Abstract
Our aim was to compare the efficacy of the Therabite® jaw motion rehabilitation system (Atos Medical) with that of wooden spatulas to relieve and prevent trismus in patients who have had radiotherapy for stage three and four oral and oropharyngeal cancer. Secondary aims were to assess the feasibility and the impact of exercise on health-related quality of life (QoL), and the use of health services after treatment. We designed a randomised, open-label, controlled, three-centre feasibility study to compare the effectiveness and cost of the Therabite® and wooden spatulas. We studied compliance with exercises and health-related QoL, assessed cost using three health economics measures, and conducted semistructured interviews with patients. Patients were randomised into two groups: the Therabite® group (n = 37) and the wooden spatula group (n = 34). All patients had some sense of jaw tightening before the study started. Mean mouth opening after six months increased in both groups, but the difference between the groups was not significant (p = 0.39). Completion rates for the three economic measures were good. There was no significant difference between the two groups in frequency of contact with care services or in QoL. Exercises during and after radiotherapy can ameliorate trismus in patients with stage three and four oral and oropharygeal cancers, but differences between groups in efficacy, compliance, QoL, or use of hospital or community health services, were not significant.
Keywords: Trismus, Head and Neck cancer, Randomised trial, Feasibility, Health economics, Exercises
Introduction
Around 7600 patients were diagnosed with cancer of the lip, oral cavity, or oropharynx in the UK in 2013. Trismus, which can develop as a result of the disease or its treatment, is under-reported as a serious complication,1 and radiotherapy is been reported as one of the most common causes. The definition of trismus by Dijkstra et al as a maximum mouth opening of 35 mm or less is now widely accepted.2 Trismus can impair the ability to chew, swallow, and speak, and can be detrimental to oral health, dental integrity, and overall quality of life (QoL).3, 4, 5, 6 Psychological difficulties can include low self-esteem, depression, and suicidal tendencies.7
Studies by van der Molen et al and and Carnaby-Mann et al on jaw exercises in patients treated with chemoradiotherapy for cancer of the head and neck showed less of a decline in mouth opening than standard rehabilitation techniques after treatment. However, both studies were small with only a 10-week follow up, and there were no economic evaluations.8, 9 Current treatments such as the use of wooden spatulas, Therabite® (Atos Medical), Dynasplint® (Dynasplint Systems Inc), and swallowing therapies, have shown only a modest effect once trismus is established.10, 11, 12, 13, 14 However, Scherpenhuizen et al suggested that jaw exercises can improve mouth opening in patients with established radiotherapy-induced trismus.12 In view of these conflicting opinions, there is consensus about the need for a rigorous, controlled study to provide clearer evidence of the value of exercise devices in patients who have trismus before radiotherapy or who have a high risk of developing it afterwards.10
This feasibility study was designed to find out whether exercises are beneficial and to inform the design of a larger study, in line with the Medical Research Council framework for complex interventions.15
Our main aim was to compare the efficacy of the Therabite® with that of the current standard treatment with wooden spatulas to relieve or prevent trismus. Secondary aims were to assess the feasibility and the impact of exercise on health-related QoL, the need for additional treatment, and completion rates of three health economics outcome measures: the Client Service Receipt Inventory (CSRI), EQ-5D-3L (EuroQol), and ICECAP-A (ICEpop CAPability measure for Adults).
Material and methods
This randomised, open-label, controlled, three-centre feasibility study was designed to compare the use of Therabite® with wooden spatulas to treat and relieve trismus in patients with stages three and four oral and oropharyngeal cancer. The study was approved by the North Manchester Ethics Committee (12/NW/0414) and all patients gave written informed consent before the study started.
Patients treated by primary chemoradiotherapy, radiotherapy, or operation followed by chemoradiotherapy or radiotherapy, were recruited from three tertiary referral centres in England. Those who had tightening of the jaw before radiotherapy were invited to participate. They were all prescribed a dose of 60-70 Gy in 30-35 fractions to the jaw over six to seven weeks using intensity-modulated radiotherapy (IMRT).
To detect a minimum mean (SD) difference in mouth opening of 5 (8) mm from baseline (previously estimated from patients who had radiotherapy without operation) with 80% power, required 42 patients/group. With a predicted 25% attrition rate, 112 patients were required in total.
Patients were randomised using the minimisation method with a random element (allocation was with a 0.75 probability to the arm yielding a lower imbalance score or 0.5 if scores were tied). Controlled factors were operation or no operation, centre, and synchronous chemotherapy given or not given. Patients were then instructed to do their exercises according to a set protocol.
Those whose mouth opening was less than 12 mm (not wide enough for the Therabite®), or who were anatomically unable to use the Therabite® because they were partially dentate, and those with a past history of operation or radiotherapy to the head and neck, were excluded.
