Abstract
Objective
Examine initial levels and pattern of change of alliance in group treatment for posttraumatic stress disorder (PTSD) for veterans.
Method
One hundred and seventy-eight male veterans with PTSD were recruited for this study. Participants were randomly assigned to either group cognitive behavioral therapy (GCBT) or to group present-centered therapy (GPCT). Alliance with fellow group members was assessed every other session throughout the group (total of seven assessments). Hierarchical linear modeling was used to determine whether treatment condition or index trauma type (interpersonal or non-interpersonal) impacted initial levels of alliance or change in alliance over time.
Results
Alliance increased significantly throughout treatment in both conditions. The presence of an interpersonal index event, compared to a non-interpersonal index event, did not significantly impact either initial levels of alliance or change in alliance over time. Participants in the GCBT condition experienced significantly greater growth in alliance over time compared to those in the GPCT condition (p > .05), but did not have significantly different initial alliance ratings.
Conclusions
The components and focus of the GCBT treatment may have facilitated more rapid bonding among members. Interpersonal traumatic experience did not negatively impact group alliance.
Keywords: Alliance, trauma, group psychotherapy
The alliance between clinician and patient in individual therapy has been regularly studied for over 40 years across many different modalities of treatment, and has been identified as a significant predictor of treatment success (Horvath, 1994; Martin, Garske, & Davis, 2000). When examining group therapy, the relationship of the group members with each other is thought to play a critical role in group treatment process and outcome (Yalom & Leszcz, 2005). Although a number of researchers have used the term “cohesion” to capture the level of emotional relatedness between group members (e.g., Barlow & Burlingame, 2006), many others have used the term “alliance” to capture more broadly the interpersonal work factors (e.g., collaboration, bonding, shared focus) among members of a group (Burlingame, MacKenzie, & Strauss, 2003). Holmes and Kivlighan (2000) found that patients in group therapy consider the relationships they develop with other group members to be equally or more impactful in their treatment than relationships with the therapist. In particular, alliance among group members has been associated with group members’ frequency of meaningful self-disclosures, which in turn has been found to lead to more frequent and intense feedback from fellow patients (Makler, Sigal, Gelkopf, Kochba, & Horeb, 1990; Tschuschke & Dies, 1994). Crowe and Grenyer (2008) found that patients in group treatment self-reported that successful recovery was more strongly associated with the social functions of group therapy (e.g. camaraderie, being around others with similar experiences) than the specific treatment modalities with which they were engaged. As such, examination of alliance among group therapy members is an important topic for further study.
Understanding alliance in group therapy
Several studies across a range of presenting problems have found that group alliance is positively associated with improved outcomes (e.g., Crowe & Grenyer, 2008; Joyce, Piper, & Ogrodniczuk, 2007; Taft, Murphy, King, Musser, & DeDeyn, 2003; Tasca & Lampard, 2012), although some other studies have failed to find a significant relationship (e.g., Oei & Browne, 2006; Woody & Adessky, 2002). Although the connection between alliance and treatment outcome in group therapy has been frequently studied, the process by which alliance among group members changes during the course of treatment has been rarely examined, despite the fact that one would expect this important interpersonal variable to be dynamic rather than static over time. Notably, the process by which alliance between patients and therapists in group settings (as opposed to alliance among the members of the group) changes over time and the relationships of this change to outcomes has been examined both from the perspective of the patient as well as from the perspective of the therapists. Findings have highlighted positive associations with outcomes, with influential factors including the timing and frequency of assessments as well as whether the patient or therapist rate the alliance (Horvath & Greenberg, 1989; Piper, Ogrodniczuk, Lamarche, Hilscher, & Joyce, 2005). Across the few studies that have examined the pattern of alliance among group members themselves over the course of multiple sessions, the results have been inconsistent. Woody and Adessky (2002) studied change in group alliance (termed cohesion in this study) in the context of a cognitive-behavioral therapy for social phobia and found that group alliance did not change over time. Lo Coco, Gullo and Kivlighan (2012) measured group alliance monthly in five groups over the course of long-term treatment in an Italian sample (n = 30). The authors examined an individual group member’s alliance ratings, other group member’s alliance ratings, and distress symptoms. Distress decreased along with increases in group alliance scores when both the individual and other group members were in agreement about alliance to the group as a whole. As noted by Joyce et al. (2007), further examinations of the development and impact of the alliance among group members, as has been highlighted between group member-therapist dyads, is indicated.
Understanding how the alliance changes throughout treatment, and what variables predict these changes, may allow clinicians and treatment developers to more effectively enhance this critical “common factor” (Castonguay, Constantino, Boswell & Kraus, 2010). Most explorations of the shape of alliance change have been done in the context of individual treatment, although no consistent results have emerged. Rather, a great number of patterns have been identified across different studies, including no growth (stable alliance), linear and increasing, linear and decreasing, quadratic (U-shaped), inverted-U-shaped, etc. (Constantino & Smith-Hansen, 2008; Kivlighan & Shaughnessy, 2000). Replicating any one pattern of results has been difficult; for example, Stiles et al. (2004) attempted to replicate and extend the finding by Kivlighan and Shaughnessy (2000) of three distinct alliance growth patterns, including a U-shaped pattern which was particularly associated with positive treatment outcomes. However, Stiles and colleagues (2004) instead identified four distinct alliance growth patterns, none of which was U-shaped; only a subset of patients with a V-shaped trajectory (a rupture-repair sequence) experienced differentially improved outcomes.
Across the studies of alliance change in treatment, the diversity of patterns may be attributable to the wide range of methods used in previous work (e.g., differing alliance scales and frequency of assessment) obscuring the true patterns of change. Additionally, there are individual and treatment-level factors that may contribute to both initial alliance levels as well as the overall trajectory of alliance development in treatment. For example, patient expectations of improvement and levels of symptom severity predict alliance ratings and alliance growth (Connolly Gibbons et al., 2003; Constantino et al., 2005). Given the established importance of the alliance in therapeutic work, identification of such salient variables may help clinicians identify situations where the alliance has the potential to be less robust and work to mitigate them.
Alliance in group treatments for PTSD
Individuals with posttraumatic stress disorder (PTSD) are perhaps particularly likely to have difficulty developing a robust therapeutic alliance. These patients often struggle considerably with social isolation, feelings of alienation, and difficulties with trust in most, if not all relationships (Brewin, Andrews, & Valentine, 2000). Such difficulties are often a barrier to individuals accessing and engaging in treatment. Group therapy has been found to provide an opportunity for these individuals to reduce social isolation and begin to build trust in a context in which symptoms are normalized and shared by other members in the group (Foy et al., 2000). Group therapy has been a mode of treatment for trauma-related problems as far back as the 1960s (Foy et al., 2000) and today represents one of the most prevalent treatment modalities for PTSD, particularly among veterans (Kingsley, 2007). Given the theoretical and empirical support for the importance of social connection in group treatment for PTSD, it is especially important to examine the alliance that group members develop with each other. Ellis et al. (2014) found that alliance among veterans with PTSD participating in group CPT was associated with outcome; however, alliance was measured posttreatment and not assessed over the course of the group. We therefore sought to examine the trajectory of change in alliance among this difficult-to-treat patient population.
Does alliance vary depending on the type of group treatment?
In addition to examining the overall shape of change in alliance during group treatment for PTSD, we recognized that treatment type is one variable that may impact alliance. Specifically, it is possible that the type of group treatment may impact alliance development over time. For instance, treatments that focus on skill building may not foster as much group alliance as groups that focus on building social support within the group. In an example from the individual treatment literature, Constantino and Smith-Hansen (2008) found that patients with bulimia nervosa who received interpersonal therapy demonstrated greater alliance growth compared to patients who received cognitive-behavioral therapy. Unfortunately, most studies of group alliance have focused only on a single treatment condition, rather than comparing alliance levels across treatments within the same study. Some preliminary evidence for the idea that group treatment conditions may differ in the level of alliance they evoke comes from a comparison between group cognitive behavioral therapy (GCBT) with group psychodynamic interpersonal psychotherapy (GPIP) in women with binge-eating disorder; in that study, ratings of group alliance were significantly higher for GCBT compared to GPIP (Tasca, Balfour, Ritchie, & Bissada, 2007). However, these results alone are insufficient for our understanding of how different group treatments may foster different levels of alliance initially or, as was found by Constantino and Smith-Hansen (2008), whether the rate of change in alliance differs as the treatments progress.
