Abstract
Background:
Few large multicity studies have been conducted in developing countries to address the acute health effects of atmospheric ozone pollution.
Objective:
We explored the associations between ozone and daily cause-specific mortality in China.
Methods:
We performed a nationwide time-series analysis in 272 representative Chinese cities between 2013 and 2015. We used distributed lag models and over-dispersed generalized linear models to estimate the cumulative effects of ozone (lagged over 0–3 d) on mortality in each city, and we used hierarchical Bayesian models to combine the city-specific estimates. Regional, seasonal, and demographic heterogeneity were evaluated by meta-regression.
Results:
At the national-average level, a increase in 8-h maximum ozone concentration was associated with 0.24% [95% posterior interval (PI): 0.13%, 0.35%], 0.27% (95% PI: 0.10%, 0.44%), 0.60% (95% PI: 0.08%, 1.11%), 0.24% (95% PI: 0.02%, 0.46%), and 0.29% (95% PI: 0.07%, 0.50%) higher daily mortality from all nonaccidental causes, cardiovascular diseases, hypertension, coronary diseases, and stroke, respectively. Associations between ozone and daily mortality due to respiratory and chronic obstructive pulmonary disease specifically were positive but imprecise and nonsignificant. There were no statistically significant differences in associations between ozone and nonaccidental mortality according to region, season, age, sex, or educational attainment.
Conclusions:
Our findings provide robust evidence of higher nonaccidental and cardiovascular mortality in association with short-term exposure to ambient ozone in China. https://doi.org/10.1289/EHP1849
Introduction
Ambient air pollution has emerged as a major public health concern worldwide (Cohen et al. 2017). As a key component of the photochemical air pollution mixture, tropospheric ozone is widely considered one of the most important air pollutants (Bell et al. 2004). A large body of epidemiological studies has shown that short-term exposure to air pollution could lead to increased mortality and morbidity, but there is far less evidence on ozone than on particulate matter, and the exisiting evidence is more inconsistent (Atkinson et al. 2014; Bell et al. 2005; Dominici et al. 2006; Pope and Dockery 2006). Interpretation of the epidemiological evidence on ozone was also constrained by a limited range of study sites, by variability in population susceptibility, and by the different statistical methods used to adjust for the confounding effects of concomitant exposures (temperature, particulate matter, etc.). Furthermore, few investigations have provided estimates on cause-specific cardiorespiratory mortality and on the potential effect modifications (Bell and Dominici 2008; Halonen et al. 2010).
Several large multicity studies have evaluated associations between ozone and daily mortality in North America, Europe, and some developed Asian cities (Bell et al. 2004, 2005; Gryparis et al. 2004; Ng et al. 2013; Peng et al. 2013; Wong et al. 2008), but these associations have been investigated in only a small number of cities in developing countries where ozone pollution has become increasingly severe in recent years owing to the rapid growth of urbanization (Anenberg et al. 2010; Bell et al. 2005; Chen et al. 2014; Yan et al. 2013). The lack of evidence in developing countries was mainly driven by the scarce monitoring data on ozone. Ozone was gradually introduced into China’s national air quality monitoring network beginning in January 2013, and its real-time monitoring data were publicly available in Chinese cities by the end of 2015.
We performed a nationwide study to evaluate the day-to-day associations between ozone and cause-specific mortality at both national and regional levels. In this study, we further evaluated whether the associations were changed by concomitant exposure to other air pollutants and how the associations varied by regional, seasonal, and demographic characteristics.
Methods
Data Collection
This analysis was based on daily air pollutant concentrations, weather conditions, and cause-specific mortality counts in 272 Chinese cities from 2013 to 2015, which have been described elsewhere (Chen et al. 2017). The 272 cities were selected because we could obtain daily data on ozone, mortality () nonaccidental deaths per day on average), and weather parameters. They included 69 cities with 3-y data, 74 cities with 2-y data, and 129 cities with 1-y data. The cities are dispersed over all 31 provincial administrative regions and include a population of nearly 290 million, accounting for approximately 20% of the total population of mainland China. These cities were classified into four regions according to the common regional divisions in terms of geography, climate, and culture in China (see Figure S1): Northwest (), North (), South () and Qing-Tibet (). In brief, the Northwest region is an arid area composed of plateaus, basins, deserts, and meadows; the Qing-Tibet region overlaps the Qinghai-Tibet Plateau, the world’s highest plateau; and the North and South regions are populous with apparent differences in climatic and cultural characteristics.
The daily mortality counts for each city were obtained from China’s Disease Surveillance Points System (DSPS), which has been shown to have good national and provincial representativeness (Liu et al. 2016). The DSPS randomly selected several districts or communities within a city. Detailed descriptions of the sampling and development of the DSPS have been published elsewhere (Liu et al. 2016; Yang et al. 2005). According to the International Classification of Diseases, 10th revision (ICD-10, WHO 2016), daily mortality counts in each city were further categorized into total nonaccidental causes (total, codes: A00–R99), cardiovascular diseases (CVD, codes: I00–I99), hypertension (codes: I10–I15), coronary heart disease (CHD, codes: I20–I25), stroke (codes: I60–I69), respiratory diseases (codes: J00–J98), and chronic obstructive pulmonary disease (COPD, codes: J41–J44). Finally, we divided daily deaths into several strata by age ranges (5–64 y, 65–74 y, and ), sex, and educational attainment (low: ; high: ).
