Abstract
Objective
Disclosure of HIV status among children and adolescents living with HIV has both beneficial and challenging aspects. To address existing knowledge gaps and update the literature on childhood disclosure, we conducted a systematic review on caregivers’ perceptions and practices of HIV disclosure in low- and middle-income countries (LMICs).
Methods
Standard databases were searched for studies conducted in LMICs, published in English between 2004 and 2015. Excluded articles were reviews or case reports, and those not reporting childhood disclosure. Data regarding prevalence, correlates and impact of disclosure, were presented as frequencies.
Results
Two authors independently screened 982 articles. After applying eligibility criteria, 22 articles representing 12 countries and 2,843 children were reviewed. The proportion of fully disclosed children ranged from 1.7% to 41.0%. Up to 49.5% children were provided “deflected” information (use of a non-HIV-related reason for explaining illness and health care visits). Factors associated with full disclosure included antiretroviral treatment initiation and caregivers’ felt need for maintaining optimal adherence. Barriers to disclosure included fear of negative psychological reactions and inadvertent disclosure to others. Caregivers perceived a strong need for active participation from health care providers to aid the process of disclosure.
Conclusions
Full disclosure of HIV status was not common among children and adolescents in LMICs, while the practice of deflected disclosure was prominent. Caregivers perceived the need for support from health care providers during the disclosure process. Evidence-based guidelines incorporating the developmental status of the child, locally prevalent cultures, and caregiver perceptions are prerequisite to enhancing disclosure in these settings.
Index terms: HIV, children, disclosure, low- and middle-income countries, systematic review
The advent of combination antiretroviral therapy (ART), better health care delivery systems and wider access to ART, ushered in an era of increased survival for children living with HIV.1 The prospect of a longer life span brings forth new issues related to the impact of HIV infection on the normative developmental processes such as growth, peer relationships, puberty, and sexuality. One of the greatest challenges is that of disclosure to the child of their own seropositive status by their parents or caregivers.2 This involves informing them about a potentially life-threatening and transmissible illness associated with significant social stigma, especially in the context of culturally complex settings in low- and middle-income countries (LMIC).
The United Nations Convention on the Rights of the Child states in article 17 that every child should have “access to information and material from a diversity of national and international sources, especially those aimed at the promotion of his or her social, spiritual and moral well-being and physical and mental health.”3 Guidelines for disclosure of HIV status to children were first put into place by the American Academy of Pediatrics in 1999 that stated that all adolescents should know their HIV status and that disclosure should be considered for school-age children.4 In recognition of the health benefits of disclosure even in younger children, and little evidence of psychological or emotional harm from HIV disclosure, the World Health Organization (WHO) in 2011 published guidelines on HIV disclosure counseling for children up to 12 years of age.5 Positive benefits of disclosure were seen in other illnesses; children suffering from cancer were able to cope with the disease better with fewer psychosocial problems if they were appropriately informed.6 Patients are likely to fare better when they are told the truth, which is essential in developing a stable physician–patient relationship conducive to treating a chronic disease.7
Another important aspect in the physician–patient relationship is family involvement, particularly in HIV,8 which is complicated by the inherent stigma of the disease, parental guilt for transmitting the illness to the child, and fear of public disclosure; these factors are strong deterrents to disclosure of HIV status to the child.8,9 The decision to provide complete disclosure rests heavily on caregivers although health care providers should be willing to be truthful in answering questions raised by the patient.10
The role of health care providers as perceived by the caregivers of the child also warrants importance in LMICs. Health care providers are more likely to favor disclosure in an age-appropriate fashion in order to prevent feelings of isolation and anxiety resulting from nondisclosure among their patients.11,12 It has been recommended that disclosure be initiated and followed procedurally taking into account the cognitive level of the child based on Paiget’s cognitive development theory.13 Two recent reviews on pediatric HIV disclosure in LMICs by Pinzon-Iregui et al and Vreeman et al14,15 have described the most common reasons for and against disclosure in these settings. However, these reviews do not address caregiver perceptions through the process of disclosure and the high rates of providing deflected information in LMIC settings, particularly the last decade. We undertook this review aiming to update knowledge about pediatric HIV disclosure and to identify knowledge gaps in the process of disclosure among children and adolescents living with HIV in LMICs.
Methods
Our search strategy aimed to identify studies that could provide information on disclosure status and determinants of disclosure among children and adolescents living with HIV in LMICs. We systematically searched the scientific databases PubMed, Embase, Cochrane Central Register of Controlled Trials, Google Scholar and Medscape, using the search terms, “HIV,” “AIDS,” “disclosure,” “children” or “pediatric,” “adolescent” and “resource-limited settings” or “low-and-middle income” or “LMIC settings.” The search terms used controlled vocabulary and included combinations intended to capture reports of disclosure (e.g., “disclos*”) in children (e.g., “adolescen*,” “child*”). Two authors independently conducted the search. Our search included studies written in English and conducted in a LMIC as defined by the World Bank classification16 and published in the last 10 years to gauge contemporary disclosure practices. Only those articles published after 2004 were included as we believed that the widespread ART access that became available after 2002 was likely to have influenced disclosure in a more uniform manner. We excluded studies that were interventional in design as these studies selectively included patients who had no knowledge of their positive status, or those studies that did not involve children or adolescents in HIV disclosure. The references cited in retrieved articles were also searched and included if eligible. Predefined variables of sample size in each article, disclosure type, including prevalence and correlates of disclosure, reasons for disclosure and preferred personnel for disclosure that were described in each article were noted and tabulated in a spreadsheet.
