19 | 0.72‐1.99 | 0.489 |
| More than high school | 2.69 | 1.96‐3.70 | 0.000 | 1.68 | 0.67‐4.25 | 0.267 | 1.88 | 1.49‐2.37 | 0.000 | 1.83 | 1.17‐2.88 | 0.009 |
| Diabetes e | 1.47 | 1.03‐2.09 | 0.034 | 1.16 | 0.45‐2.97 | 0.752 | 1.60 | 1.19‐2.14 | 0.002 | 1.74 | 1.12‐2.71 | 0.015 |
| Arthritis e | 1.08 | 0.75‐1.57 | 0.668 | 3.21 | 1.40‐7.39 | 0.007 | 1.28 | 1.04‐1.56 | 0.018 | 1.19 | 0.84‐1.68 | 0.316 |
| Physical difficulty g | 1.18 | 0.70‐1.97 | 0.527 | 1.03 | 0.21‐5.13 | 0.970 | 0.70 | 0.56‐0.87 | 0.002 | 1.65 | 1.05‐2.59 | 0.030 |
| Race | ||||||||||||
| Non‐Hispanic white | 1.00 | — | — | 1.00 | — | — | 1.00 | — | — | 1.00 | — | — |
| Non‐Hispanic black | 0.30 | 0.22‐0.42 | 0.000 | 0.66 | 0.35‐1.26 | 0.208 | 1.20 | 0.97‐1.48 | 0.097 | 1.12 | 0.88‐1.43 | 0.343 |
| Hispanic | 0.75 | 0.50‐1.14 | 0.176 | 0.90 | 0.44‐1.86 | 0.778 | 1.28 | 1.00‐1.64 | 0.048 | 0.89 | 0.62‐1.28 | 0.529 |
| Other | 0.55 | 0.29‐1.07 | 0.079 | 1.22 | 0.26‐5.79 | 0.798 | 1.32 | 0.87‐2.02 | 0.186 | 0.88 | 0.50‐1.54 | 0.641 |
| Survey year | ||||||||||||
| 2005‐2006 | 1.00 | — | — | 1.00 | — | — | 1.00 | — | — | 1.00 | — | — |
| 2007‐2008 | 0.53 | 0.34‐0.81 | 0.004 | 0.81 | 0.31‐2.14 | 0.666 | 0.74 | 0.61‐0.89 | 0.002 | 0.94 | 0.63‐1.42 | 0.781 |
| 2009‐2010 | 0.60 | 0.39‐0.94 | 0.025 | 1.09 | 0.41‐2.87 | 0.866 | 0.74 | 0.57‐0.95 | 0.020 | 0.78 | 0.52‐1.17 | 0.230 |
| 2011‐2012 | 0.54 | 0.30‐0.95 | 0.034 | 0.68 | 0.28‐1.65 | 0.384 | 0.79 | 0.58‐1.08 | 0.134 | 0.90 | 0.64‐1.27 | 0.537 |
| Subpopulation (n) | 4,585 | 4,170 | 4,093 | 2,756 | ||||||||
Multivariable AORs estimated using continuation ratio logit model with coefficients freely varying across stages. Analysis incorporated sample weights and accounted for complex design of NHANES.
BMI at examination and BMI at 25 effect sizes scaled for 5‐kg/m2 units.
BMI at examination calculated with measured height and weight.
BMI at 25 calculated with measured height and recalled weight at age 25.
Age effect size scaled for 10‐y unit.
Self‐reported diabetes, arthritis, and insurance status.
High school or equivalent includes GED.
Physical difficulty included 6 measures of physical function indicated by difficulty walking a quarter of a mile; walking up 10 steps; stooping, crouching, or kneeling; lifting or carrying 10 lb; walking between rooms on the same floor; or standing up from an armless chair.
AOR, adjusted odds ratio; GED, general equivalency diploma; NHANES, National Health and Nutrition Examination Survey.
BMI at examination and at age 25 showed similar patterns of association at the next stage of the cascade, desiring to lose weight. With respect to trying to lose weight, males had 0.59 times the odds (95% CI: 0.49‐0.72) compared to females; and compared to those without insurance, individuals with insurance had 1.25 times the odds (95% CI: 1.03‐1.52). Furthermore, we found that those with insurance had particularly high odds of seeking a health professional, with 2.15 times the odds (95% CI: 1.36‐3.40).
Coefficients for BMI at examination, BMI at age 25, race/ethnicity, and physical difficulty varied significantly across stages of the cascade (Supporting Information Table S2).