Daily ozone data were derived from China’s National Urban Air Quality Real-time Publishing Platform (http://106.37.208.233:20035/). We calculated maximum 8-h mean concentrations of ozone, which was typically measured from 1000 hours to 1800 hours. To allow adjustment for the simultaneous exposure to copollutants, we also collected daily 24-h average concentrations of particulate matter with an aerodynamic diameter (), sulfur dioxide (), nitrogen dioxide (), carbon monoxide (), and nitrogen dioxide (). Through 2015, a total of 1,265 monitors were included in the present study; however, the number varied appreciably in each city, with a median of 4 (minimum: 1, maximum: 17). To calculate daily 8-h or 24-h mean concentrations, of the 1-h values must have been available on that particular day; otherwise, the entire station was excluded. We then averaged the measurements from all valid monitoring sites in a city. We obtained daily mean temperature and mean relative humidity in each city from the China Meteorological Data Sharing Service System (http://data.cma.cn/). More information about data sources for cause-specific deaths, air pollutants, and weather conditions is available in our previous publication (Chen et al. 2017). Our study protocol was approved by the Institutional Review Board at the School of Public Health, Fudan University (No. 2014-07-0523), with a waiver of informed consent because all data were aggregated at city level, and no subjects were contacted.
Statistical Analysis
Daily mortality counts, ozone concentrations, and weather parameters were linked by date in each city. A two-stage Bayesian hierarchical model was applied to obtain regional- and national-average associations between ozone and cause-specific mortality (Dominici et al. 2006).
In the first stage, the associations in each city were estimated using over-dispersed generalized linear models (GLM). The polynomial distributed lag model (PDLM) was selected a priori for ozone in our main analyses because it can account for collinearity between different lag days and is, in principle, more appropriate than single-day lags and averaging-day lags for exploring the cumulative health risks of an exogenous exposure (Gasparrini 2011). Linear models were used in the present analysis because most previous studies hypothesized linear associations between ozone and adverse health outcomes (Bell et al. 2004; Gryparis et al. 2004; Halonen et al. 2010; Peng et al. 2013). A maximum lag of 3 d in the PDLM (PDLM 0–3) was selected a priori in main analyses because previous studies have reported that associations between adverse health outcomes and short-term air pollutant exposures (including ozone) were limited to exposures on the present day and the previous 3 d (Bell et al. 2004, 2005; Samoli et al. 2009). However, we also considered other lag structures, including single-day lags [same day (lag 0) or 1, 2, or 3 d prior (lag 1–lag 3)], exposures averaged over multiple lag days (lag 0–1, 0–2, and 0–3), and PDLM estimates for cumulative exposures over the same day and 3, 6, or 9 d prior (PDLM 0–3, 0–6, and 0–9, respectively).
Several covariates were incorporated in the main GLM: a) a natural cubic spline smooth function of calendar day with 7 degrees of freedom (df) per year to exclude seasonality in mortality; b) a factor variable for “day of week” to exclude possible variations of mortality within a week; c) a cross-basis function of temperature built by the distributed lag nonlinear model (DLNM) to control for its potentially nonlinear and lagged confounding effects; and d) a natural smooth function with 3 df for the present-day relative humidity. In the DLNM of temperature, a cross-basis function was established by a natural cubic spline for the space of temperature with three internal knots at equally spaced temperature percentiles to account for the potentially nonlinear relationships between temperature and mortality. For the lags, we selected a natural cubic spline with two internal knots at equally spaced values of lags (plus intercept) to allow for more flexible lag effects at short delays (Guo et al. 2014). We selected a cumulative lag over the same day and 13 d prior for temperature in the DLNM (DLNM 0–13) according to previous epidemiological studies on ozone and temperature (Chen et al. 2017, 2014; Qin et al. 2017).
In the second stage, we used Bayesian hierarchical models to combine city-specific estimates for the associations between ozone and cause-specific mortality at national and regional levels. This approach has been widely used to pool risk estimates obtained from multiple locations while accounting for within-city statistical error and between-city variability (heterogeneity) of the true risks (Chen et al. 2012; Dominici et al. 2006; Peng et al. 2013). We reported the posterior mean percentage change and 95% posterior interval (PI) in daily mortality in association with a increase in ozone concentration (Dominici et al. 2006). The 95% PI is the Bayesian formulation of the 95% confidence interval (CI). We also calculated statistics and p-values for the between-city heterogeneity in random-effect models.
Using the model parameters from the main analyses, we further conducted several subgroup analyses on potential effect modification by geographical (four typical regions), seasonal (warm period, from May through October; cool period, from November through April), and demographic (age, sex, and education) factors. First, we used Bayesian hierarchical models to separately estimate the mortality effects of ozone within each subgroup (defined by region, age, sex, or educational attainment). Next, we derived p-values for differences among subgroups based on likelihood ratio tests comparing the fit of a meta-regression model with the potential modifier to the simple meta-analysis model. In addition, for cities with of data (), we evaluated effect modification by season (cool or warm) within each region (Northwest, North, or South) using a meta-regression model with season, region (two indicator terms for North vs. Northwest and South vs. Northwest), and interaction terms. The Qing-Tibet region was excluded from this analysis because of insufficient data. Finally, we evaluated effect modification of the associations between ozone and daily mortality (total nonaccidental, CVD, and respiratory) by annual-mean daily temperatures, concentrations, and ozone concentrations in each city using meta-regression models.