Definitions of disclosure were formulated based on themes prevalent in literature pertaining to pediatric HIV disclosure and were broadly termed as “full,” “partial,” “no” and “deflected” disclosure, which are further described in Box 1. The studies were reviewed critically by all 4 coauthors to determine inclusion, and disagreements were settled by consensus.
Box 1. Definitions of disclosure.
Full disclosure: Disclosure was generally considered as “full” when it involved the caregiver having disclosed to the child that he or she has HIV specifically.
Partial disclosure: Disclosure was considered “partial” when the illness was described in a way that was consistent with HIV although the term “HIV” was avoided.
No disclosure: When the caregiver reported telling the child nothing about his or her illness.
Deflected disclosure: The strategy of deceptive disclosure that caregivers often use, frequently out of concern for the child’s psychological well-being, telling their children only about an unrelated condition (e.g., asthma, cancer), and attributing all medical needs (e.g., appointments, medication) to that less-stigmatized condition.
Results
Article Inclusion
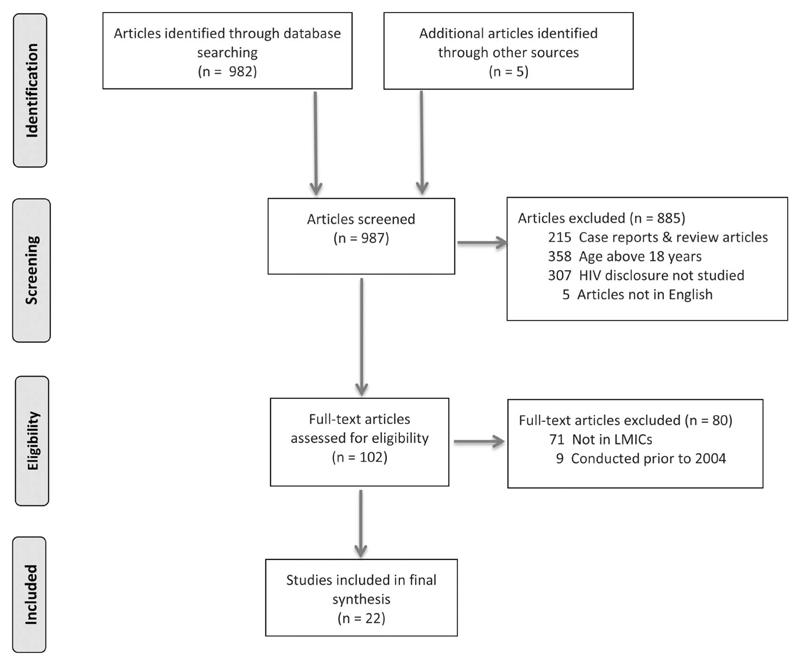
The initial broad search identified 982 articles. Five additional articles were identified through bibliography searches. Among the total of 987 articles, 358 were ineligible, as they were not centered on child disclosure; and another 307 were studies that analyzed HIV adherence rather than disclosure. A further 215 articles were excluded as they were review articles, case reports, or interventional studies. Five articles were non-English and 71 articles reported studies not conducted in LMICs and were thus not included. Nine articles that reported studies conducted prior to 2004 were removed, resulting in 22 articles17–38 that were included in the final analysis (Fig. 1).
Figure 1. Flow diagram of the phases of this systematic review.
Data Extraction and Study Sites
A structured data extraction table was used to evaluate returned articles. Relevant data from the studies were tabulated by 2 authors (C.B. and R.T.) and verified independently by another author (K.M.). Tabulated data variables included the study population or place where the study was conducted, the tools used for collecting information such as hospital-based interview administered by research staff or self-administered questionnaire, sociodemographic factors, definition and method of disclosure, patterns and correlates of disclosure, and supportive or opposing arguments for disclosure. Of the 22 studies included in this review, most were cross-sectional studies conducted in a hospital or clinic setting that engaged children and their primary caregivers receiving health care at that setting (Table 1). The studies were conducted in the following countries: Kenya, Ghana, Nigeria, Congo, Tanzania, Uganda, Zambia, South Africa, Brazil, Thailand, and India. A majority of the children were described as being perinatally infected and aged between 1 and 17 years. Factors statistically associated with disclosure were considered as “correlates” of disclosure in the review. The reasons for disclosure and nondisclosure described in some of these included articles were tabulated and reported.
