Abstract
Background
The 2007 Guidelines for the Diagnosis and Management of Asthma provide evidence-based recommendations to improve asthma care. Limited national-level data are available about clinician agreement and adherence to these guidelines.
Objective
To assess clinician-reported adherence with specific guideline recommendations, as well as agreement with and self-efficacy to implement guidelines
Methods
We analyzed 2012 National Asthma Survey of Physicians data for 1412 primary care clinicians and 233 asthma specialists about four cornerstone guideline domains: asthma control, patient education, environmental control, and pharmacologic treatment. Agreement and self-efficacy were measured using Likert scales; two overall indices of agreement and self-efficacy were compiled. Adherence was compared between primary care clinicians and asthma specialists. Logistic regression models assessed the association of agreement and self-efficacy indices with adherence.
Results
Asthma specialists expressed stronger agreement, higher self-efficacy, and greater adherence with guideline recommendations than primary care clinicians. Adherence was low among both groups for specific core recommendations, including written asthma action plan (30.6% and 16.4%, respectively P<.001); home peak flow monitoring, (12.8% and 11.2%, P=.34); spirometry testing, (44.7% and 10.8%, P<.001); and repeated assessment of inhaler technique, (39.7% and 16.8%, P<.001). Among primary care clinicians, greater self-efficacy was associated with greater adherence. For specialists, self-efficacy was associated only with increased odds of spirometry testing. Guideline agreement was generally not associated with adherence.
Conclusions
Agreement with and adherence to asthma guidelines was higher for specialists than primary care clinicians, but was low in both groups for several key recommendations. Self-efficacy was a good predictor of guideline adherence among primary care clinicians but not among specialists.
Keywords: asthma guidelines, agreement, confidence, adherence, specialist, primary care, national survey
Introduction
Clinical guidelines aid in disease diagnosis and management, and exist for multiple conditions including asthma.(1) Previous reports on primary care clinicians and specialists demonstrate that adherence to guidelines in general is low (2–6) and that adherence to the 2007 National Asthma Education and Prevention Program’s (NAEPP) Expert Panel Report 3 (EPR-3) asthma guidelines(1) is no exception.(7–10) The National Ambulatory Medical Care Survey (NAMCS), an ongoing nationally representative survey, covers visits to office-based physicians and clinicians in Community Health Centers (CHC).(11) In 2012, the National Asthma Survey of Physicians (NAS) was fielded as a one-time provider questionnaire supplement to NAMCS.(12) The supplement was conceived of and sponsored by the National Asthma Education and Prevention Program Coordinating Committee (NAEPP-CC). The questionnaire design group was co-lead by the National Center for Environmental Health, CDC and the National Heart, Lung and Blood Institute with staff and NAEPP-CC members participating (see supplemental material in Online Repository). It queried primary care clinicians’ and specialists’ opinions, self-efficacy, and self-reported adherence regarding asthma care and key recommendations in the EPR-3 report. The goal of this manuscript is to characterize and compare agreement with the national asthma guidelines by primary care and asthma specialty clinicians, their confidence in implementing the guidelines, and assess their self-reported adherence to the four core components of the guidelines. This information could inform new guidelines and future studies.
Methods
Data Source and Study Population
NAMCS is conducted annually by the National Center for Health Statistics (NCHS) to collect information about patient, clinician, and office visit characteristics. Data from the 2012 NAS supplement(12) to NAMCS were released in 2017. Clinician eligibility for NAMCS was determined by responses to the Physician Induction Interview (PII).(11, 13) Participating clinicians who responded affirmatively to the PII asthma screener question (“Do you treat patients with asthma?”), regardless of specialty, were included in the NAS. Since 2006, NAMCS has included visits to office-based physicians and a panel of CHCs with up to three physicians and/or midlevel clinicians sampled per CHC. Sample selection is designed to produce nationally representative estimates for both NAMCS and CHC visits. Starting in 2012, the office-based component of NAMCS was split from the CHC component to produce separate data files for visits to private physician offices and CHCs to increase flexibility in use of patient visit data.(11) However, patient visit data from either component could not be linked to physician responses to the NAS supplement. This analysis utilized the 2012 NAS file released by NCHS that included NAMCS office-based physicians, CHC physicians and CHC mid-level clinicians. The 2012 NAS file included specific physician/clinician survey weights provided by NCHS. The NAMCS physician sampling frame included non-federally employed physicians who were classified as being engaged primarily in office-based patient care by the American Medical Association or the American Osteopathic Association and included general/family practitioners, internists, pediatricians and obstetricians. Specialty physicians in anesthesiology, radiology, and pathology, and those over age 85 years were excluded. Allergists and pulmonologists were oversampled to provide a sufficient sample size of asthma specialists for the NAS supplement. The CHC sampling frame included physicians and mid-level practitioners (i.e., physician assistants, nurse practitioners, and nurse midwives) from sampled CHC delivery sites. No asthma specialists were sampled in the CHC-based portion of the NAS. The NCHS Institutional Review Board approved NAS and informed consent was obtained from participating clinicians.
The unweighted and weighted response rates for the overall combined NAS sample were 38% and 28%, respectively, similar or higher than other national physician surveys.(14) The weighted response rate was higher for CHC providers (73%) than for NAMCS physicians (26%). Of the 1726 respondents, 49 were specialists unlikely to directly manage asthma, leaving 1677 eligible participants. Seventeen records were missing demographic data and were excluded from the sample. Clinician race/ethnicity was not included in the NAMCS questionnaire used in CHCs. Non-clinical respondents were also excluded (n=15). The final sample of 1645 included 1412 primary care clinicians (primary care physicians from the office-based and CHC samples and CHC mid-level practitioners from the CHC sample) and 233 asthma specialists (allergists and pulmonologists from the office-based sample). Available information on demographic characteristics included specialty, age, sex, and Census practice region, level of practice urbanization, practice ownership, and age of patient population.
Outcomes
Outcome variables were categorized into the four EPR-3 cornerstones of care: assessment and monitoring, patient education, environmental control, and pharmacologic treatment (Table E1). Clinician agreement with and adherence to specific EPR-3 recommendations and self-efficacy defined as clinician confidence in their ability to competently implement specific EPR-3 recommendations were determined by self-report (Table E2). Missing responses were low (0.01%-2.0%) and were excluded for individual outcomes.(15)
Indices for Agreement and Self-efficacy
The association between adherence and overall agreement and overall self-efficacy with providing guideline-based care were assessed using two index variables. An agreement index variable was defined dichotomously as a response of “strongly agree” versus all other responses to all 5 questions about agreement (Table E2). Similarly, a self-efficacy index variable was defined as a response of “very confident” versus all other responses for all 5 questions about self-efficacy (Table E2).