Protocol for use of Therabite® or wooden spatula and measurement of mouth opening
Patients randomised to either group were asked to follow the 5-5-30 protocol, which comprised five sessions/day for six months. At each session they had to open their mouths for 30 seconds then close it. They had to do this five times.16, 17 They started the exercises about three weeks postoperatively or one to three weeks before radiotherapy, and recorded the maximum mouth opening at the end of each day using a Platon Therabite® range of motion scale (Atos Medical) to show compliance. They also used a Willis bite gauge to measure from the bottom of the nose to the chin with the mouth closed and open at baseline and again three and six months after treatment.
Table 1 shows the patients’ details.
Table 1.
Baseline characteristics of patients.
| Wooden spatulas | Therabite® | |
|---|---|---|
| Centre: | ||
| Liverpool | 10 | 12 |
| Birmingham | 1 | 3 |
| Manchester | 23 | 22 |
| Operation: | ||
| No | 14 | 11 |
| Yes | 20 | 26 |
| Chemoradiation: | ||
| No | 9 | 14 |
| Yes | 25 | 23 |
| Sex: | ||
| Male | 24 | 25 |
| Female | 10 | 12 |
| Alcohol use: | ||
| Current heavy | 4 | 2 |
| Previous heavy | 8 | 16 |
| Never heavy | 22 | 19 |
| Smoking status: | ||
| Current smoker | 4 | 4 |
| Ex smoker | 17 | 25 |
| Never smoked | 13 | 8 |
| Site of disease: | ||
| Oral | 11 | 15 |
| Oropharyngeal | 23 | 22 |
| Stage: | ||
| T1/2 N+ M0 | 14 | 16 |
| T3/4 N0 M0 | 5 | 4 |
| T3/4 N+ M0 | 15 | 17 |
Quality of life
Quality of life (QoL) was assessed at baseline, and at three and six months after treatment using the European Organisation for Research and Treatment of Cancer Quality of Life Questionnaire (EORTC QLQ-C 30) and the Head and Neck (H&N) module (EORTC QLQ H&N 35).18 Data were collected on a pro forma.
Health economics assessments
To assess health economics we used the EQ-5D-3L (European Quality of Life - 5 Dimensions -3 Levels) at baseline and three and six months after treatment.19 This is a validated, generic, health-related, preference-based measure that comprises five domains: mobility; self-care; usual activities; pain and discomfort; and anxiety and depression. Each domain has three levels (no problem, some problems, and major problems) giving a total of 243 possible health states.20 We converted these into EQ-5D-3L index scores (single utility scores anchored at 0 for death and one for perfect health), which can be “negative” if patients consider their health to be worse than death.20, 21 We then translated the index scores into quality-adjusted life years (QALY) by weighting them with quantity of life (the aggregated number of years lived), using the area-under-the-curve method.22, 23 Quality-adjusted life years is a common unit of effect (a measure of utility) that has been advocated by the National Institute for Health and Care Excellence (NICE) in the UK for the evaluation of cost-effectiveness.24
ICECAP-A (ICEpop CAPability measure for Adults) (baseline, and at three and six months) is a measure of QoL with five domains: attachment, security, role, enjoyment, and independence.25
At three and six months we interviewed patients using the Client Service Receipt Inventory (CSRI) to find out how often they had used primary and secondary care services26 such as speech and language therapy; dietary and nutritional advice or artificial feeding, or both, and orthodontic interventions including surgery.
Nested qualitative study
We used semistructured telephone interviews up to six months after completion of the study to find out about the patients’ experiences of the study and how trismus affected their daily lives. To plan possible variables for a future phase III trial, patients were asked about compliance with the protocol and whether pain had affected it. Data were transcribed verbatim and were analysed according to the framework analysis reported by Ritchie and Spencer.27
Data analysis
Statistical analysis was done with the help of Stata statistical software, release 13 (StataCorp LP, College Station, USA) and SPSS for Windows, version 16 (SPSS Inc, Chicago, USA). The null hypothesis for the primary analysis was that there would be no difference between the groups in the amount of mouth opening at six months.
Descriptive statistics were used to report the prevelence of trismus and mouth opening. Similarly descriptive statistics were used to calculate the number of patients who completed different parts of the study and the amount of missing data.
The original power calculation was based on a t test of change in scores, but the analysis of covariance (ANCOVA) is more efficient. An ANCOVA model was fitted with the six-month measurement of mouth opening as the response, and the trial arm as the variable of primary interest after adjustments had been made for baseline, centre, operation, and chemoradiation.
