Abstract
Objectives
We investigate the reporting of obesity on death certificates in three countries (France, Italy, and the United States) with different levels of prevalence, and we examine which causes are frequently associated with obesity.
Methods
We use cause-of-death data for all deaths at ages 50–89 in 2010–2011. Since obesity may not be the underlying cause (UC) of death, we compute age- and sex- standardized death rates considering all mentions of obesity (multiple causes or MC). We use cluster analyses to identify patterns of cause-of-death combinations.
Results
Obesity is selected as UC in no more than 20% of the deaths with a mention of obesity. Mortality levels, whether measured from the UC or the MC, are weakly related to levels of prevalence. Patterns of cause-of-death combinations are similar across the countries. In addition to strong links with cardiovascular diseases and diabetes, we identify several less familiar associations.
Conclusions
Considering all mentions on the deaths certificates reduces the underestimation of obesity-related mortality based on the UC only. It also enables us to describe the various mortality patterns involving obesity.
Keywords: Obesity, Mortality, Multiple causes of death, International comparison
Introduction
Over the past 40 years, excess weight has become a growing public health concern worldwide (Prospective Studies Collaboration 2009; Finucane et al. 2011; NCD Risk Factor Collaboration 2016). Individuals are usually classified by Body Mass Index (BMI) into one of four categories (underweight, normal weight, overweight, and obese), with the last category sometimes disaggregated into moderately obese, severely obese, and morbidly obese. A number of studies have found an excess risk of death of obese individuals compared to normal-weight adults (Calle et al. 2003; Fontaine et al. 2003; Katzmarzyk and Ardern 2004; Flegal et al. 2005; Adams et al. 2006; Kitahara et al. 2014). Though all cause-of-death categories contribute to this excess mortality, obesity is most strongly associated with diseases of the circulatory system, diabetes, kidney diseases, and respiratory infections, as well as with cancers of several sites (Calle et al. 2003; Kitahara et al. 2014; Poirier et al. 2006; Flegal et al. 2007; Karlsson and Beck 2010; National Cancer Institute 2016).
The association between obesity and mortality calls for further monitoring and investigation of obesity-related mortality. In this study, we explore the contribution of obesity to mortality using vital statistics, which provide information on all deaths, in France, Italy, and the United States (U.S.). To our knowledge, vital statistics have rarely been used to analyse obesity-related mortality and never in a comparative perspective. According to the latest national estimates, the prevalence of self-reported obesity in the adult population is much higher in the U.S. than in the two European countries, with a prevalence of over 35% (36% for females and 35% for males) in the former (Flegal et al. 2016) compared with 15% (16% for females and 14% for males) in France (ObEpi 2012) and 11% (10% for females and 12% for males) in Italy (authors’ calculations based on the 2013 Health Survey “Indagine sulla salute”). When only morbid obesity is considered, the picture is similar, with a female disadvantage in all three countries (1.6% for females vs 0.6% for males in France, 0.6 vs 0.5% in Italy, 8 vs 4% in the U.S.).
We first compute mortality indicators for the three countries, and we examine how they reflect these differences in prevalence. Cause-specific mortality indicators usually rely on the “underlying cause of death” as proposed by the World Health Organization (WHO) that is “the disease or injury which initiated the train of morbid events leading directly to death”. Recently, research has emerged that takes into account all causes recorded on the certificates, or all “multiple causes” (Désesquelles et al. 2015). Duncan et al. (2010) and Duncan and Goldacre (2012) have used this approach to study the certification of obesity in England. The strategy is motivated by the fact that obesity may not be selected as the underlying cause even though it played a prominent role in the morbid process. Taking all mentions on the death certificate into account also provides an opportunity for detailed examination of the causes most frequently associated with obesity, the second aim of this paper. The comparative design of our research allows for the identification of similarities and dissimilarities in the pattern of cause-of-death combinations across the three countries.