Statistical Analysis
Descriptive statistics were used to summarize clinician characteristics and outcome measures using provided sample weights to calculate nationally representative estimates. Differences between primary care clinicians and asthma specialists in distributions across response categories for guideline adherence outcomes were assessed using chi-square tests, with P<.05 (2-sided) considered statistically significant. Thus, P values in the text and tables reflect differences across the range of Likert scale response categories (e.g., “never (0% of the time)” to “almost always (75% to 100% of the time)” in Table II) rather than differences for one particular response category. Separate logistic regression models assessed the impact of agreement and self-efficacy on guideline adherence for each outcome that could be dichotomized to “almost always” versus all other responses. For some covariate categories, there were zero cells for asthma specialists. Therefore, the simplest models with the control indices for agreement and self-efficacy as the only independent variables are reported. Multivariate results that include additional covariates but that omit covariates with zero counts for any category are shown in the supplement. National estimates were calculated using NAS sample weights that accounted for the probability of clinician selection and non-response. Estimation of standard errors (SE) and statistical inference took the complex survey design into account. Analyses were conducted using SAS 9.4 (SAS Institute Inc., Cary, NC) and SUDAAN 11.0 (RTI, Research Triangle Park, NC). Estimates with a relative standard error >30% (SE/estimate) are flagged to indicate that these estimates have lower precision.
Table II.
Assessment and Monitoring of Asthma Severity and Control: Clinician - Reported Adherence to EPR - 3 Asthma Guideline Component 1
| Primary Care Clinicians | Asthma Specialists | |||||||
|---|---|---|---|---|---|---|---|---|
| n | Almost always | Often | Sometimes /Never | Almost always | Often | Sometimes /Never | P Value | |
| Assessment of impairment frequency, weighted % (SE) | ||||||||
| Document asthma control | 1550 | 32.0 (2.2) | 44.6 (2.4) | 23.4 (2.0) | 76.8 (3.8) | 20.5 (3.7) | 2.7* (1.2) | <.001 |
| Ask about ability to engage in normal activities | 1625 | 48.4 (2.4) | 38.7 (2.3) | 12.9 (1.5) | 84.5 (3.3) | 14.9 (3.2) | 0.6* (0.6) | <.001 |
| Ask about frequency of daytime symptoms | 1632 | 56.0 (2.3) | 35.9 (2.3) | 8.1 (1.3) | 91.1 (2.5) | 8.5 (2.5) | 0.4* (0.4) | <.001 |
| Ask about frequency of nighttime awakening | 1630 | 53.4 (2.4) | 31.8 (2.2) | 14.8 (1.8) | 81.7 (3.6) | 14.9 (3.3) | 3.4* (1.9) | <.001 |
| Ask about perception of control | 1629 | 50.7 (2.4) | 33.1 (2.1) | 16.2 (1.8) | 70.7 (4.2) | 26.0 (4.0) | 3.3* (1.9) | <.001 |
| Use control assessment tool | 1629 | 13.2 (1.5) | 17.2 (1.9) | 69.7 (2.2) | 28.6 (3.5) | 20.4 (3.4) | 51.0 (4.2) | <.001 |
| Ask about frequency rescue inhaler | 1632 | 72.3 (2.1) | 23.1 (1.9) | 4.6 (1.1) | 90.6 (2.8) | 6.5* (2.2) | 2.9* (1.7) | <.001 |
| Assessment of risk frequency, weighted % (SE) | ||||||||
| Ask about oral steroid frequency | 1629 | 52.9 (2.4) | 34.0 (2.2) | 13.1 (1.6) | 86.8 (3.1) | 11.6 (3.1) | 1.6* (0.8) | <.001 |
| Ask about ED visit frequency | 1631 | 56.2 (2.3) | 29.2 (2.0) | 14.6 (1.8) | 81.9 (3.4) | 12.6 (3.2) | 5.6* (2.2) | <.001 |
| Objective assessment and monitoring, weighted % (SE) | ||||||||
| Ask about peak flow results | 1628 | 11.2 (1.5) | 22.9 (2.0) | 65.9 (2.2) | 12.8 (2.5) | 27.9 (3.7) | 59.3 (4.1) | .34 |
| Perform spirometry | 1611 | 10.8 (1.6) | 25.1 (2.0) | 61.6 (2.2) | 44.7 (4.1) | 35.0 (4.0) | 20.3 (4.0) | <.001 |
| Ongoing monitoring frequency, weighted % (SE) | ||||||||
| Assess daily controller use for persistent asthma | 1625 | 59.5 (2.3) | 31.6 (2.1) | 8.9 (1.4) | 91.7 (2.4) | 8.2 (2.4) | 0.2* (0.1) | <.001 |
| Repeated assessment of inhaler technique | 1627 | 16.8 (1.7) | 38.7 (2.4) | 44.6 (2.3) | 39.7 (4.0) | 44.9 (4.3) | 15.5 (3.0) | <.001 |
The relative standard error is >30%.
ED: emergency department; EPR-3: Expert Panel Report 3; SE: standard error Data Source: NCHS, National Asthma Survey of Physicians, 2012.
Results
Compared to primary care clinicians, asthma specialists were more likely to be older, male, work in private practice settings, and practice in the South, and in large metropolitan areas (Table I). Asthma specialists were less likely to exclusively treat pediatric populations.
Table I.
National Asthma Survey clinician characteristics, 2012
| Total (n=1645) | Primary care cliniciansa (n=1,412) | Asthma specialistsb (n=233) | |||
|---|---|---|---|---|---|
| n | weighted % (SE) |
weighted % (SE) |
weighted % (SE) |
P Valuec | |
| Clinician age (years) | |||||
| <40 | 372 | 15.6 (1.4) | 16.0 (1.5) | 9.5 (2.3) | .004 |
| 40 - 59 | 907 | 60.3 (2.1) | 60.6 (2.2) | 54.0 (4.1) | |
| 60+ | 366 | 24.1 (1.9) | 23.4 (2.0) | 36.5 (4.0) | |
| Clinician sex | |||||
| Female | 772 | 40.0 (2.0) | 41.4 (2.1) | 15.7 (2.7) | <.001 |
| Male | 873 | 60.0 (2.0) | 58.6 (2.1) | 84.3 (2.7) | |
| Ownership of practice | |||||
| Private | 653 | 61.7 (1.8) | 60.3 (2.0) | 84.4 (2.8) | <.001 |
| CHC | 688 | 16.0 (0.8) | 17.0 (0.8) | 0.0* (0.0) | |
| HMO, Academic Center, Other hospital/health care corporation | 194 | 16.1 (1.6) | 16.4 (1.7) | 12.0 (2.5) | |
| missing | 110 | 6.2 (1.1) | 6.3 (1.2) | 3.6* (1.4) | |
| Census region | |||||
| Northeast | 255 | 20.7 (0.9) | 20.6 (0.9) | 21.1 (2.0) | .007 |
| Midwest | 400 | 19.5 (0.6) | 19.6 (0.7) | 17.8 (1.5) | |
| South | 553 | 30.2 (0.8) | 29.7 (0.9) | 38.0 (2.7) | |
| West | 437 | 29.7 (0.8) | 30.1 (0.9) | 23.2 (1.8) | |
| Level of urbanization | |||||
| Large Metro | 737 | 56.8 (1.9) | 56.3 (2.0) | 66.5 (3.8) | .002 |
| Medium/Small Metro | 532 | 28.8 (1.9) | 28.9 (2.0) | 27.2 (3.7) | |
| Non - metro | 376 | 14.3 (1.1) | 14.8 (1.2) | 6.3* (2.2) | |
| Patient population | |||||
| Pediatric only | 333 | 22.6 (1.7) | 23.4 (1.8) | 8.2* (2.8) | <.001 |
| Adult or all ages | 1312 | 77.4 (1.7) | 76.6 (1.8) | 91.9 (2.8) | |
Primary care clinicians include general/family practitioners, internists, pediatricians, obstetricians and CHC mid-level providers.
