Abstract
Background
Exercise-based cardiac rehabilitation (CR) is under-utilized. CR is indicated after heart transplantation, but there are no data regarding CR participation in transplant recipients. We characterized current CR utilization among heart transplant recipients in the United States and the association of CR with 1-year readmissions using the 2013–2014 Medicare files.
Methods
The study population included Medicare beneficiaries enrolled due to disability (patients on the transplant list are eligible for disability benefits under Medicare regulations) or age ≥65 years. We identified heart transplant patients by diagnosis codes and cumulative CR sessions occurring within 1 year after the transplant hospitalization.
Results
There were 2,531 heart transplant patients in the USA in 2013, of whom 595 (24%) received Medicare coverage and were included in the study. CR utilization was low, with 326 patients (55%) participating in CR programs. The Midwest had the highest proportion of transplant recipients initiating CR (68%, p = 0.001). Patients initiating CR attended a mean of 26.7 (standard deviation 13.3) sessions, less than the generally prescribed program of 36 sessions. Transplant recipients age 35 to 49 years were less likely to initiate CR (odds ratio [OR] 0.39, 95% confidence interval [CI] 0.23 to 0.66, < 0.001) and attended 8.2 fewer sessions (95% CI 3.5 to 12.9, p < 0.001) than patients age ≥ 65 years. CR participation was associated with a 29% lower 1-year readmission risk (95% CI 13% to 42%, p = 0.001).
Conclusions
Only half of cardiac transplant recipients participate in CR, and those who do have a lower 1-year readmission risk. These data invite further study on barriers to CR in this population.
Keywords: cardiac rehabilitation, cardiac transplantation, heart transplantation, rehabilitation, readmissions, health services research
Cardiac rehabilitation (CR), a program of prescribed exercise and risk factor modification, is recommended in patients undergoing heart transplantation as well as those with in ischemic heart disease and systolic heart failure.1,2 CR is associated with an approximate 25% decrease in mortality in patients with ischemic heart disease.3 Despite its known benefits, < 20% of these patients participate in CR programs.1,3–9 There are, however, no data on CR utilization after heart transplantation.
CR is clearly beneficial for heart transplant recipients.10–12 Exercise training after heart transplantation improves maximal oxygen consumption,13–15 peak heart rate,16 ventilatory capacity,14 autonomic function17 and quality of life.18,19 As such, CR programs offer a promising modality to improve outcomes during the months after transplantation.
Patients on the waiting list for heart transplantation in the USA are eligible for Medicare disability benefits upon reaching United Network of Organ Transplantation (UNOS) Status IA or IB.20 Therefore, we evaluated CR utilization after heart transplantation in the USA using Medicare data. We also characterized the association of CR with 1-year readmissions among heart transplant recipients. We hypothesized that CR is associated with a decreased risk of readmission in these patients.
Methods
Data source
We obtained data regarding CR utilization in heart transplant recipients in the USA from 2013–2014 and 2008–2009 Medicare 100% Limited Data Set (LDS) files from the Centers for Medicare & Medicaid Services (CMS). These files contain all inpatient and institutional outpatient claims for fee-for-service Medicare beneficiaries. For purposes of evaluating the generalizability of transplant recipients receiving Medicare coverage in 2013, we also obtained demographic characteristics of all heart transplant patients during that time period from the Organ Procurement and Transplantation Network national data report.21 The institutional review board of Vanderbilt University Medical Center approved the study, which was conducted under the terms of a data use agreement with CMS.
Patient population
The study population included Medicare beneficiaries enrolled in 2013 due to disability or age ≥ 65 years who were residing in the USA and who had uninterrupted fee-for-service coverage until their death or for 1 year after discharge. We used the same criteria for the 2008 cohort. Inclusion in the study was based on discharge diagnosis code (International Classification of Diseases, 9th Revision [ICD-9], Code 37.51) or procedure code (Current Procedure Terminology [CPT], Code 33945) for heart transplantation.
Outcomes
Participation in CR programs, defined as a binary variable (yes/no), was the primary outcome. We searched the Medicare outpatient LDS files for CR claims (CPT Codes 93797, 93798, G0422, G0423 or S9472) occurring within 1 year after the transplant hospitalization discharge date. Our secondary outcome examined CR as a continuous variable (number of sessions attended).
Additional secondary outcomes included: (1) the number of days between discharge from the transplant hospitalization and the first CR session, obtained from the Medicare files; and (2) the number of readmissions that occurred in the 1-year period after patients underwent transplantation, also obtained from the Medicare files. We specifically queried readmissions, not observation stays.
Other variables
We obtained demographic characteristics, including age, gender, race (black, white, other) and geographic census division (Midwest, Northeast, West and South), from the denominator file. We characterized the burden of comorbidities with Elixhauser comorbidity groups present during the index hospitalization, which were identified by ICD-9 codes as described previously.22
We determined whether patients had a ventricular assist device (VAD) before transplant by identifying ICD-9 (37.64) and CPT codes (33977, 33978, 33980) for VAD explantation during the transplant hospitalization. We also identified patients who were discharged to inpatient rehabilitation facilities (IRFs) or skilled nursing facilities (SNFs) after transplantation using the inpatient file. In addition, we determined whether the transplant hospital had a CR program from the American Hospital Association Annual Survey of Hospitals.23
Statistical analysis
Demographic and geographic characteristics of cardiac transplant recipients receiving Medicare coverage in 2013 were compared with all heart transplant patients using Pearson's chi-square tests. We used multivariable-adjusted logistic regression to evaluate the effect of individual covariates on CR initiation rates and linear regression to analyze predictors of the number of CR sessions attended. The Andersen–Gill model with a robust sandwich covariance estimate (also known as a proportional means model), a technique for the analysis of repeated events, was used to model the effect of participating in CR on 1-year readmission risk after adjusting for covariates.24,25 CR participation was used as a time-updated covariate such that all individuals in the sample were considered non-CR participants at baseline and remained so until beginning CR (Figure 1). For example, if an individual had no readmissions in the year after transplant and did not initiate CR until 3 months post-transplant, he or she would contribute 3 months of non-readmission time to the CR non-participant group and the remaining 9 months to the CR participant group. This approach, known as the Mantel–Byar method, was chosen to minimize immortal person-time bias.26–28
Figure 1.