Table 1. Summary of Articles Included in the Systematic Review.
| Patterns of Disclosure (Proportion) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|
| Authors | Year and Place | Setting | Number of Children or Caregivers Interviewed | Age of Children, Mean or Median (Range) in Years | Age at Disclosure, Mean or Median (Range) in Years | Full Disclosure (%) | No Disclosure (%) | Partial Disclosure (%) | Deflected Disclosure (%) |
| Kouyoumdjian et al, J Trop Pediatr. 200528 | 2001, South Africa | Hospital/clinic based | 17 caregivers | NR | NR | NR | NR | NR | NR |
| Boon Yasidhi et al, J Med Assoc Thai. Nov 200523 | 2005, Bangkok, Thailand | Hospital/clinic based | 96 caregivers, 19 children | Mean 9.6 (5–15) | Mean 9.6 ± 3.2 | 19.8 | NR | NR | NR |
| Abadia-Barrero et al, AIDS Patient Care STDs. 200615 | 1999–2001, Sao Paolo, Brazil | Community based | 36 children | (1–15) | NR | NR | NR | NR | NR |
| Bikaako-Kajura et al, AIDS Behav. 200614 | 2002, Kampala, Uganda | Hospital/clinic based | 42 caregiver–child pairs | Median 12 (5–17) | NR | 29 | 33 | 38 | Yes, not specified |
| Oberdorfer et al, J Paediatr Child Health. 200619 | 2004, Chiang Mai, Thailand | Hospital/clinic based | 103 caregiver–child pairs | Mean 9.5 ± 3.3 (6–16) | Mean 9.2 ± 3 (6–16) | 30.1 | NR | NR | 49.5 |
| Moodley et al, S Afr Med J. 200622 | 2006, Cape Town, South Africa | Hospital/clinic based | 176 children | Median 3.3 (0–11) | Mean 8.1 (5–11) | 9 | NR | NR | NR |
| Menon et al, J Acquir Immune Defic Syndr. 200721 | 2007, Lusaka, Zambia | Hospital/clinic based | 127 children | Mean 12.4 ± 1.4 (11–15) | NR | 37.8 | NR | NR | NR |
| Vaz et al, AIDS Care. 200826 | 2008, Kinshasa, Congo | Hospital/clinic based | 19 youth, 21 caregivers | Mean 16.1 (11–21) | Median 15 | 100* | — | — | — |
| Arun et al, Indian J Pediatr. 200916 | 2007, New Delhi, India | Hospital/clinic based | 50 children | Mean 8.98 ± 0.4 | NR | 14 | 68 | 0 | 18 |
| Vreeman et al, AIDS Patient Care and STDs. 201025 | 2007, Western Kenya | Hospital/clinic based | 120 caregivers | Mean 6.8 ± 6.4 (0–14) | NR | 1.7 | NR | NR | Yes, not specified |
| Vaz et al, AIDS Patient Care and STDs. 201017 | 2009, Kinshasa, Congo | Hospital/clinic based | 259 children | (8–17) | Median 13 | 3 | 97 | — | — |
| Bhattacharya et al, J Trop Pediatr. 201018 | 2010, New Delhi, India | Hospital/clinic based | 145 caregiver–child pairs | Mean 9.1 ± 2.5 | Mean 9.1 ± 1.4 | 41 | 14.5 | 0 | 44.1 |
| Biadgilign et al, PLoS One 201130 | 2008, Addis Ababa, Ethiopia | Hospital/clinic based | 390 caregiver–child pairs | Mean 8.5 ± 2.9 (1–14) | NR | 17.4 | 50.3 | 0 | 32.3 |
| Brown et al, AIDS Care. 201124 | 2009, Ibadan, Nigeria | Hospital/clinic based | 96 children–caregiver pairs | Mean 8.8 ± 2.2 (6–14) | Mean 8.7 ± 2.2 | 13.5 | NR | NR | NR |
| Kallem et al, AIDS Behav. 201020 | 2009, Accra, Ghana | Hospital/clinic based | 71 children–caregiver pairs | Mean 10.4 ± 1.7 (8–14) | NR | 9.8 | 79 | 0 | 11.2 |
| Vaz et al, J Dev Behav Pediatr. 201131 | 2011, Kinshasa, Congo | Hospital/clinic based | 201 caregivers | Median 8 (5–17) | NR | 0† | 46 | 15 | 33 |
| Stewart et al, AIDS Care. 201227 | 2007, Nairobi, Kenya | Community based | 271 caregivers | Median 9 (IQR 7–12) | NR | 19 | NR | NR | NR |
| Abebe et al, AIDS Care. 201229 | 2009, Addis Ababa, Ethiopia | Hospital/clinic based | 172 caregivers | Mean 9.4 ± 6.4 (6–15) | Median 10 ± 3 | 16.3 | NR | NR | NR |
| Negese et al, ISRN AIDS. 201234 | 2012, North Gondar, Ethiopia | Hospital/clinic based | 428 caregivers | Mean 9.96 ± 3 | Mean 10.7 ± 2.3 | 39.5 | NR | NR | NR |
| Vreeman et al, Plos One 201435 | 2011–2012, Western Kenya | Hospital/clinic based | 792 caregiver–child pairs | Mean 9.8 ± 2.6 (6–14) | NR | 26 | NR | NR | NR |
| Atwiine et al, AIDS Care. 201433 | 2012, Southwestern Uganda | Hospital/clinic based | 307 caregiver–child pairs | Median 8 (IQR 7–11) | NR | 31 | 49 | 7 | 13 |
| Mumburi et al, Pan Afr Med J. 201432 | 2011–2012, Moshi, Tanzania | Hospital/clinic based | 211 caregiver–child pairs | Mean 9.7 ± 2.6 (5–14) | Mean 10.6 ± 1.7 (6–14) | 22.3 | 53.1 | 24.6 | 0 |
Sample included only fully disclosed.