Economic analysis was done using Microsoft Excel 2013 and SPSS Statistics for Windows, version 22 (IBM Corp, Armonk, USA). Confidence intervals (CI) for costs and health-related QoL were estimated using non-parametric bootstrapping methods.28, 29 A simulation of 5000 non-parametric bootstrapping iterations was run to construct 95% CI around estimates of costs and QoL scores using Microsoft Excel 2013.
Results
Of the 237 patients screened, 71 were included. Most of those not included had had no subjective tightening of the jaw or had declined participation.
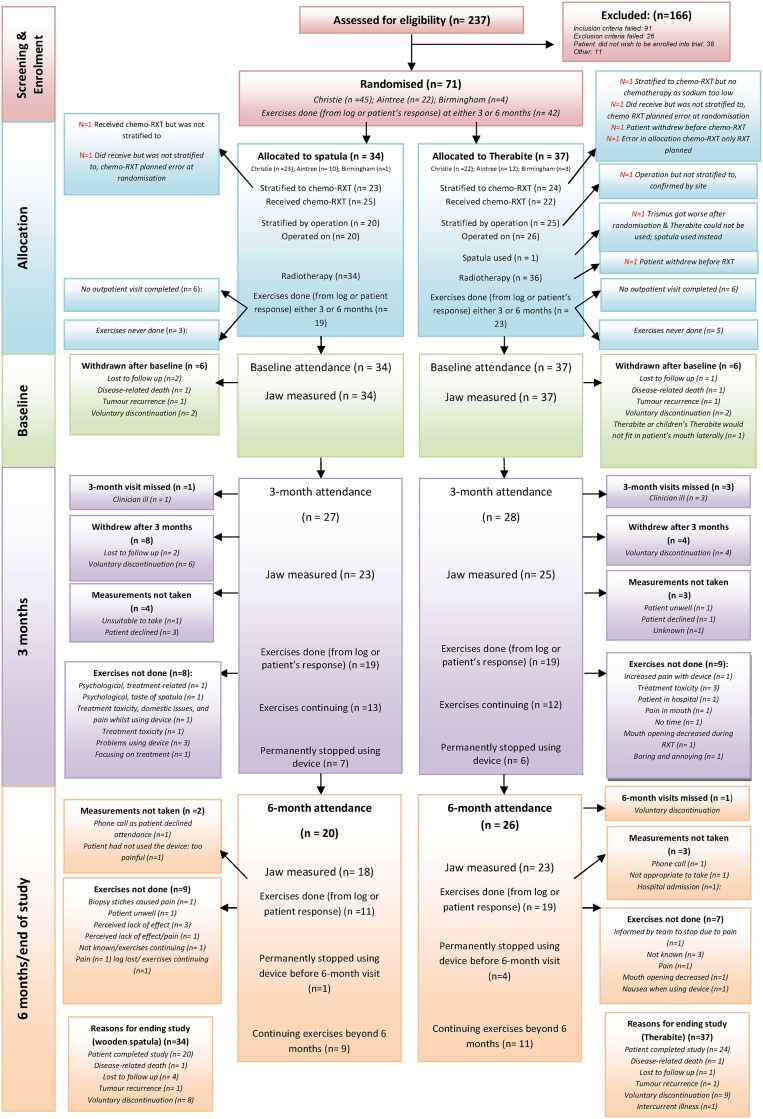
There were 37 patients in the Therabite® group and 34 in the wooden spatula group (Fig. 1). Median (range) maximum mouth opening at baseline was 24.0 (12.0-58.0) mm for the Therabite® group and 21.8 (12.5–48.0) mm for the spatula group. Recorded baseline characteristics (age, sex, previous operation, radiotherapy or chemoradiotherapy, site and stage of disease, use of alcohol, and smoking status) were broadly similar in both groups. This was made possible by using priori stratification factors to minimise differences at baseline (Table 1).
Fig. 1.
Consort diagram.
Maximum mouth opening
Measurements of mouth opening at six months were supplied by 41/71 participants, which may indicate that mouth opening in both groups had not deteriorated. The difference between the two interventions was not significant although the power of the study was low because we failed to achieve the target recruitment and the attrition rate was higher than anticipated. The estimated difference in mean mouth opening at six months after adjustment for baseline, centre, operation, and chemoradiation in an analysis of covariance model was -2.43 mm (95% CI -8.15 to 3.29). This was not significant (t35 = -0.86, 2-tail p = 0.39). There was no formal evidence against two key assumptions of the fitted model: normality of the residuals (Shapiro-Wilk W test, Z = 0.6, 1-tail p = 0.27) and homogeneity of variance (Cook-Weisberg test for heteroskedasticity, X52 = 7.90, 1-tail p = 0.16)
Compliance with the exercises was poor, particularly at the end of radiotherapy, but there were no appreciable differences between the groups (data obtained from the patients’ logs).