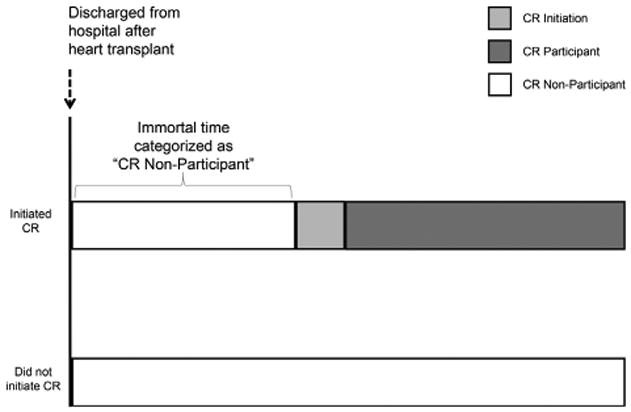
Person-time approach (Mantel–Byar method) to defining cardiac rehabilitation (CR) participation status in modeling the association of CR with readmissions. In CR participants, the time between hospital discharge and CR initiation (immortal person-time) is classified as CR non-participation until CR initiation and CR participation thereafter.
We used Pearson's chi-square tests to compare demographic and geographic characteristics of Medicare beneficiaries receiving heart transplants in the context of CR participation between 2008 and 2013. Comorbidities could not be directly compared between the 2008 and 2013 samples because the inpatient file version used in 2008 (Version I) has 10 fields for additional diagnoses, whereas the version used in 2013 (Version J) has 25 fields for additional diagnoses.
All analyses utilized SAS (version 9.4) and R (version 3.1.2) software.29,30
Results
Cohort derivation
According to the Organ Procurement and Transplantation Network, there were 2,531 heart transplants in 2013.21 A total of 696 (27%) of these patients received Medicare coverage. We excluded 61 patients who did not have uninterrupted fee-for-service Medicare coverage and 40 patients who died in the hospital or were participating in CR programs at the time of transplantation, resulting in a final sample size of 595 transplant recipients.
Comparison of all transplant recipients to those receiving Medicare
Compared with all transplant recipients in 2013 (N = 2,531), the cohort of transplant recipients with Medicare coverage (N = 595) was comprised of more patients age ≥65 years of age and fewer patients <35 years age, but with a similar proportion of patients 35 to 65 years of age (Table 1). There was a greater proportion of men (78% vs 70%, p < 0.001) in the Medicare cohort and a similar proportion of black transplant recipients. There was a slightly greater proportion of Medicare beneficiaries receiving transplants in the South as compared with all transplant patients (43% vs 37%, p = 0.02).
Table 1. Baseline Characteristics of Medicare Beneficiaries Receiving Heart Transplants in 2013 (N = 595).
| Characteristic | All transplants | Transplants Receiving Medicare | p-valuea | Medicare CR non-participants | Medicare CR participants | p-valuea |
|---|---|---|---|---|---|---|
| Total | 2,531 | 595 (24%) | 269 (45%) | 326 (55%) | NA | |
| Demographic | ||||||
| Age group (years) | <0.001 | 0.009 | ||||
| <35 | 643 (25%) | 34 (6%) | 20 (7%) | 14 (4%) | ||
| 35 to 49 | 435 (17%) | 95 (16%) | 55 (20%) | 40 (12%) | ||
| 50 to 64 | 1,007 (40%) | 227 (38%) | 98 (36%) | 129 (40%) | ||
| ≥65 | 446 (18%) | 239 (40%) | 96 (36%) | 143 (44%) | ||
| Gender | <0.001 | 0.86 | ||||
| Female | 770 (30%) | 133 (22%) | 61 (23%) | 72 (22%) | ||
| Male | 1,761 (70%) | 462 (78%) | 208 (77%) | 254 (78%) | ||
| Race | <0.001 | 0.37 | ||||
| White | 1,628 (64%) | 424 (71%) | 184 (68%) | 240 (74%) | ||
| Black | 559 (22%) | 124 (21%) | 62 (23%) | 62 (19%) | ||
| Other | 344 (14%) | 47 (8%) | 23 (9%) | 24 (7%) | ||
| Census region | 0.02 | 0.005 | ||||
| Midwest | 569 (22%) | 118 (20%) | 38 (14%) | 80 (25%) | ||
| Northeast | 500 (20%) | 121 (20%) | 65 (24%) | 56 (17%) | ||
| South | 928 (37%) | 253 (43%) | 122 (45%) | 131 (40%) | ||
| West | 534 (20%) | 103 (17%) | 44 (16%) | 59 (18%) | ||
| CR program at transplant hospital | NA | 584 (98%) | NA | 262 (97%) | 322 (99%) | 0.24 |
| Clinical | ||||||
| Previous VAD | NA | 237 (40%) | NA | 117 (43%) | 120 (37%) | 0.10 |
| Discharge to IRF or SNF | NA | 102 (17%) | NA | 58 (22%) | 44 (14%) | 0.009 |
| Chronic pulmonary disease | NA | 94 (16%) | NA | 38 (14%) | 56 (17%) | 0.31 |
| Coagulopathy | NA | 257 (43%) | NA | 116 (43%) | 141 (43%) | 0.97 |
| Deficiency anemia | NA | 137 (23%) | NA | 60 (22%) | 77 (24%) | 0.70 |
| Depression | NA | 83 (14%) | NA | 33 (12%) | 50 (15%) | 0.28 |
| Diabetes | NA | 236 (40%) | NA | 113 (42%) | 123 (38%) | 0.29 |
| Fluid and electrolyte disorders | NA | 363 (61%) | NA | 170 (63%) | 193 (59%) | 0.32 |
| Hypertension | NA | 312 (52%) | NA | 134 (50%) | 178 (55%) | 0.24 |
| Obesity | NA | 56 (9%) | NA | 27 (10%) | 29 (9%) | 0.64 |
| Peripheral vascular disease | NA | 39 (7%) | NA | 20 (7%) | 19 (6%) | 0.43 |
| Renal failure | NA | 252 (42%) | NA | 123 (46%) | 129 (40%) | 0.13 |
| Weight loss | NA | 81 (14%) | NA | 38 (14%) | 43 (13%) | 0.74 |
CR, cardiac rehabilitation; IRF, inpatient rehabilitation facility; NA, not available; SD, standard deviation; SNF, skilled nursing facility; VAD, ventricular assist device.
All p-values obtained using Pearson's chi-square test.
Cohort characteristics
CR utilization among Medicare beneficiaries receiving heart transplants was low, with 55% of eligible patients initiating CR (Table 1). Almost all patients in the study (98%) were transplanted at hospitals that reported having CR programs. The average age of the cohort was 58%, and 22% of transplant recipients were female. The majority of patients undergoing heart transplantation were white (71%), whereas 21% were black and 8% were categorized as another ethnicity, including Asian and Hispanic. Before transplantation, 40% of patients had ventricular assist devices (VADs). After transplantation, 17% of patients were discharged to inpatient rehabilitation facilities (IRFs) or skilled nursing facilities (SNFs).