Sample included only those not yet disclosed. NR, not reported.
Definitions, Rates, and Patterns of Disclosure
Due to the lack of a “gold standard” definition of disclosure in available literature, we found a good deal of variability when different degrees of disclosure were discussed by various authors. However, our review found certain consistent themes of disclosure described by various authors. Box 1 summarizes the concepts of “full,” “partial,” “no” and “deflected” disclosure described by various authors. We have discussed these themes in our review.
The overall rate of disclosure reported in these studies was low as shown in Table 1. The rate of “full disclosure” was 1.7% to 41.0% and had a wide range. Partial disclosure was reported in some studies and ranged from 7.0% to 38.0%. The proportion of children who were not disclosed to was as high as 97.0% in one study,20 with half the studies that documented no disclosure reporting that over 50.0% of their participants were not disclosed to (Table 1). The prevalence of providing deflected information ranged from 11.2% to 49.5% (Table 1). The range of the reported patterns of disclosure is depicted in Figure 2. There was no correlation between mean or median age at disclosure and the proportion of those with full disclosure indicating that the age at disclosure was variable across the studies. The concept of disclosure was addressed in 2 different ways by the respective authors. In some cases, disclosure was considered a one-time event where the child was informed that he or she specifically has HIV infection.18–22,33 In other cases, disclosure was deemed a gradual process that occurred over a period of time when the child was informed in stages about being infected with HIV.23,34
Figure 2. Range of reported patterns of disclosure.
Preferred Child Age and Personnel for Disclosure
Synthesis of extracted data revealed that caregivers opined that disclosure should be a gradual process, best done between the ages of 10 and 16 years.25–28 Seven out of the 9 studies that documented the person who disclosed to the child reported that parents or primary caregivers played this role.22–25,29–31 Health care providers who played a prominent role in disclosure were mentioned in the remaining 2 studies32,33 Participants in 7 other studies that did not mention who disclosed to the child endorsed parents or primary caregivers as ideal personnel to initiate and complete the disclosure process.23,25,31–35 In 2 studies, participants suggested that the presence of health care workers could potentially help the disclosure process initiated by the parents or primary caregivers.21,25
Reasons for Disclosure and Nondisclosure
Caregiver opinions on the necessity of disclosure to children were varied. Common reasons for disclosure were ART-related, pertaining to perceived improvements in adherence and initiation of ART,20–23,25,27–30,35–37 followed by fulfilling the child’s right to know.21,25,29,30,35–37 Increasing age of the child20,23,29,30,36,37 and avoidance of inadvertent partial disclosure from other sources21,36,37 were also cited as reasons for disclosure by some studies. Some caregivers felt that disclosure would help protect others20,34,36 as the knowledge of one’s HIV status may curtail risky behavior on one’s part. In some cases, disclosure was done following insistence of the involved health care professional23,36 (Table 2). Caregiver-reported reasons for nondisclosure included fear of negative psychological reactions among the children22,23,26–28,30,32,34–37 and the fear of subsequent disclosure to others, leading to stigmatization and further discrimination.22,23,25–28,30,32,35–37 Disclosure was not done in several cases when the child was perceived to be too young and immature to understand the implications of the disease.22,23,26–28,30,32,35–37 Caregiver guilt was another factor preventing disclosure to children.21,36 In 4 studies, caregivers mentioned that they did not know how best to disclose to their child30,31,35,36(Table 2). Several studies found that older age of the child correlated with disclosure.21–24,28,30,32–37 The initiation or requirement of ART, lower socioeconomic level, lower educational status of the caregiver, and the absence of the father or primary caregiver were some of the other factors that correlated with presence of disclosure (Table 3).
Table 2. Caregiver-Reported Reasons for Disclosure and Nondisclosure.
| Cited Reasons | Number of Studies (% of Studies) | References |
|---|---|---|
| Reasons for disclosure | ||
| ART initiation and presumed improved adherence | 12 (55) | 18–21,23,25–28,33–35 |
| Child’s right to know | 7 (32) | 19,23,27,28,33–35 |
| Increasing age of the child | 6 (27) | 18,21,27,28,34,35 |
| Avoidance of partial disclosure from external sources | 3 (14) | 19,34,35 |
| To prevent them from further spreading the disease/to protect others | 3 (14) | 18,32,34 |
| Current illness | 2 (9) | 20,32 |
| Insistence of health worker | 2 (9) | 21,34 |
| Parental death | 1 (4.5) | 33 |
| Reasons for nondisclosure | ||
| Negative psychological reactions | 11 (50) | 19,20,24–28,30,33–35 |
| Subsequent disclosure to others | 11 (50) | 20,21,23–26,28,30,33–35 |
| Lower age of the child | 10 (45) | 20,21,24–26,28,30,33–35 |
| Stigma/discrimination | 7 (32) | 19,20,26,28,29,32,35 |
| Lack of knowledge of correct disclosure procedure | 4 (18) | 28,29,33,34 |
| Caregiver guilt | 2 (9) | 19,34 |
Table 3. Observed Correlates* of Disclosure.