Methods
The analysis is based on the information reported on all death certificates for the years 2010 and 2011 (pooled to guarantee a sufficient number of cases) with data prepared by the French National Institute for Health and Medical Research (INSERM) for France, by the National Register on Causes of Death under the Italian National Institute of Statistics (ISTAT) for Italy, and by the National Center for Health Statistics (NCHS) within the Centers for Disease Control (CDC) in the United States. In all three countries, there is no restriction on the number of causes recorded in the databases. We distinguish between the underlying cause of death (UC) and all other causes mentioned on the certificate, herein labelled contributing causes (CC). Underlying and contributing causes combine into the multiple causes (MC). In all three countries, causes are coded under the 10th Revision of the International Classification of Diseases (ICD-10), in which obesity is coded E66. The analysis is restricted to deaths between the ages of 50 and 89 years. Deaths under 50 and over 90 have been excluded because of an insufficient number of cases in France and Italy (less than 1300 deaths when all mentions are considered, representing 11% of those deaths in France and 13% in Italy). Interestingly, in 2010–2011, 27% of all deaths with a mention of obesity in the U.S. occurred under the age of 50. This calls for a specific analysis on that age group in the U.S. that we leave for further research.
Obesity-related mortality is measured by computing age- and sex-standardized death rates using (1) records with obesity as the UC and (2) records with obesity as MC. We use the Eurostat European standard population by sex and 5-year age groups as the standard age structure (Eurostat 2013). To identify the causes most frequently associated with obesity, we perform a multiple correspondence analysis (MCA) on all deaths with at least one mention of obesity, together with a cluster analysis using the mixed classification package (SEMIS method) in ©SPAD, version 8.0 (Confais and Nakache 2006). The clusters are determined from the first ten principal components constructed with the MCA. For the purpose of this analysis, all causes other than obesity are reduced into an exhaustive set of 71 groups of causes (Online Resource Table S1). This list is very similar to the Eurostat shortlist of causes of death (Eurostat 2012). In the rest of the paper, quotation marks are used to indicate that we use the exact name of the group of causes as it appears in our list.
For each death record, each of these groupings is represented by a dichotomous variable that takes the value of 1 when the group is listed on the death certificate and 0 otherwise. Obesity is treated differently, since all death certificates in our study include by designing a mention of obesity. The corresponding variable takes the value of 1 when obesity is the UC and 0 when it is a CC. Age (in 5-year groups), sex, country, and the underlying cause classified according to the same 71 groupings as above are included as supplementary variables. Analyses first performed separately for each country yielded very similar results (Online Resource Table S2). Therefore, the analysis has been repeated after pooling the deaths for all three countries, with each death weighted to account for the differences in age and sex structure and the unequal number of cases between France, Italy, and the U.S. (Table 1).
Table 1.
Total number of death records at ages 50–89 years with any mention of obesity as underlying/multiple cause, crude death rates, and average number of mentions per certificate
| France | Italy | U.S. | |
|---|---|---|---|
| Deaths with obesity as UC | |||
| Frequency | 1950 | 1376 | 7960 |
| Crude death rate (p 100,000) | 4.3 | 3.0 | 4.1 |
| Average age at death | 70 | 71 | 64 |
| % Females | 58% | 62% | 54% |
| Average number of entries/certificate | 3.2 | 3.6 | 3.7 |
| Deaths with obesity as MC | |||
| Frequency | 10,233 | 8882 | 42,728 |
| Crude death rate (p 100,000) | 22.8 | 19.1 | 21.9 |
| Average age at death | 71 | 73 | 65 |
| % Females | 54% | 64% | 51% |
| Average number of entries/certificate | 4.7 | 5.1 | 4.6 |
| Deaths from all causes | |||
| Frequency | 807,855 | 912,014 | 3,692,756 |
| Crude death rate (p 100,000) | 1798 | 1964 | 1891 |
| Average number of entries/certificate | 2.6 | 3.4 | 2.6 |
France, Italy, and the United States, 2010–2011
Results
Over the years 2010 and 2011, the total number of deaths at ages 50–89 years with obesity as the UC was 1950 in France, 1376 in Italy, and 7960 in the U.S. (Table 1). These figures increase to 10,233 in France, 8882 in Italy, and 42,728 in the U.S. when all mentions of obesity are considered. The average number of causes mentioned on these certificates is similar in France and in the U.S. (4.7 and 4.6) and slightly higher in Italy (5.1). In all three countries, these figures are higher than for deaths from all causes, indicating that obesity is involved in complex lethal processes.