CR utilization
CR initiation rates by demographic, geographic and clinical characteristics are displayed in Table 2. Patients in the Midwest census region had markedly higher odds of initiating CR (odds ratio [OR] 2.23, 95% confidence interval [CI] 1.37 to 3.63, p = 0.001) as compared with those in the South, after multivariable adjustment. The West census region was not significantly different from the South and there was a nonsignificant trend toward lower CR utilization in the Northeast. Younger transplant recipients were less likely to initiate CR than older patients (Table 2). Patients discharged to an IRF or SNF were also less likely to participate in CR (OR 0.58, 95% CI 0.36 to 0.94, p = 0.03). None of the comorbidities on admission, defined by Elixhauser comorbidity groups, were associated with the odds of attending CR.
Table 2. Predictors of Cardiac Rehabilitation Initiation Among Medicare Beneficiaries Receiving Heart Transplants in 2013 (N = 595).
| Participation in a CR programa | ||||
|---|---|---|---|---|
|
|
||||
| Characteristic | Proportion of patients initiating CR (%) | OR | 95% CI | p-value |
| All | 55% | |||
| Demographic | ||||
| Age group (years) | ||||
| <35 | 41% | 0.36 | 0.16 to 0.79 | 0.01 |
| 35 to 49 | 42% | 0.39 | 0.23 to 0.66 | o0.001 |
| 50 to 64 | 57% | 0.83 | 0.56 to 1.23 | 0.36 |
| ≤65 | 60% | Referent | ||
| Gender | ||||
| Female | 54% | 0.94 | 0.61 to 1.45 | 0.78 |
| Male | 55% | Referent | ||
| Race | ||||
| Black | 50% | 0.94 | 0.60 to 1.47 | 0.78 |
| Other | 51% | 1.03 | 0.53 to 2.01 | 0.92 |
| White | 57% | Referent | ||
| Census region | ||||
| Midwest | 68% | 2.23 | 1.37 to 3.63 | 0.001 |
| Northeast | 46% | 0.74 | 0.46 to 1.17 | 0.19 |
| West | 57% | 1.07 | 0.64 to 1.78 | 0.80 |
| South | 52% | Referent | ||
| Clinical | ||||
| Previous VAD | 51% | 0.79 | 0.55 to 1.12 | 0.18 |
| Discharge to IRF or SNF | 43% | 0.58 | 0.36 to 0.94 | 0.03 |
| Chronic pulmonary disease | 60% | 1.15 | 0.72 to 1.85 | 0.56 |
| Coagulopathy | 55% | 0.99 | 0.70 to 1.40 | 0.94 |
| Deficiency anemia | 56% | 1.05 | 0.70 to 1.59 | 0.81 |
| Depression | 60% | 1.30 | 0.78 to 2.15 | 0.31 |
| Diabetes | 52% | 0.83 | 0.57 to 1.19 | 0.30 |
| Fluid and electrolyte disorders | 53% | 0.82 | 0.57 to 1.17 | 0.27 |
| Hypertension | 57% | 1.29 | 0.90 to 1.84 | 0.16 |
| Obesity | 52% | 0.83 | 0.46 to 1.51 | 0.54 |
| Peripheral vascular disease | 49% | 0.69 | 0.35 to 1.40 | 0.30 |
| Renal failure | 51% | 0.76 | 0.53 to 1.10 | 0.14 |
| Weight loss | 53% | 1.10 | 0.65 to 1.84 | 0.73 |
CI, confidence interval; CR, cardiac rehabilitation; IRF, inpatient rehabilitation facility; OR, odds ratio; SNF, skilled nursing facility; VAD, ventricular assist device.
Adjusted for all listed variables.
Those patients who did initiate CR attended a mean of 26.7 ± 13.3 sessions, fewer than the generally prescribed program of 36 sessions (Table 3). Only 95 CR attendees (29%) participated in the full course of 36 sessions. Younger transplant patients attended far fewer sessions than older patients, with transplant recipients < 35 years old attending a mean of 16.0 ± 12.8 sessions as compared with 29.4 ± 12.1 sessions in those > 65 years old (p < 0.001). Women attended 4.3 (95% CI 0.7 to 7.9, p = 0.02) fewer sessions than men. Among CR participants, the average time between discharge and the first CR session was 71.0 (standard deviation 62.2) days, with a median of 54 (interquartile range 27 to 96) days.
Table 3. Predictors of Number of Sessions Attended Among Cardiac Rehabilitation Participants Receiving Heart Transplants and Medicare Coverage in 2013 (N = 326).
| Number of CR sessions attendeda | ||||
|---|---|---|---|---|
|
|
||||
| Characteristic | CR sessions among participants (mean ± SD) | Coefficient | 95% CI | p-value |
| All | 26.7 ± 13.3 | |||
| Demographic | ||||
| Age group (years) | ||||
| <35 | 16.0 ± 12.8 | −11.8 | −19.0, –4.6 | 0.001 |
| 35 to 49 | 21.2 ± 14.3 | −8.2 | −12.9, –3.5 | o0.001 |
| 50 to 64 | 26.5 ± 13.3 | −2.4 | −5.5, 0.8 | 0.15 |
| ≥65 | 29.4 ± 12.1 | Referent | ||
| Gender | ||||
| Female | 22.9 ± 12.7 | −4.3 | −7.9, –0.7 | 0.02 |
| Male | 27.7 ± 13.3 | Referent | ||
| Race | ||||
| Black | 22.0 ± 13.2 | −3.6 | −7.4, 0.3 | 0.07 |
| Other | 24.3 ± 12.5 | −1.1 | −6.8, 4.6 | 0.70 |
| White | 28.1 ± 13.1 | Referent | ||
| Census region | ||||
| Midwest | 28.3 ± 14.4 | 3.5 | −0.4, 7.4 | 0.07 |
| Northeast | 27.2 ± 12.0 | 0.9 | −3.3, 5.1 | 0.67 |
| West | 26.9 ± 12.1 | 0.02 | −4.2, 4.2 | 0.99 |
| South | 25.4 ± 13.7 | Referent | ||
| Clinical | ||||
| Previous VAD | 24.0 ± 13.8 | −4.5 | −7.5, –1.6 | 0.003 |
| Discharge to IRF or SNF | 29.2 ± 10.8 | 3.3 | −1.1, 7.7 | 0.14 |
| Chronic pulmonary disease | 26.3 ± 12.1 | −0.2 | −4.0, 3.6 | 0.92 |
| Coagulopathy | 25.8 ± 12.4 | −2.0 | −4.9, 0.9 | 0.17 |
| Deficiency anemia | 28.1 ± 10.9 | 1.6 | −1.8, 5.1 | 0.36 |
| Depression | 27.1 ± 13.0 | 0.2 | −3.8, 4.2 | 0.91 |
| Diabetes | 26.6 ± 13.4 | −0.8 | −3.9, 2.3 | 0.60 |
| Fluid and electrolyte disorders | 26.7 ± 13.5 | −1.3 | −4.3, 1.8 | 0.41 |
| Hypertension | 26.9 ± 13.2 | 0.03 | −2.9, 3.0 | 0.99 |
| Obesity | 28.4 ± 13.6 | 2.4 | −2.7, 7.5 | 0.35 |
| Peripheral vascular disease | 27.8 ± 10.0 | −0.2 | −6.4, 5.9 | 0.94 |
| Renal failure | 27.6 ± 12.4 | 0.9 | −2.1, 3.9 | 0.57 |
| Weight loss | 28.2 ± 14.9 | 0.9 | −3.6, 5.3 | 0.71 |
CI, confidence interval; CR, cardiac rehabilitation; SD, standard deviation; VAD, ventricular assist device; IRF, inpatient rehabilitation facility; SNF, skilled nursing facility.