Health-related QoL
Subscales (taken from the EORTC QLC-C30) related to eating, weight loss, pain, and mouth opening, were predicted to be more sensitive to changes than others in patients with trismus. However, there was no appreciable difference in the change in mean scores from baseline to six months between groups for any of these items.
Telephone interviews
Telephone interviews were designed to explore the consequences and possible effects of the exercises on pain and compliance with the exercises as well as their nature, acceptability, and impact in terms of motivation and perceived improvement in mouth opening. Of the 15 patients interviewed, some had complied and some had not during the three and six-month follow-up periods, but compliance in the Therabite® group seemed better at both time points. Patients felt they had to stop or do fewer exercises towards the end of the course of radiotherapy until roughly four weeks after it had stopped because of painful mucositis. They began again when the side effects had abated.
Key feasibility and acceptability messages were: change the wording of the exercise regimen to at “least three times a day” rather than five times a day; stop doing the exercises when the side effects of radiotherapy are at their worst; contact healthcare professionals more regularly.
Health economics assessments
Completion rates (at baseline, and at three and six months) of the three health economics measures were: CSRI: 89%, and 100%, at three and six months, respectively; EQ-5D-3L: 90%, 78%, and 87%, respectively; and ICECAP-A: 59%, 49%, and 74%, respectively. Across the time points, overall completion rates were 95%, 85% and 61% for the CSRI, EQ-5D-3L and ICECAP-A, respectively.
Although it was not a core feasibility objective, we also made an exploratory analysis of the cost consequences (from the perspective of the NHS) of the participants who had complete cost and outcome data (n = 30) (Table 2, Table 3, Table 4, Table 5).
Table 2.
Contacts with primary and secondary care health services by 30 participants six months after baseline.
| Therabite (n = 16) | Wooden spatula (n = 14) | Mann Whitney | |
|---|---|---|---|
| Total; mean, median (range) | Total; mean, median (range) | p valuea | |
| NHS primary care: | |||
| Cancer nurse | 10; 0.63, 0 (0-4) | 6; 0.43, 0 (0-6) | 0.313 |
| General practitioner | 51; 3.19, 2 (0-13) | 32; 2.29, 2 (0-5) | 0.697 |
| Practice nurse | 25; 1.56, 0 (0-14) | 7; 0.50, 0 (0-3) | 0.637 |
| Community nurse | 128; 8.00, 1 (0-56) | 47; 3.36, 1 (0-22) | 0.667 |
| Physiotherapist | 2; 0.13, 0 (0-2) | 18; 1.29, 0 (0-9) | 0.294 |
| Speech and language therapist | 43; 2.69, 2 (0-14) | 36; 2.57, 2 (0-9) | 1.000 |
| Occupational health therapist | 0 | 0 | 1.000 |
| Dietician | 41; 2.56, 1 (0-16) | 51; 3.64, 2 (0-11) | 0.637 |
| Other healthcare professional | 81; 5.06, 1 (0-52) | 28; 2.00, 1 (0-10) | 0.667 |
| NHS secondary care: | |||
| Oncology inpatient ward (bed days) | 256; 16.06, 9 (0-78) | 217; 15.50, 6 (0-74) | 0.790 |
| Medical inpatient ward (bed days) | 31; 1.94, 0 (0-14) | 51; 3.64, 0 (0-30) | 0.854 |
| Intensive care inpatient ward (bed days) | 0 | 0 | 1.000 |
| Other inpatient ward (bed days) | 6; 0.38, 0 (0-6) | 0 | 0.790 |
| Physiotherapist inpatient consultation | 62; 3.88, 0 (0-55) | 3; 0.21, 0 (0-2) | 1.000 |
| Speech and language therapist inpatient consultation | 4; 0.25, 0 (0, 2) | 4; 0.29, 0 (0, 2) | 0.918 |
| Dietician inpatient consultation | 56; 3.50, 1 (0, 25) | 38; 2.71, 1 (0, 20) | 0.822 |
| Occupational health therapist inpatient consultation | 2; 0.13, 0 (0, 2) | 0; 0.00, 0 (0, 0) | 0.790 |
| Other inpatient consultation | 3; 0.19, 0 (0, 2) | 0; 0.00, 0 (0, 0) | 0.580 |
| Outpatient visits | 76; 4.75, 1 (0, 30) | 74; 5.29, 1 (0, 58) | 1.000 |
| Accident and emergency | 1; 0.06, 0 (0, 1) | 18; 1.29, 0 (0, 12) | 0.154 |
Significant at 5% significance level.
Table 3.