For females, standardized mortality rates from obesity as the UC are higher in France (4.4 per 100,000) than in the U.S. (3.9 per 100,000), and the lowest in Italy (3.1 per 100,000) (Fig. 1a). For males, the rate in the U.S. (4.2 per 100,000) slightly exceeds that for France (4.0) with Italy again falling far below (2.5) (Fig. 1b). When all mentions of obesity are taken into account, the rates increase by a factor of about 6 for males and by about 5 for females (except in Italy where the increase is as for males) (Fig. 2). The country ranking remains the same: obesity-related MC standardized mortality rates for females are basically the same in France (21.2 per 100,000) and in the U.S. (21.3), and hardly lower in Italy (20.0). The corresponding MC rates for males are 23.9 per 100,000 in France and 23.0 in the U.S., and the rate is much lower in Italy (15.1 per 100,000). Sex differences vary by country. In Italy, both the UC and the MC female rates exceed those for males. The opposite is true in the U.S. In France, female rates exceed male rates only when obesity is the UC.
Fig. 1.
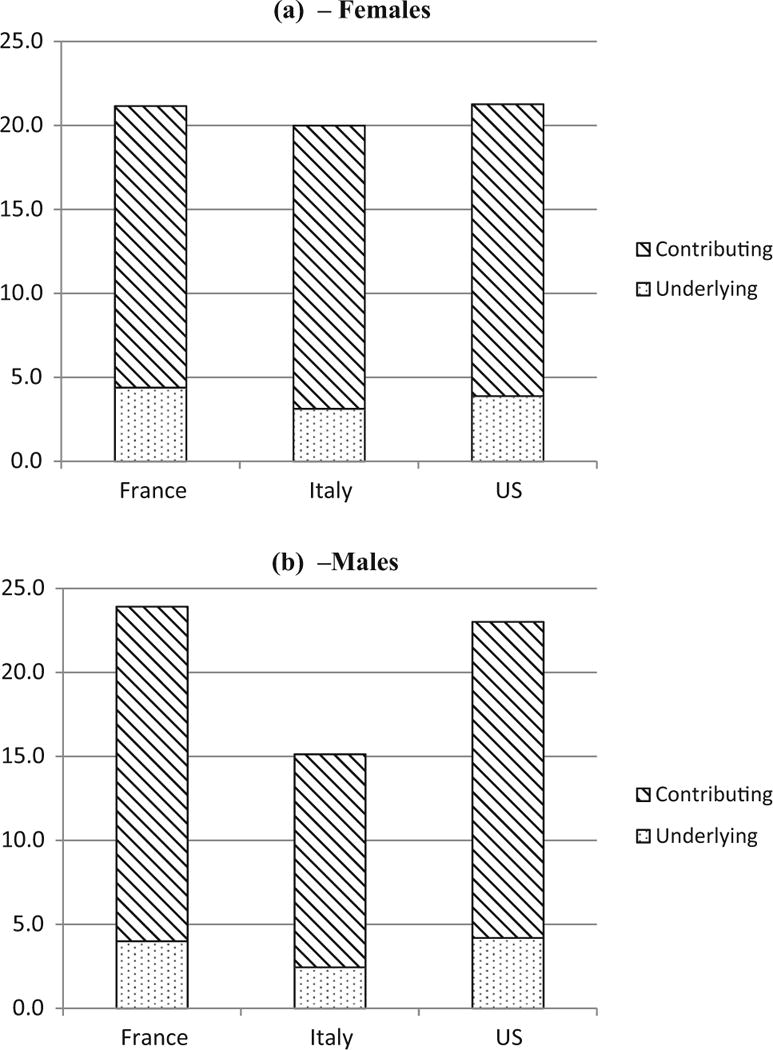
Age-standardized mortality rates (per 100,000) at ages 50–89 years for obesity as the underlying cause or as a contributing cause. France, Italy, and the United States, 2010–2011. a Females, b males
Fig. 2.