Finally, based on the main models, we performed three sensitivity analyses to assess the robustness of our estimates for the associations between ozone and daily total mortality. First, we fitted two-pollutant models with adjustment for the concomitant exposure to , , , and , which were introduced by using the same PDLMs as those used for ozone. Second, we controlled for confounding by temperature using alternative lag structures, including parallel lags of temperature on the same day and averaging lags over 1–3 d (abbreviated as “lag 0 and 1–3”), DLNM 0–3, and DLNM 0–6. Third, we changed the degrees of freedom in the smoothness of time from 4 df to 8 df per year.
All analyses were conducted using R version 3.1.1 (R Foundation for Statistical Computing) with the stats package for fitting the GLM, the dlnm package for the PDLM and the DLNM, the tlnise package for the Bayesian hierarchical model, and the metafor package for meta-regression analyses. were considered statistically significant in all analyses, except for a false discovery rate (FDR) of in correcting for multiple testing on the between-season differences in each region.
Results
Descriptive Statistics
Table 1 summarizes the environmental and mortality data in 272 cities in China from 2013 to 2015. The annual-mean concentrations of ozone varied considerably, with an average of (ranging from to ) across all cities. In general, there were appreciable variations in concentrations of ozone and copollutants within each region and between regions (Table 1; see also Table S1). Ozone concentrations were higher during the warm period than during the cool period at both national and regional levels (see Table S2). There were two to three times more deaths in the North and South regions than in the Northwest and Qing-Tibet regions (see Table S1). On average per city, there were 16 deaths from total causes, eight from CVD, one from hypertension, three from CHD, four from stroke, two from respiratory diseases, and two from COPD. The climatic conditions also varied greatly in these cities.
Table 1.
Summary statistics of environment and health data in 272 Chinese cities, 2013–2015.
| Variable | Mean | SD | Min | P25 | P50 | P75 | Max |
|---|---|---|---|---|---|---|---|
| Ozone () | |||||||
| Nationwide | 77 | 14 | 36 | 68 | 77 | 87 | 113 |
| Northwest | 77 | 17 | 44 | 68 | 72 | 93 | 102 |
| North | 79 | 13 | 36 | 72 | 79 | 88 | 113 |
| South | 75 | 13 | 41 | 67 | 75 | 85 | 104 |
| Qing-Tibet | 76 | 26 | 45 | 59 | 80 | 96 | 99 |
| Daily deaths | |||||||
| Total | 16 | 16 | 3 | 7 | 12 | 20 | 165 |
| CVD | 8 | 7 | 1 | 3 | 6 | 10 | 65 |
| Hypertension | 1 | 1 | 0 | 0 | 0 | 1 | 7 |
| CHD | 3 | 3 | 0 | 1 | 2 | 3 | 28 |
| Stroke | 4 | 4 | 0 | 2 | 3 | 5 | 33 |
| RD | 2 | 3 | 0 | 1 | 1 | 3 | 34 |
| COPD | 2 | 2 | 0 | 0 | 1 | 2 | 29 |
| Weather conditions | |||||||
| Mean temperature (°C) | 15 | 5 | 12 | 16 | 18 | 25 | |
| Relative humidity (%) | 68 | 10 | 35 | 61 | 71 | 77 | 91 |
Note: CHD, coronary heart disease; COPD, chronic obstructive pulmonary disease; CVD, cardiovascular diseases; Max, maximum; Min, minimum; P, percentile; RD, respiratory disease; SD, standard deviation.
Regression Results
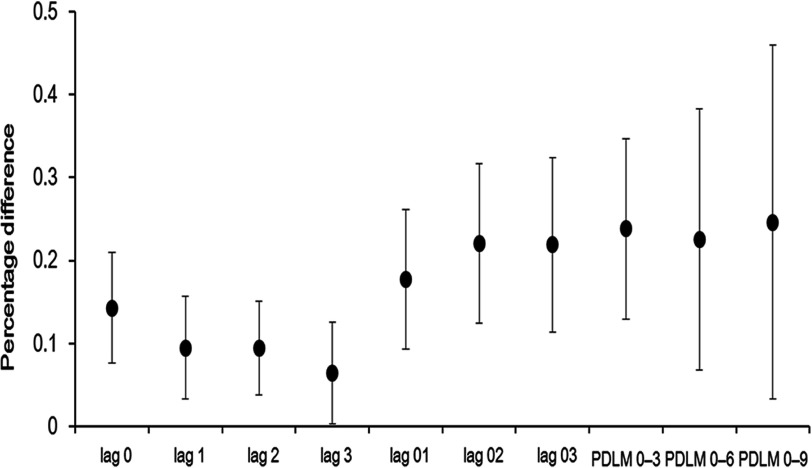
Figure 1 depicts the lag structures in national-average associations between ozone and daily total mortality. For single-day lags, the association was strongest for ozone exposure on the same day (lag 0) and weakest for exposure three days before death (lag 3). When exposures were lagged over multiple days, associations were stronger for exposures during the 0–2 d and 0–3 d lag periods than for the 0–1 d lag and were similar to the PDLM estimates for all three lag periods evaluated. Notably, the 95% PIs became much broader when the maximum lags were extended from 4 d (as in the main model) to 7 and 10 d. Based on the main model, we estimated that a increase in ozone (PDLM 0–3) was associated with a 0.24% (95% PI: 0.13, 0.35%) increase in daily total mortality.
Figure 1.