| Correlates of Disclosure | Number of Studies (% of Studies) | References |
|---|---|---|
| Older age of the child | 12 (55) | 19–22,26,28,30–35 |
| ART requirement or initiation | 4 (18) | 19,21,22,26 |
| Disclosure of caregiver HIV status | 3 (13) | 23,28,31 |
| Absent father/primary caregiver | 3 (13) | 20,21,35 |
| Lower caregiver socioeconomic status | 2 (9) | 18,20 |
| Low-educational status of caregiver/child | 2 (9) | 20,31 |
| Longer duration on ART | 1 (4.5) | 21 |
| Nonperinatal modes of acquisition | 1 (4.5) | 19 |
| Self-supervised ART intake | 1 (4.5) | 33 |
| Disclosure of child’s status to other family members | 1 (4.5) | 34 |
Correlates were derived from the individual studies based on statistical analysis and results described in each of the studies.
Impact of Disclosure
While learning about one’s own HIV status was clearly an emotional and pivotal point in a child’s life, the psychological impact of disclosure on children was less understood in most studies. A study from India noted that disclosure was met with quiet acceptance, anger, and sadness.21 Another study from the Democratic Republic of Congo reported that youth who had been disclosed to experienced a greater degree of negative rather than positive feelings after disclosure.29 However, several studies from Africa and one from Thailand reported that despite the negative emotions of grief and worry following disclosure, being aware of their HIV status translated into better adherence to ART.17,22,27,32 The caregivers also concurred that disclosing the HIV-positive status to a child was not an easy task. While some caregivers immediately felt sad and worried after disclosure,29 others felt relieved and were at ease,20 considering the eventuality of improving adherence to ART and better outcomes among their children.
Discussion
Our review of disclosure of HIV-positive status among children and adolescents in LMIC settings highlights the low rates of disclosure in these settings, even among older adolescent age groups. We found that perceived improvements in their child’s health, initiation and improved adherence to ART as well as increasing age of the child were factors that most commonly favored disclosure in LMIC settings. Factors that influenced caregivers’ decisions against disclosure included the fear of negative psychological consequences on the child, possible disclosure to others, and subsequent stigma. In resonance with previous literature in the field, we find that in LMIC settings, the preferred age range for disclosure tends to be older than that stated by caregivers in high-income settings.14,15 Tighter socioeconomic barriers, less flexible cultural norms, and lower levels of literacy compounded by massive HIV-related stigma in LMIC settings might be some of the main reasons for this observation.
High rates of partial disclosure and somewhat alarmingly, disclosure using deflected information were conspicuous findings in our review. Nine out of the 22 studies in our review addressed the issue of deflected information. The concept of “deflected” information being imparted as disclosure has not been fully explored. Literature suggests that offering limited information with the intention of attaining minimal emotional arousal in the child could be counterproductive in the long run.39 Laird et al,40 while researching information reception strategies in adolescence, suggested that in the process of masking a grave diagnosis, the provision of deflected information was often used as a concealment strategy. This possibly occurred secondary to the caregiver’s intention of protecting the child from the negative consequences, which arose from learning about their terminal diagnosis. A similar phenomenon might well be at play in the setting of HIV. The reasons for such high rates of providing deflected information in LMIC settings could be several. The sociocultural milieu, lower economic freedoms, and poor literacy levels could be contributing reasons. Guidelines and support systems for HIV disclosure need to therefore be mindful of these prevalent attributes of disclosure. An earlier review of 32 articles from LMICs suggested that disclosure should be “proactive and thoughtful” taking into account emotional vulnerability and maturity levels.15 Our review highlights the high levels of deflected information, which could subsequently lead to detrimental outcomes, particularly in aspects relating to adherence to ART and the adoption of safe sexual practices. Poor adherence is known to contribute to evolution of resistant virus and this, coupled with high-risk behavior in the adolescent age group, could potentially lead to the spread of resistant HIV strains in the community.41
In comparison with other infectious diseases and terminal diseases such as malignancies, disclosure of HIV status is more challenging. Rates and negative consequences of disclosure to children with malignancy improved as efficient treatment protocols emerged and survival rates increased.42,43 Although treatment strategies in the HIV field have similarly advanced by leaps and bounds leading to a remarkable enhancement in survival, this trend of improved perception has not been seen with HIV, largely owing to the stigma and negative moralistic values associated with the disease. Louthernoo et al44 recently showed that adolescents are still likely to have psychosocial difficulties despite combination ART enhancing survival. Further, following the initiation of the disclosure process, children with poor support systems and inadequate coping skills may fare poorly if they are not adequately prepared and if health care retention is weak.