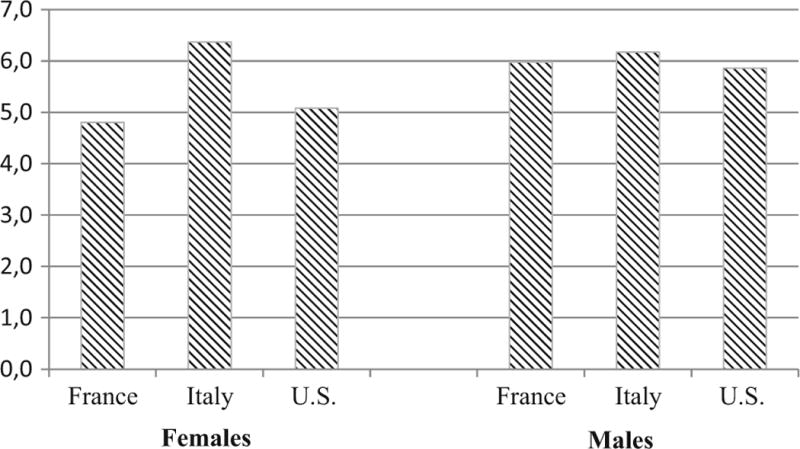
Ratio of the age-standardized “multiple causes” mortality rates to the “underlying cause” mortality rates at ages 50–89 years. France, Italy, and the United States, 2010–2011
Table 2 describes the nine main clusters of causes of death resulting from the analysis performed for all countries together. The first cluster, representing 16% of all weighted deaths (WD), mostly combines all cases where obesity is the underlying cause (72% of those deaths). Two main groups of causes associated with obesity are overrepresented: respiratory diseases and diseases of the nervous system (mainly sleep disorders like sleep apnea and anoxic brain damage). Deaths in France are more heavily represented in this cluster.
Table 2.
Clusters resulting from the multiple correspondence analysis on the pooled data. Deaths at ages 50–89 years with any mention of obesity, France, Italy and the United States, 2010–2011
| Cluster 1/9 (16%) | Obesity UC 84% |
| Other respiratory diseases 16% | |
| Other nervous diseases 14% | |
| France 39% Italy 30% U.S 31% | |
| Cluster 2/9 (24%) | Obesity CC 97% ischemic heart diseases 63% hypertension 69% Diabetes 53% |
| Ischemic heart diseases as UC 44% | |
| Other endocrine or metabolic diseases 22% | |
| France 28% Italy 32% U.S. 40% | |
| Cluster 3/9 (18%) | Obesity CC 96% other heart diseases 74% |
| Chronic lower respiratory diseases 38% | |
| Renal failure 36% | |
| Other circulatory diseases 30% | |
| Other respiratory diseases 21% | |
| France 28% Italy 44% U.S. 28% | |
| Cluster 4/9 (8%) | Obesity CC 93% cerebrovascular diseases 87% hypertension 67% |
| Diabetes 46% | |
| Cerebrovascular diseases as UC 45% | |
| Other nervous diseases 29% | |
| France 34% Italy 43% U.S. 23% | |
| Cluster 5/9 (12%) | Obesity CC 94% septicemia 63% |
| Pneumonia 35% | |
| Renal failure 31% | |
| Other digestive diseases 20% | |
| Skin diseases 19% | |
| Genitourinary diseases 15% | |
| France 34% Italy 35% U.S. 31% | |
| Cluster 6/9 (9%) | Obesity CC 87% mental disorders 90% |
| Ischemic heart diseases 42% | |
| Chronic lower respiratory diseases 37% | |
| Other nervous diseases 18% | |
| Alcoholic psychosis-chronic alcohol abuse 15% | |
| France 33% Italy 17% U.S. 50% | |
| Cluster 7/9 (8%) | Obesity CC 91% external causes 81% |
| Other diseases of the circulatory system 26% | |
| Other diseases of the musculoskeletal system/connective tissue 21% | |
| Other digestive diseases 19% | |
| France 40% Italy 26% U.S. 34% | |
| Cluster 8/9 (3%) | Obesity CC 90% chronic liver disease 90% other digestive diseases 53% |
| Alcoholic psychosis-chronic alcohol abuse 23% | |
| Septicemia 15% | |
| France 47% Italy 32% U.S. 21% | |
| Cluster 9/9 (2%) | Obesity CC 99% secondary neoplasm 100% |
| France 54% Italy 36% U.S. 10% |
Deaths at ages 50–89 years with any mention of obesity, France, Italy, and the United States, 2010–2011. 16% of all weighted deaths are included in the first cluster. For 84% of those deaths, obesity is the underlying cause. Groups of causes that are mentioned on more than 50% of the death certificates of a cluster are in italics. Note that the percentages in a cluster add up to more than 100, because several groups of causes can be listed simultaneously on a death certificate
In all other clusters, obesity is predominantly a contributing cause (from 87% in cluster 6 to 99% in cluster 9). The largest grouping is the second cluster (with 24% of the WD), which essentially captures the combination of obesity with ischemic heart disease, mostly as the UC, as well as with hypertension, diabetes, and other endocrine or metabolic diseases. In this second cluster, deaths from the U.S. are overrepresented.
