Abstract
Background
Visualization of intersegmental planes in the lung is desirable for precise anatomical lung segmentectomy. We developed the slip-knot method for creating inflation-deflation lines. This study aimed to assess relevant data for thoracoscopic segmentectomy performed using this method.
Methods
In the slip-knot method, the objective segmental bronchus is looped with a monofilament thread. One end of the thread is then pulled during temporary bilateral ventilation, causing the knot to slip toward the bronchus. Thereafter, bronchial ligation is tightened to block the outflow of segmental air, ensuring that the segment remains expanded while the other reserved segments collapse on resumption of unilateral ventilation. Data from 221 patients who underwent thoracoscopic pulmonary segmentectomy between 2010 and 2016 were analyzed.
Results
A total of 147 patients (67%) were indicated for the slip-knot method, and 74 cases (33%) were non-adaptive cases. Ninety six percent of 147 cases were well adapted to the slip-knot method, which allowed us to obtain good inflation-deflation line images to determine the intersegmental plane. The mean operative time was 171±51 min (range, 71–367 min). The mean duration of chest tube insertion was 1.5±1.2 days (range, 1–7 days). Three cases (2.0%) had prolonged air-leakage and one (0.7%) case had readmission for late air-leakage.
Conclusions
Our method enables determination of anatomical intersegmental planes using only one monofilament thread, thus facilitating thoracoscopic pulmonary anatomical segmentectomy.
Keywords: Lung cancer, segmentectomy, video-assisted thoracic surgery
Introduction
The development of computed tomography (CT) has enabled the detection of small lung cancer with a ground glass nodule (GGN), indicating noninvasive lung cancer with good prognosis (1-4). These improvements in diagnosis have allowed for greater opportunities of sublobar resection, such as anatomic segmentectomy. Pulmonary segmentectomy is still a complicated procedure, requiring the surgical resection of a small volume of lung thoracoscopically. Therefore, segmentectomy under only thoracoscopic surgery have not been widely performed (5-8). Anatomical thoracoscopic segmentectomy needs precise visualization of the inflation-deflation line and identification of the intersegmental veins between the resected segment and reserved segments, which are anatomical landmarks of the intersegmental plane (9-11).
The conventional maneuver for recognizing the intersegmental plane was used to utilize delineation between collapse of the resected segment and inflation of the reserved segment (12-14). A disadvantage of this method is the expansion of reserved segments in the spatially limited thoracic cavity during thoracoscopic surgery. Additionally, collateral ventilation at the level of the pulmonary alveolus occasionally makes the inflation-deflation line unclear following the reserved segment inflation. A Method for resected segment inflation was reported to indicate advantages securing a surgical margin from the tumor and a sufficient working space in the thorax (15). Several methods, including the jet ventilation method of insufflating air into the targeted segment, are used (9,16). However, serious risks have been reported concerning this air insufflating method (17). To address these issues, we developed the slip-knot method and have used it to successfully perform thoracoscopically anatomical segmentectomy (18,19).
The aim of this study was to describe a series of port-access thoracoscopic anatomical segmentectomies using the slip-knot method and to determine the feasibility of this method by assessing surgical and clinical results of 221 resections.
Methods
Patients
Among the 301 patients who underwent a port-access thoracoscopic anatomic segmentectomy between September 2004 and December 2016, we retrospectively analyzed data from 221 cases in which the procedure was performed after the introduction of the slip-knot method in 2010. The slip-knot method was used for 147 thoracoscopic segmentectomies. Patients enrolled in the present study gave both oral and written informed consent. Perioperative data recorded in the database were approved from the Institutional Review Board of Yamagata University.
Indication for segmentectomy
Patients who had, or were suspected of having T1aN0 non-small cell lung cancer (20), lung metastasis, or a benign lesion underwent a segmentectomy. A segmentectomy was preferred in patients who were “compromised” in that they had impaired cardiopulmonary reserve or presented other comorbidities. Lung cancer was histopathologically diagnosed based on the World Health Organization Classification (21).
Three-dimensional images were processed using preoperatively acquired CT volume data. The 3-D images were created and manipulated during surgery. Thus, we performed the operations while comparing and contrasting the simulation under real-time conditions (10,11,22). We think that perceiving the anatomical relationship between the tumor and neighboring structures is important. The 3-D CT simulation images were used to identify (I) the segmental arterial branches, (II) the intersegmental veins, and (III) the venous branches in the affected segment. In cases of malignancy, we designed resection lines with a larger surgical margin than the tumor diameter (at least 2 cm).
Preoperative simulation by 3-D CT imaging and operative procedure
The use of 3-D imaging and CT volume data for modeling enabled preoperative recognition of the anatomy and trajectory navigation during surgery (10,11,22).