We found that most caregivers preferred to disclose to their children as they grew older, citing better cognitive abilities. However, it is important to note that as the children mature emotionally and cognitively, their adaptation strategies are likely to vary. Younger children use behavioral coping strategies while older children are more likely to adopt cognitive strategies on receiving news of terminal illness.39 Children and adolescents living with HIV who have been disclosed to feel that disclosure helps them adapt to a “normal” life, while there may be negative emotional feelings of anger and distrust among children not disclosed to.38 In the context of disclosure of a delicate diagnosis to a child, the social cognitive theory model assumes that the course of disclosure will vary according to the child’s cognitive abilities, social experiences, and the situation they find themselves in. As the child’s cognitive capacities and social experiences expand, reactions to disclosure are expected to be easier.
Although several studies in this review reported that caregivers perceived that disclosure was necessary, not knowing how to disclose emerged as an important barrier to disclosure. An interesting pattern that further arises from this review is that a significant number of caregivers perceived the need for support from health care providers during the disclosure process. In LMIC settings, health care providers are often pivotal in helping the child understand and deal with potential consequences related to HIV disclosure. They are central figures in ensuring retention, and importantly, understanding the local cultural factors at play. This places them in a vital position to use their discretion in deciding what information suits the cognitive ability of each child during the disclosure process. The WHO and American Academy of Pediatrics also recommend that health care providers be an integral part of the incremental disclosure process.4,5 Lesch et al have described a potential conundrum; that of provider preference to leave disclosure to the family, along with caregiver’s desire to have providers more involved in the process. It should be acknowledged that health care providers are constantly surrounded by discussions and situations pertaining to HIV/AIDS and may be complacent to the emotional arousal this disease brings about when it is discussed in a patient/physician scenario, particularly in the setting of disclosure.13 However, in LMIC settings, caregivers are generally lesser educated than their counterparts in HICs, and the cultural fabric is even more complex. This perhaps propels the need for support from more “experienced” and “educated” health care providers in the context of disclosure of HIV diagnosis. The need for customized disclosure strategies in the interest of the child as well as the caregiver, with the health care provider playing an important role, is an important conclusion we drew from this review. This triangular relationship has the potential to make disclosure a more effective process. Further context-specific guidelines should consider evolving strategies to train health care providers, particularly those in direct contact with the child. A one-size-fits-all model is not a practical option given the cognitive diversity among children as well as the varying levels of education among the caregivers.
The interpretation of this review however does need to consider certain potential limitations. Due to linguistic challenges, we could include only studies that were reported in English. The heterogeneity in definitions for disclosure, disease severity, and certain demographic factors among several of the studies could also impact the overall understanding of the process. The different cultures of disclosure and the tendency toward early versus later disclosure as practiced in different field settings also have a potential to limit the conclusions that could be drawn from this review.
Conclusions
This systematic review highlights the low rate of disclosure, and the practice of deflected disclosure of HIV status to children and adolescents in low- and middle-income settings. Our synthesis also underscores the central role of the health care provider in the disclosure process. Although national agencies in different countries as well as the WHO have recognized the need for age-appropriate disclosure and have instituted guidelines facilitating the process of disclosure, these processes are not widely practiced in many high-burden settings. This review further highlights the urgent necessity to develop evidence-based recommendations that take into consideration locally prevalent cultural practices, individual family circumstances, social adjustment structures, and national realities in order to facilitate the process of disclosure of HIV status to children and adolescents in low- and middle-income settings.
Acknowledgments
The study was financially supported by the Wellcome Trust, Department of Biotechnology India Alliance Senior Fellowship (IA/S/13/2/501017) awarded to AS. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Footnotes
Disclosure: The authors declare no conflict of interest.