The impact of interpersonal trauma
Recent distinctions between different types of trauma and their potential differential trajectories for recovery suggest that this factor may also impact the development of alliance. One particular distinction differentiates between interpersonal forms of trauma and non-interpersonal forms of trauma. Interpersonal trauma is typically defined as events in which an individual is personally assaulted or violated by another human being. Interpersonal trauma includes sexual assault, intimate partner violence, and child physical or sexual abuse.Non-interpersonal forms of trauma include fires, disasters, and motor vehicle accidents. Research has found that individuals who experience interpersonal trauma tend to have greater psychosocial consequences as well as greater risk for PTSD (Ford, Stockton, Kaltman, & Green, 2006; Luthra et al., 2009). Chung and Breslau (2008) found that survivors of assaultive (interpersonal) violence reported higher levels of PTSD symptoms, especially emotional numbing and exaggerated startle response, than those who experienced other types of traumatic events. It is understandable that individuals who have experienced an interpersonal violation may have difficulty connecting with others and may intentionally withdraw from social connections. These responses have clear consequences: the avoidance and numbing symptoms of PTSD have strong negative correlations with relationship quality (Riggs, Byrne, Weathers, & Litz, 1998). Notably, while the distinction between interpersonal and non-interpersonal trauma seems to have clear implications for the functioning and psychopathology of survivors, the degree to which it impacts therapeutic processes such as alliance has yet to be examined. However, work across many different diagnoses (largely in individual treatments) has shown that patients with a hostile or domineering interpersonal stance unsurprisingly struggle to form an alliance in therapy (Puschner, Bauer, Horowitz, & Kordy, 2005; Saunders, 2001), as do patients with generally high levels of interpersonal distress (Beretta et al., 2005; Connolly Gibbons et al., 2003).
Current aims
In light of these important questions regarding group alliance, we examined baseline levels of alliance, as well as change in alliance over time, in the context of a clinical trial of two group treatments for PTSD in veterans (Sloan, Unger, & Beck, 2016). The outcomes for PTSD symptoms in that trial are described elsewhere (Sloan, Unger, Lee, & Beck, under review). We focused the present study on the alliance itself and on factors we hypothesized might affect alliance. As noted, the alliance-outcome link has been extensively studied (e.g., Horvath et al., 2011); more recent research has begun to focus on the interactions between alliance and individual or process variables, allowing for a more contextualized understanding. Although most of the work examining the determinants and mechanisms of alliance itself has been conducted in individual therapy (e.g., Connors et al., 2000; Diamond et al., 1999; Fitzpatrick & Irannejad, 2008; Tsai, Ogrodniczuk, Sochting, & Mirmiran, 2014), a smaller number of studies have tested the development of the alliance in group treatment. For example, Taft et al. (2004) found that high readiness to change, self-referral to therapy, married status, older age, and higher income were all associated with stronger working alliance (as measured at a single time point) among men in group treatment for intimate partner violence. By understanding in detail the factors that impact the alliance, clinicians can maximize this important therapeutic variable by using alliance-fostering techniques (e.g., Crits-Christoph, Connolly Gibbons, Narducci, Schamberget, & Gallop, 2005) and addressing ruptures in alliance as they occur (Safran & Muran, 2000). If research reveals that particular treatment activities facilitate a stronger connection, these can be liberally incorporated into the therapeutic process.
In the current study, we were interested in the role of treatment type and interpersonal trauma. We examined whether the two treatments differed in their baseline levels of alliance or in alliance growth over time; as the literature in this area is not yet robust, we did not propose an a priori hypothesis. Furthermore, as difficulties with trust and social isolation have been described as core interpersonal consequences of chronic PTSD (Clapp & Beck, 2009; King et al., 2006), we hypothesized that those individuals who have PTSD as a result of interpersonal trauma would have both lower initial levels of alliance and a reduced rate of alliance growth over time compared to group members who have PTSD as a result of non-interpersonal trauma. Finally, given the large variety of alliance trajectories supported in individual treatment research (e.g., Constantino & Smith-Hansen, 2008; Stiles et al., 2004) and the relative dearth of trajectories that have been identified in group treatment, we did not propose an a priori hypothesis regarding the shape of alliance change overall in our sample, but instead tested three potential patterns (linear, quadratic, and cubic).
Method
Participants
Participants were 198 male veterans recruited at two VA Medical Centers in the Northeast United States; all study procedures were approved by the Institutional Review Boards at each site and the trial was registered through ClinicalTrials.gov (NCT01544088). Participants were recruited in “waves” of 12-16 individuals to allow for group formation, as part of a study comparing two group-based treatments for PTSD. Inclusion criteria for the study were a current diagnosis of PTSD as determined by the Clinician-Administered PTSD Scale for DSM-5 (CAPS-5; Weathers et al., in press), and a stable regimen of psychiatric medications (if any) of at least 30 days. Exclusion criteria were a current diagnosis of substance dependence, psychosis, or unstable bipolar disorder, or significant cognitive impairment. Additionally, participants were excluded if they were currently receiving psychosocial treatment targeting PTSD, or if they had previously received an adequate dose of exposure-based PTSD treatment (e.g., 8 sessions or more). Following a baseline assessment to determine eligibility, participants were randomized to one of the two treatment conditions, each lasting for 14 sessions over 16 weeks (Sloan, Unger, & Beck 2016). The average group size was 6.60 individuals.
Participant study flow can be seen in Figure 1; only those participants who completed at least one CALPAS assessment were included in the present analyses, giving a sample size of 178 for the present study. The average age of participants was 56.04 (SD = 11.97), and they were largely Caucasian (73.4%) with a minority of African-American (17.5%) and other races (9.1%). Additional sample demographics are presented in Table 1.
Figure 1.
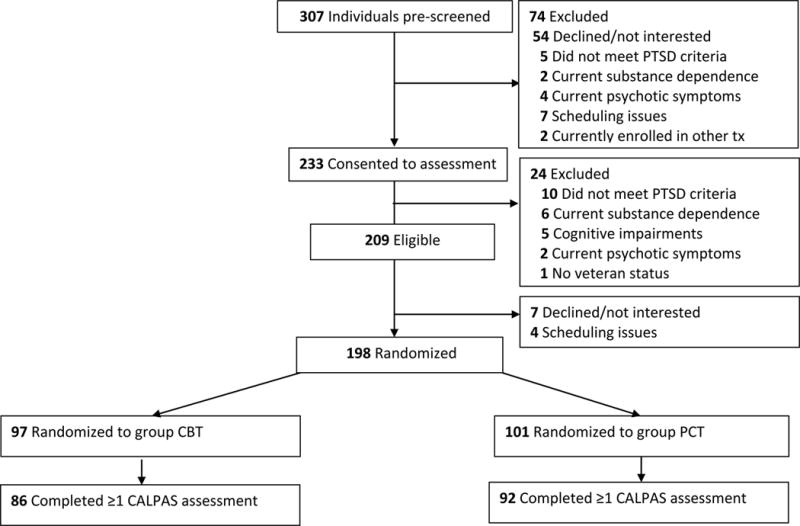
Participant flow
Table 1.