Asthma specialist include allergists and pulmonologists.
Chi-square test for difference between primary care clinicians and asthma specialists.
The relative standard error is >30%. Source: NCHS, National Ambulatory Medical Care Survey, 2012.
EPR-3 Component 1: Assessment and Monitoring of Asthma Severity and Control
EPR-3 recommends that clinicians assess asthma impairment (symptom frequency and asthma control) and risk for adverse outcomes (hospitalizations, ED visits, and courses of systemic corticosteroids) during clinic visits. A higher percentage of asthma specialists almost always assessed all measures of asthma impairment than primary care clinicians, including a patient’s ability to engage in normal daily activities (84.5% versus 48.4%), frequency of daytime symptoms (91.1% versus 56.0%) and nighttime awakenings (81.7% versus 53.4%), and patient’s perception of control (70.7% versus 50.7%) (P<0.001 for distributional comparison across the Likert scale for all comparisons) (Table II). Most primary care clinicians (72.3%) asked about frequency of rescue inhaler use, albeit less frequently than asthma specialists (90.6%; P<.001). In contrast, use of a control assessment tool (e.g., Asthma Control Test, Asthma Control Questionnaire, Asthma Therapy Assessment Questionnaire, or similar tool) was low in both groups. More than half of the specialists (51.0%) and 69.7% of the primary care clinicians reported that they either sometimes or never used such tools. Indeed, 39.7% of primary care clinicians and 28.9% of specialists reported that they never used control assessment tools (data not shown).
The assessment of risk also differed between the two groups (Table II). While 86.8% and 81.9% of asthma specialists reported almost always asking patients about oral steroid use and emergency department (ED)/urgent care visits, fewer primary care clinicians (52.9% and 56.2%, respectively; P<.001 for comparison between clinician groups) almost always assessed these risk factors for adverse outcomes.
Both groups reported low frequencies of objective asthma assessment and monitoring. Only 11.2% of primary care clinicians and 12.8% of specialists almost always asked about home peak flow results (P=.34). Specialists were more likely to report almost always performing spirometry than primary care clinicians (e.g., 44.7% versus 10.8%; P<.001). The 64.1% of primary care clinicians who reported that they sometimes or never performed spirometry was made up of 36.3% who sometimes and 27.8% who never performed spirometry.
Asthma specialists were more likely to report assessing daily controller use for persistent asthma than primary care clinicians (91.7% versus 59.5% respectively, P<.001). Repeated assessment of inhaler technique was less frequently reported by both groups: 39.7% of asthma specialists reported almost always assessing technique versus 16.8% of primary care clinicians (P<.001).
EPR-3 Component 2: Patient Education
Guideline-recommended patient education items covered in the survey included the frequency of providing asthma action plans (Likert scale), and whether or not the clinician provided trigger and risk education, inhaler use observation and advised changing home and work environment (Table III). Although written asthma action plans can improve asthma-related outcomes,(1, 16, 17) only 30.6% (SE 3.6) of specialists and 16.4% (SE 1.6) of primary care clinicians used them almost always (P <.001), and 6.1% (SE 2.3, RSE>30%) and 17.6% (SE 1.8) never used them, respectively (P <.001) (Table III, Panel A). Almost all specialists reported providing patient education regarding asthma symptom recognition, avoiding risk factors, inhaler technique and changing the home/work environment. Primary care providers also reported providing patient education in these areas with a high frequency but with a lower frequency than specialists, especially for inhaler use observation (Table III, Panel B).
Table III.
Patient education: Clinician-Reported Adherence to EPR-3 Asthma Guideline Component 2
| Primary Care Clinicians | Asthma Specialists | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Panel A: Frequency of asthma action plan provision, Likert scale (weighted %, SE) | ||||||||||
|
| ||||||||||
| n | Almost always | Often | Sometimes | Never | Almost always | Often | Sometimes | Never | p-value | |
|
| ||||||||||
| Provide asthma action plan with medication, triggers, etc | 1625 | 16.4 (1.6) | 30.7 (2.2) | 35.4 (2.2) | 17.6 (1.8) | 30.6 (3.6) | 32.7 (4.1) | 30.6 (4.3) | 6.1* (2.3) | <0.001 |
|
| ||||||||||
| Panel B: Provision of patient education, yes versus no (weighted %, SE) | ||||||||||
|
| ||||||||||
| n | Yes | No | Yes | No | ||||||
|
| ||||||||||
| Educate patient to recognize symptoms | 1645 | 95.2 (1.0) | 4.8 (1.0) | 99.9 (0.1) | 0.1* (0.1) | <0.001 | ||||
| Educate patient to avoid risk factors | 1645 | 96.1 (0.8) | 3.9 (0.8) | 99.9 (0.1) | 0.1* (0.1) | <0.001 | ||||
| Observe inhaler use | 1621 | 73.1 (2.1) | 26.9 (2.1) | 99.5 (0.3) | 0.5* (0.3) | <0.001 | ||||
| Advise patient to change home/work environment | 1645 | 89.5 (1.6) | 10.5 (1.6) | 95.5 (1.6) | 4.5* (1.6) | 0.009 | ||||
The relative standard error is >30%.
Both groups reported patient concerns and misunderstandings about asthma pharmacologic therapies (Figure 1). Both groups reported patients sometimes or often misunderstood medication risks, were concerned about the side effects of inhaled corticosteroid (ICS) therapy, and were confused between rescue and controller medications. Specialists, however, more often than primary care clinicians reported that patients were almost always concerned about long-term ICS effects (8.6% versus 5.1%; P=.002) while primary care clinicians more often reported that patients were almost always confused rescue and controller medications, although the estimate for asthma specialists had an RSE>30% (11.7% versus 4.0%; P=.004).
Figure 1.