The third cluster is slightly smaller, including 18% of the WD. It is characterized by a combination of obesity with “Other heart diseases”, as well as with “Other diseases of the circulatory system”. Respiratory diseases (mainly chronic lower respiratory diseases other than asthma and “Other diseases of the respiratory system”) as well as renal failure are also frequently mentioned on the certificates in this cluster. Those deaths are more often Italian than French or American.
In the fourth cluster (8% of the WD), obesity is very frequently associated with cerebrovascular diseases (including 45% as the UC) as well as with hypertension and diabetes. Mentions of “Other diseases of the nervous system” are overrepresented in this cluster. Deaths in this cluster occurred more frequently in Italy.
The fifth cluster (12% of the WD) is characterized by various infectious diseases: septicaemia, pneumonia, skin diseases (mainly decubitus ulcer and ulcers of the lower limbs), as well as diseases of the genitourinary system (mainly urinary tract infections). Renal failure and some diseases of the digestive system are also frequent contributing causes in this cluster.
The sixth cluster (9% of the WD) strongly characterizes the association between obesity and mental disorders (mainly tobacco use and depression). Chronic lower respiratory diseases other than asthma, some diseases of the nervous system, as well as ischemic heart diseases are also frequently mentioned in this cluster. Though much less commonly mentioned, alcohol consumption (15% of deaths) is overrepresented. Deaths in this cluster occurred more frequently in the U.S.
The seventh cluster is similar in size (8% of the WD). It is largely characterized by an association between obesity and external causes. This cluster also includes an overrepresentation of death certificates with mentions of “Other diseases of the musculoskeletal system/connective tissue”, “Other diseases of the circulatory system”, and “Other diseases of the digestive system”. Deaths in France are overrepresented.
The remaining two clusters are very small. Only 3% of all WD belong to the eighth cluster. 90% of those death certificates include a mention of a chronic liver disease and/or another disease of the digestive system. They also often mention “Alcoholic psychosis/chronic alcohol abuse” and septicaemia. Deaths in this cluster are more frequently French than Italian or American. The ninth cluster includes only 2% of the WD. All certificates in this cluster include mention of a secondary neoplasm as contributing cause. A large variety of cancer sites are selected as underlying cause. Deaths in France are overrepresented.
Discussion
In this analysis of obesity-related mortality in France, Italy, and the U.S., we find that mortality levels at ages 50–89 are not consistent with prevalence levels in self-reported obesity. While Italy ranks the lowest on both indicators, the U.S. exhibits obesity-related mortality rates very close to those in France, despite its much higher prevalence of obesity. Similarly, the higher prevalence of morbid obesity among females compared with males is not reflected in a higher rate of obesity-related mortality. When recorded on a death certificate, the frequency with which obesity is selected as the underlying cause does not vary much across countries and between men and women. Underlying cause mortality identifies no more than 20% of all deaths with obesity as a certified cause, a percentage similar to that found by Duncan et al. for England in (2010). This result confirms that monitoring obesity-related mortality on the basis of the underlying cause alone is clearly insufficient, and it is absolutely necessary to take the contributing causes into account.
The reason for the discrepancy between country ranking on obesity prevalence and country ranking on obesity-related mortality could be partly due to cross-country differences in certification. Obesity is a risk factor for many diseases. It may also aggravate other diseases or render their treatment more complex. In either case, it should be recorded on the death certificate, but physicians’ propensity to do so may differ from one country to another. The fact that, despite large differences in terms of prevalence, obesity-related mortality is similar in the three countries which suggests that this propensity could be lower in the U.S. than in France and Italy. Because of the higher frequency of obesity, U.S. physicians may only be sensitive to abnormally high BMIs and under-report moderate obesity compared with France and Italy.