Adjusted for all listed variables.
CR and readmissions
Readmissions within 1 year after transplantation were cumulated among Medicare beneficiaries receiving heart transplants. There were 953 total readmissions within 1 year of transplant in the cohort, with 391 patients (66%) admitted at least once during this time. After multivariable adjustment, participation in a CR program was associated with a 29% (95% CI 13% to 42%, p = 0.001) decrease in 1-year readmissions (Table 4). Patients discharged to an IRF or SNF had a significantly increased risk of being readmitted within 1 year after transplant (HR 1.40, 95% CI 1.13 to 1.74, p = 0.002). Female transplant recipients had a higher risk of readmission compared with men (HR 1.32, 95% CI 1.06 to 1.64, p = 0.01). Multivariable-adjusted cumulative readmissions over time for heart transplant recipients, stratified by CR participation, are shown in Figure 2. Readmission curves for CR participants and non-participants diverge within 90 days after discharge, with CR participants showing a lower rate of readmission throughout the 1-year follow-up period.
Table 4. Predictors of 1-year Readmission Risk Among Medicare Beneficiaries Receiving Heart Transplants in 2013 (N = 595).
| One-year readmission risk | |||
|---|---|---|---|
|
|
|||
| Characteristic | Hazard ratioa | 95% CI | p-value |
| CR participation | 0.71 | 0.58 to 0.87 | 0.001 |
| Age group (years) | |||
| <35 | 0.61 | 0.41 to 0.91 | 0.02 |
| 35 to 49 | 1.09 | 0.80 to 1.48 | 0.60 |
| 50 to 64 | 0.89 | 0.73 to 1.09 | 0.26 |
| ≥65 | Referent | ||
| Gender | |||
| Female | 1.32 | 1.06 to 1.64 | 0.01 |
| Male | Referent | ||
| Race | |||
| Black | 0.93 | 0.72 to 1.21 | 0.59 |
| Other | 0.97 | 0.68 to 1.37 | 0.86 |
| White | Referent | ||
| Census region | |||
| Midwest | 1.01 | 0.78 to 1.31 | 0.93 |
| Northeast | 0.95 | 0.75 to 1.19 | 0.64 |
| West | 0.73 | 0.54 to 0.99 | 0.04 |
| South | Referent | ||
| Clinical | |||
| Previous VAD | 0.91 | 0.75 to 1.09 | 0.30 |
| Discharge to IRF or SNF | 1.40 | 1.13 to 1.74 | 0.002 |
| Chronic pulmonary disease | 1.33 | 1.03 to 1.72 | 0.03 |
| Coagulopathy | 0.96 | 0.80 to 1.16 | 0.68 |
| Deficiency anemia | 1.08 | 0.86 to 1.35 | 0.52 |
| Depression | 1.12 | 0.85 to 1.48 | 0.42 |
| Diabetes | 1.11 | 0.91 to 1.35 | 0.30 |
| Fluid and electrolyte disorders | 0.94 | 0.78 to 1.14 | 0.55 |
| Hypertension | 0.80 | 0.66 to 0.97 | 0.02 |
| Obesity | 0.98 | 0.73 to 1.33 | 0.91 |
| Peripheral vascular disease | 0.91 | 0.66 to 1.26 | 0.58 |
| Renal failure | 1.05 | 0.87 to 1.26 | 0.64 |
| Weight loss | 1.00 | 0.78 to 1.28 | 0.99 |
CI, confidence interval; CR, cardiac rehabilitation; IRF, inpatient rehabilitation facility; SNF, skilled nursing facility; VAD, ventricular assist device.
Hazard ratios derived from the multivariable-adjusted AndersenGill model with robust sandwich covariance estimator (or proportional means model).
Figure 2.
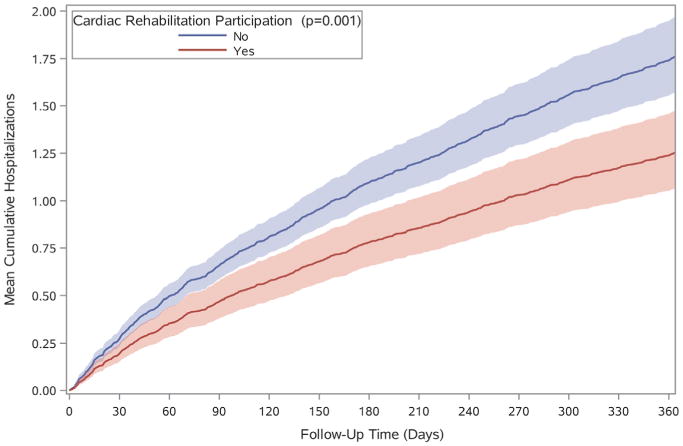
Cumulative readmissions over time for Medicare beneficiaries receiving heart transplants in 2013, stratified by participation in cardiac rehabilitation. Cumulative readmissions were calculated using the Andersen–Gill model with a robust sandwich covariance estimator adjusted for age, gender, race, census region, comorbidities, discharge to an inpatient rehabilitation facility or skilled nursing facility, and previous ventricular assist device. Shaded areas represent 95% confidence intervals.