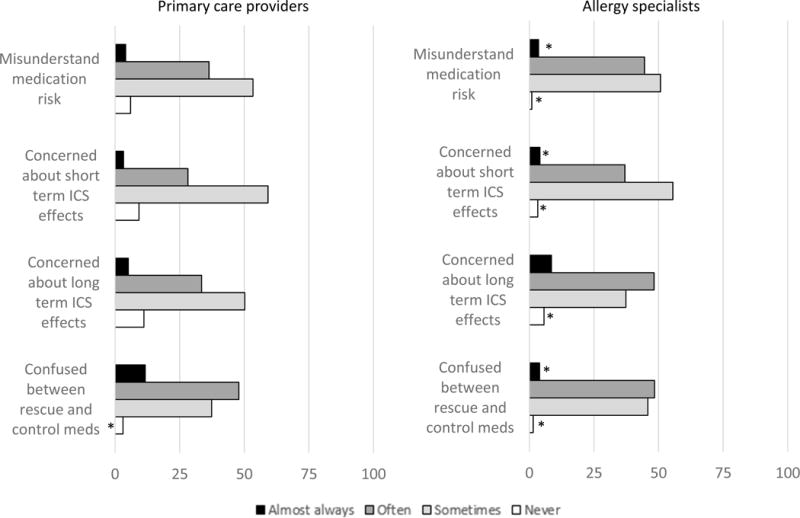
Clinician reported frequency of patient misunderstanding and concerns about asthma medications
Note: Results for all four medication questions differ statistically significantly between primary care clinicians and allergy specialists (chi square P value<.05).
* Relative standard error > 30%.
Source: NCHS, National Ambulatory Medical Care Survey, 2012.
EPR-3 Component 3: Control of Environmental Factors
Control of environmental factors can reduce asthma morbidity.(18) Asthma specialists were more likely to assess environmental triggers at home, school and/or workplace than primary care clinicians (Table IV). Specialists more often (67.3%) reported performing allergy testing “almost always” or “often” versus 24.8% of primary care clinicians (P<.001). Nearly a third (30.4%, SE 2.2) of primary care clinicians reported never performing these tests versus 5.3% (SE 2.1) of specialists (P<.001) (data not shown).
Table IV.
Control of Environmental Factors: Clinician-Reported Adherence to EPR-3 Asthma Guideline Component 3
| Primary Care Clinicians | Asthma Specialists | |||||||
|---|---|---|---|---|---|---|---|---|
| n | Almost always | Often | Sometimes /Never | Almost always | Often | Sometimes /Never | P Value | |
| Assessment of triggers, weighted % (SE) | ||||||||
| Assess home triggers | 1628 | 40.1 (2.3) | 42.0 (2.3) | 17.9 (1.8) | 58.7 (4.2) | 35.2 (4.2) | 6.1* (2.2) | <.001 |
| Assess school or workplace triggers | 1619 | 35.4 (2.3) | 38.4 (2.2) | 26.2 (2.0) | 71.3 (3.9) | 24.2 (3.6) | 4.5* (2.0) | <.001 |
| Test for allergic sensitivity | 1617 | 7.2 (1.4) | 17.6 (1.8) | 75.3 (2.1) | 35.0 (3.6) | 32.3 (4.1) | 32.8 (4.0) | <.001 |
| Recommendations, weighted % (SE) | n | Most patients | Patients with sensitivity | Sometimes/never recommend | Most patients | Patients with sensitivity | Sometimes/never recommend | P Value |
| Recommend d ust mite control measures | 1609 | 40.8 (2.3) | 46.8 (2.4) | 12.4 (1.5) | 36.5 (3.8) | 56.8 (3.9) | 6.8* (2.3) | .039 |
| Recomme nd control of mold and pests | 1608 | 44.1 (2.4) | 42.6 (2.3) | 13.3 (1.7) | 46.9 (4.4) | 47.1 (4.3) | 6.0* (2.3) | .025 |
| Recommend pet removal | 1609 | 28.6 (2.1) | 59.8 (2.3) | 11.6 (1.4) | 29.3 (3.9) | 58.8 (4.1) | 11.9 (2.4) | .97 |
| Recommend avoiding pollen | 1611 | 43.3 (2.3) | 47.7 (2.3) | 9.1 (1.6) | 37.3 (4.4) | 55.4 (4.3) | 7.3 (1.9) | .28 |
| Recommend avoiding air pollution | 1604 | 44.8 (2.3) | 33.6 (2.2) | 21.6 (2.1) | 63.2 (4.2) | 30.0 (4.1) | 6.8 (1.9) | <.001 |
| Recommend cooking appliance change | 1610 | 16.2 (1.8) | 30.7 (2.2) | 53.1 (2.4) | 21.7 (3.5) | 33.6 (4.0) | 44.7 (4.3) | .18 |
| Recommend avoiding ETS | 1611 | 83.5 (1.8) | 12.2 (1.5) | 4.3 (1.1) | 85.4 (3.3) | 12.7 (3.2) | 1.9* (0.8) | .24 |
The relative standard error is >30%.
EPR-3: Expert Panel Report 3; ETS: environmental tobacco smoke; SE: standard error Data Source: NCHS, National Asthma Survey of Physicians, 2012.
Recommendations for control of environmental factors differed between specialists and primary care clinicians. Primary care clinicians were less likely to recommend dust mite, mold and pest control measures than specialists but almost 60% of all clinicians recommended removing pets from homes with pet-sensitive patients. While both clinician groups provided recommendations on pollen avoidance, recommendations regarding cooking appliances were infrequent (i.e., 44.7%-53.1% of clinicians sometimes or never gave recommendations). The majority of specialists and primary care clinicians (>83%) recommended environmental tobacco smoke (ETS) avoidance, whereas air pollution avoidance was more frequently recommended by specialists. The biggest differences between primary care clinicians and specialists were observed for recommendations regarding air pollution avoidance. Specialists more often recommended air pollution avoidance for most patients than primary care clinicians (63.2 % vs 44.8%; P<.001). In addition, more primary care clinicians sometimes/never recommended air pollution avoidance as compared to specialists (21.6% vs 6.8%; P<.001).
EPR-3 Component 4: Pharmacologic Treatment
Self-reported medication prescription for both groups was consistent with EPR-3 recommendations (e.g., short-acting beta agonists for symptom relief, and ICS for difficult to control asthma, add-on daily control and long-term control) (Figure 2). Asthma specialists reported greater use of other asthma medications than primary care clinicians (e.g., the percentage reporting never using specific medications was 16.6% of specialists versus 42.2% of primary care providers for long-course oral steroids, 14.1% versus 83.3% for Omalizumab, 45.9% versus 75.3% for methylxanthines, and 13.7% versus 30.6% for anticholinergics). Both groups prescribed short courses of oral steroids for asthma exacerbations, but specialists were less likely to prescribe short course oral steroids for symptom relief (43.2% versus 56.9%), and more likely to prescribe this medication for difficult-to-control asthma (60.7% versus 45.1%) and as add-on daily therapy (12.1% versus 5.3%) (P<0.05 for all comparisons).