References
- 1.World Health Organization. Global HIV/AIDS response: Epidemic Update and Health Sector Progress Towards Universal Access. World Health Organization; 2011. [Accessed January 1, 2016]. Available at: http://www.who.int/hiv/pub/progress_report2011/en/ [Google Scholar]
- 2.Wiener L, Mellins CA, Marhefka S, et al. Disclosure of an HIV diagnosis to children: history, current research, and future directions. J Dev Behav Pediatr. 2007;28:155–166. doi: 10.1097/01.DBP.0000267570.87564.cd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.UNICEF. [Accessed January 1, 2016];Convention on the Rights of the Child. 1990 Available at: http://www.unicef.org/crc/
- 4.Disclosure of illness status to children and adolescents with HIV infection. American Academy of Pediatrics Committee on Pediatrics AIDS. Pediatrics. 1999;103:164–166. doi: 10.1542/peds.103.1.164. [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization. Guideline on HIV Disclosure Counseling for Children up to 12 Years of Age. Geneva, Switzerland: World Health Organization; [Accessed January 1, 2016]. [Internet] Available from: http://www.who.int/hiv/pub/hiv_disclosure/en/ [Google Scholar]
- 6.Slavin LA, O’Malley JE, Koocher GP, et al. Communication of the cancer diagnosis to pediatric patients: impact on long-term adjustment. Am J Psychiatry. 1982;139:179–183. doi: 10.1176/ajp.139.2.179. [DOI] [PubMed] [Google Scholar]
- 7.Hebert PC, Hoffmaster B, Glass KC, et al. Bioethics for clinicians: 7. Truth telling. CMAJ. 1997;156:225–228. [PMC free article] [PubMed] [Google Scholar]
- 8.Wiener L, Theut S, Steinberg SM, et al. The HIV-infected child: parental responses and psychosocial implications. Am J Orthopsychiatry. 1994;64:485–492. doi: 10.1037/h0079539. [DOI] [PubMed] [Google Scholar]
- 9.Naswa S, Marfatia YS. Adolescent HIV/AIDS: issues and challenges. Indian J Sex Transm Dis. 2010;31:1–10. doi: 10.4103/2589-0557.68993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kazdaglis GA, Arnaoutoglou C, Karypidis D, et al. Disclosing the truth to terminal cancer patients: a discussion of ethical and cultural issues. East Mediterr Health J. 2010;16:442–447. [PubMed] [Google Scholar]
- 11.Flanagan-Klygis E, Ross LF, Lantos J, et al. Disclosing the diagnosis of HIV in pediatrics. J Clin Ethics. 2001;12:150–157. [PubMed] [Google Scholar]
- 12.Lipson M. Disclosure of diagnosis to children with human immunodeficiency virus or acquired immunodeficiency syndrome. J Dev Behav Pediatr. 1994;15(3 suppl):S61–S65. [PubMed] [Google Scholar]
- 13.Lesch A, Swartz L, Kagee A, et al. Paediatric HIV/AIDS disclosure: towards a developmental and process-oriented approach. AIDS Care. 2007;19:811–816. doi: 10.1080/09540120601129301. [DOI] [PubMed] [Google Scholar]
- 14.Pinzon-Iregui MC, Beck-Sague CM, Malow RM. Disclosure of their HIV status to infected children: a review of the literature. J Trop Pediatr. 2013;59:84–89. doi: 10.1093/tropej/fms052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vreeman RC, Gramelspacher AM, Gisore PO, et al. Disclosure of HIV status to children in resource-limited settings: a systematic review. J Int AIDS Soc. 2013;16:18466. doi: 10.7448/IAS.16.1.18466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.World Bank. [Accessed January 1, 2016];New countries classification 2015. Available from: http://data.worldbank.org/about/country-and-lending-groups.
- 17.Bikaako-Kajura W, Luyirika E, Purcell DW, et al. Disclosure of HIV status and adherence to daily drug regimens among HIV-infected children in Uganda. AIDS Behav. 2006;10(4 suppl):S85–S93. doi: 10.1007/s10461-006-9141-3. [DOI] [PubMed] [Google Scholar]
- 18.Abadia-Barrero CE, Larusso MD. The disclosure model versus a developmental illness experience model for children and adolescents living with HIV/AIDS in Sao Paulo, Brazil. AIDS Patient Care STDS. 2006;20:36–43. doi: 10.1089/apc.2006.20.36. [DOI] [PubMed] [Google Scholar]
- 19.Arun S, Singh AK, Lodha R, et al. Disclosure of the HIV infection status in children. Indian J Pediatr. 2009;76:805–808. doi: 10.1007/s12098-009-0177-z. [DOI] [PubMed] [Google Scholar]
- 20.Vaz LM, Eng E, Maman S, et al. Telling children they have HIV: lessons learned from findings of a qualitative study in sub-Saharan Africa. AIDS Patient Care STDS. 2010;24:247–256. doi: 10.1089/apc.2009.0217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bhattacharya M, Dubey AP, Sharma M. Patterns of diagnosis disclosure and its correlates in HIV-Infected North Indian children. J Trop Pediatr. 2010;57:405–411. doi: 10.1093/tropej/fmq115. [DOI] [PubMed] [Google Scholar]
- 22.Oberdorfer P, Puthanakit T, Louthrenoo O, et al. Disclosure of HIV/AIDS diagnosis to HIV-infected children in Thailand. J Paediatr Child Health. 2006;42:283–288. doi: 10.1111/j.1440-1754.2006.00855.x. [DOI] [PubMed] [Google Scholar]
- 23.Kallem S, Renner L, Ghebremichael M, et al. Prevalence and pattern of disclosure of HIV status in HIV-infected children in Ghana. AIDS Behav. 2010;15:1121–1127. doi: 10.1007/s10461-010-9741-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Menon A, Glazebrook C, Campain N, et al. Mental health and disclosure of HIV status in Zambian adolescents with HIV infection: implications for peer-support programs. J Acquir Immune Defic Syndr. 2007;46:349–354. doi: 10.1097/QAI.0b013e3181565df0. [DOI] [PubMed] [Google Scholar]