Baseline demographics and severity across the sample
| All (N = 178) |
GPCT (n = 92) |
GCBT (n = 86) |
t or χ2 | |
|---|---|---|---|---|
| Age | 56.04 (11.97) | 57.66 (12.10) | 54.30 (11.66) | 1.885 |
| Caucasian | 73.4% | 70.7% | 75.6% | .548 |
| Hispanic | 7.1% | 8.7% | 4.7% | 1.156 |
| 12+ years education | 20.2% | 18.5% | 22.1% | .360 |
| CAPS-5 | 39.56 (9.72) | 39.22 (9.82) | 39.93 (9.65) | −.488 |
| Interpersonal index event | 14.61% | 16.30% | 12.79% | .440 |
| CALPAS session 2 | 124.45 (20.56) | 125.89 (18.67) | 122.96 (22.36) | .387 |
| CALPAS session 14 | 133.97 (18.93) | 131.64 (19.11) | 136.96 (18.42) | .115 |
Notes. GPCT = Group Present-Centered Therapy; GCBT = Group Cognitive Behavior Therapy; CAPS-5 = Clinician-Administered PTSD Scale version 5; CALPAS = California Psychotherapy Alliance Scales for Group.
Treatment conditions
Group Cognitive Behavior Therapy (GCBT; Beck & Coffey, 2005) focuses on stabilization of symptoms, facing traumatic events directly, habituating responses to memories of the trauma and its aftermath, cognitive restructuring, increasing social supports and connection, and encouraging positive emotion associated with pleasant activities. Each group session lasts two hours and includes check-in, review of practice assignments, a mindfulness exercise, a review of between session practice assignments, introduction and practice of new material, and check out. At the beginning of each group, members state their first names, pledge their confidentiality to the group and report their subjective units of distress (SUDS) rating. At the end of each session, group members check out by sharing what they got from group and reporting their SUDS.
GCBT conceptualizes PTSD into 4 symptom clusters: physical (e.g. hyperarousal), cognitive (e.g., intrusive memories, thoughts), behavioral (e.g., avoidance), and emotional (e.g., numbing, anger) and targets each of these directly through relaxation training, cognitive therapy, behavioral practice (developing a hierarchy of feared situations, in vivo exposure, written exposure), addressing emotions, and relapse prevention. The therapist’s role is to be a coach who both understands and acknowledges the struggles of each group member and who also encourages group members to push themselves to engage in assignments that are difficult and to help each other. Group members do not discuss details of the traumatic event in group, but do share their responses to the exposures with each other.
Present-Centered Therapy (PCT) is a manual-based intervention that was initially developed as a treatment control condition for PTSD randomized controlled treatment studies (Schnurr et al., 2003). The protocol has now been used in multiple PTSD randomized controlled trials (e.g., McDonagh et al., 2005; Schnurr et al., 2003; Surís, Link-Malcolm, Chard, Ahn, & North, 2013), including in a group format (Classen et al., 2011; Resick et al., 2015; Schnurr et al., 2003). The theoretical rationale for PCT is based on shifting maladaptive behavioral patterns in the present and examining the impact of trauma on the patient’s current life and functioning (Classen et al., 2011). A 2014 meta-analysis of clinical trials using PCT compared to evidence-based treatments for PTSD found that differences between the treatments on both primary and secondary outcome measures were not statistically significant (Frost, Laska, & Wampold, 2014).
The central elements of Group Present-Centered Therapy (GPCT) include psycho-education about the typical symptoms and features associated with PTSD in Veterans, particularly those affecting interpersonal relationships, and the use of group format to decrease isolation, normalize symptoms, provide the experience of giving and receiving support and feedback, and offer opportunities for positive interpersonal interactions. The focus of the group is increasing awareness of PTSD-related themes in the individual’s current life, and increasing the mastery and ability to cope with such issues. GPCT is relatively less structured than GCBT, with members of the group having more input into the agenda of the sessions. Although facilitators in this condition may assist with problem-solving among group members and provide suggestions and advice about coping with symptoms and stress, GPCT also does not include disclosure about, discussion of, or exposure to individual traumatic events, nor systematic training in the use of exposure-based techniques or challenging cognitions related to the traumatic event. Instead, the focus is on managing the sequelae of traumatic experiences in behavior and feelings in day-to-day life.
Both GCBT and GPCT were delivered by two-person therapist teams. A total of 19 therapists (male and female) delivered treatment over the course of the study, covering 30 separate groups of GCBT or GPCT. Pairings of therapists were not held constant, but instead were altered for virtually every group. Therapists were doctoral-level psychologists with five or more years of clinical experience, and were nested within treatment condition. Therapists were civilians in all cases.
Measures
PTSD diagnostic status and symptom severity were determined using the CAPS-5 (Weathers et al., in press), a structured diagnostic interview and the gold standard for measuring the severity of PTSD symptoms. A single 5-point ordinal rating scale (reflecting information regarding symptom frequency and intensity, as obtained by the interviewer) is used to measure the severity of each symptom. The CAPS-5 demonstrates high criterion and construct validity, and high correspondence with a self-report measure of PTSD (Weathers et al., in press).
Overall lifetime trauma experience was assessed using the Traumatic Life Events Checklist (TLEQ; Kubany et al., 2000). The TLEQ is a self-report questionnaire that assesses for lifetime exposure to a variety of potentially traumatic events. A total of 23 categories of potentially traumatic events, including a free-response “other” category, are presented. The participant indicates whether and how many times they have experienced each event in their lifetime, from 0 (“Never”) to 6 (“More than 5 times”). Participants also indicate which category of event is currently causing them the most distress; this is considered their index trauma. The TLEQ demonstrates good content validity, convergent validity, and test-retest reliability (Kubany et al., 2000).
Responses on the TLEQ were used to categorize participants’ index traumas as interpersonal (e.g., a rape or childhood physical abuse) or non-interpersonal (e.g., a motor vehicle accident or a natural disaster). Combat was categorized as a non-interpersonal trauma, consistent with previous research that has used TLEQ categories to determine the interpersonal nature of trauma (Lilly & Valdez, 2012; Lim, Adams, & Lilly, 2012; Orcutt, Pickett, & Pope, 2005). The determination to consider combat as a non-interpersonal trauma is due to the fact that it likely represents a very different type and context of trauma compared to, for example, a sexual assault. Both the CAPS-5 and the TLEQ were administered at baseline.
Alliance was measured using the California Psychotherapy Alliance Scales for Group (CALPAS-G; Gaston & Marmar, 1994), which consists of 24 Likert-scale items pertaining to the other group members (e.g., “Did you feel pressured by the group members to make changes before you were ready?” “Did you feel accepted and respected by the group members for who you are?” “Did you feel that you were working together with the group members, that you were joined in a struggle to overcome your problems?”) as well as reactions to the therapy (“Did you find yourself tempted to stop therapy when you were upset or disappointed with therapy?” “How much did you hold back your feelings during this session?”). Responses are made based on a 1 (“Not at all”) to 7 (“Very much so”) scale. The CALPAS is a frequently used measure of alliance that has shown good psychometric properties and adequate criterion-related validity (Gaston, 1991). The measure was administered at every other group session (seven administrations in total), beginning at session two. Cronbach’s alpha in the current sample was .871 at the first administration.
Analysis
All analyses were conducted using hierarchical linear modeling (HLM) with restricted maximum likelihood estimation in SPSS v.23 (IBM Corp., 2015). Across the seven CALPAS administration time points, 27% of the data were missing; however, HLM is well able to estimate models using incomplete data.
A series of 2-level nested models (sessions within person) were run:
A null (no predictors) model including only a fixed intercept effect and a random intercept effect. The covariance structure was identity.
- Growth models:
- A model including fixed effects for intercept, linear time, and quadratic time, as well as a random effect for intercept. Covariance structures were autoregressive (repeated effects at level 1) and identity (random effect at level 2). For both of the time effects, time was centered at session 2, when the CALPAS was first administered, and numbered either 0-6 (linear) or 0, 1, 4, etc. (quadratic) to correspond with CALPAS administration points.