Figure 2.
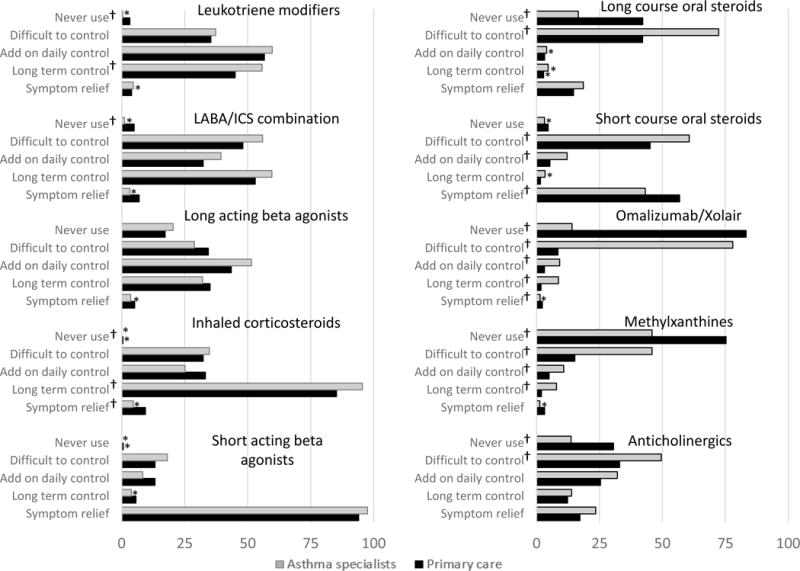
Clinician-Reported Use of Asthma Medications, by Specialty
† P Value <.05 for pairwise difference between asthma specialists and primary care.
* Relative standard error > 30%.
Source: NCHS, National Ambulatory Medical Care Survey, 2012.
Agreement and Self-Efficacy with EPR-3 Guideline Recommendations
More asthma specialists than primary care clinicians agreed strongly with the EPR-3 recommendations regarding spirometry for asthma diagnosis (77.6% versus 35.5%), the effectiveness of inhaled corticosteroids (ICS) for persistent asthma (76.0% versus 48.3%), twice yearly follow-up visits for persistent asthma (68.8% versus 48.9%) and assessment of asthma severity for initial treatment (79.3% versus 50.3%) (P<0.001 for all comparisons) (Table V, Panel A). In contrast, less than half of specialists and primary care clinicians strongly agreed that asthma action plans are effective, but strong agreement was still higher among specialists (41.0% versus 30.6%, P=.026). Strong agreement with all five guideline recommendations included in the survey was higher among specialists than primary care clinicians (27.9% versus 12.1%, P<.001).
Table V.
Clinician-Reported Agreement and Self-efficacy with EPR-3 Asthma Guidelines
| Primary Care Clinicians | Asthma Specialists | |||
|---|---|---|---|---|
| Panel A: Agreement, weighted % (SE) | n | Strongly agree | Strongly agree | P Valuea |
| Spirometry is essential for diagnosis | 1638 | 35.5 (2.3) | 77.6 (3.8) | <.001 |
| ICS are effective for persistent asthma | 1633 | 48.3 (2.3) | 76.0 (3.4) | <.001 |
| Asthma Action Plans are effective | 1639 | 30.6 (2.1) | 41.0 (4.1) | .0258 |
| Follow up visits for persistent asthma every 6 months | 1639 | 48.9 (2.3) | 68.8 (3.5) | <.001 |
| Assessing severity is necessary for initial therapy | 1632 | 50.3 (2.4) | 79.3 (3.3) | <.001 |
| Overall agreement index | 1642 | 12.1 (1.4) | 27.9 (3.9) | <.001 |
| Panel B: Asthma Self - efficacy, weighted % (SE) | n | Very confident | Very confident | |
| Confidence using spirometry | 1636 | 37.0 (2.3) | 92.8 (2.1) | <.001 |
| Confidence assessing severity | 1635 | 49.4 (2.4) | 81.3 (3.5) | <.001 |
| Confidence prescribing ICS | 1642 | 65.2 (2.2) | 91.1 (2.2) | <.001 |
| Confidence step ping up therapy | 1641 | 64.5 (2.3) | 89.5 (2.4) | <.001 |
| Confidence step ping down therapy | 1639 | 49.8 (2.4) | 87.0 (2.6) | <.001 |
| Overall self - efficacy index | 1642 | 21.5 (2.1) | 72.3 (3.9) | <.001 |
| Primary Care Clinicians | Asthma Specialists | |||||
|---|---|---|---|---|---|---|
| Panel C: Association between adherence and strong agreement and high self-efficacy, OR (95% CI)b | n | Strong agreement (vs other) | High self-efficacy (vs. other) | n | Strong agreement (vs. other) | High self-efficacy (vs other) |
| Provide Asthma Action Plan | 1391 | 2.0 (1.1, 3.6)* | 2.4 (1.3, 4.3)* | 233 | 1.6 (0.7, 3.3) | 1.1 (0.5, 2.5) |
| Document asthma control | 1321 | 1.4 (0.8, 2.5) | 1.8 (1.0, 3.0)* | 226 | 0.8 (0.3, 2.1) | 1.5 (0.6, 3.5) |
| Ask about ability to engage in normal activities | 1392 | 1.7 (0.9, 3.2) | 2.1 (1.2, 3.5)* | 232 | 1.3 (0.4, 4.4) | 1.5 (0.6, 4.3) |
| Ask about frequency of daytime symptoms | 1398 | 1.5 (0.8, 2.9) | 2.3 (1.3, 4.1)* | 233 | 1.6 (0.4, 7.5) | 3.9 (1.0, 16.0) |
| Ask about frequency of nighttime awakenings | 1396 | 1.4 (0.8, 2.5) | 1.7 (1.0, 2.9) | 233 | 0.7 (0.2, 2.0) | 2.7 (0.9, 7.8) |
| Ask about patient perception of control | 1395 | 0.9 (0.5, 1.5) | 1.9 (1.1, 3.3)* | 233 | 1.6 (0.6, 4.3) | 1.2 (0.4, 3.0) |
| Use a control assessment tool | 1395 | 1.5 (0.8, 2.9) | 1.7 (0.9, 3.0) | 233 | 1.0 (0.5, 2.1) | 1.3 (0.6, 2.9) |
| Ask about frequency of rescue inhaler use | 1398 | 2.9 (1.6, 5.5)* | 2.7 (1.5, 4.7)* | 233 | 0.4 (0.1, 2.2) | 3.0 (0.6, 14.4) |
| Ask about ED visit frequency | 1398 | 1.3 (0.7, 2.3) | 3.0 (1.8, 4.8)* | 232 | 0.8 (0.3, 2.8) | 2.9 (1.0, 8.4) |
| Ask about oral steroid frequency | 1396 | 1.1 (0.6, 2.1) | 4.3 (2.6, 7.1)* | 232 | 0.7 (0.2, 2.8) | 1.4 (0.4, 5.1) |
| Ask about home peak flow results | 1396 | 2.0 (1.0, 4.0) | 3.1 (1.6, 6.1)* | 231 | 1.8 (0.7, 5.0) | 2.4 (0.8, 7.6) |
| Perform spirometry | 1378 | 2.1 (0.9, 4.7) | 6.3 (3.0, 13.4)* | 232 | 1.1 (0.5, 2.2) | 4.3 (2.0, 9.0)* |
| Assess daily controller use for persistent asthma | 1392 | 1.9 (1.1, 3.2)* | 2.4 (1.4, 4.4)* | 232 | 0.7 (0.2, 2.7) | 2.0 (0.6, 6.6) |
| Repeated assessment of inhaler technique | 1393 | 1.5 (0.7, 2.9) | 2.8 (1.6, 5.0)* | 233 | 1.5 (0.8, 3.1) | 0.8 (0.4, 1.9) |
| Assess home triggers | 1394 | 1.5 (0.9, 2.5) | 3.3 (1.9, 5.5)* | 233 | 0.8 (0.4, 1.7) | 1.9 (0.9, 4.2) |
| Assess school or workplace triggers | 1408 | 1.4 (0.8, 2.4) | 4.1 (2.5, 6.9)* | 233 | 0.8 (0.3, 1.7) | 1.5 (0.7, 3.6) |
| Test for allergic sensitivity | 1383 | 1.3 (0.5, 3.7) | 6.0 (2.5, 14.4)* | 233 | 1.1 (0.5, 2.4) | 1.8 (0.9, 3.8) |
P<.05.