- 25.Moodley K, Myer L, Michaels D, et al. Paediatric HIV disclosure in South Africa—caregivers’ perspectives on discussing HIV with infected children. S Afr Med J. 2006;96:201–204. [PubMed] [Google Scholar]
- 26.Boon-Yasidhi V, Kottapat U, Durier Y, et al. Diagnosis disclosure in HIV-infected Thai children. J Med Assoc Thai. 2005;88(suppl 8):S100–S105. [PubMed] [Google Scholar]
- 27.Brown BJ, Oladokun RE, Osinusi K, et al. Disclosure of HIV status to infected children in a Nigerian HIV care programme. AIDS Care. 2011;23:1053–1058. doi: 10.1080/09540121.2011.554523. [DOI] [PubMed] [Google Scholar]
- 28.Vreeman RC, Nyandiko WM, Ayaya SO, et al. The perceived impact of disclosure of pediatric HIV status on pediatric antiretroviral therapy adherence, child well-being, and social relationships in a resource-limited setting. AIDS Patient Care STDS. 2010;24:639–649. doi: 10.1089/apc.2010.0079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vaz L, Corneli A, Dulyx J, et al. The process of HIV status disclosure to HIV-positive youth in Kinshasa, Democratic Republic of the Congo. AIDS Care. 2008;20:842–852. doi: 10.1080/09540120701742276. [DOI] [PubMed] [Google Scholar]
- 30.John-Stewart GC, Wariua G, Beima-Sofie KM, et al. Prevalence, perceptions, and correlates of pediatric HIV disclosure in an HIV treatment program in Kenya. AIDS Care. 2012;25:1067–1076. doi: 10.1080/09540121.2012.749333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kouyoumdjian FG, Meyers T, Mtshizana S. Barriers to disclosure to children with HIV. J Trop Pediatr. 2005;51:285–287. doi: 10.1093/tropej/fmi014. [DOI] [PubMed] [Google Scholar]
- 32.Abebe W, Teferra S. Disclosure of diagnosis by parents and caregivers to children infected with HIV: prevalence associated factors and perceived barriers in Addis Ababa, Ethiopia. AIDS Care. 2012;24:1097–1102. doi: 10.1080/09540121.2012.656565. [DOI] [PubMed] [Google Scholar]
- 33.Biadgilign S, Deribew A, Amberbir A, et al. Factors associated with HIV/AIDS diagnostic disclosure to HIV infected children receiving HAART: a multi-center study in Addis Ababa, Ethiopia. PLoS One. 2011;6:e17572. doi: 10.1371/journal.pone.0017572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Vaz LM, Maman S, Eng E, et al. Patterns of disclosure of HIV status to infected children in a Sub-Saharan African setting. J Dev Behav Pediatr. 2011;32:307–315. doi: 10.1097/DBP.0b013e31820f7a47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mumburi LP, Hamel BC, Philemon RN, et al. Factors associated with HIV-status disclosure to HIV-infected children receiving care at Kilimanjaro christian medical centre in Moshi, Tanzania. Pan Afr Med J. 2014;18:50. doi: 10.11604/pamj.2014.18.50.2307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Atwiine B, Kiwanuka J, Musinguzi N, et al. Understanding the role of age in HIV disclosure rates and patterns for HIV-infected children in southwestern Uganda. AIDS Care. 2014;27:424–430. doi: 10.1080/09540121.2014.978735. [DOI] [PubMed] [Google Scholar]
- 37.Negese D, Addis K, Awoke A, et al. HIV-positive status disclosure and associated factors among children in North Gondar, Northwest Ethiopia. ISRN AIDS. 2012;2012:485720. doi: 10.5402/2012/485720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Vreeman RC, Scanlon ML, Mwangi A, et al. A cross-sectional study of disclosure of HIV status to children and adolescents in Western Kenya. PLoS One. 2014;9:e86616. doi: 10.1371/journal.pone.0086616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Claflin CJ, Barbarin OA. Does “telling” less protect more? Relationships among age, information disclosure, and what children with cancer see and feel. J Pediatr Psychol. 1991;16:169–191. doi: 10.1093/jpepsy/16.2.169. [DOI] [PubMed] [Google Scholar]
- 40.Laird RD, Marrero MD, Melching JA, et al. Information management strategies in early adolescence: developmental change in use and transactional associations with psychological adjustment. Dev Psychol. 2012;49:928–937. doi: 10.1037/a0028845. [DOI] [PubMed] [Google Scholar]
- 41.Bangsberg DR. Preventing HIV antiretroviral resistance through better monitoring of treatment adherence. J Infect Dis. 2008;197(suppl):S272–S278. doi: 10.1086/533415. [DOI] [PubMed] [Google Scholar]
- 42.Mitchell JL. Cross-cultural issues in the disclosure of cancer. Cancer Pract. 1998;6:153–160. doi: 10.1046/j.1523-5394.1998.006003153.x. [DOI] [PubMed] [Google Scholar]
- 43.Mystakidou K, Parpa E, Tsilila E, et al. Cancer information disclosure in different cultural contexts. Support Care Cancer. 2004;12:147–154. doi: 10.1007/s00520-003-0552-7. [DOI] [PubMed] [Google Scholar]
- 44.Louthrenoo O, Oberdorfer P, Sirisanthana V. Psychosocial functioning in adolescents with perinatal HIV infection receiving highly active antiretroviral therapy. J Int Assoc Provid AIDS Care. 2013;13:178–183. doi: 10.1177/2325957413488171. [DOI] [PubMed] [Google Scholar]