- A model identical to 2a above but with cubic time rather than quadratic time.
- A model including fixed effects for only intercept and linear time, as well as random effects for intercept and linear time. Covariance structures were autoregressive (repeated effects at level 1) and unstructured (random effects at level 2).
A model including fixed effects for intercept, interpersonal versus non-interpersonal index trauma, and interpersonal trauma*time, as well as random effects for slope and intercept. Again, covariance structures were autoregressive at level 1 and unstructured at level 2.
Finally, a model including fixed effects for intercept, treatment condition (GCBT versus GPCT), and condition*time, as well as random effects for slope and intercept. As before, covariance structures were autoregressive at level 1 and unstructured at level 2.
Results
Sample characteristics
Baseline demographics and severity scores for the sample can be seen in Table 1. There were no significant differences between the two treatment conditions on any variable. In total, 26 individuals (14.61%) reported an interpersonal index event; the most commonly reported events, each of which was reported by six participants, were physical assault by a stranger and experiencing family violence. Interpersonal index events occurring in childhood were endorsed by eight participants, and rape was endorsed as the index event by three participants.
HLM models
First we ran a null (no predictor) model (Model A, Table 2), which revealed significant level 1 (within-person) variability as well as significant level 2 (between people) variability, with approximately two-thirds of the variance being between people. Next we examined possible shapes of a growth curve of time: linear, quadratic, or cubic time. When both linear and quadratic fixed effects were entered, the linear coefficient was significant (t(465.80) = 2.307, p = .021) while the quadratic coefficient was not significant (t(488.28) = 0.089, p = .929); the same result was found when entering both linear (t(401.26) = 3.470, p = .001) and cubic fixed effects (t(492.29) = 0.116, p = .908). Given these results, for all subsequent models only linear time was included. The growth model including only linear time (Model B, Table 2) showed a significant effect of time (b = 1.62, SE = .22, p = .000), indicating that alliance levels tended to increase by approximately 1.62 points on the CALPAS every-other session. Goodness-of-fit statistics indicated that the growth model was significantly better fitting than the null model (null model Baysian information criterion (BIC): 7440.96, −2 log likelihood(−2LL): 7427.32; growth model BIC: 7362.54, −2LL: 7328.45).
Table 2.
Hierarchical linear models of the effect of time, interpersonal index event, and treatment condition on initial alliance levels and change in alliance
| Parameter |
Model A Null |
Model B Growth |
Model C Interpersonal |
Model D Condition |
|
|---|---|---|---|---|---|
| Initial level | Intercept | 128.10** (1.30) |
123.72** (1.39) |
123.57** (1.51) |
125.36** (1.93) |
| Interpersonal | 1.01 (3.98) |
||||
| Condition | −3.41 (2.79) |
||||
|
| |||||
| Change | Time | 1.62** (0.22) |
1.56** (0.24) |
1.14** (0.29) |
|
| Inter*time | 0.49 (0.68) |
||||
| Cond*time | 1.05* (0.44) |
||||
|
| |||||
| Variance | Within | 121.73** (6.34) |
101.83** (8.06) |
102.99** (8.10) |
102.83** (8.01) |
| Between (intercept) | 270.17** (32.18) |
272.12** (37.01) |
273.86** (37.32) |
272.23** (37.07) |
|
| Between (slope) | 2.48* (1.01) |
2.50* (1.01) |
2.24* (0.98) |
||
| Intercept-slope covariance | −4.91 (4.76) |
−5.29 (4.81) |
−4.64 (4.68) |
||
|
| |||||
| Goodness-of-fit | −2LL | 7427.32 | 7328.45** | 7322.10 | 7318.79** |
| BIC | 7440.96 | 7362.54 | 7356.18 | 7352.87 | |
Notes. −2LL = −2 log likelihood; BIC = Bayesian information criterion. Interpersonal index event was not significant for either initial alliance level or change in alliance over time. Treatment condition was not significant for initial alliance level, but was significant for change in alliance over time.
p > .05,
p > .001
The next model included the interpersonal index event and the cross-level interaction between interpersonal index event and time (Model C, Table 2). Both were nonsignificant (interpersonal b = 1.01, SE = 3.98, p = .799; interpersonal*time b = .49, SE = .68, p = .469), and goodness-of-fit was not significantly improved by the inclusion of the new variables (growth model BIC: 7362.54, −2LL: 7328.45; interpersonal model BIC: 7356.18, −2LL: 7322.10). This indicated that an interpersonal index event, compared to a noninterpersonal index event, did not significantly impact either initial alliance ratings or change in alliance over time.
The final model included treatment condition and the cross-level interaction between condition and time (Model D, Table 2). There was a significant condition by time interaction (b = 1.06, SE = .44, p = .018), indicating that while there was no significant difference between the two conditions in initial alliance ratings (b = −3.41, SE = 2.79, p = .223), the CBT condition was associated with a significantly greater rate of alliance growth over time. Goodness-of-fit was significantly improved by the addition of the treatment condition variables, relative to the pure growth model (growth model BIC: 7362.54, −2LL: 7328.45; condition model BIC: 7352.87, −2LL: 7318.79).
Regarding the random effects of slope and intercept, across all models both intercept and slope were consistently found to vary significantly between people. However, again across all models, the variances of intercept and slope were not significantly correlated at level 2, indicating that initial alliance levels were not related to change in alliance over time1.
Discussion
The findings showed that there is significant variability across alliance ratings in group PTSD treatment, both within and between individuals. We found significant growth in group alliance across treatment for both conditions, although the rate of alliance growth was more rapid for participants in the GCBT condition. The two treatments did not differ with regard to initial alliance levels at session 2. Whether an individual reported that their index trauma was of an interpersonal or non-interpersonal nature did not significantly impact either their initial alliance to the group or the change in alliance over time. Across the entire sample, initial group alliance levels were not significantly related to changes in those levels across treatment.
In light of our results, it is useful to consider the findings of Tasca et al. (2007), who compared GCBT and group psychodynamic interpersonal psychotherapy (GPIP) for binge eating disorder. They found that group members in the GCBT condition reported significantly higher alliance levels on the CALPAS across all sessions of treatment. The authors hypothesized that this was because the GPIP condition focused on direct examination of maladaptive interpersonal patterns as they were manifested in the group environment, resulting in more personally challenging interactions. However, in the current study the GPCT condition did not involve this type of direct discussion of interpersonal patterns among group members, yet the GCBT group still experienced more rapid increases in alliance.
We propose that, in the present study, the GCBT condition promoted faster growth in alliance to the group via the tasks and focus of the therapy itself. GCBT participants were strongly encouraged to work through a variety of in vivo exposures as homework, and to report back to the group on their successes and difficulties. Such open disclosure and collaboration may have more quickly drawn the group members together and given them a shared sense of purpose. Empirical findings from the social psychology literature have suggested that sharing a novel or difficult experience with another person can result in greater levels of disclosure, liking, and relationship satisfaction (e.g., Aron, Norman, Aron, McKenna, & Heyman, 2000; Latané, Eckman, & Joy, 1966), and the group processing and planning for between-session exposures may have facilitated a similar response among the GCBT members. Discussion of day-to-day difficulties in GPCT did not require systematic sharing of new challenges as part of each session. Thus, it may have been easier for GPCT group members to avoid revealing meaningful struggles and to forestall deeper conversation, and this may have contributed to the slower growth in alliance for this group. Perhaps it would be possible to develop another mechanism for GPCT participants to select and report back to the group on novel or challenging experiences. For example, group members could select a goal that is consistent with improving their current quality of life and pushing themselves to take on a new role (e.g., signing up for community college classes, volunteering as a Little League coach). The sharing of progress towards these goals, and being held accountable by the group each week, might serve a similar alliance-building function as the exposure hierarchy in GCBT.