Mean (SD) costs (£) of all contacts with NHS primary and secondary care services by participants over the six-month follow-up period.
| Therabite (n = 16) | Wooden spatula (n = 14) | Mean difference in £ (bootstrapped 95%CI) | |
|---|---|---|---|
| NHS primary care: | |||
| Cancer nurse | 60.47 (139.12) | 38.57 (144.32) | 21.90 |
| General practitioner | 188.91 (210.35) | 190.82 (194.58) | -1.91 |
| Practice nurse | 18.22 (34.96) | 11.99 (26.24) | 6.23 |
| Community nurse | 307.66 (704.63) | 113.14 (223.99) | 194.52 |
| Physiotherapist | 4.50 (18.00) | 27.85 (56.46) | -23.35 |
| Speech and language therapist | 45.56 (47.64) | 46.93 (48.14) | -1.37 |
| Occupational health therapist | 0.00 (0.00) | 0.00 (0.00) | 0.00 |
| Dietician | 37.77 (49.38) | 95.58 (122.89) | -57.81 |
| Other healthcare professional | 172.48 (316.27) | 135.57 (246.80) | 36.91 |
| Total cost NHS primary care | 835.56 (974.13) | 660.46 (637.13) | 175.10 (-358.51 to 759.77) |
| NHS secondary care: | |||
| Oncology inpatient ward | 9678.00 (12783.29) | 9001.93 (12641.66) | 676.07 |
| Medical inpatient ward | 1110.19 (2532.19) | 2087.36 (4797.26) | -977.17 |
| Intensive care inpatient ward | 0.00 (0.00) | 0.00 (0.00) | 0.00 |
| Other inpatient ward | 120.75 (483.00) | 0.00 (0.00) | 120.75 |
| Physiotherapist inpatient consultation | 164.00 (579.91) | 10.43 (27.76) | 153.57 |
| Speech and language therapist inpatient consultation | 24.13 (54.54) | 27.57 (57.71) | -3.44 |
| Dietician inpatient consultation | 216.19 (388.57) | 169.14 (316.15) | 47.05 |
| Occupational health therapist inpatient consultation | 8.50 (34.00) | 0.00 (0.00) | 8.50 |
| Other inpatient consultation | 16.94 (48.06) | 0.00 (0.00) | 16.94 |
| Outpatient visits | 513.56 (1000.97) | 466.29 (1205.24) | 47.27 |
| Accident and emergency | 6.56 (26.23) | 134.88 (332.85) | -128.32 |
| Total cost NHS secondary care | 11858.81 (14055.02) | 11897.60 (13421.63) | -38.79 (-9463.46 to 9446.84) |
| Total cost NHS primary and secondary care | 12694.37 (14136.93) | 12558.06 (13675.36) | 136.31 (-9419.24 to 9791.03) |
| Intervention cost (intervention – Therabite and control – wooden spatula) | 251.94 (0.00) | 2.84 (0.00) | 249.10 |
| Total cost | 12946.31 (14136.93) | 12560.90 (13675.36) | 385.41 (-8916.37 to 10013.82) |
NHS: National Health Service
Table 4.
Mean (SD) EQ-5D-3L index scores, mean (SD) quality-adjusted life years (QALY) and incremental mean (SD) QALY six months after baseline.
| Therabite (n = 16) |
Wooden spatula (n = 14) |
Incremental mean QALY between groupsa (bootstrapped 95% CI) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Baseline | 3 months | 6 months | QALY over 6 months | Baseline | 3 months | 6 months | QALY over 6 months | ||
| EQ-5D-3L index | 0.6914 (0.1863) | 0.6209 (0.2806) | 0.6935 (0.2523) | 0.3283 (0.1082) | 0.6232 (0.3599) | 0.6824 (0.2999) | 0.7481 (0.1844) | 0.3420 (0.1330) | -0.0137 (-0.0978 to 0.0706) |
Incremental mean QALY between groups = mean QALY for intervention group minus mean QALY for control group.
Table 5.
Mean (SD) ICECAP-A capability index scores, change in mean ICECAP-A index score between study time points and difference in mean (SD) change in scores between groups six months after baseline (n = 19/30).b
| Therabite® (n = 8)b |
Wooden spatula (n = 11)b |
Difference in mean change scores between groupsa (bootstrapped 95% CI) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Baseline | 3 months | 6 months | Change in mean score between baseline and 6 months | Baseline | 3 months | 6 months | Change in mean score between baseline and 6 months | ||
| ICECAP-A capability index scores | 0.8733 (0.1092) | 0.8095 (0.1967) | 0.8551 (0.1209) | -0.0182 (0.0873) | 0.8914 (0.1524) | 0.9175 (0.0927) | 0.9079 (0.1506) | 0.0165 (0.2029) | -0.0347 (-0.1726 to 0.0828) |
Difference in mean change scores between groups = (Mean change score for intervention) minus (Mean change score for control).