This said that obesity may be under-reported on death certificates in the other two countries likewise. First, the deterioration of health before death often results in weight loss, which is likely to reduce the probability of reporting a prior obesity status on the certificate. More generally, the quality of the reporting of “conditions” (e.g., hypertension) or behaviours (e.g., smoking, drinking) as opposed to “diseases” is a matter of concern. Though obesity has been included in the International Classification of Diseases as far back as the 7th revision published in 1955, WHO first referred to obesity as a disease in a 1997 report only (WHO 1997). Since then, the appropriateness of this denomination has been questioned (Heshka and Allison 2001). In 2013, the American Medical Association decided to classify obesity as a disease (Pollack 2016). In France and in Italy, obesity has also been designated as a “chronic disease […] due to economic and nutritional changes” (Ministère du travail, de l’emploi et de la santé) or as a “social disease” (Istituto superiore di sanità). The lack of consensus on whether obesity is a clinical entity or a social and behavioural problem (Stoner and Cornwall 2014) creates uncertainty among physicians, which may contribute to under-reporting.
Another important result of this research is that, despite differences in the reporting of obesity on death certificates in the three countries, obesity is involved in morbid processes in a fairly similar manner across countries. The association between obesity and cardiovascular diseases is the most frequent combination of causes: half of the death certificates belong to one of the clusters characterized by cardiovascular diseases (clusters 2, 3, and 4). These clusters also emphasize the link between obesity and diabetes and other endocrine diseases. It must be noted that the share of the three countries in these three clusters is not alike. Once controlled for the different age and sex structure of the deceased, deaths in the U.S. are overrepresented in the cluster characterized by ischaemic heart diseases, while the association between obesity and cerebrovascular diseases is more frequent in Italy. These differences are likely to reflect specificities in the general mortality patterns of the three countries, independently from obesity.
The link between obesity and chronic liver diseases and other diseases of the digestive system mainly reflects the hepatic consequences of obesity. Severe liver damage is partly attributed to the common association between obesity on one hand, and diabetes and other metabolic abnormalities on the other (Adler and Schaffner 1979). Interestingly, three clusters that represent about one tenth of the deaths certificates each (clusters 5, 6, and 7) correspond to less familiar combinations of causes. Obesity appears to be strongly associated with infectious diseases. In the literature, obesity has been shown to impair the immune functions and to reduce antigen stimulation, resulting in increased susceptibility to infections (Karlsson and Beck 2010). As noted before, mental disorders recorded with obesity are mainly tobacco use, likely explained by the prevalence of smoking in the general population, and depression, previously found in the literature to be associated with obesity (Onyike et al. 2003; Zhao et al. 2009). The association between obesity and external causes includes conditions as diverse as drug poisoning (both pharmaceutical and illegal), complications of injuries and medical interventions [probably due to the known delays in healing and the risks of infection from open wounds in obese people (Wilson and Clark 2003)], and choking, because of airway obstruction (Kitahara et al. 2014).
Finally, the proportion of deaths in the cluster characterized by secondary neoplasms is fairly low (only 2%) relative to findings in the literature on biological mechanisms relating obesity and cancer (Calle et al. 2003). This suggests that certifying physicians frequently overlook the role of obesity in cancer mortality, possibly in part because of the weight loss resulting from cancer. However, it has been shown that contributing conditions are generally less likely to be mentioned on death certificates with cancer as the UC (Désesquelles et al. 2012).
Vital statistics underestimate the contribution of obesity to mortality, especially when taking only the underlying cause of death into account. Because the role of obesity in mortality is likely to increase, together with its prevalence in most populations, the certification of obesity needs to be improved through clear instructions to physicians. More research is needed on the factors influencing certification practices. With regard to the causes associated with obesity on the death certificates, the consistency of findings across countries indicates that multiple cause-of-death data represent a very valuable source of information to characterize the complex morbid processes involving obesity. In this paper, we described the most frequent combinations of causes. In doing so, we might have overlooked more specific mechanisms by which obesity increases the risk of death. Further research is needed to explore those combinations of causes.
Supplementary Material
Acknowledgments
Magali Barbieri was partly supported by awards from the U.S. National Institute on Aging (R01-AG011552 and R01- AG040245), the Society of Actuaries-REX Pool fund, and the Canadian Institute of Actuaries. However, any opinions, findings, and conclusions or recommendations expressed in this material are those of the authors alone and do not necessarily represent the official views of the National Institute on Aging and other funders. The authors would like to thank Professor Irma Elo (University of Pennsylvania) for her helpful comments on an earlier version of this manuscript.