Contrary to our hypothesis, individuals with an interpersonal index trauma were not negatively impacted in terms of their group alliance levels or growth. Although much previous research suggests that interpersonal trauma is particularly damaging in terms of PTSD symptoms (Chung & Breslau, 2008; Forbes et al., 2011; Jakob, Lamp, Rauch, Smith, & Buchholz, 2017; Norris, 1992), it is promising that on the whole, participants whose index traumas were classified as interpersonal were not systematically hampered in their ability to form connections with fellow group members.
It may be the case that, rather than the interpersonal/non-interpersonal index trauma distinction, other interpersonal variables are more salient in terms of predicting alliance development. Specifically, a line of research has developed that explores the role of attachment style in predicting alliance levels and growth in alliance throughout group treatment. Several groups have reported that attachment insecurity and attachment avoidance are associated with distinct patterns in alliance development (Chen & Mallinckrodt, 2002; Kanninen, Salo, & Punamäki, 2000). In a finding that highlights the layered nature of alliance formation, Tasca and colleages (2007) found that patients’ attachment styles moderated their rate of alliance growth in a psychodynamically-oriented group treatment (GPIP) but not in GCBT. The interactions among patient, group, therapist, and treatment factors that combine to produce the alliance (both at a single timepoint and as a dynamically evolving variable) are complex.
Encouragingly, we found that initial alliance levels were not statistically correlated with individuals’ later growth in alliance. These findings underscore that participants’ initial impressions of their connection to the group do not necessarily predict their eventual bond with others. Group members who initially appear aloof or unfriendly may nonetheless develop strong connections over time.
The present study had several limitations. First, our decision to consider combat as a non-interpersonal trauma, while consistent with prior research, may not be accurate in all cases. It is likely that the impact of a traumatic combat exposure for an individual may depend on the facts of the situation (e.g., an air raid strike versus a single suicide bomber, an enemy attack versus a “friendly fire” accident), as well as the individual’s appraisals regarding the event (e.g., “It was our side against theirs” versus “My superiors made bad decisions that cost us lives.”). We did not have access to sufficiently detailed information regarding every participant’s combat trauma in order to make a more nuanced determination of the nature of the event. Second, our analysis of the role of interpersonal compared to non-interpersonal events focused on the participant’s index trauma, but virtually every patient in our sample reported multiple potentially traumatic events on the TLEQ, and almost all reported at least one event that was interpersonal in nature. This broad exposure to interpersonal trauma in our sample may account for the finding that interpersonal index events did not impact group alliance; alternatively, as noted above, cognitive schemas such as attachment style may better predict alliance development. Third, we limited our examination of alliance to group members’ ratings of their alliance with the group, and did not include examinations of group members’ ratings with other individual members or with their therapist(s), nor therapists’ ratings of any of these alliances. While such additional examinations of relationship factors and perspectives would be interesting to compare, and some studies have begun to examine such differences (e.g. Joyce, Piper, & Ogrodnizcuk, 2007), we were limited in what alliance data were collected in this sample. Additionally, there is reason to believe that the degree to which Veterans with chronic PTSD in particular feel connected to other group members is especially relevant to the effectiveness of the group and their recovery (Brewin, Andrews, & Valentine, 2000; Foy, 2000). Regarding generalizability, our sample was entirely male and largely White, which is reflective of the majority of the VA patient population but may not correspond to other highly traumatized populations. Relatedly, our sample was comprised exclusively of veterans, a group with notable challenges compared to the general population in terms of their physical health (Hoge, Terhakopian, Castro, Messer, & Engel, 2007), mental health (Seal, Bertenthal D, Miner, Sen, & Marmar, 2007), and socioeconomic status (Teachman & Call, 1996). They may also have unique preferences with regard to treatment approaches, which could in turn have influenced our results related to treatment format. All of these factors limit the broader applicability of our findings. Finally, we were unfortunately missing approximately one-quarter of the CALPAS data. Although HLM is considered an excellent choice for analysis when data are missing (Bickel 2007), it is possible that these missing values have biased our results and impact the inferences that may be drawn from them.
Despite these limitations, the findings contribute to our understanding of group process during the course of group therapy for PTSD. The present study is one of the first to examine predictors of and change over time in group alliance, and the large sample size is a significant advance relative to previous smaller studies of alliance in group treatment. To continue building on these results, future studies should continue to explore factors that may contribute to alliance (both initially and throughout treatment), and also to explore the pattern of change by incorporating repeated assessments. Subsequent studies might also include a focus on other types of alliance, such as the patient-therapist alliance in group treatment, and whether this develops in ways that are similar or different to the patient-group alliance.
Our findings indicate that the distinction between interpersonal and non-interpersonal trauma used in this study was not predictive of a group member’s connection with fellow participants. The results also highlight the potential impact of group activities that promote sharing of hardships and challenges to quickly generate bonds among group members. Findings such as these suggest that our group treatments can be modified in ways that may maximize the development of alliance, therefore increasing their efficacy, efficiency, and value.
Acknowledgments
This work was supported by the United States (U.S.) Department of Veterans Affairs under Merit Review Award # 1 IO1 CX000467. The first author was supported by the U.S. Department of Veterans Affairs (Clinical Sciences Research and Development Service) under Career Development Award # IK2 CX001589. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the U.S. Department of Veterans Affairs or the U.S. government.
Footnotes
Disclosure: The authors report no conflicts of interest.