Discussion
Medical management of obesity through behavioral modification alone or in combination with pharmacotherapy or weight loss surgery can result in reductions in rates of complications among people with obesity (2). However, the uptake of medical interventions remains low. In this study, we developed a cascade model to quantify engagement with obesity care in the US adult population and to identify points along the continuum responsible for the greatest losses in care. Our results indicate that, in total, 96% of adults with obesity in the US are not accessing adequate obesity care. Although the percentage of adults living with obesity with unmet needs varied, rates were uniformly high across all groups examined.
Disengagement was most pronounced in the transitions from trying to lose weight to seeking help from a health care professional for obesity and from seeking help from a health care professional to seeking help from a physician specifically. Inaccurate weight perceptions and disengagement between desired and attempted weight loss also contributed. In regression, we observed that those with obesity‐related comorbidities were more likely to seek help from health professionals to lose weight, as were those with insurance.
Other factors apart from those investigated in the current study may explain the disengagement observed in step 1 and the transition from step 2 to 3 of the cascade. First, studies suggest that cultural norms toward what constitutes a normal body weight may have shifted over time 5. This finding is consistent with recent data showing declines in perception of overweight and in attempts to lose weight, even as the prevalence of overweight has continued to increase 6, 7.
Second, some estimates of the association between obesity and mortality have found little or no excess risk, which may result in fewer people with obesity attempting to lose weight. Finally, the increasing prominence of the “health at every size” movement, which emphasizes nutrition and physical activity over weight status, may explain disengagement at these stages.
Further disengagement was also observed at stages 4 and 5. This loss may be explained by several factors, including weight‐related stigma 8, patient misperceptions about effectiveness and safety of obesity pharmacotherapy and weight loss surgery or lack of understanding of eligibility requirements for these interventions 1, 9, lack of insurance coverage, and limited reimbursement for treatment of obesity by insurance providers 10. An analysis of state essential health benefit plans in 2012 showed that many states' benchmark plans did not include coverage of weight loss surgery and that few covered weight loss programs 11. The situation has evolved in recent years, with the expansion of insurance coverage, increased access to obesity screening, counseling, and referral under the Affordable Care Act mandate 12, and recent guidelines recognizing obesity as a disease 13. However, although the Affordable Care Act requires all health plans to cover diagnostic screening and counseling for obesity, it does not guarantee access to effective treatment for obesity.
This study had several limitations. Although the current analysis defined seeking care from a physician for obesity as the final stage of the care cascade, this step may be necessary but not sufficient for adequate diagnosis, counseling, and referral for obesity‐related treatment services. Studies suggest that obesity is underdiagnosed in primary practice and that many patients with obesity may not receive adequate counseling and treatment for weight management 14, 15. Increasing access and use of obesity‐related treatments will likely involve addressing provider beliefs, attitudes, and perceptions toward screening, diagnosis, and treatment of obesity 16.
Through a cascade model, we quantified engagement with obesity care in the US and the most common points along the cascade at which disengagement occurred. Our finding that few individuals with obesity make it to the end of the cascade suggests that there is significant unmet need for obesity care at the population level. Engaging with this last step is essential to gaining access to managed, effective care and can result in a myriad of treatment outcomes, including behavioral modification, pharmacotherapy, bariatric surgery, and/or referral to another care provider 17, 18, 19, 20, 21. Our findings thus highlight the need for physicians to engage in conversation about obesity treatment at routine clinical visits, even when patients are not seeking obesity care. The results also suggest that meaningful efforts aimed at increasing engagement across stages of the cascade could greatly improve access to effective medical treatment options for those with obesity.
Supporting information
Supporting Information 1
Acknowledgments
We thank Professor Rich Feeley, JD, at the Boston University School of Public Health for his valuable input.
Funding agencies: This research was funded by Ethicon, Inc. (a Johnson & Johnson Company).
Disclosure: AS has received research funding from Ethicon, Inc. BFG, CWH, and RFS are employees of Ethicon, Inc.; SSJ and EMA are employees of Johnson & Johnson. BFG, CWH, SSJ, and RFS are stockholders of Johnson & Johnson. CT is an employee of Janssen Research & Development. JMC and KMB declare no conflict of interest.