National-average percentage difference (posterior mean and 95% posterior intervals) in daily total mortality per increase in ozone concentration in 272 Chinese cities during single-day lags (lag 0, 1, 2, 3), multiple-day averaging lags (lag 0–1, 0–2, 0–3), and cumulative lags based on a polynomial distributed lag model (PDLM 0–3, 0–6, 0–9). Estimates were generated using over-dispersed generalized linear models adjusted for calendar day [natural cubic spline with 7 degrees of freedom (df)], day of the week, temperature (cross-basis function for temperature lagged for 0–13 d from distributed lag nonlinear model), and humidity (lag 0, natural smooth function, 3 df) to estimate city-specific associations that were combined using hierarchical Bayesian models.
Table 2 presents national average estimates for the associations between ozone concentrations and cause-specific mortality obtained using the main model. At the national level, the association with overall CVD mortality was slightly stronger than the association with total mortality. Associations with CHD and stroke mortality were similar to associations with overall CVD mortality, whereas the association with hypertension was stronger but less precise. Estimated percentage differences in daily mortality per increment in ozone (PDLM 0–3) were 0.27% (95% PI: 0.10%, 0.44%) for CVD, 0.60% (95% PI: 0.08%, 1.11%) for hypertension, 0.24% (95% PI: 0.02%, 0.46%) for CHD, and 0.29% (95% PI: 0.07%, 0.50%) for stroke. Associations with respiratory and COPD mortality were slightly weaker than the association with total mortality but were much less precise and were not statistically significant.
Table 2.
National- and regional-average percentage difference (posterior means and 95% posterior intervals) in daily cause-specific mortality per increase in ozone concentration in 272 Chinese cities.
| Regions | Total | CVD | Hypertension | CHD | Stroke | RD | COPD |
|---|---|---|---|---|---|---|---|
| Nationwide | 0.24 (0.13, 0.35) | 0.27 (0.10, 0.44) | 0.60 (0.08, 1.11) | 0.24 (0.02, 0.46) | 0.29 (0.07, 0.50) | 0.18 (, 0.47) | 0.20 (, 0.53) |
| North | 0.28 (0.06, 0.51) | 0.26 (0.01, 0.52) | 0.15 (, 1.03) | 0.13 (, 0.50) | 0.40 (0.09, 0.70) | 0.03 (, 0.62) | 0.15 (, 0.81) |
| South | 0.24 (0.09, 0.39) | 0.31 (0.09, 0.52) | 0.66 (0.02, 1.30) | 0.30 (0.04, 0.55) | 0.25 (0.02, 0.49) | 0.29 (, 0.63) | 0.27 (, 0.65) |
| Northwest | (, 1.28) | 0.36 (, 2.42) | 2.11 (, 6.90) | 2.40 (, 6.92) | 0.50 (, 2.84) | (, 3.91) | (, 2.72) |
| Qing-Tibet | 0.90 (, 3.93) | 1.47 (, 3.74) | 1.79 (, 6.90) | 1.85 (, 6.90) | 2.23 (, 6.10) | (, 2.68) | (, 2.65) |
Note: Estimates were generated using over-dispersed generalized linear models and polynomial distributed lag model for cumulative exposures over the same day and 3 days prior, adjusted for calendar day [natural cubic spline with 7 degrees of freedom (df)], day of the week, temperature (cross-basis function for temperature lagged for 0–13 days from distributed lag nonlinear model), and humidity (lag 0, natural smooth function, 3 df) to estimate city-specific associations that were combined using hierarchical Bayesian models. CHD, coronary heart disease; COPD, chronic obstructive pulmonary disease; CVD, cardiovascular diseases; RD, respiratory disease.
There was moderate between-city heterogeneity for total mortality () and CVD mortality (), and the heterogeneity for respiratory mortality was low (). Notably, the associations between ozone and various causes of mortality in the Northwest and Qing-Tibet regions of China were not statistically significant and had much broader 95% PIs than the other two regions (Table 2); however, there were no significant differences among regions according to the results of likelihood ratio tests, with p-values varying from 0.29 to 0.90 by cause of mortality. The meta-regression analysis showed greater effects of daily ozone concentrations on total mortality in cities with lower annual temperatures (). For each increment in daily ozone concentration, a city with lower annual-mean temperature would have an additional increase of 0.14% (95% CI: 0.02%, 0.25%) in daily total mortality. Annual-mean levels did not have a significant influence on associations between ozone and daily total mortality. For daily CVD mortality, only annual-mean had a significant effect of modification (), with a decrease leading to an additional increase of 0.11% (95% CI: 0.02%, 0.20%) in mortality per increment in daily ozone concentration. We did not conduct such an analysis for daily respiratory mortality because it was not statistically associated with ozone exposure.
In the meta-regression model with season, region, and the interaction term (Table 3), the associations in the North and South regions were stronger than those in the Northwest region, but differences by region were statistically nonsignificant ( and 0.09, respectively); although there were somewhat stronger associations in the cool period at the national-average level, the between-season differences were statistically nonsignificant (). In meta-regression models with season for each region, there were stronger associations in the warm season in the Northwest and North regions and weaker associations in the warm season in the South region, but all of these differences remained statistically nonsignificant after correcting for multiple testing (FDR from 0.08 to 0.79).
Table 3.