In addition to the 2-level models presented here, we also conducted a series of 3-level models (sessions within person within group). We found minimal clustering at the group level (unconditional ICC for initial alliance ratings = .065, design effect = 1.33) (Bickel, 2007; Muthén & Satorra, 1995; Snijders & Bosker, 1999). Models conducted with 3 levels were consistent with the 2-level results, although with slightly higher p-values reflecting the decreased degrees of freedom. For the model including condition and condition*time (Model D), the significance of the condition*time fixed effect was reduced from p=0.018 in the 2-level model to p=0.053 in the 3-level model. Comparison of BIC values indicated that the 2-level Model D demonstrated a “very strong” improvement in fit over the 3-level Model D (2-level BIC = 7352.87; 3-level BIC = 7366.92; Raftery, 1995)
References
- Aron A, Norman CC, Aron EN, McKenna C, Heyman RE. Couples’ shared participation in novel and arousing activities and experienced relationship quality. Journal of Personality and Social Psychology. 2000;78(2):273–284. doi: 10.1037//0022-3514.78.2.273. https://doi.org/10.1037/0022-3514.78.2.273. [DOI] [PubMed] [Google Scholar]
- Barlow SH, Burlingame GM. Essential theory, process, and procedures for successful group therapy: Group cohesion as an exemplar. Journal of Contemporary Psychotherapy. 2006;36:107–112. https://doi.org/http://dx.doi.org.ezproxy.library.uwa.edu.au/10.1007/BF02729053. [Google Scholar]
- Beck JG, Coffey SF. Group cognitive behavioral treatment for PTSD: Treatment of motor vehicle accident survivors. Cognitive and Behavioral Practice. 2005;12:267–277. doi: 10.1016/s1077-7229(05)80049-5. https://doi.org/10.1016/S1077-7229(05)80049-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beretta V, de Roten Y, Drapeau M, Kramer U, Favre N, Despland J. Clinical significance and patients’ perceived change in four sessions of brief psychodynamic intervention: Characteristics of early responders. Psychology and Psychotherapy: Theory, Research and Practice. 2005;78:347–362. doi: 10.1348/147608305X25766. https://doi.org/10.1348/147608305X25766. [DOI] [PubMed] [Google Scholar]
- Bickel R. Multilevel analysis for applied research: It’s just regression! New York, NY: The Guilford Press; 2007. [Google Scholar]
- Brewin CR, Andrews B, Valentine JD. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. Journal of Consulting and Clinical Psychology. 2000;68(5):748–766. doi: 10.1037//0022-006x.68.5.748. https://doi.org/10.1037/0022-006X.68.5.748. [DOI] [PubMed] [Google Scholar]
- Burlingame GM, MacKenzie KR, Strauss B. Small group treatment: Evidence for effectiveness and mechanisms of change. In: Lambert M, editor. Bergin and Garfield’s Handbook of Psychotherapy and Behavior Change. New York: Wiley; 2003. pp. 647–696. [Google Scholar]
- Burlingame GM, McClendon DT, Alonso J. Cohesion in group therapy. Psychotherapy. 2011;48:34–42. doi: 10.1037/a0022063. https://doi.org10.1037/a0022063. [DOI] [PubMed] [Google Scholar]
- Castonguay LG, Constantino MJ, Boswell JF, Kraus D. The therapeutic alliance: Research and theory. In: Horowitz L, Strack S, editors. Handbook of interpersonal psychology: Theory, research, assessment, and therapeutic interventions. New York, NY: Wiley; 2010. pp. 509–518. [Google Scholar]
- Chen EC, Mallinckrodt B. Attachment, group attraction, and self-other agreement in interpersonal circumplex problems and perceptions of group members. Group Dynamics. 2002;6:311–324. http://dx.doi.org/10.1037/1089-2699.6.4.311. [Google Scholar]
- Chung H, Breslau N. The latent structure of post-traumatic stress disorder: tests of invariance by gender and trauma type. Psychological Medicine. 2008;38:563–573. doi: 10.1017/S0033291707002589. https://doi.org/10.1017/s0033291707002589. [DOI] [PubMed] [Google Scholar]
- Clapp JD, Beck JG. Understanding the relationship between PTSD and social support: The role of negative network orientation. Behaviour Research and Therapy. 2009;47:237–244. doi: 10.1016/j.brat.2008.12.006. https://doi.org/10.1016/j.brat.2008.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Classen CC, Palesh OG, Cavanaugh CE, Koopman C, Kaupp JW, Kraemer HC, Spiegel D. A comparison of trauma-focused and present-focused group therapy for survivors of childhood sexual abuse: A randomized controlled trial. Psychological Trauma: Theory, Research, Practice, and Policy. 2011;3(1):84–93. https://doi.org/10.1037/a0020096. [Google Scholar]
- Connolly Gibbons MB, Crits-Christoph P, de la Cruz C, Barber JP, Siqueland L, Gladis M. Pretreatment expectations, interpersonal functioning, and symptoms in the prediction of the therapeutic alliance across supportive-expressive psychotherapy and cognitive therapy. Psychotherapy Research. 2003;13:59–76. doi: 10.1093/ptr/kpg007. http://dx.doi.org/10.1093/ptr/kpg007. [DOI] [PubMed] [Google Scholar]
- Connors GJ, DiClemente CC, Dermen KH, Kadden R, Carroll KM, Frone MR. Predicting the therapeutic alliance in alcoholism treatment. Journal of Studies on Alcohol and Drugs. 2000;61:139–149. doi: 10.15288/jsa.2000.61.139. https://doi.org/10.15288/jsa.2000.61.139. [DOI] [PubMed] [Google Scholar]
- Constantino MJ, Arnow BA, Blasey C, Agras WS. The association between patient characteristics and the therapeutic alliance in cognitive-behavioral and interpersonal therapy for bulimia nervosa. Journal of Consulting and Clinical Psychology. 2005;73:203–211. doi: 10.1037/0022-006X.73.2.203. http://dx.doi.org/10.1037/0022-006X.73.2.203. [DOI] [PubMed] [Google Scholar]
- Constantino M, Smith-Hansen L. Patient interpersonal factors and the therapeutic alliance in two treatments for bulimia nervosa. Psychotherapy Research. 2008;18:683–698. doi: 10.1080/10503300802183702. http://dx.doi.org/10.1080/10503300802183702. [DOI] [PubMed] [Google Scholar]
- Crits-Christoph P, Connolly Gibbons MB, Narducci J, Schamberger M, Gallop R. Interpersonal problems and the outcome of interpersonally oriented psychodynamic treatment of GAD. Psychotherapy: Theory, Research, Practice, Training. 2005;42:211–224. http://dx.doi.org/10.1037/0033-3204.42.2.211. [Google Scholar]
- Crowe TP, Grenyer BFS. Is therapist alliance or whole group cohesion more influential in group psychotherapy outcomes? Clinical Psychology & Psychotherapy. 2008;15(4):239–246. doi: 10.1002/cpp.583. https://doi.org/10.1002/cpp.583. [DOI] [PubMed] [Google Scholar]
- Diamond GM, Liddle HA, Hogue A, Dakof GA. Alliance-building interventions with adolescents in family therapy: A process study. Psychotherapy. 1999;36:355–368. http://dx.doi.org/10.1037/h0087729. [Google Scholar]
- Ellis CC, Peterson M, Bufford R, Benson J. The importance of group cohesion in inpatient treatment of combat-related PTSD. International Journal of Group Psychotherapy. 2014;64(2):208–226. doi: 10.1521/ijgp.2014.64.2.208. https://doi.org/10.1521/ijgp.2014.64.2.208. [DOI] [PubMed] [Google Scholar]
- Fitzpatrick MR, Irannejad S. Adolescent readiness for change and the working alliance in counseling. Journal of Counseling and Development. 2008;86:438–445. doi: 10.1002/j.1556-6678.2008.tb00532.x. [DOI] [Google Scholar]
- Forbes D, Fletcher S, Parlow R, Phelps A, O’Donnell M, Bryant RA, Creamer M. Trauma at the hands of another: Longitudinal study of differences in the posttraumatic stress disorder symptom profile following interpersonal compared with noninterpersonal trauma. The Journal of Clinical Psychiatry. 2011;73:372–376. doi: 10.4088/JCP.10m06640. https://doi.org/10.4088/JCP.10m06640. [DOI] [PubMed] [Google Scholar]
- Ford JD, Stockton P, Kaltman S, Green BL. Disorders of extreme stress (DESNOS) symptoms are associated with type and severity of interpersonal trauma exposure in a sample of healthy young women. Journal of Interpersonal Violence. 2006;21(11):1399–1416. doi: 10.1177/0886260506292992. https://doi.org/10.1177/0886260506292992. [DOI] [PubMed] [Google Scholar]