Chi-square test for difference between primary care clinicians and asthma specialists.
Logistic regression models stratified by primary care clinicians and asthma specialists. Independent variables included agreement index (strong agreement versus all other responses) and self-efficacy index (high self-efficacy versus all other responses). See Supplemental Table e4 for logistic regression models with additional covariates.
CI: confidence interval; ED: emergency department; EPR-3: Expert Panel Report 3; ICS: inhaled corticosteroids; SE: standard error
Data Source: NCHS, National Asthma Survey of Physicians, 2012
Asthma specialists reported higher self-efficacy with providing guideline-recommended care than primary care clinicians (Table V, Panel B). Specialists were very confident in using spirometry (92.8%), in assessing severity (81.3%), in prescribing inhaled corticosteroids (91.1%), and in stepping up or down therapy (89.5%, 87.0%), while percentages were lower among primary care clinicians (37.0%, 49.4%, 65.2%, 64.5%, and 49.8%, respectively; P <.001). Accordingly, self-efficacy for all five recommendations was higher among specialists than primary care clinicians (72.3% versus 21.5%, P<.001).
The association between guideline agreement and self-efficacy with self-reported adherence to guideline recommendations was analyzed for outcomes for which responses could be dichotomized as “almost always” performed versus other responses (Table V, Panel C). Strong agreement was not associated with almost always performing any guideline component for either clinician group with three exceptions. In unadjusted models, among primary care clinicians, agreement with guidelines was significantly associated with almost always providing a written asthma action plan (OR 2.0, 95% CI 1.1, 3.6), almost always asking about the frequency of rescue inhaler use (OR 2.9, 95% CI 1.6, 5.5) and assessing daily controller use (OR 1.9, 95% CI 1.1, 3.2), but not among specialists. For primary care clinicians, higher self-efficacy in providing guideline components was associated with higher adherence to most guideline recommendations. For specialists, high self-efficacy was associated with higher odds of performing spirometry (OR 4.3, 95% CI 2.0, 9.0). In models adjusted for clinician age, sex, and region (Table E3), guideline agreement was associated with asking about rescue inhaler use, home peak flow monitoring, and assessing daily controller use for persistent asthma, but not with providing a written asthma action plan for primary care clinicians. Self-efficacy continued to be associated with adherence to most guideline recommendations for primary care clinicians in adjusted models but not for specialists in whom only high self-efficacy regarding spirometry and testing for allergic sensitivity were associated with guideline agreement (Table E3).
Discussion
In this representative sample of U.S. clinicians, most asthma specialists but less than half of primary care clinicians strongly agreed with key EPR-3 guideline recommendations for asthma assessment and treatment including use of spirometry, ICS therapy, follow-up visits for persistent asthma and assessment of asthma severity. Self-reported asthma medication use for both groups was consistent with EPR-3 recommendations and more than 80% of both clinician groups recommended ETS avoidance. Specialist self-efficacy overall was higher than primary care clinician self-efficacy and for most measures, including environmental control assessment and testing, specialist assessment and monitoring were higher. Primary care clinicians with high self-efficacy in using the guidelines more likely reported guideline adherence while guideline agreement was generally not associated with adherence for either group. This suggests that further efforts to increase clinician self-efficacy might increase guideline use and adherence.
While the lack of strong endorsement of guideline recommendations among primary care clinicians is notable, there were several key guideline recommendations that were not strongly endorsed by either group including the provision of a written asthma action plan. This result extends published data from several smaller studies and is in contrast to the evidence (Grade B, small number of randomized control trials) that support use of treatment plans (19–23) although their effectiveness when used by specialists has recently been questioned.(24) In addition, neither of the clinician groups reported frequent use of asthma control assessment tools, and home peak flow assessment rates were especially low. Furthermore, rates of adherence to spirometry testing and repeated inhaler technique assessment were low among both specialists and primary care clinicians.
It is possible that the strength and/or the “age” of the scientific evidence supporting the recommendation influence agreement and adherence. The 2007 EPR-3 guidelines used an evidence-based approach to assess strength of evidence for the first time. The EPR-3 guidelines were also the first to recommend routine spirometry (Grade B and C, observational studies), the assessment of risk in the determination of asthma severity (Grade C and D, expert panel consensus) and use of peak flow testing (Grade B).(1) However, the low uptake of components supported by higher grade evidence such as spirometry, asthma treatment plans, and peak flow testing suggests that adherence may not be directly related to strength of evidence. Of note, the survey did not ask clinicians about perceived usefulness of guideline recommendations, a factor related to adherence in smaller studies.(19) Time constraints, clinical inertia, and workflow barriers are factors in addition to agreement and self-efficacy that affect adherence, and these factors may work differently for primary care clinicians compared to specialists.(3, 8, 10, 25) Further studies to understand barriers may be needed, especially in primary care which provides most of the asthma care in the US.