Estimated percentage difference (posterior means and 95% posterior intervals) in daily total mortality per increase in ozone concentration in 143 Chinese cities with of data, according to region and season.
| Region | All-year | p-Valuea | Cool season | Warm season | p-Value | FDRb |
|---|---|---|---|---|---|---|
| Nationwide | 0.23 (0.11, 0.34) | — | 0.43 (0.21, 0.65) | 0.20 (0.08, 0.31) | 0.13c | — |
| Northwest | 0.02 (, 1.91) | — | (, 2.51) | 0.69 (, 2.64) | 0.13b | 0.19 |
| North | 0.27 (0.03, 0.51) | 0.12 | 0.25 (, 0.68) | 0.39 (0.04, 0.75) | 0.79b | 0.79 |
| South | 0.21 (0.07, 0.35) | 0.09 | 0.51 (0.26, 0.76) | 0.13 (, 0.33) | 0.03b | 0.08 |
Note: Analysis excludes the Qing-Tibet region because few cities had of data. Estimates were generated using over-dispersed generalized linear models and polynomial distributed lag model for cumulative exposures over the same day and 3 days prior, adjusted for calendar day [natural cubic spline with 7 degrees of freedom (df)], day of the week, temperature (cross-basis function for temperature lagged for 0–13 days from distributed lag nonlinear model), and humidity (lag 0, natural smooth function, 3 df) to estimate city-specific associations that were combined using hierarchical Bayesian models. —, no comparison or the reference for comparisons; FDR, false discovery rate.
p-Values comparing effect estimates for the North and South regions to the Northwest (referent) region in meta-regression models with region, season (warm vs. cool), and interaction terms.
FDR or p-values comparing effect estimates for the warm versus cool seasons from separate meta-regression models stratified by region, with season as the predictor.
p-Value comparing effect estimates for the warm versus cool seasons over all cities in meta-regression models with region (two indicator terms for North vs. Northwest and South vs. Northwest), season, and interaction terms.
The association between ozone and total mortality also varied with demographic characteristics (Table 4). The effect estimates increased consecutively in the three age groups (5–64 y, 65–74 y, and ), but the differences were not significant based on the likelihood ratio test (). There were very similar estimates in males and females. The estimated percentage difference in total mortality with a increase in daily ozone was four times as high in less-educated people than in more-educated people, although the difference was not statistically significant (). Patterns of association with CVD mortality according to age, sex, and education were similar to those for total mortality, with statistically nonsignificant differences among subgroups (see Table S3).
Table 4.
National-average percentage differences (posterior means and 95% posterior intervals) in daily total mortality per increase in ozone concentration in 272 Chinese cities, classified by age, sex and educational attainment.
| Characteristic | Level | Estimates | p-Valuea |
|---|---|---|---|
| Age | 5–64 y | 0.13 (, 0.48) | 0.12 |
| 65–74 y | 0.19 (0.03, 0.34) | ||
| 0.42 (0.21, 0.64) | |||
| Sex | Male | 0.26 (0.13, 0.39) | 0.75 |
| Female | 0.21 (0.05, 0.36) | ||
| Education | 0.25 (0.14, 0.37) | 0.41 | |
| 0.06 (, 0.43) |
Note: Estimates were generated using over-dispersed generalized linear models and polynomial distributed lag model for cumulative exposures over the same day and 3 days prior, adjusted for calendar day [natural cubic spline with 7 degrees of freedom (df)], day of the week, temperature (cross-basis function for temperature lagged for 0–13 days from distributed lag nonlinear model), and humidity (lag 0, natural smooth function, 3 df) to estimate city-specific associations that were combined using hierarchical Bayesian models.
The p-values were calculated by performing a likelihood ratio test between the simple meta-analysis model (overall estimates) and a separate meta-regression model with a categorical variable (age, sex, or education).
In sensitivity analyses, the estimates for associations between ozone and daily total mortality were changed little by adjustment for concomitant exposure to or CO in two-pollutant models; they attenuated appreciably but remained statistically significant after controlling for or (see Figure S2). The use of alternative lag structures for temperature did not lead to obviously different estimates for the associations (see Figure S3). The estimates for daily total mortality per increase in ozone remained stable when the degrees of freedom per year varied from four to eight (see Figure S4).
Discussion
This multisite analysis in 272 representative Chinese cities had the advantage of analyzing national data using the same protocol and avoiding potential publication bias. It also provided a unique opportunity to explore effect modification by geographical, seasonal, and demographic characteristics. Another key advantage of this analysis was the use of distributed lag models in cumulating the mortality effects of ozone over several days (avoiding underestimates) as well as in controlling for the lagged and nonlinear effects of temperature (a strong confounder). Our estimates were also relatively robust to adjustment of concomitant exposure to copollutants (, , , and ).
This study estimated a 0.24% increase of daily total mortality per increase in ozone concentration, which was generally comparable to previous findings in meta-analyses and multicity studies (Bell et al. 2004, 2005; Peng et al. 2013; Tao et al. 2012; Wong et al. 2008). To allow for comparability when diverse metrics for ozone were adopted, previous estimates were converted based on a metric of per increase in maximum 8-h average concentration with a relationship of 20:15:8 for the 1-h maximum:8-h maximum:daily average. We assumed that to convert previous estimates into the same metric (Thurston and Ito 2001). For example, a recent multisite study of 21 cities in East Asia (Japan, South Korea, mainland China, Hong Kong, and Taiwan) indicated a 0.30% increase in total mortality (Chen et al. 2014). The Air Pollution and Health: A Combined European and North American Approach project estimated an overall 0.20% increment in total mortality based on a collaborative data set from 125 cities, but the values differed in the United States (0.23%), Canada (0.64%), and Europe (0.14%) (Peng et al. 2013). Investigators reported a 0.38% increase in total mortality in a multicity analysis (Bangkok, Hong Kong, Shanghai, and Wuhan) in the Public Health and Air Pollution in Asia project (Wong et al. 2008). A meta-analysis by Bell et al. (2005) summarized 144 effect estimates from 39 time-series studies worldwide and found that the estimate was 0.33% (95% CI: 0.28%, 0.60%).