- Foy DW, Glynn SM, Schnurr PP, Jankowski MK, Wattenberg MS, Weiss DS, Gusman FD. Group therapy. In: Foa EB, Keane TM, Friedman MJ, editors. Effective treatments for PTSD: Practice guidelines from the International Society for Traumatic Stress Studies. New York, NY, US: Guilford Press; 2000. pp. 336–338. [Google Scholar]
- Frost ND, Laska KM, Wampold BE. The evidence for Present-Centered Therapy as a treatment for posttraumatic stress disorder. Journal of Traumatic Stress. 2014;27(1):1–8. doi: 10.1002/jts.21881. https://doi.org/10.1002/jts.21881. [DOI] [PubMed] [Google Scholar]
- Gaston L. Reliability and criterion-related validity of the California Psychotherapy Alliance Scales—patient version. Psychological Assessment: A Journal of Consulting and Clinical Psychology. 1991;3(1):68–74. https://doi.org/10.1037/1040-3590.3.1.68. [Google Scholar]
- Gaston L, Marmar CR. The California Psychotherapy Alliance Scales. In: Horvath AO, Greenberg LS, editors. The Working Alliance: Theory, Research, and Practice. New York: Wiley; 1994. pp. 85–108. [Google Scholar]
- Hoge CW, Terhakopian A, Castro CA, Messer SC, Engel CC. Association of Posttraumatic Stress Disorder With Somatic Symptoms, Health Care Visits, and Absenteeism Among Iraq War Veterans. American Journal of Psychiatry. 2007;164(1):150–153. doi: 10.1176/ajp.2007.164.1.150. https://doi.org/10.1176/ajp.2007.164.1.150. [DOI] [PubMed] [Google Scholar]
- Holmes SE, Kivlighan DM. Comparison of therapeutic factors in group and individual treatment processes. Journal of Counseling Psychology. 2000;47(4):478–484. https://doi.org/10.1037/0022-0167.47.4.478. [Google Scholar]
- Horvath AO. Research on the alliance. In: Horvath AO, Greenberg LS, editors. The Working Alliance: Theory, Research, and Practice. New York: Wiley; 1994. pp. 259–286. [Google Scholar]
- Horvath AO, Del Re AC, Flückiger C, Symonds D. Alliance in individual psychotherapy. Psychotherapy. 2011;48:9–16. doi: 10.1037/a0022186. http://dx.doi.org/10.1037/a0022186. [DOI] [PubMed] [Google Scholar]
- Horvath AO, Greenberg LS. Development and validation of the Working Alliance Inventory. Journal of Counseling Psychology. 1989;36:223–233. http://dx.doi.org/10.1037/0022-0167.36.2.223. [Google Scholar]
- Corp IBM. IBM SPSS Statistics for Windows. 2015 Version 23.0. [Google Scholar]
- Jakob J, Lamp K, Rauch SAM, Smith ER, Buchholz KR. The impact of trauma type or number of traumatic events on PTSD diagnosis and symptom severity in treatment seeking veterans. Journal of Nervous and Mental Disease. 2017;205:83–86. doi: 10.1097/NMD.0000000000000581. https://doi.org/10.1097/NMD.0000000000000581. [DOI] [PubMed] [Google Scholar]
- Joyce AS, Piper WE, Ogrodniczuk JS. Therapeutic alliance and cohesion variables as predictors of outcome in short–term group psychotherapy. International Journal of Group Psychotherapy. 2007;57(3):269–296. doi: 10.1521/ijgp.2007.57.3.269. https://doi.org/10.1521/ijgp.2007.57.3.269. [DOI] [PubMed] [Google Scholar]
- Kanninen K, Salo J, Punamäki RL. Attachment patterns and working alliance in trauma therapy for victims of political violence. Psychotherapy Research. 2000;10:435–449. doi: 10.1093/ptr/10.4.435. https://doi.org/10.1093/ptr/10.4.435. [DOI] [PubMed] [Google Scholar]
- King DW, Taft C, King LA, Hammond C, Stone ER. Directionality of the association between social support and posttraumatic stress disorder: A longitudinal investigation. Journal of Applied Social Psychology. 2006;36:2980–2992. https://doi.org/10.1111/j.0021-9029.2006.00138.x. [Google Scholar]
- Kingsley G. Contemporary group treatment of combat-related posttraumatic stress disorder. Journal of the American Academy of Psychoanalysis and Dynamic Psychiatry. 2007;35:51–69. doi: 10.1521/jaap.2007.35.1.51. https://doi.org/10.1521/jaap.2007.35.1.51. [DOI] [PubMed] [Google Scholar]
- Kivlighan DM, Jr, Shaughnessy P. Patterns of working alliance development: A typology of client’s working alliance ratings. Journal of Counseling Psychology. 2000;47:362–371. http://dx.doi.org/10.1037/0022-0167.47.3.362. [Google Scholar]
- Kubany ES, Haynes SN, Leisen MB, Owens JA, Kaplan AS, Watson SB, Burns K. Development and preliminary validation of a brief broad-spectrum measure of trauma exposure: the Traumatic Life Events Questionnaire. Psychological Assessment. 2000;12(2):210–224. doi: 10.1037//1040-3590.12.2.210. http://dx.doi.org/10.1037/1040-3590.12.2.210. [DOI] [PubMed] [Google Scholar]
- Latané B, Eckman J, Joy V. Shared stress and interpersonal attraction. Journal of Experimental Social Psychology. 1966;1(Supplement 1):80–94. https://doi.org/10.1016/0022-1031(66)90068-0. [Google Scholar]
- Lilly MM, Valdez CE. Interpersonal trauma and PTSD: The roles of gender and a lifespan perspective in predicting risk. Psychological Trauma: Theory, Research, Practice, and Policy. 2012;4(1):140–144. https://doi.org/10.1037/a0022947. [Google Scholar]
- Lim BH, Adams LA, Lilly MM. Self-worth as a mediator between attachment and posttraumatic stress in interpersonal trauma. Journal of Interpersonal Violence. 2012;27:2039–2061. doi: 10.1177/0886260511431440. https://doi.org.10.1177/0886260511431440. [DOI] [PubMed] [Google Scholar]
- Lo Coco G, Gullo S, Kivlighan DM. Examining patients’ and other group members’ agreement about their alliance to the group as a whole and changes in patient symptoms using response surface analysis. Journal of Counseling Psychology. 2012;59(2):197–207. doi: 10.1037/a0027560. https://doi.org/10.1037/a0027560. [DOI] [PubMed] [Google Scholar]
- Luthra R, Abramovitz R, Greenberg R, Schoor A, Newcorn J, Schmeidler J, Chemtob CM. The relationship between type of trauma exposure and posttraumatic stress disorder among urban children and adolescents. Journal of Interpersonal Violence. 2009;24:1919–1927. doi: 10.1177/0886260508325494. https://doi.org/10.1177/0886260508325494. [DOI] [PubMed] [Google Scholar]
- Makler S, Sigal M, Gelkopf M, Kochba BB, Horeb E. Combat-related, chronic posttraumatic stress disorder: Implications for group-therapy intervention. American Journal of Psychotherapy. 1990;44(3):381–395. doi: 10.1176/appi.psychotherapy.1990.44.3.381. [DOI] [PubMed] [Google Scholar]
- Martin DJ, Garske JP, Davis KM. Relation of the therapeutic alliance with outcome and other variables: A meta-analytic review. Journal of Consulting and Clinical Psychology. 2000;68(3):438–450. https://doi.org/10.1037/0022-006X.68.3.438. [PubMed] [Google Scholar]
- McDonagh A, Friedman M, McHugo G, Ford J, Sengupta A, Mueser K, Descamps M. Randomized trial of cognitive- behavioral therapy for chronic posttraumatic stress disorder in adult female survivors of childhood sexual abuse. Journal of Consulting and Clinical Psychology. 2005;73:515–524. doi: 10.1037/0022-006X.73.3.515. https://doi.org/10.1037/0032-006X.73.3.515. [DOI] [PubMed] [Google Scholar]
- Muthén BO, Satorra A. Complex sample data in structural equation modeling. Sociological Methodology. 1995;25:267–316. doi: 10.2307/271070. [DOI] [Google Scholar]
- Norris FH. Epidemiology of trauma: Frequency and impact of different potentially traumatic events on different demographic groups. Journal of Consulting and Clinical Psychology. 1992;60:409–418. doi: 10.1037//0022-006x.60.3.409. http://dx.doi.org/10.1037/0022-006X.60.3.409. [DOI] [PubMed] [Google Scholar]