Results from this study could be used to help guide the NAEPP recommendations that are currently being revised. These revised guidelines should carefully assess the strength of evidence for specific recommendations, identify areas and approaches to implementation that are specific for primary care clinicians and specialists, and focus clinical research on strengthening recommendations that are currently not embraced by clinicians. The guidelines also need to recommend new approaches to meeting patient concerns and to improving adherence by addressing barriers, especially workflow barriers.
Perceptions of patient concerns were more similar than disparate, but primary care clinicians reported greater patient confusion between controller and rescue medications whereas specialists reported more patient concerns regarding long-term corticosteroid therapy. This and other observed differences may reflect differences in disease severity and visit duration. Specialists care for patients with greater asthma severity and may spend more time explaining how to use asthma medications as their patient visits are longer compared to primary care clinicians.(25)
Strengths of the NAS include the national-representativeness of the survey sample, the inclusion of both adult and pediatric generalists and specialists, examination of the 4 cornerstones of the 2007 NAEPP guidelines and the inclusion of guideline agreement and clinician self-efficacy. Two other studies have reported asthma guideline results in primary care clinicians—one (26) reported low utilization of spirometry in the assessment of newly diagnosed patients with asthma, while the other (27) surveyed both clinicians and patients and noted low use of asthma treatment plans and spirometry. In contrast to these studies, this study offers valuable insight into areas of guideline disagreement and where additional evidence may be needed to achieve behavior changes. The differences between primary care clinicians and specialists suggest that the achievement of guideline adherence may require interventions specifically tailored to different groups of clinicians and to different health care systems and settings.
Although new literature/evidence has accumulated since 2007, the results reflect clinical practice after the latest guideline update. Self-reported behaviors are subject to social and recall bias, and actual behavior might differ.(27) Low response rates are known limitations in physician surveys,(28) and declining trends have been reported.(29, 30) The NAS response rate is, however, higher than the 2014 National Physician Survey which surveyed 63,817 physicians and had a response rate of 16%.(14) The characteristics of the NAS asthma specialists were also comparable to the allergists in a 2014 workforce survey.(31) NCHS evaluated whether lower response rates and the changes in the design and implementation (larger sample size, electronic data collection) introduced bias in 2012 NAMCS and found no or minimal bias in physician-level estimates.(29)
In conclusion, overall agreement, confidence and adherence to the EPR-3 guidelines are higher for specialists than primary care clinicians but vary between different elements. Low rates of agreement and adherence are reported for several important core elements of the guidelines including use of a written asthma treatment plan, use of an asthma control assessment tool, home peak flow monitoring, spirometry performance, repeated assessment of inhaler technique, and environmental control assessment and testing. Follow-up studies to examine reasons for low adherence and interventions designed to increase adherence in these areas may improve guideline use and overall asthma care and may reduce asthma morbidity.
Supplementary Material
Highlights.
What is known about this topic?
Adherence to the 2007 National Asthma Education and Prevention Program’s (NAEPP) Expert Panel Report 3 asthma guidelines have been suboptimal, and a long-standing target of implementation interventions. However, little national data are available on adherence.
What does this article add to our knowledge?
Nationally representative data shows higher adherence among asthma specialists versus primary care clinicians, and highlights overall low clinician adherence with written asthma action plans, home peak flow monitoring, spirometry testing and assessment of inhaler technique.
How does this study impact current management guidelines?
Among primary care physicians who deliver the majority of asthma care, self-efficacy with the recommended measures was a predictor of higher adherence. These data highlight areas for progress in realizing clinical asthma guidelines.
Acknowledgments
We acknowledge Anjali Talwakar, MD and Elizabeth Rechsteiner for their assistance in processing the NAS data. The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention. This research was supported in part by the Intramural Research Program of the NIH, National Institute of Environmental Health Sciences (Grant number: Z01-ES-025041).
Abbreviations
- AAP
Asthma Action Plan
- CHC
Community Health Center
- EPR-3
Expert Panel Report 3
- ETS
Environmental Tobacco Smoke
- ICS
Inhaled corticosteroids
- LABA
Long acting beta agonist
- NAEPP
National Asthma Education and Prevention Program
- NAMCS
National Ambulatory Medical Care Survey
- NAS
National Asthma Survey of Physicians
- RSE
relative standard error
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure: No conflicts of interest for any author.
References
- 1.National Asthma Education and Prevention Program. Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma. National Heart, Lung, and Blood Institute, National Institutes of Health; 2007. Aug 28, 2007. [Google Scholar]
- 2.Abdel-Kader K, Greer RC, Boulware LE, Unruh ML. Primary care physicians’ familiarity, beliefs, and perceived barriers to practice guidelines in non-diabetic CKD: a survey study. BMC Nephrol. 2014;15:64. doi: 10.1186/1471-2369-15-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Aujoulat I, Jacquemin P, Rietzschel E, Scheen A, Trefois P, Wens J, et al. Factors associated with clinical inertia: an integrative review. Adv Med Educ Pract. 2014;5:141–7. doi: 10.2147/AMEP.S59022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Karam M, Holland C, Yang Z, Samuels K, Sanders G. Allergen immunotherapy at university health services and allergist’s reasons for guidelines nonadherence. Allergy and asthma proceedings: the official journal of regional and state allergy societies. 2017;38(2):115–20. doi: 10.2500/aap.2017.38.4017. [DOI] [PubMed] [Google Scholar]
- 5.Seidu S, Khunti K. Non-adherence to diabetes guidelines in primary care - the enemy of evidence-based practice. Diabetes Res Clin Pract. 2012;95(3):301–2. doi: 10.1016/j.diabres.2012.01.015. [DOI] [PubMed] [Google Scholar]
- 6.Pronovost PJ. Enhancing physicians’ use of clinical guidelines. JAMA. 2013;310(23):2501–2. doi: 10.1001/jama.2013.281334. [DOI] [PubMed] [Google Scholar]