We found stronger associations of ozone with CVD mortality than with total mortality, consistent with findings from most previous studies (Bell et al. 2005; Peng et al. 2013; Wong et al. 2008). Few previous studies have evaluated short-term associations between ozone exposure and mortality from hypertension and CHD. A previous meta-analysis estimated a 0.86% increase in stroke mortality per increase in ozone (Shah et al. 2015), which was considerably higher than our corresponding estimate (0.29%). The mechanisms behind the cardiovascular effects of ozone were somewhat biologically plausible. A number of studies have suggested appreciable changes in circulating biomarkers of inflammation, oxidative stress, coagulation, vasoreactivity, lipidology, and glucose metabolism after ozone exposure (Goodman et al. 2015). However, these results lack consistency and are of uncertain clinical relevance; hence, the exact mechanisms remain to be elucidated in further investigations (Goodman et al. 2015). For example, some human studies found that short-term exposure to ozone did not impair vascular function, elevate blood pressure, or affect heart rate variability in either direction (Barath et al. 2013; Hoffmann et al. 2012).
In line with many multicity studies and meta-analyses (Bell et al. 2005; Peng et al. 2013; Wong et al. 2008), we did not observe statistically significant associations between ozone and respiratory mortality. In contrast, some other studies found significant associations with respiratory mortality and morbidity (Ji et al. 2011; Kan et al. 2008; Zmirou et al. 1998). The inconsistent results in the respiratory system might be due to limitations of the time-series approach, different model specifications, location-dependent characteristics, or greater statistical uncertainty in relation to smaller numbers of respiratory deaths than CVD deaths (particularly in warm periods, when ozone concentrations are high).
We did not find significant effect modification by geographical region, but our ability to estimate associations for the Northwest and Qing-Tibet regions was limited by the small numbers of cities (21 and 4, respectively) and daily deaths in these areas. There were no significant differences according to demographic characteristics, although estimates suggested stronger associations in the oldest age group () and among those with less education. In the meta-regression analysis, we found evidence of a stronger association between ozone and daily mortality with a reduction in annual-mean temperature at the city level. Similarly, data from 98 U.S. cities included in the National Morbidity, Mortality, and Air Pollution Study (NMMAPS) indicated that the association between ozone and mortality was strongest in the northeast United States and stronger in association with lower temperatures (Bell and Dominici 2008). Aging and low educational attainment have been the two most commonly reported demographic characteristics to increase susceptibility to short-term ozone exposure in previous studies (Kan et al. 2008; Bell et al. 2014).
We found some evidence of seasonal variation in associations between ozone and daily mortality, although patterns appeared to vary by region, and differences by season within regions did not reach FDR significance. In the Northwest and North regions, the association was stronger during the warm period than during the cool period, consistent with findings from previous multicity studies in North America and western Europe as well as from a recent study in East Asia (Bell et al. 2005; Chen et al. 2014; Peng et al. 2013). Stronger associations during warm seasons might be explained by the following: a) Ozone concentrations were typically higher during the warm period; b) there was widespread use of household heating in northern China during the cool period, which reduced exposure to outdoor ozone because of restricted outdoor activities and reduced natural ventilation; and c) there were more pronounced synergistic effects with high temperatures during the summer (Bell and Dominici 2008; Li et al. 2017). In southern China, however, the association between ozone and mortality was stronger during the cool season than during the warm season, consistent with findings from previous Chinese studies even when extended lags of temperature were adjusted for (Chen et al. 2017; Kan et al. 2008; Qin et al. 2017; Tao et al. 2012). It has been suggested that this pattern might result from the reduced use of air conditioning, and the consequent exposure to more natural ventilation, during cool weather (Kan et al. 2008). A stronger association between ozone and mortality during cool versus warm seasons was also reported in the U.S. NMMAPS study (Chen et al. 2012).
Limitations should be noted when interpreting our results. First, exposure measurement errors would be inevitable because we used the average of measurements across various monitors in a city as the proxy of personal exposure, but such errors have been reported to lead to an underestimate of the effects (Zeger et al. 2000). Second, ecological bias was inherent in the time-series studies because all analyses were conducted on an aggregate level rather than on an individual level. Third, owing to limited availability of such data in China, we were unable to evaluate heterogeneity or effect modification caused by the use of air conditioning, by income, by urbanization, by transportation use, or by time spent outdoors or indoors.
Conclusion
In conclusion, using a large data set covering 272 cities throughout China, we found robust evidence of higher nonaccidental and cardiovascular mortality in association with short-term exposure to ambient ozone. Our results support previous evidence of acute effects of ozone on mortality in developing countries and are generally consistent with findings for populations in North America and Europe.
Supplemental Material
Acknowledgments
The study was supported by the National Natural Science Foundation of China (91643205), the Public Welfare Research Program of the National Health and Family Planning Commission of China (201502003), the Shanghai 3-Year Public Health Action Plan (GWTD2015S04 and 15GWZK0202), and the China Medical Board Collaborating Program (13-152).