Temporal trends in CR utilization
Temporal trends in CR participation among transplant recipients were analyzed by comparing patients in 2013 with patients undergoing transplantation 5 years earlier, in 2008 (Table 5). There were 2,163 heart transplants in 2008, of which 486 (22%) had Medicare coverage. Among Medicare beneficiaries receiving heart transplants in 2008, 205 (42%) participated in CR programs, a significantly lower percentage than in 2013 (55%, p < 0.001). CR participants attended a mean of 23.0 ±11.9 sessions in 2008, also significantly lower than in 2013 (p < 0.001). As in 2013, patients receiving transplants in 2008 were more likely to participate in CR if they were older and from the Midwest.
Table 5. Characteristics, Cardiac Rehabilitation Initiation Rates and Number of Sessions Attended Among Medicare Beneficiaries Receiving Heart Transplants in 2008 (N = 486).
| Characteristic | All transplants | CR non-participants | CR participants | CR initiation rate | p-valuea | Mean CR sessions among CR participants | p-valueb |
|---|---|---|---|---|---|---|---|
| All [n (%)] | 486 | 281 (58%) | 205 (42%) | 42% | 23.0 ± 11.9 | ||
| Demographic | |||||||
| Age group (years) | 0.63 | 0.002 | |||||
| <35 | 32 (7%) | 19 (7%) | 13 (6%) | 41% | 15.3 ± 11.7 | ||
| 35 to 49 | 80 (16%) | 50 (18%) | 30 (15%) | 38% | 17.3 ± 13.5 | ||
| 50 to 64 | 231 (48%) | 135 (48%) | 96 (47%) | 42% | 24.0 ± 11.6 | ||
| ≥65 | 143 (29%) | 77 (27%) | 66 (32%) | 46% | 25.6 ± 10.4 | ||
| Gender | 0.16 | 0.18 | |||||
| Female | 125 (26%) | 79 (28%) | 46 (22%) | 37% | 20.7 ± 13.1 | ||
| Male | 361 (74%) | 202 (72%) | 159 (78%) | 44% | 23.6 ± 11.5 | ||
| Race | 0.27 | 0.45 | |||||
| White | 350 (72%) | 195 (69%) | 155 (76%) | 44% | 23.6 ± 11.9 | ||
| Black | 91 (19%) | 56 (20%) | 35 (17%) | 38% | 21.6 ± 12.7 | ||
| Other | 45 (9%) | 30 (11%) | 15 (7%) | 33% | 20.1 ± 10.6 | ||
| Region | 0.004 | 0.18 | |||||
| Midwest | 110 (23%) | 49 (17%) | 61 (30%) | 55% | 24.8 ± 11.5 | ||
| Northeast | 77 (16%) | 41 (15%) | 36 (18%) | 47% | 21.4 ± 12.8 | ||
| South | 202 (42%) | 128 (46%) | 74 (36%) | 36% | 23.3 ± 11.9 | ||
| West | 97 (20%) | 63 (22%) | 34 (17%) | 35% | 20.7 ± 11.8 | ||
| Clinical | |||||||
| Previous VAD | 0.21 | 0.79 | |||||
| Yes | 85 (18%) | 44 (16%) | 41 (20%) | 48% | 23.5 ± 12.2 | ||
| No | 401 (82%) | 237 (84%) | 164 (80%) | 41% | 22.9 ± 12.0 | ||
| Discharge to IRF or SNF | 0.38 | 0.36 | |||||
| Yes | 47 (10%) | 30 (11%) | 17 (8%) | 36% | 21.5 ± 12.5 | ||
| No | 439 (90%) | 251 (89%) | 188 (92%) | 43% | 23.4 ± 11.8 |
CR, cardiac rehabilitation; IRF, inpatient rehabilitation facility; ; SD, standard deviation; VAD, ventricular assist device.
Pearson's chi-square test.
Wilcoxon's test.
Discussion
This is the first study to report CR utilization rates in patients undergoing heart transplantation in the USA. CR was underutilized among transplant recipients, with slightly over half of patients participating in CR programs. There is geographic variation in CR after heart transplantation, with the Midwest having the highest CR initiation rates. Those transplant patients who do participate in CR programs begin an average of 2 months after discharge and attend two thirds of the recommended course of 36 sessions. Younger transplant CR participants attend significantly fewer CR sessions than older patients. CR was found to be associated with a significant decrease in 1-year readmission risk in transplant patients after multivariable adjustment.
CR utilization varies by indication, with reported initiation rates ranging from < 10% in patients with systolic heart failure6 to 10% to 20% in patients with acute myocardial infarction and percutaneous coronary intervention7,8,31 and up to 30% to 35% after coronary artery bypass grafting.4,5,9,32 Our observed initiation rate of 55% in cardiac transplant recipients is the highest to date among CR's indications. However, the fact that only half of heart transplant patients undergo CR is both surprising and sub-optimal. Cardiac transplant candidates must have the potential to regain functional capacity to be listed, and a significant proportion of transplant recipients are likely capable of attending CR programs.33
Younger heart transplant recipients have the highest functional capacity in the immediate post-operative period34 and, on this basis, would be expected to be more likely to participate in CR. Our findings suggest the opposite, with younger patients less than half as likely to initiate CR than those age ≥65 years old. Moreover, younger transplant patients attend significantly fewer CR sessions than older transplant recipients. The intensity of CR participation is important as a dose-dependent relationship has been identified between the number of sessions attended and mortality in patients with ischemic heart disease.4,5 Work responsibilities are a potential barrier to CR attendance that disproportionately affects younger patients.
In addition to work responsibilities, other barriers to CR participation include distance to the nearest CR center, availability of transportation, caregiver responsibilities and social anxiety.35–8 Insurance status and the clinical specialty of the referring provider can present barriers to referral.39,40 All of these barriers are likely to vary by geographic region, and we have identified significant geographic variation in CR initiation rates. Although the South accounts for the largest proportion of heart transplants, transplant recipients in the Midwest are more than twice as likely to attend CR programs as those in the South. This geographic variation in CR utilization is consistent with earlier studies of CR use after acute myocardial infarction and coronary artery bypass grafting.9 Some of the geographic variation in CR utilization may be related to access, although nearly every transplant center in this analysis reported having a CR program. We identified similar geographic patterns in CR use among heart transplants in 2008, suggesting that this variation represents a durable trend.