Footnotes
Electronic supplementary material The online version of this article (doi:10.1007/s00038-017-0978-1) contains supplementary material, which is available to authorized users.
Compliance with ethical standards
Conflict of interest The authors declare that there is no competing interests.
References
- Adams KF, Schatzkin A, Harris TB, Kipnis V, Mouw T, Ballard-Barbash R, Hollenbeck A, Leitzmann MF. Overweight, obesity, and mortality in a large prospective cohort of persons 50 to 71 years old. N Engl J Med. 2006;355(8):763–778. doi: 10.1056/NEJMoa055643. [DOI] [PubMed] [Google Scholar]
- Adler M, Schaffner F. Fatty liver hepatitis and cirrhosis in obese patients. Am J Med. 1979;67(5):811–816. doi: 10.1016/0002-9343(79)90740-x. [DOI] [PubMed] [Google Scholar]
- Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of US adults. N Engl J Med. 2003;348(17):1625–1638. doi: 10.1056/NEJMoa021423. [DOI] [PubMed] [Google Scholar]
- Confais J, Nakache JP. Approche pragmatique de la classification. Revue MODULAD. 2006;119:34. [Google Scholar]
- Désesquelles A, Salvatore MA, Pappagallo M, Frova L, Pace M, Meslé F, et al. Analysing multiple causes of death: which methods for which data? An application to the cancer-related mortality of France and Italy. Eur J Popul. 2012;28(4):467–498. [Google Scholar]
- Désesquelles A, Demuru E, Pappagallo M, Frova L, Meslé F, Egidi E. After the epidemiologic transition: a reassessment of mortality from infectious diseases among over-65 s in France and Italy. Int J Public Health. 2015;60(5):515–628. doi: 10.1007/s00038-015-0704-9. [DOI] [PubMed] [Google Scholar]
- Duncan ME, Goldacre MJ. Certification of deaths from diabetes mellitus and obesity in England: trends into the twenty- first century. J Public Health (Oxf) 2012;35(2):293–297. doi: 10.1093/pubmed/fds074. [DOI] [PubMed] [Google Scholar]
- Duncan M, Griffith M, Rutter H, Goldacre MJ. Certification of obesity as a cause of death in England 1979-2006. Eur J Public Health. 2010;20(6):671–675. doi: 10.1093/eurpub/ckp230. [DOI] [PubMed] [Google Scholar]
- Eurostat. Shortlist of causes of death. 2012 http://ec.europa.eu/eurostat/ramon/nomenclatures/index.cfm?TargetUrl=LST_NOM_DTL&StrNom=COD_2012&StrLanguageCode=EN&IntPcKey=&StrLayoutCode=HIERARCHIC.
- Eurostat. (Eurostat, methodologies and working papers).Revision of the European Standard Population—report of Eurostat’s task force. (2013th) 2013 http://ec.europa.eu/eurostat/documents/3859598/5926869/KS-RA-13-028-EN.PDF/e713fa79-1add-44e8-b23d-5e8fa09b3f8f.
- Finucane MM, Stevens GA, Cowan MJ, Danaei G, Lin JK, Paciorek CJ, Singh GM, Gutierrez HR, Lu Y, Bahalim AN, Farzadfar F. National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9.1 million participants. Lancet. 2011;377(9765):557–567. doi: 10.1016/S0140-6736(10)62037-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flegal KM, Graubard BI, Williamson DF, Gail MH. Excess deaths associated with underweight, overweight, and obesity. J Am Med Assoc. 2005;293(15):1861–1867. doi: 10.1001/jama.293.15.1861. [DOI] [PubMed] [Google Scholar]
- Flegal KM, Graubard BI, Williamson DF, Gail MH. Cause- specific excess deaths associated with underweight, overweight, and obesity. J Am Med Assoc. 2007;298(17):2028–2037. doi: 10.1001/jama.298.17.2028. [DOI] [PubMed] [Google Scholar]
- Flegal KM, Kruszon-Moran D, Carroll MD, Fryar CD, Ogden CL. Trends in obesity among adults in the United States, 2005 to 2014. J Am Med Assoc. 2016;315(21):2284–2291. doi: 10.1001/jama.2016.6458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fontaine KR, Redden DT, Wang C, Westfall AO, Allison DB. Years of life lost due to obesity. J Am Med Assoc. 2003;289(2):187–193. doi: 10.1001/jama.289.2.187. [DOI] [PubMed] [Google Scholar]
- Heshka S, Allison DB. Is obesity a disease? Int J Obes Relat Metab Disord. 2001;25(10):1401–1404. doi: 10.1038/sj.ijo.0801790. [DOI] [PubMed] [Google Scholar]
- Istituto superiore di sanità. http://www.epicentro.iss.it/temi/croniche/ObesitaEpidemiaSociale.asp.