ICECAP-A analysis was conducted on 19 out of 30 participants who had complete ICECAP-A data (n = 8 Therabite® group, n = 11 wooden spatula group).
Table 2 shows the number of contacts with primary and secondary care health services six months after baseline. Differences between the groups were not significant. Table 3 shows the mean costs of all contacts with NHS primary and secondary care services over the same period. The Therabite® intervention cost £251.94/patient compared with £2.84/patient for wooden spatulas. The mean (SD) total cost/patient was £12 946 (£14 137) in the Therabite® group and £12 561 (£13 675) in the spatula group (£385 more in the Therabite® group; bootstrapped 95% CI: -£8916 to £10 014).
Table 4 shows mean EQ-5D-3L index scores, mean (SD) quality-adjusted life years (QALY) and incremental mean (SD) QALY between the groups over the six-month period.
Change in mean ICECAP-A index scores between study time points and the difference in change in the mean ICECAP-A index scores between groups over the six-month study period were assessed for 19 of the 30 participants who had complete ICECAP-A data (Table 5).
Discussion
A recent systematic review has shown that exercises with devices to mobilise the jaw after treatment yield better results than no exercise in patients with radiotherapy-induced trismus after treatment for cancer of the head and neck.12 Our study has shown that exercises with the Therabite® or wooden spatulas, before, during, and after radiotherapy, can relieve radiation-induced trismus in this group. Melchers et al described an increase in mouth opening when patients did the exercises more often.30 The authors also found that self-discipline and clearly-set objectives were important for maintaining the necessary effort. The main factor that negatively affected adherence was painful mucositis, as in our study. Other factors, such as anxiety, ill-fitting Therabite® pads, and failure to set goals during treatment, also had a negative effect. Tang et al showed that rehabilitation training can slow down the progress of trismus in patients with nasopharyngeal carcinoma after radiotherapy.31 Several studies have shown that use of a Therabite® was no more effective than use of wooden spatulas or active range-of-motion exercises.32, 33 However, Pauli et al reported that mouth opening increased more after use of a Therabite® than after use of the Engström device (a wooden clothespeg with an attached rubber band), although compliance was comparable.34 An earlier study by Buchbinder et al also showed that the Therabite® was more efficient than unassisted stretching or stretching using wooden spatulas, although it included only a small number of patients.35
Limitations of the study
Patients who felt a tightening of the jaw before radiotherapy were included in the study, but those in whom it may have developed during treatment were omitted. This could be considered in a more adaptive study design such as a stepped wedge design in which patients would be randomised as soon as the jaw tightened.
A larger group of patients and more study-specific follow up may have provided more representative data on both the quantitative and qualitative aspects of the study. Telephone interviews with a larger group of patients would have provided additional information about the problems they face. Patients’ suggestions to alter the exercise regimen to “up to five times a day”, when exercises were more likely to be done three times a day, have not been validated. A dose-effect analysis of a new protocol would be required in future studies.
The attrition rate for this study, which was set at 25% as in other head and neck cancer toxicity intervention studies, was higher than we expected. This could have been caused by the demands of the prescribed exercise regimen and the difficulty of complying in the presence of severe mucositis.
It would be useful to use a more sensitive scale such as the Gothenburg Trismus Questionnaire to measure trismus-specific symptoms in a full-scale trial, as it can be used to track changes in symptoms.36 Unfortunately it was not available at the start of our study.
To the best of our knowledge, this is the first study to provide a exercise regimen before radiotherapy, and to include a health economics aspect within the design to enable healthcare professionals make evidence-based decisions about treatment and use of resources. The overall response rates for all the health economics measures were good. In line with a study by Clarke et al, our findings show that it is feasible to collect information about health economics in a definitive randomised trial in this group.37
In conclusion, this feasibility study has shown that mouth opening had generally increased in both groups, and that exercises during and after radiotherapy can relieve trismus in these patients.
Conflict of interest
We have no conflicts of interest.
Ethics statement/confirmation of patients’ permission
The study was approved by the ethics committee and all patients gave written informed consent before the study started.
Acknowledgements
We would like to thank the dedicated clinical, research, and allied health professional teams in helping to run this study. Special thanks for all patients for their participation, help, and time in assisting with this study.
Footnotes
The Christie NHS Foundation Trust acknowledges the support of the National Institute of Health Research Clinical Research Network (NIHR CRN:-Trismus RfPB trial (portfolio ID 13415).
Trial registration with clinicaltrials.gov NCT01733797.