- Oei TPS, Browne A. Components of group processes: Have they contributed to the outcome of mood and anxiety disorder patients in a group cognitive-behaviour therapy program? American Journal of Psychotherapy. 2006;60:53–69. doi: 10.1176/appi.psychotherapy.2006.60.1.53. [DOI] [PubMed] [Google Scholar]
- Orcutt HK, Pickett SM, Pope EB. Experiential Avoidance and Forgiveness As Mediators in the Relation Between Traumatic Interpersonal Events and Posttraumatic Stress Disorder Symptoms. Journal of Social and Clinical Psychology. 2005;24(7):1003–1029. https://doi.org/10.1521/jscp.2005.24.7.1003. [Google Scholar]
- Piper WE, Ogrodniczuk JS, Lamarche C, Hilscher T, Joyce AS. Level of alliance, pattern of alliance, and outcome in short-term group therapy. International Journal of Group Psychotherapy. 2005;55:527–550. doi: 10.1521/ijgp.2005.55.4.527. https://doi.org/10.1521/ijgp.2005.55.4.527. [DOI] [PubMed] [Google Scholar]
- Puschner B, Bauer S, Horowitz LM, Kordy H. The relationship between interpersonal problems and the helping alliance. Journal of Clinical Psychology. 2005;61:415. doi: 10.1002/jclp.20050. https://doi.org/10.1002/jclp.20050. [DOI] [PubMed] [Google Scholar]
- Raftery AE. Bayesian model selection in social research. Sociological Methodology. 1995;25:111–163. doi: 10.2307/271063. [DOI] [Google Scholar]
- Resick PA, Wachen JS, Mintz J, Young-McCaughan S, Roache JD, Borah AM, Peterson AL. A randomized clinical trial of group cognitive processing therapy compared with group present-centered therapy for PTSD among active duty military personnel. Journal of Consulting and Clinical Psychology. 2015;83(6):1058–1068. doi: 10.1037/ccp0000016. https://doi.org/10.1037/ccp0000016. [DOI] [PubMed] [Google Scholar]
- Riggs DS, Byrne CA, Weathers FW, Litz BT. The quality of the intimate relationships of male Vietnam veterans: Problems associated with posttraumatic stress disorder. Journal of Traumatic Stress. 1998;11:87–101. doi: 10.1023/A:1024409200155. https://doi.org/10.1023/A:1024409200155. [DOI] [PubMed] [Google Scholar]
- Safran JD, Crocker P, McMain S, Murray P. The therapeutic alliance rupture as a therapy event for empirical investigation. Psychotherapy. 1990;27:154–165. http://dx.doi.org/10.1037/0033-3204.27.2.154. [Google Scholar]
- Safran JD, Muran JC. The resolution of ruptures in the therapeutic alliance. Journal of Consulting and Clinical Psychology. 1996;64:447–458. doi: 10.1037//0022-006x.64.3.447. http://dx.doi.org/10.1037/0022-006X.64.3.447. [DOI] [PubMed] [Google Scholar]
- Saunders SM. Pretreatment correlates of the therapeutic bond. Journal of Clinical Psychology. 2001;57:1339–1352. doi: 10.1002/jclp.1101. https://doi.org/10.1002/jclp.1101. [DOI] [PubMed] [Google Scholar]
- Schnurr PP, Friedman MJ, Foy DW, Shea MT, Hsieh FY, Lavori PW, Bernardy NC. Randomized trial of trauma-focused group therapy for posttraumatic stress disorder: Results from a department of veterans affairs cooperative study. Archives of General Psychiatry. 2003;60(5):481–489. doi: 10.1001/archpsyc.60.5.481. https://doi.org/10.1001/archpsyc.60.5.481. [DOI] [PubMed] [Google Scholar]
- Seal KH, Bertenthal D, Miner M, Sen S, Marmar CR. Bringing the war back home: Mental health disorders among 103 788 us veterans returning from iraq and afghanistan seen at department of veterans affairs facilities. Archives of Internal Medicine. 2007;167(5):476–482. doi: 10.1001/archinte.167.5.476. https://doi.org/10.1001/archinte.167.5.476. [DOI] [PubMed] [Google Scholar]
- Sloan DM, Unger W, Beck JG. Cognitive-behavioral group treatment for veterans diagnosed with PTSD: Design of a hybrid efficacy-effectiveness clinical trial. Contemporary Clinical Trials. 2016;47:123–130. doi: 10.1016/j.cct.2015.12.016. https://doi.org/10.1016/j.cct.2015.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sloan DM, Unger W, Lee DJ, Beck JG. A randomized controlled trial of Cognitive-behavioral group treatment for Veterans diagnosed with PTSD (under review) [Google Scholar]
- Snijders T, Bosker R. Multilevel Analysis. Thousand Oaks, CA: Sage; 1999. [Google Scholar]
- Stiles WB, Glick MJ, Osatuke K, Hardy GE, Shapiro DA, Agnew-Davies R, Barkham M. Patterns of alliance development and the rupture-repair hypothesis: Are productive relationships U-shaped or V-shaped? Journal of Counseling Psychology. 2004;51:81–92. http://dx.doi.org/10.1037/0022-0167.51.1.81. [Google Scholar]
- Surís A, Link-Malcolm J, Chard K, Ahn C, North C. A randomized clinical trial of Cognitive Processing Therapy for veterans with PTSD related to military sexual trauma. Journal of Traumatic Stress. 2013;26(1):28–37. doi: 10.1002/jts.21765. https://doi.org/10.1002/jts.21765. [DOI] [PubMed] [Google Scholar]
- Taft CT, Murphy CM, King DW, Musser PH, DeDeyn JM. Process and treatment adherence factors in group cognitive-behavioral therapy for partner violent men. Journal of Consulting and Clinical Psychology. 2003;71(4):812–820. doi: 10.1037/0022-006x.71.4.812. https://doi.org/10.1037/0022-006X.71.4.812. [DOI] [PubMed] [Google Scholar]
- Taft CT, Murphy CM, Musser PH, Remington NA. Personality, interpersonal, and motivational predictors of the working alliance in group cognitive-behavioral therapy for partner violent men. Journal of Consulting and Clinical Psychology. 2004;72:349–354. doi: 10.1037/0022-006X.72.2.349. http://dx.doi.org/10.1037/0022-006X.72.2.349. [DOI] [PubMed] [Google Scholar]
- Tasca GA, Balfour L, Ritchie K, Bissada H. The relationship between attachment scales and group therapy alliance growth differs by treatment type for women with binge-eating disorder. Group Dynamics: Theory, Research, and Practice. 2007;11(1):1–14. https://doi.org/10.1037/1089-2699.11.1.1. [Google Scholar]
- Tasca GA, Lampard AM. Reciprocal influence of alliance to the group and outcome in day treatment for eating disorders. Journal of Counseling Psychology. 2012;59(4):507–517. doi: 10.1037/a0029947. https://doi.org/10.1037/a0029947. [DOI] [PubMed] [Google Scholar]
- Teachman JD, Call VRA. The effect of military service on educational, occupational, and income attainment. Social Science Research. 1996;25(1):1–31. https://doi.org/10.1006/ssre.1996.0001. [Google Scholar]
- Tsai M, Ogrodniczuk JS, Sochting I, Mirmiran J. Forecasting success: Patients’ expectations for improvement and their relations to baseline, process and outcome variables in group cognitive-behavioural therapy for depression. Clinical Psychology and Psychotherapy. 2014;21:97–107. doi: 10.1002/cpp.1831. http://dx.doi.org/10.1002/cpp.1831. [DOI] [PubMed] [Google Scholar]
- Tschuschke V, Dies RR. Intensive analysis of therapeutic factors and outcome in long-term inpatient groups. International Journal of Group Psychotherapy. 1994;44(2):185–208. doi: 10.1080/00207284.1994.11490742. https://doi.org/10.1080/00207284.1994.11490742. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Bovin MJ, Lee DJ, Sloan DM, Schnurr PP, Kaloupek DG, Keane TM, Marx BP. The Clinician-Administered PTSD Scale for DSM-5 (CAPS-5): Development and initial psychometric evaluation in military veterans. Psychological Assessment. doi: 10.1037/pas0000486. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woody SR, Adessky RS. Therapeutic alliance, group cohesion, and homework compliance during cognitive-behavioral group treatment of social phobia. Behavior Therapy. 2002;33(1):5–27. https://doi.org/10.1016/S0005-7894(02)80003-X. [Google Scholar]
- Yalom ID, Leszcz M. The Theory and Practice of Group Psychotherapy. 5th. New York, NY: Basic Books; 2005. [Google Scholar]