Although there were similar geographic patterns in CR among transplant patients in 2008 and 2013, the proportion of the entire cohort initiating CR increased from 42% to 55% (p < 0.001). CR participants attended an average of 3.7 more sessions (p < 0.001) in 2013 compared with 5 years earlier. These findings likely represent a gradual increase over the past 10 years, as Medicare began reimbursing CR after heart transplantation in 2006.41 CR referral for heart transplantation and other conditions became a National Quality Forum–endorsed performance measure in 2007,2 after which referral rates for acute myocardial infarction42 and heart failure6 both began to rise. Of note, the CR quality measure does not apply to patients discharged to post-acute rehabilitation facilities.2
Our analysis has demonstrated that CR initiation rates are lower in transplant patients discharged to IRFs or SNFs, possibly due to lower referral rates. Severe functional impairment or frailty may limit CR participation in these patients,43 although we were unable to characterize this with administrative claims data. This population is also less able to participate in CR due to a higher burden of comorbidities, as demonstrated by the fact that heart transplant patients discharged to post-acute care facilities have a significantly higher risk of being readmitted over 1 year.
Readmissions represent a major source of morbidity and economic cost in heart transplant patients. Our study has clinical implications in demonstrating an association between CR and decreased risk of readmissions. CR programs may be an effective way for facilities to attenuate readmissions in the critical first year after heart transplantation. Healthy cohort bias is inherent to observational studies involving CR, and it is possible that such bias could lead to an overestimate of the effect of CR on readmissions. Frailty or functional impairment could contribute to this bias. However, our analysis controlled extensively for sociodemographic and clinical factors, and Elixhauser comorbidity groups provide effective comorbidity adjustment in surgical populations,22,44 including heart transplant patients.45 The most common causes of readmission in heart transplant patients are rejection, infection and cardiovascular complications.46,47 Future studies could investigate CR in the context of indications for readmission, although identifying these diagnoses would likely require adjudication.
One way that heart transplant centers could increase CR utilization is to focus on decreasing the time between discharge and the first CR session. A randomized, controlled trial between early appointments to CR after discharge (median time 8.5 days) and standard appointments (median time 42 days) in patients with ischemic heart disease demonstrated that early appointments significantly improved attendance at the orientation visit.48 Median time between discharge and first CR appointment for our cohort was 54 days, longer than the standard appointment group of the trial referenced previously. The causes of delays in CR initiation are complex and include insurance pre-approval as well as facility capacity and patient comorbidities.49,50 Another study also identified an association of time between heart transplantation and first CR appointment with greater body mass index and body fat percent, providing another rationale for early CR appointments after discharge.51 Given the fact that most transplant centers have CR programs, it is feasible for hospitals to work with CR providers to ensure that heart transplant patients are given timely appointments. Automatic enrollment of heart transplant patients in CR programs by institutional protocol has also been used to increase CR utilization.52
Our study has limitations. First, we were only able to capture utilization data on transplant patients age ≥65 years old or with Medicare disability benefits, which comprised approximately one quarter of total transplant recipients. However, the fact that most patients in our cohort received disability coverage under Medicare does not indicate that they would be inherently less likely to participate in CR, as all patients reaching UNOS IA or IB status are eligible for disability benefits. Rather, some patients may not have had disability benefits approved by the time they undergo transplantation. In addition, age, gender and racial characteristics of Medicare beneficiaries undergoing heart transplantation approximate the entire cohort of heart transplant recipients.53 Second, our data were obtained from CMS administrative claims. These data are not adjudicated and lack granular data on clinical characteristics. However, CMS data have been used to effectively study many cardiovascular therapies, including CR, in earlier work.4,5,9 Third, our analyses were limited to heart transplant patients enrolled in fee-for-service Medicare and may not be generalizable to patients enrolled in Medicare private health plans. However, fee-for-service Medicare still accounted for 72% of Medicare beneficiaries in 2013.54
In summary, only half of heart transplant recipients in the USA participate in CR programs, but CR is associated with a decreased risk of readmission at 1 year after discharge. These data suggest a path for reducing readmissions in a high-risk population that requires an enormous amount of health-care resources. Our findings invite further research on the etiology of CR under-utilization in cardiac transplant recipients, including the possibility of under-referral to CR programs as well as characterization of barriers to CR participation. This research will inform quality improvement interventions to increase CR uptake and the number of sessions attended in heart transplant recipients.
Acknowledgments
This project received grant support from Vanderbilt Clinical and Translational Science from the National Center for Advancing Translational Sciences at the National Institutes of Health (Grant UL1 TR000445), the Agency for Healthcare Research and Quality (Grant No. K12HS022990), and was supported in part by the Health Resources and Services Administration (Contract No. 234-2005-37011C).
Footnotes
Disclosure statement: The authors have no conflicts of interest to disclose. The content is the responsibility of the authors alone and does not necessarily reflect the views or policies of the supporting agencies, nor does mention of trade names, commercial products or organizations imply endorsement by the U.S. Government.
References