References
- 1.Lee R., Slevin N., Musgrove B. Prediction of post-treatment trismus in head and neck cancer patients. Br J Oral Maxillofac Surg. 2012;50:328–332. doi: 10.1016/j.bjoms.2011.06.009. [DOI] [PubMed] [Google Scholar]
- 2.Dijkstra P.U., Huisman P.M., Roodenburg J.L. Criteria for trismus in head and neck oncology. Int J Oral Maxillofac Surg. 2006;35:337–342. doi: 10.1016/j.ijom.2005.08.001. [DOI] [PubMed] [Google Scholar]
- 3.Weber C., Dommerich S., Pau H.W. Limited mouth opening after primary therapy of head and neck cancer. Oral Maxillofac Surg. 2010;14:169–173. doi: 10.1007/s10006-010-0220-2. [DOI] [PubMed] [Google Scholar]
- 4.Scott B., Butterworth C., Lowe D. Factors associated with restricted mouth opening and its relationship to health-related quality of life in patients attending a maxillofacial oncology clinic. Oral Oncol. 2008;44:430–438. doi: 10.1016/j.oraloncology.2007.06.015. [DOI] [PubMed] [Google Scholar]
- 5.Louise Kent L., Brennan M.T., Noll J.L. Radiation-induced trismus in head and neck cancer patients. Support Care Cancer. 2008;16:305––309. doi: 10.1007/s00520-007-0345-5. [DOI] [PubMed] [Google Scholar]
- 6.Scott B., D’Souza J., Perinparajah N. Longitudinal evaluation of restricted mouth opening (trismus) in patients following primary surgery for oral and oropharyngeal squamous cell carcinoma. Br J Oral Maxillofac Surg. 2011;49:106–111. doi: 10.1016/j.bjoms.2010.02.008. [DOI] [PubMed] [Google Scholar]
- 7.Zeller J.L. High suicide risk found for patients with head and neck cancer. JAMA. 2006;296:1716–1717. doi: 10.1001/jama.296.14.1716. [DOI] [PubMed] [Google Scholar]
- 8.van der Molen L., van Rossum M.A., Burkhead L.M. A randomized preventive rehabilitation trial in advanced head and neck cancer patients treated with chemoradiotherapy: feasibility, compliance, and short-term effects. Dysphagia. 2011;26:155–170. doi: 10.1007/s00455-010-9288-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Carnaby-Mann G., Crary M.A., Schmalfuss I. “Pharyngocise”: randomized controlled trial of preventative exercises to maintain muscle structure and swallowing function during head-and-neck chemoradiotherapy. Int J Radiat Oncol Biol Phys. 2012;83:210–219. doi: 10.1016/j.ijrobp.2011.06.1954. [DOI] [PubMed] [Google Scholar]
- 10.Carvalho A.P., McNeely M.L., Vital F.M. Interventions for preventing and treating trismus in patients with head and neck cancer. Cochrane Database of Systematic Reviews. 2016;8 [Google Scholar]
- 11.Rapidis A.D., Dijkstra P.U., Roodenburg J.L. Trismus in patients with head and neck cancer: etiopathogenesis, diagnosis and management. Clin Otolaryngol. 2015;40:516–526. doi: 10.1111/coa.12488. [DOI] [PubMed] [Google Scholar]
- 12.Scherpenhuizen A., van Waes A.M., Janssen L.M. The effect of exercise therapy in head and neck cancer patients in the treatment of radiotherapy-induced trismus: a systematic review. Oral Oncol. 2015;51:745–750. doi: 10.1016/j.oraloncology.2015.05.001. [DOI] [PubMed] [Google Scholar]
- 13.Loorents V., Rosell J., Karlsson C. Prophylactic training for the prevention of radiotherapy-induced trismus- a randomised study. Acta Oncol. 2014;53:530–538. doi: 10.3109/0284186X.2014.892211. [DOI] [PubMed] [Google Scholar]
- 14.Kamstra J.I., Roodenburg J.L., Beurskens C.H. TheraBite exercises to treat trismus secondary to head and neck cancer. Support Care Cancer. 2013;21:951–957. doi: 10.1007/s00520-012-1610-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Medical Research Council; 2006. Developing and evaluating complex interventions: new guidance. Available from URL: https://www.mrc.ac.uk/documents/pdf/complex-interventions-guidance/ (last accessed 10 February 2018) [Google Scholar]
- 16.Atos Medical; 2009. Therabite® jaw motion rehabilitation system. Available from URL: https://www.atosmedical.co.uk/product/therabite-jaw-motion-rehabilitation-system/ (last accessed 10 February 2018) [Google Scholar]
- 17.Bandy W.D., Irion J.M. The effect of time on static stretch on the flexibility of the hamstring muscles. Phys Ther. 1994;74:845–852. doi: 10.1093/ptj/74.9.845. [DOI] [PubMed] [Google Scholar]
- 18.EORTC QLQ-C30. EORTC Quality of life. Available from URL: http://groups.eortc.be/qol/eortc-qlq-c30 (last accessed 10 February 2018).