References
- Anenberg SC, Horowitz LW, Tong DQ, West JJ. 2010. An estimate of the global burden of anthropogenic ozone and fine particulate matter on premature human mortality using atmospheric modeling. Environ Health Perspect 118(9):1189–1195, PMID: 20382579, 10.1289/ehp.0901220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atkinson RW, Kang S, Anderson HR, Mills IC, Walton HA. 2014. Epidemiological time series studies of PM2.5 and daily mortality and hospital admissions: a systematic review and meta-analysis. Thorax 69(7):660–665, PMID: 24706041, 10.1136/thoraxjnl-2013-204492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barath S, Langrish JP, Lundbäck M, Bosson JA, Goudie C, Newby DE, et al. 2013. Short-term exposure to ozone does not impair vascular function or affect heart rate variability in healthy young men. Toxicol Sci 135(2):292–299, PMID: 23872581, 10.1093/toxsci/kft157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell ML, Dominici F. 2008. Effect modification by community characteristics on the short-term effects of ozone exposure and mortality in 98 US communities. Am J Epidemiol 167(8):986–997, PMID: 18303005, 10.1093/aje/kwm396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell ML, Dominici F, Samet JM. 2005. A meta-analysis of time-series studies of ozone and mortality with comparison to the national morbidity, mortality, and air pollution study. Epidemiology 16(4):436–445, PMID: 15951661, 10.1097/01.ede.0000165817.40152.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell ML, McDermott A, Zeger SL, Samet JM, Dominici F. 2004. Ozone and short-term mortality in 95 US urban communities, 1987–2000. JAMA 292(19):2372–2378, PMID: 15547165, 10.1001/jama.292.19.2372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell ML, Zanobetti A, Dominici F. 2014. Who is more affected by ozone pollution? A systematic review and meta-analysis. Am J Epidemiol 180(1):15–28, PMID: 24872350, 10.1093/aje/kwu115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen C, Zhao B, Weschler CJ. 2012. Assessing the influence of indoor exposure to “outdoor ozone” on the relationship between ozone and short-term mortality in U.S. communities. Environ Health Perspect 120(2):235–240, PMID: 22100611, 10.1289/ehp.1103970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen K, Zhou L, Chen X, Bi J, Kinney PL. 2017. Acute effect of ozone exposure on daily mortality in seven cities of Jiangsu Province, China: no clear evidence for threshold. Environ Res 155:235–241, PMID: 28231551, 10.1016/j.envres.2017.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen R, Cai J, Meng X, Kim H, Honda Y, Guo YL, et al. 2014. Ozone and daily mortality rate in 21 cities of East Asia: how does season modify the association? Am J Epidemiol 180(7):729–736, PMID: 25139207, 10.1093/aje/kwu183. [DOI] [PubMed] [Google Scholar]
- Chen R, Kan H, Chen B, Huang W, Bai Z, Song G, et al. 2012. Association of particulate air pollution with daily mortality: the China Air Pollution and Health Effects Study. Am J Epidemiol 175(11):1173–1181, PMID: 22510278, 10.1093/aje/kwr425. [DOI] [PubMed] [Google Scholar]
- Chen R, Yin P, Meng X, Liu C, Wang L, Xu X, et al. 2017. Fine particulate air pollution and daily mortality: a nationwide analysis in 272 Chinese cities. Am J Respir Crit Care Med 196(1):73–81, PMID: 28248546, 10.1164/rccm.201609-1862OC. [DOI] [PubMed] [Google Scholar]
- Cohen AJ, Brauer M, Burnett R, Anderson HR, Frostad J, Estep K, et al. 2017. Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: an analysis of data from the Global Burden of Diseases Study 2015. Lancet 389(10082):1907–1918, PMID: 28408086, 10.1016/S0140-6736(17)30505-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dominici F, Peng RD, Bell ML, Pham L, McDermott A, Zeger SL, et al. 2006. Fine particulate air pollution and hospital admission for cardiovascular and respiratory diseases. JAMA 295(10):1127–1134, PMID: 16522832, 10.1001/jama.295.10.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gasparrini A. 2011. Distributed lag linear and non-linear models in R: the package dlnm. J Stat Softw 43(8):1–20, PMID: 22003319. [PMC free article] [PubMed] [Google Scholar]
- Goodman JE, Prueitt RL, Sax SN, Pizzurro DM, Lynch HN, Zu K, et al. 2015. Ozone exposure and systemic biomarkers: Evaluation of evidence for adverse cardiovascular health impacts. Crit Rev Toxicol 45(5):412–452, PMID: 25959700, 10.3109/10408444.2015.1031371. [DOI] [PubMed] [Google Scholar]
- Gryparis A, Forsberg B, Katsouyanni K, Analitis A, Touloumi G, Schwartz J, et al. 2004. Acute effects of ozone on mortality from the “Air Pollution and Health: A European Approach” project. Am J Respir Crit Care Med 170(10):1080–1087, PMID: 15282198, 10.1164/rccm.200403-333OC. [DOI] [PubMed] [Google Scholar]
- Guo Y, Gasparrini A, Armstrong B, Li S, Tawatsupa B, Tobias A, et al. 2014. Global variation in the effects of ambient temperature on mortality: A systematic evaluation. Epidemiology 25(6):781–789, PMID: 25166878, 10.1097/EDE.0000000000000165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halonen JI, Lanki T, Tiittanen P, Niemi JV, Loh M, Pekkanen J. 2010. Ozone and cause-specific cardiorespiratory morbidity and mortality. J Epidemiol Commun H 64(9):814–820, PMID: 19854743, 10.1136/jech.2009.087106. [DOI] [PubMed] [Google Scholar]