- 1.Thomas RJ, King M, Lui K, et al. AACVPR/ACCF/AHA 2010 update: Performance measures on cardiac rehabilitation for referral to cardiac rehabilitation/secondary prevention services: a report of the American Association of Cardiovascular and Pulmonary Rehabilitation and the American College of Cardiology Foundation/American Heart Association Task Force on Performance Measures (Writing Committee to Develop Clinical Performance Measures for Cardiac Rehabilitation) J Cardiopulm Rehabil Prev. 2010;30:279–88. doi: 10.1097/HCR.0b013e3181f5e36f. [DOI] [PubMed] [Google Scholar]
- 2.Thomas RJ, King M, Lui K, et al. AACVPR/ACC/AHA 2007 performance measures on cardiac rehabilitation for referral to and delivery of cardiac rehabilitation/secondary prevention services endorsed by the American College of Chest Physicians, American College of Sports Medicine, American Physical Therapy Association, Canadian Association of Cardiac Rehabilitation, European Association for Cardiovascular Prevention and Rehabilitation, Inter-American Heart Foundation, National Association of Clinical Nurse Specialists, Preventive Cardiovascular Nurses Association, and the Society of Thoracic Surgeons. J Am Coll Cardiol. 2007;50:1400–33. doi: 10.1016/j.jacc.2007.04.033. [DOI] [PubMed] [Google Scholar]
- 3.Anderson L, Oldridge N, Thompson DR, et al. Exercise-based cardiac rehabilitation for coronary heart disease: Cochrane systematic review and meta-analysis. J Am Coll Cardiol. 2016;67:1–12. doi: 10.1016/j.jacc.2015.10.044. [DOI] [PubMed] [Google Scholar]
- 4.Hammill BG, Curtis LH, Schulman KA, et al. Relationship between cardiac rehabilitation and long-term risks of death and myocardial infarction among elderly Medicare beneficiaries. Circulation. 2010;121:63–70. doi: 10.1161/CIRCULATIONAHA.109.876383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Suaya JA, Stason WB, Ades PA, et al. Cardiac rehabilitation and survival in older coronary patients. J Am Coll Cardiol. 2009;54:25–33. doi: 10.1016/j.jacc.2009.01.078. [DOI] [PubMed] [Google Scholar]
- 6.Golwala H, Pandey A, Ju C, et al. Temporal trends and factors associated with cardiac rehabilitation referral among patients hospitalized with heart failure: findings from Get With The Guidelines-Heart Failure Registry. J Am Coll Cardiol. 2015;66:917–26. doi: 10.1016/j.jacc.2015.06.1089. [DOI] [PubMed] [Google Scholar]
- 7.Doll JA, Hellkamp A, Ho PM, et al. Participation in cardiac rehabilitation programs among older patients after acute myocardial infarction. JAMA Int Med. 2015:E1–3. doi: 10.1001/jamainternmed.2015.3819. [DOI] [PubMed] [Google Scholar]
- 8.Schopfer DW, Takemoto S, Allsup K, et al. cardiac rehabilitation use among veterans with ischemic heart disease. JAMA Int Med. 2014:E1–3. doi: 10.1001/jamainternmed.2014.3441. [DOI] [PubMed] [Google Scholar]
- 9.Suaya JA, Shepard DS, Normand SL, et al. Use of cardiac rehabilitation by Medicare beneficiaries after myocardial infarction or coronary bypass surgery. Circulation. 2007;116:1653–62. doi: 10.1161/CIRCULATIONAHA.107.701466. [DOI] [PubMed] [Google Scholar]
- 10.Squires RW. Exercise therapy for cardiac transplant recipients. Progr Cardiovasc Dis. 2011;53:429–36. doi: 10.1016/j.pcad.2011.03.010. [DOI] [PubMed] [Google Scholar]
- 11.Stewart KJ, Badenhop D, Brubaker PH, et al. Cardiac rehabilitation following percutaneous revascularization, heart transplant, heart valve surgery, and for chronic heart failure. Chest. 2003;123:2104–11. doi: 10.1378/chest.123.6.2104. [DOI] [PubMed] [Google Scholar]
- 12.Kavanagh T. Physical training in heart transplant recipients. J Cardiovasc Risk. 1996;3:154–9. [PubMed] [Google Scholar]
- 13.Haykowsky M, Taylor D, Kim D, et al. Exercise training improves aerobic capacity and skeletal muscle function in heart transplant recipients. Am J Transplant. 2009;9:734–9. doi: 10.1111/j.1600-6143.2008.02531.x. [DOI] [PubMed] [Google Scholar]
- 14.Kobashigawa JA, Leaf DA, Lee N, et al. A controlled trial of exercise rehabilitation after heart transplantation. N Engl J Med. 1999;340:272–7. doi: 10.1056/NEJM199901283400404. [DOI] [PubMed] [Google Scholar]
- 15.Kavanagh T, Yacoub MH, Mertens DJ, et al. Cardiorespiratory responses to exercise training after orthotopic cardiac transplantation. Circulation. 1988;77:162–71. doi: 10.1161/01.cir.77.1.162. [DOI] [PubMed] [Google Scholar]
- 16.Keteyian S, Shepard R, Ehrman J, et al. Cardiovascular responses of heart transplant patients to exercise training. J Appl Physiol (1985) 1991;70:2627–31. doi: 10.1152/jappl.1991.70.6.2627. [DOI] [PubMed] [Google Scholar]
- 17.Bernardi L, Radaelli A, Passino C, et al. Effects of physical training on cardiovascular control after heart transplantation. Int J Cardiol. 2007;118:356–62. doi: 10.1016/j.ijcard.2006.07.032. [DOI] [PubMed] [Google Scholar]
- 18.Karapolat H, Engin C, Eroglu M, et al. Efficacy of the cardiac rehabilitation program in patients with end-stage heart failure, heart transplant patients, and left ventricular assist device recipients. Transplant Proc. 2013;45:3381–5. doi: 10.1016/j.transproceed.2013.06.009. [DOI] [PubMed] [Google Scholar]
- 19.Hsu CJ, Chen SY, Su S, et al. The effect of early cardiac rehabilitation on health-related quality of life among heart transplant recipients and patients with coronary artery bypass graft surgery. Transplant Proc. 2011;43:2714–7. doi: 10.1016/j.transproceed.2011.04.025. [DOI] [PubMed] [Google Scholar]
- 20.Social Security Administration Program Operations Manual System. [Accessed March 28, 2016];DI 23022.080 List of Compassionate Allowance (CAL) conditions. 2015 https://secure.ssa.gov/poms.nsf/lnx/0423022080/
- 21.United States Department of Health and Human Services, Health Resources and Services Administration. [Accessed March 29, 2016];Organ Procurement and Transplantation Network National Data. 2016 https://optn.transplant.hrsa.gov/data/view-data-reports/national-data/
- 22.Elixhauser A, Steiner C, Harris DR, et al. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 23.American Hospital Association. [Accessed November 2, 2016];American Hospital Association annual survey of hospitals. 2016 https://www.ahadataviewer.com/book-cd-products/AHA-Survey/
- 24.Lin DY, Wei LJ, Yang I, et al. Semiparametric regression for the mean and rate functions of recurrent events. J R Stat Soc B. 2000;62:711–30. [Google Scholar]
- 25.Dunlay SM, Pack QR, Thomas RJ, et al. Participation in cardiac rehabilitation, readmissions, and death after acute myocardial infarction. Am J Med. 2014;127:538–46. doi: 10.1016/j.amjmed.2014.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mi X, Hammill BG, Curtis LH, et al. Use of the landmark method to address immortal person-time bias in comparative effectiveness research: a simulation study. Stat Med. 2016;35:4824–36. doi: 10.1002/sim.7019. [DOI] [PubMed] [Google Scholar]