- 7.Boulet LP, FitzGerald JM, Levy ML, Cruz AA, Pedersen S, Haahtela T, et al. A guide to the translation of the Global Initiative for Asthma (GINA) strategy into improved care. The European respiratory journal. 2012;39(5):1220–9. doi: 10.1183/09031936.00184511. [DOI] [PubMed] [Google Scholar]
- 8.Cloutier MM. Asthma management programs for primary care providers: increasing adherence to asthma guidelines. Current opinion in allergy and clinical immunology. 2016;16(2):142–7. doi: 10.1097/ACI.0000000000000242. [DOI] [PubMed] [Google Scholar]
- 9.Doerschug KC, Peterson MW, Dayton CS, Kline JN. Asthma guidelines: an assessment of physician understanding and practice. American journal of respiratory and critical care medicine. 1999;159(6):1735–41. doi: 10.1164/ajrccm.159.6.9809051. [DOI] [PubMed] [Google Scholar]
- 10.Lugtenberg M, Zegers-van Schaick JM, Westert GP, Burgers JS. Why don’t physicians adhere to guideline recommendations in practice? An analysis of barriers among Dutch general practitioners. Implement Sci. 2009;4:54. doi: 10.1186/1748-5908-4-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.National Center for Health Statistics Division of Health Care Statistics. 2012 NAMCS micro-data file documentation. Hyattsville, MD: National Center for Health Statistics; 2016. [August 21, 2015:[Available from: ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NAMCS/doc2012.pdf. [Google Scholar]
- 12.National Center for Health Statistics Division of Health Care Statistics. National Ambulatory Medical Care Survey 2012 Asthma Supplement. Hyattsville, MD: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2012. [Available from: https://www.cdc.gov/nchs/data/ahcd/2012_NAMCS_Asthma_Supplement.pdf. [Google Scholar]
- 13.National Center for Health Statistics Division of Health Care Statistics. Physician Induction Interview Sample Card. Hyattsville, MD: National Center for Health Statistics; 2012. [OMB No. 0920-0234:[Available from: https://www.cdc.gov/nchs/data/ahcd/2012_NAMCS_Physician_Induction_Interview_Sample_Card.pdf. [Google Scholar]
- 14.The College of Family Phyisicians of Canada CMA, Royal College. National Physician Survey: 2014 Response Rates. Mississauga, Ontario: National Phyiscian Survey; 2014. [Available from: http://nationalphysiciansurvey.ca/surveys/2014-survey/response-rates/ [Google Scholar]
- 15.Knol MJ, Janssen KJ, Donders AR, Egberts AC, Heerdink ER, Grobbee DE, et al. Unpredictable bias when using the missing indicator method or complete case analysis for missing confounder values: an empirical example. J Clin Epidemiol. 2010;63(7):728–36. doi: 10.1016/j.jclinepi.2009.08.028. [DOI] [PubMed] [Google Scholar]
- 16.Gibson PG, Powell H, Coughlan J, Wilson AJ, Abramson M, Haywood P, et al. Self-management education and regular practitioner review for adults with asthma. Cochrane Database Syst Rev. 2003;(1):CD001117. doi: 10.1002/14651858.CD001117. [DOI] [PubMed] [Google Scholar]
- 17.National Asthma Education and Prevention Program. Guidelines Implementation Panel Report for: Expert Panel Report 3—Guidelines for the Diagnosis and Management of Asthma. National Institutes of Health; 2008. (Report No.: NIH Publication No. 09-6147). [Google Scholar]
- 18.Crocker DD, Kinyota S, Dumitru GG, Ligon CB, Herman EJ, Ferdinands JM, et al. Effectiveness of home-based, multi-trigger, multicomponent interventions with an environmental focus for reducing asthma morbidity: a community guide systematic review. Am J Prev Med. 2011;41(2 Suppl 1):S5–32. doi: 10.1016/j.amepre.2011.05.012. [DOI] [PubMed] [Google Scholar]
- 19.Tumiel-Berhalter LM, Watkins R. The impact of provider knowledge and attitudes toward national asthma guidelines on self-reported implementation of guidelines. The Journal of asthma: official journal of the Association for the Care of Asthma. 2006;43(8):625–8. doi: 10.1080/02770900600878867. [DOI] [PubMed] [Google Scholar]
- 20.Boulet LP, Devlin H, O’Donnell DE. The Physicians’ Practice Assessment Questionnaire on asthma and COPD. Respiratory medicine. 2011;105(1):8–14. doi: 10.1016/j.rmed.2010.07.022. [DOI] [PubMed] [Google Scholar]
- 21.Cimbollek S, Plaza V, Quirce S, Costa R, Urrutia I, Ojeda P, et al. Knowledge, attitude and adherence of Spanish healthcare professionals to asthma management recommendations during pregnancy. Allergologia et immunopathologia. 2013;41(2):114–20. doi: 10.1016/j.aller.2011.09.010. [DOI] [PubMed] [Google Scholar]
- 22.Finkelstein JA, Lozano P, Shulruff R, Inui TS, Soumerai SB, Ng M, et al. Self-reported physician practices for children with asthma: are national guidelines followed? Pediatrics. 2000;106(4 Suppl):886–96. [PubMed] [Google Scholar]
- 23.Yeh KW, Chen SH, Chiang LC, Chen LC, Huang JL. Survey of asthma care in Taiwan: a comparison of asthma specialists and general practitioners. Annals of allergy, asthma & immunology: official publication of the American College of Allergy, Asthma, & Immunology. 2006;96(4):593–9. doi: 10.1016/S1081-1206(10)63555-7. [DOI] [PubMed] [Google Scholar]
- 24.Sheares BJ, Mellins RB, Dimango E, Serebrisky D, Zhang Y, Bye MR, et al. Do Patients of Subspecialist Physicians Benefit from Written Asthma Action Plans? American journal of respiratory and critical care medicine. 2015;191(12):1374–83. doi: 10.1164/rccm.201407-1338OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Diette GB, Skinner EA, Nguyen TT, Markson L, Clark BD, Wu AW. Comparison of quality of care by specialist and generalist physicians as usual source of asthma care for children. Pediatrics. 2001;108(2):432–7. doi: 10.1542/peds.108.2.432. [DOI] [PubMed] [Google Scholar]
- 26.Sokol KC, Sharma G, Lin YL, Goldblum RM. Choosing wisely: adherence by physicians to recommended use of spirometry in the diagnosis and management of adult asthma. Am J Med. 2015;128(5):502–8. doi: 10.1016/j.amjmed.2014.12.006. [DOI] [PubMed] [Google Scholar]
- 27.Murphy KR, Meltzer EO, Blaiss MS, Nathan RA, Stoloff SW, Doherty DE. Asthma management and control in the United States: results of the 2009 Asthma Insight and Management survey. Allergy and asthma proceedings: the official journal of regional and state allergy societies. 2012;33(1):54–64. doi: 10.2500/aap.2011.32.3518. [DOI] [PubMed] [Google Scholar]
- 28.Kellerman SE, Herold J. Physician response to surveys. A review of the literature. Am J Prev Med. 2001;20(1):61–7. doi: 10.1016/s0749-3797(00)00258-0. [DOI] [PubMed] [Google Scholar]
- 29.Hing E, Shimizu IM, Talwalkar A. (Vital and health statistics Series 2, Data evaluation and methods research).Nonresponse Bias in Estimates From the 2012 National Ambulatory Medical Care Survey. 2016;(171):1–42. [PubMed] [Google Scholar]
- 30.Cook JV, Dickinson HO, Eccles MP. Response rates in postal surveys of healthcare professionals between 1996 and 2005: an observational study. BMC Health Serv Res. 2009;9:160. doi: 10.1186/1472-6963-9-160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Association of American Medical Colleges. 2014 Physician Specialty Data Book: Center for Workforce Studies. Washington, DC: Association of American Medical Colleges; 2014. Nov, 2014. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