- Karlsson EA, Beck MA. The burden of obesity on infectious disease. Exp Biol Med. 2010;235(12):1412–1424. doi: 10.1258/ebm.2010.010227. [DOI] [PubMed] [Google Scholar]
- Katzmarzyk PT, Ardern CI. Overweight and obesity mortality trends in Canada, 1985-2000. Can J Public Health. 2004;1:16–20. doi: 10.1007/BF03403627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kitahara CM, Flint AJ, de Gonzalez AB, Bernstein L, Brotzman M, MacInnis RJ, Moore SC, Robien K, Rosenberg PS, Singh PN, Weiderpass E. Association between class III obesity (BMI of 40–59 kg/m2) and mortality: a pooled analysis of 20 prospective studies. PLoS Med. 2014;11(7):e1001673. doi: 10.1371/journal.pmed.1001673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ministère du travail, de l’emploi et de la santé. Plan Obésité 2010-2013. http://social-sante.gouv.fr/IMG/pdf/Plan_Obesite_2010_2013.pdf.
- National Cancer Institute. Factsheet on obesity and cancer risk. 2016 http://www.cancer.gov/about-cancer/causes-prevention/risk/obesity/obesity-fact-sheet.
- NCD Risk Factor Collaboration. Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19.2 million participants. Lancet. 2016;387(10026):1377–1396. doi: 10.1016/S0140-6736(16)30054-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ObEpi. Enquête épidémiologique nationale sur le surpoids et l’obésité. 2012 http://www.roche.fr/innovation-recherche-medicale/decouverte-scientifique-medicale/cardio-metabolisme/enquete-nationale-obepi-2012.html.
- Onyike CU, Crum RM, Lee HB, Lyketsos DG, Eaton WW. Is obesity associated with major depression? Results from the Third National Health and Nutrition Examination Survey. Am J Epidemiol. 2003;158(12):1139–1147. doi: 10.1093/aje/kwg275. [DOI] [PubMed] [Google Scholar]
- Poirier P, Giles TD, Bray GA, Hong Y, Stern JS, Pi-Sunyer FX, Eckel RH. Obesity and cardiovascular disease: pathophysiology, evaluation, and effect of weight loss an update of the 1997 American Heart Association Scientific statement on obesity and heart disease from the obesity committee of the council on nutrition, physical activity, and metabolism. Circulation. 2006;113(6):898–918. doi: 10.1161/CIRCULATIONAHA.106.171016. [DOI] [PubMed] [Google Scholar]
- Pollack AAMA. Recognizes obesity as a disease. 2016 http://www.nytimes.com/2013/06/19/business/ama-recognizes-obesity-as-a-disease.html.
- Prospective Studies Collaboration. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009;373(9669):1083–1096. doi: 10.1016/S0140-6736(09)60318-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stoner L, Cornwall J. Did the American Medical Association make the correct decision classifying obesity as a disease? Aust Med J. 2014;7(11):462–464. doi: 10.4066/AMJ.2014.2281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO. Report of a WHO consultation obesity. WHO; Geneva: 1997. Obesity: preventing and managing the global epidemic. [PubMed] [Google Scholar]
- Wilson JA, Clark JJ. Obesity: impediment to wound healing. Crit Care Nurs Q. 2003;26(2):119–132. doi: 10.1097/00002727-200304000-00006. [DOI] [PubMed] [Google Scholar]
- Zhao G, Ford ES, Dhingra S, Li C, Strine TW, Mokdad AH. Depression and anxiety among US adults: associations with body mass index. Int J Obesity. 2009;33(2):257–266. doi: 10.1038/ijo.2008.268. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