- 27.Suissa S. Immortal time bias in pharmaco-epidemiology. Am J Epidemiol. 2008;167:492–9. doi: 10.1093/aje/kwm324. [DOI] [PubMed] [Google Scholar]
- 28.Rothman KJ, Greenland S, Lash TL. Modern epidemiology. 3rd. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2008. [Google Scholar]
- 29.SAS Institute. Statistical Analysis Software, version 9.4. Cary, NC: SAS Institute; 2016. [Google Scholar]
- 30.R Core Team. [Accessed October 22, 2016];R: a language and environment for statistical computing. 2015 https://www.r-project.org/
- 31.Doll JA, Hellkamp A, Thomas L, et al. Effectiveness of cardiac rehabilitation among older patients after acute myocardial infarction. Am Heart J. 2015;170:855–64. doi: 10.1016/j.ahj.2015.08.001. [DOI] [PubMed] [Google Scholar]
- 32.Pack QR, Goel K, Lahr BD, et al. Participation in cardiac rehabilitation and survival after coronary artery bypass graft surgery: a community-based study. Circulation. 2013;128:590–7. doi: 10.1161/CIRCULATIONAHA.112.001365. [DOI] [PubMed] [Google Scholar]
- 33.Mehra MR, Kobashigawa J, Starling R, et al. Listing criteria for heart transplantation: International Society for Heart and Lung Transplantation guidelines for the care of cardiac transplant candidates—2006. J Heart Lung Transplant. 2006;25:1024–42. doi: 10.1016/j.healun.2006.06.008. [DOI] [PubMed] [Google Scholar]
- 34.Weiss ES, Nwakanma LU, Patel ND, et al. Outcomes in patients older than 60 years of age undergoing orthotopic heart transplantation: an analysis of the UNOS database. J Heart Lung Transplant. 2008;27:184–91. doi: 10.1016/j.healun.2007.11.566. [DOI] [PubMed] [Google Scholar]
- 35.Reges O, Vilchinsky N, Leibowitz M, et al. Systemic determinants as barriers to participation in cardiac prevention and rehabilitation services after acute coronary syndrome. Int J Cardiol. 2013;168:4865–7. doi: 10.1016/j.ijcard.2013.07.056. [DOI] [PubMed] [Google Scholar]
- 36.Shanmugasegaram S, Gagliese L, Oh P, et al. Psychometric validation of the cardiac rehabilitation barriers scale. Clin Rehabil. 2012;26:152–64. doi: 10.1177/0269215511410579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Grace SL, Gravely-Witte S, Kayaniyil S, et al. A multisite examination of sex differences in cardiac rehabilitation barriers by participation status. J Womens Health. 2009;18:209–16. doi: 10.1089/jwh.2007.0753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dunlay SM, Witt BJ, Allison TG, et al. Barriers to participation in cardiac rehabilitation. Am Heart J. 2009;158:852–9. doi: 10.1016/j.ahj.2009.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Aragam KG, Dai D, Neely ML, et al. Gaps in referral to cardiac rehabilitation of patients undergoing percutaneous coronary intervention in the United States. J Am Coll Cardiol. 2015;65:2079–88. doi: 10.1016/j.jacc.2015.02.063. [DOI] [PubMed] [Google Scholar]
- 40.Ades PA, Waldmann ML, McCann WJ, et al. Predictors of cardiac rehabilitation participation in older coronary patients. Arch Intern Med. 1992;152:1033–5. [PubMed] [Google Scholar]
- 41.Cardiac intensive cardiac rehabilitation program: conditions of coverage (42 CFR 410.49) Federal Register. 2009;226:74. [Google Scholar]
- 42.Beatty AL, Li S, Thomas L, et al. Trends in referral to cardiac rehabilitation after myocardial infarction: data from the National Cardiovascular Data Registry 2007 to 2012. J Am Coll Cardiol. 2014;63:2582–3. doi: 10.1016/j.jacc.2014.03.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Vigorito C, Abreu A, Ambrosetti M, et al. Frailty and cardiac rehabilitation: a call to action from the EAPC Cardiac Rehabilitation Section. Eur J Prev Cardiol. 2017;224:577–90. doi: 10.1177/2047487316682579. [DOI] [PubMed] [Google Scholar]
- 44.Southern DA, Quan H, Ghali WA. Comparison of the Elixhauser and Charlson/Deyo methods of comorbidity measurement in administrative data. Med Care. 2004;42:355–60. doi: 10.1097/01.mlr.0000118861.56848.ee. [DOI] [PubMed] [Google Scholar]
- 45.Mujib M, Khanna N, Mazumder NK, et al. Pretransplant coagulopathy and in-hospital outcomes among heart transplant recipients: a propensity-matched nationwide inpatient sample study. Clin Cardiol. 2015;38:300–8. doi: 10.1002/clc.22391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tsao CI, Chou NK, Chi NH, et al. Unplanned readmission within 1 year after heart transplantation in Taiwan. Transplant Proc. 2010;42:946–7. doi: 10.1016/j.transproceed.2010.02.053. [DOI] [PubMed] [Google Scholar]
- 47.Donovan MP, Drusin RE, Edwards NM, et al. Analysis of trends in hospital readmissions and postoperative complications in heart transplant recipients: single center study. Transplant Proc. 2002;34:1853–4. doi: 10.1016/s0041-1345(02)03070-1. [DOI] [PubMed] [Google Scholar]
- 48.Pack QR, Mansour M, Barboza JS, et al. An early appointment to outpatient cardiac rehabilitation at hospital discharge improves attendance at orientation: a randomized, single-blind, controlled trial. Circulation. 2013;127:349–55. doi: 10.1161/CIRCULATIONAHA.112.121996. [DOI] [PubMed] [Google Scholar]
- 49.Collins ZC, Suskin N, Aggarwal S, et al. Cardiac rehabilitation wait times and relation to patient outcomes. Eur J Phys Rehabil Med. 2015;51:301–9. [PubMed] [Google Scholar]
- 50.Russell KL, Holloway TM, Brum M, et al. Cardiac rehabilitation wait times: effect on enrollment. J Cardiopulm Rehabil Prevent. 2011;31:373–7. doi: 10.1097/HCR.0b013e318228a32f. [DOI] [PubMed] [Google Scholar]
- 51.Marzolini S, Grace SL, Brooks D, et al. Time-to-referral, use, and efficacy of cardiac rehabilitation after heart transplantation. Transplantation. 2015;99:594–601. doi: 10.1097/TP.0000000000000361. [DOI] [PubMed] [Google Scholar]
- 52.Rosenbaum AN, Kremers WK, Schirger JA, et al. association between early cardiac rehabilitation and long-term survival in cardiac transplant recipients. Mayo Clin Proc. 2016;91:149–56. doi: 10.1016/j.mayocp.2015.12.002. [DOI] [PubMed] [Google Scholar]
- 53.Bentley TS. U.S. organ and tissue transplant cost estimates and discussion. [Accessed September 1, 2016];Milliman Research Report. 2014 2014 http://www.milliman.com/insight/research/health/2014-U_S_-organ-and-tissue-transplant-cost-estimates-and-discussion/
- 54.Kaiser Family Foundation. [Accessed September 27, 2016];Fact Sheet: Medicare Advantage. 2016 http://files.kff.org/attachment/Fact-Sheet-Medicare-Advantage/