- Hoffmann B, Luttmann-Gibson H, Cohen A, Zanobetti A, de Souza C, Foley C, et al. 2012. Opposing effects of particle pollution, ozone, and ambient temperature on arterial blood pressure. Environ Health Perspect 120(2):241–246, PMID: 22020729, 10.1289/ehp.1103647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ji M, Cohan DS, Bell ML. 2011. Meta-analysis of the association between short-term exposure to ambient ozone and respiratory hospital admissions. Environ Res Lett 6(2):pii: 024006, PMID: 21779304, 10.1088/1748-9326/6/2/024006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kan H, London SJ, Chen G, Zhang Y, Song G, Zhao N, et al. 2008. Season, sex, age, and education as modifiers of the effects of outdoor air pollution on daily mortality in Shanghai, China: The Public Health and Air Pollution in Asia (PAPA) Study. Environ Health Perspect 116(9):1183–1188, PMID: 18795161, 10.1289/ehp.10851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J, Woodward A, Hou XY, Zhu T, Zhang J, Brown H, et al. 2017. Modification of the effects of air pollutants on mortality by temperature: a systematic review and meta-analysis. Sci Total Environ 575:1556–1570, PMID: 27780592, 10.1016/j.scitotenv.2016.10.070. [DOI] [PubMed] [Google Scholar]
- Liu S, Wu X, Lopez AD, Wang L, Cai Y, Page A, et al. 2016. An integrated national mortality surveillance system for death registration and mortality surveillance, China. Bull World Health Organ 94(1):46–57, PMID: 26769996, 10.2471/BLT.15.153148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ng CF, Ueda K, Nitta H, Takeuchi A. 2013. Seasonal variation in the acute effects of ozone on premature mortality among elderly Japanese. Environ Monit Assess 185(10):8767–8776, PMID: 23604788, 10.1007/s10661-013-3211-6. [DOI] [PubMed] [Google Scholar]
- Peng RD, Samoli E, Pham L, Dominici F, Touloumi G, Ramsay T, et al. 2013. Acute effects of ambient ozone on mortality in Europe and North America: results from the APHENA study. Air Qual Atmos Health 6(2):445–453, PMID: 23734168, 10.1007/s11869-012-0180-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pope CA III, Dockery DW. 2006. Health effects of fine particulate air pollution: lines that connect. J Air Waste Manag Assoc 56(6):709–742, PMID: 16805397, 10.1080/10473289.2006.10464485. [DOI] [PubMed] [Google Scholar]
- Qin LJ, Gu JQ, Liang SJ, Fang F, Bai WM, Liu X, et al. 2017. Seasonal association between ambient ozone and mortality in Zhengzhou, China. Int J Biometeorol 61(6):1003–1010, PMID: 27981338, 10.1007/s00484-016-1279-8. [DOI] [PubMed] [Google Scholar]
- Samoli E, Zanobetti A, Schwartz J, Atkinson R, LeTertre A, Schindler C, et al. 2009. The temporal pattern of mortality responses to ambient ozone in the APHEA project. J Epidemiol Community Health 63(12):960–966, PMID: 19648130, 10.1136/jech.2008.084012. [DOI] [PubMed] [Google Scholar]
- Shah AS, Lee KK, McAllister DA, Hunter A, Nair H, Whiteley W, et al. 2015. Short term exposure to air pollution and stroke: systematic review and meta-analysis. BMJ 350:h1295, PMID: 25810496, 10.1136/bmj.h1295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tao Y, Huang W, Huang X, Zhong L, Lu SE, Li Y, et al. 2012. Estimated acute effects of ambient ozone and nitrogen dioxide on mortality in the Pearl River Delta of southern China. Environ Health Perspect 120(3):393–398, PMID: 22157208, 10.1289/ehp.1103715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thurston GD, Ito K. 2001. Epidemiological studies of acute ozone exposures and mortality. J Expo Anal Environ Epidemiol 11(4):286–294, PMID: 11571608, 10.1038/sj.jea.7500169. [DOI] [PubMed] [Google Scholar]
- WHO (World Health Organization). 2016. International Statistical Classification of Diseases and Related Health Problems, 10th Revision. http://apps.who.int/classifications/icd10/browse/2016/en [accessed 1 February 2017].
- Wong CM, Vichit-Vadakan N, Kan H, Qian Z. 2008. Public health and air pollution in Asia (PAPA): a multicity study of short-term effects of air pollution on mortality. Environ Health Perspect 116(9):1195–1202, PMID: 18795163, 10.1289/ehp.11257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yan M, Liu Z, Liu X, Duan H, Li T. 2013. Meta-analysis of the Chinese studies of the association between ambient ozone and mortality. Chemosphere 93(6):899–905, PMID: 23786810, 10.1016/j.chemosphere.2013.05.040. [DOI] [PubMed] [Google Scholar]
- Yang G, Hu J, Rao KQ, Ma J, Rao C, Lopez AD. 2005. Mortality registration and surveillance in China: history, current situation and challenges. Popul Health Metr 3(1):3, PMID: 15769298, 10.1186/1478-7954-3-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeger SL, Thomas D, Dominici F, Samet JM, Schwartz J, Dockery D, et al. 2000. Exposure measurement error in time-series studies of air pollution: concepts and consequences. Environ Health Perspect 108(5):419–426, PMID: 10811568, 10.1289/ehp.00108419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zmirou D, Schwartz J, Saez M, Zanobetti A, Wojtyniak B, Touloumi G, et al. 1998. Time-series analysis of air pollution and cause-specific mortality. Epidemiology 9(5):495–503, PMID: 9730027, 10.1097/00001648-199809000-00005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.