- 19.EuroQoL Group. EQ-5D-3L, 2017. Available from URL: https://euroqol.org/eq-5d-instruments/eq-5d-3l-about/ (last accessed 10 February 2018).
- 20.Kind P., Hardman G., Macran S. Centre for Health Economics, University of York; York: 1999. UK population norms for EQ-5D. Discussion paper 172. [Google Scholar]
- 21.Dolan P., Gudex C., Kind P. Centre for Health Economics, University of York; York: 1995. A social tariff for EuroQoL: results from a UK general population survey. Discussion paper 138. [Google Scholar]
- 22.Morris S., Devlin N., Parkin D. John Wiley & Sons; Chichester: 2007. Economic analysis in health care. [Google Scholar]
- 23.Drummond M.F., Sculpher M.J., Claxton K. 4th ed. Oxford University Press; Oxford: 2015. Methods for the economic evaluation of health care programmes. [Google Scholar]
- 24.National Institute for Health and Care Excellence (NICE). Guide to the methods of technologyappraisal 2013. Available from URL: https://www.nice.org.uk/process/pmg9/resources/guide-to-the-methods-of-technology-appraisal-2013-pdf-2007975843781 (last accessed 10 February 2018).
- 25.Flynn T.N., Huynh E., Peters T.J. Scoring the Icecap- a capability instrument. Estimation of a UK general population tariff. Health Econ. 2015;24:258–269. doi: 10.1002/hec.3014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.DIRUM (Database of instruments for resource use measurement). Available from URL:http://www.dirum.org/ (last accessed 10 February 2018).
- 27.Ritchie J., Spencer L. Qualitative data analysis for applied policy research. In: Bryman A., Burgess R.G., editors. Analyzing qualitative data. Routledge; Oxford: 1994. pp. 172–194. [Google Scholar]
- 28.Gray A.M., Clarke P.M., Wolstenholme J.L. Oxford University Press; Oxford: 2011. Applied methods of cost-effectiveness analysis in health care. [Google Scholar]
- 29.Russell I.T., Edwards R.T., Gliddon A.E. Cancer of oesophagus or gastricus- new assessment of technology of endosonography (COGNATE): report of pragmatic randomised trial. Health Technol Assess. 2013;17:1–170. doi: 10.3310/hta17390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Melchers L.J., Van Weert E., Beurskens C.H. Exercise adherence in patients with trismus due to head and neck oncology: a qualitative study into the use of the Therabite. Int J Oral Maxillofac Surg. 2009;38:947––954. doi: 10.1016/j.ijom.2009.04.003. [DOI] [PubMed] [Google Scholar]
- 31.Tang Y., Shen Q., Wang Y. A randomized prospective study of rehabilitation therapy in the treatment of radiation-induced dysphagia and trismus. Strahlenther Onkol. 2011;187:39–44. doi: 10.1007/s00066-010-2151-0. [DOI] [PubMed] [Google Scholar]
- 32.Ren W.H., Ao H.W., Lin Q. Efficacy of mouth opening exercises in treating trismus after maxillectomy. Chin Med J (Engl) 2013;126:2666––2669. [PubMed] [Google Scholar]
- 33.Høgdal N., Juhl C., Aadahl M. Early preventive exercises versus usual care does not seem to reduce trismus in patients treated with radiotherapy for cancer in the oral cavity or oropharynx: a randomised clinical trial. Acta Oncol. 2015;54:80––87. doi: 10.3109/0284186X.2014.954677. [DOI] [PubMed] [Google Scholar]
- 34.Pauli N., Andréll P., Johansson M. Treating trismus: a prospective study on effect and compliance to jaw exercise therapy in head and neck cancer. Head Neck. 2015;37:1738–1744. doi: 10.1002/hed.23818. [DOI] [PubMed] [Google Scholar]
- 35.Buchbinder D., Currivan R.B., Kaplan A.J. Mobilization regimens for the prevention of jaw hypomobility in the radiated patient: a comparision of three techniques. J Oral Maxillofac Surg. 1993;51:863–867. doi: 10.1016/s0278-2391(10)80104-1. [DOI] [PubMed] [Google Scholar]
- 36.Johnson J., van As-Brooks C.J., Fagerberg-Mohlin B. Trismus in head and neck cancer patients in Sweden: incidence and risk factors. Med Sci Monit. 2010;16 [PubMed] [Google Scholar]
- 37.Clarke M., Hogan V., Buck D. An external pilot study to test the feasibility of a randomised controlled trial comparing eye muscle surgery against active monitoring for childhood intermittent exotropia [X(T)] Health Technol Assess. 2015;19:1–144. doi: 10.3310/hta19390. [DOI] [PMC free article] [PubMed] [Google Scholar]