References
- 1. Wadden TA, Webb VL, Moran CH, Bailer BA. Lifestyle modification for obesity: new developments in diet, physical activity, and behavior therapy. Circulation 2012;125:1157‐1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Moyer V; US Preventive Services Task Force. Screening for and management of obesity in adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med 2012;157:373‐378. [DOI] [PubMed] [Google Scholar]
- 3. Bray GA, Ryan DH. Update on obesity pharmacotherapy. Ann N Y Acad Sci 2014;1311:1‐13. [DOI] [PubMed] [Google Scholar]
- 4. US Department of Health and Human Services . Healthy People 2020 topics and objectives. http://healthypeople.gov/2020/topicsobjectives2020/. Updated March 19, 2018. Accessed October 2, 2017.
- 5. Robinson E, Christiansen P. The changing face of obesity: exposure to and acceptance of obesity. Obesity (Silver Spring) 2014;22:1380‐1386. [DOI] [PubMed] [Google Scholar]
- 6. Snook KR, Hansen AR, Duke CH, Finch KC, Hackney AA, Zhang J. Change in percentages of adults with overweight or obesity trying to lose weight, 1988‐2014. JAMA 2017;317:971‐973. [DOI] [PubMed] [Google Scholar]
- 7. Swift A. Fewer Americans in this decade want to lose weight. Gallup. http://news.gallup.com/poll/198074/fewer-americans-lose-weight-past-decade.aspx. Published November 22, 2016. Accessed October 2, 2017.
- 8. Puhl RM, Brownell KD. Confronting and coping with weight stigma: an investigation of overweight and obese adults. Obesity (Silver Spring) 2006;14:1802‐1815. [DOI] [PubMed] [Google Scholar]
- 9. Afonso BB, Rosenthal R, Li KM, Zapatier J, Szomstein S. Perceived barriers to bariatric surgery among morbidly obese patients. Surg Obes Relat Dis 2010;6:16‐21. [DOI] [PubMed] [Google Scholar]
- 10. Lee JS, Sheer JLO, Lopez N, Rosenbaum S. Coverage of obesity treatment: a state‐by‐state analysis of Medicaid and state insurance laws. Public Health Rep 2010;125:596‐604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Gallagher C; Obesity Care Continuum. OCC health policy memo: summary of state benchmark plan coverage of obesity treatment services. http://www.obesityaction.org/wp-content/uploads/1212-OCC-Summary-of-Obesity-Treatment-State-Benchmark-Plan-Coverage.pdf. Published December 4, 2012. Accessed October 2, 2017.
- 12. Wang YC, Pamplin J, Long MW, Ward ZJ, Gortmaker SL, Andreyeva T. Severe obesity in adults cost state Medicaid programs nearly $8 billion in 2013. Health Aff 2015;34:1923‐1931. [DOI] [PubMed] [Google Scholar]
- 13.American Medical Association House of Delegates. Resolution 420 (A‐13). Recognition of Obesity as a Disease. https://www.npr.org/documents/2013/jun/ama-resolution-obesity.pdf
- 14. Rose S, Poynter P, Anderson J, Noar S, Conigliaro J. Physician weight loss advice and patient weight loss behavior change: a literature review and meta‐analysis of survey data. Int J Obes (Lond) 2013;37:118‐128. [DOI] [PubMed] [Google Scholar]
- 15. Turner M, Jannah N, Kahan S, Gallagher C, Dietz W. Current knowledge of obesity treatment guidelines by health care professionals. Obesity (Silver Spring) 2018;26:665–671. [DOI] [PubMed] [Google Scholar]
- 16. Stunkard A, McLaren‐Hume M. The results of treatment for obesity. AMA Arch Intern Med 1959;103:79‐85. [DOI] [PubMed] [Google Scholar]
- 17. Tsai AG, Wadden TA. Treatment of obesity in primary care practice in the United States: a systematic review. J Gen Intern Med 2009;24:1073‐1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Jay M, Gillespie CC, Schlair S, Sherman S, Kalet AL. Physicians' use of the 5As in counseling obese patients: is the quality of counseling associated with patients' motivation and intention to lose weight? BMC Health Serv Res 2010;10:159. doi: 10.1186/1472-0000-0000-0000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Huang J, Yu H, Marin E, Brock S, Carden D, Davis T. Physicians' weight loss counseling in two public hospital primary care clinics. Acad Med 2004;79:156‐161. [DOI] [PubMed] [Google Scholar]
- 20. Greiner KA, Born W, Hall S, Hou Q, Kimminau KS, Ahluwalia JS. Discussing weight with obese primary care patients: physician and patient perceptions. J Gen Intern Med 2008;23:581‐587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Massetti GM, Dietz WH, Richardson LC. Excessive weight gain, obesity, and cancer: opportunities for clinical intervention. JAMA 2017;318:1975‐1976. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting Information 1