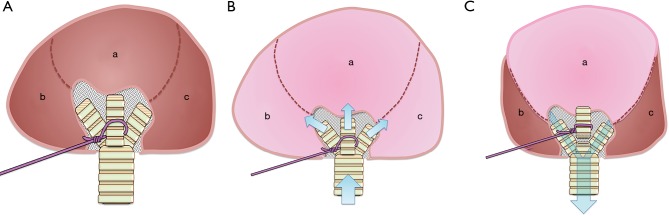
The surgical approach involves a 4-port access (one soft port of 2 or 1.5 cm in size and three of <5 mm). The hilar parenchyma was dissected along the intersegmental vein and the pulmonary artery into the affected segment was then exposed and divided. The targeted bronchus behind it was isolated and looped with a polypropylene monofilament thread. The slip-knot was made outside of the thorax and advanced by pulling the opposite side of the thread (Figure 1A). Bilateral ventilation was started with 100% oxygen (Figure 1B) (19). After lung expansion the suture was pulled, which ligated the bronchus and blocked the outflow of air from the affected segment. This ensured that the segment remained expanded while the other reserved segment collapsed on resumption of unilateral ventilation. During further hilar dissection, including targeted bronchus division with a stapler and dissection along intersegmental veins, the inflation-deflation line gradually appeared (Figure 1C). Parenchymal dissection of the hilar side was performed along the inflation-deflation line and the intersegmental pulmonary vein. Finally, staplers were used on the periphery to complete the resection.
Figure 1.
The slip-knot method for creating the inflation-deflation line. (A) The broken line divides the intersegmental line. Each segment is deflated, and the slip-knot is made with a monofilament thread looping the target bronchus; (B) the lung is ventilated and inflated preferably with pure oxygen; (C) the slip-knot is fully pulled to ligate the bronchus with expansion of the targeted segment (segment a). The affected segment (segment a) remains inflated while the other segments (segment b, c) appear collapsed. The difference between the inflated and deflated lung parenchyma forms the demarcation line. The surgeon then dissects the parenchyma along the inflation-deflation line. Each letter a, b and c indicate the pulmonary segments in each panel.
Statistical analysis
Data were analyzed using JMP software, version 13.0.1J (SAS Institute Inc., Cary NC, USA). The chi-squared test was used to compare the two groups. For continuous variables, the unpaired t test or the Wilcoxon rank-sum test was used to compare distributed variables. A P value <0.05 was considered statistically significant.
Results
Patient characteristics are listed in Table 1. Histologically, the majority of patients had a diagnosis of malignancy (208/221, 94%), with 175 patients (79%) diagnosed with lung cancer. Curative resection with free surgical margins was pathologically proven in all groups.
Table 1. Patients’ characteristics.
| Characteristics | All cases (n=221) | Case using the slip-knot | P value | |
|---|---|---|---|---|
| Yes (n=147) | No (n=74) | |||
| Male sex | 112 [51] | 69 [47] | 43 [58] | 0.117 |
| Age (years) | 66±13 [5–90] | 66±13 [10–90] | 68±14 [5–87] | 0.228 |
| Smoking history, yes | 115 [48] | 73 [50] | 42 [57] | 0.319 |
| Pack-year smoking | 43±31 [0–150] | 18±25 [0–120] | 31±38 [0–150] | 0.003 |
| FVC (%) | 102±16 [56–159] | 102±15 [56–140] | 101±19 [58–159] | 0.888 |
| FEV1% (%) | 75±11 [35–113] | 75±12 [42–113] | 73±10 [35–93] | 0.101 |
| Tumor size (cm) | 1.7±0.8 [0.3–5.4] | 1.6±0.7 [0.3–4.5] | 1.9±0.9 [0.5–5.4] | 0.002 |
| Clinical diagnosis | 0.115 | |||
| Lung cancer | 175 [79] | 120 [82] | 55 [74] | |
| Metastatic tumor | 29 [13] | 20 [13] | 9 [12] | |
| Lymphoma | 4 [2] | 1 [1] | 3 [4] | |
| Benign | 13 [6] | 6 [4] | 7 [10] | |
Data are shown as mean ± SD [range] or number [percentage].
Regarding utilization of the slip-knot method, 147 cases (67%) were indicated for the slip-knot method, and 74 cases (33%) were non-adaptive cases. The reasons for non-adaptation were as follows: 35 cases with apparently sufficient surgical margin as the resected segment was large enough (superior, basal, left upper division, lingular division), 21 cases with palpable or visible tumor capable to accomplish segmentectomy with only guidance of the intersegmental pulmonary vein, 5 cases resected by the conventional preserved segment inflation method with apparently sufficient surgical margin, 4 cases with severe emphysema and apparently sufficient surgical margin, etc.
In the 96% of the 147 cases that were well adapted to the slip-knot method, we obtained a good inflation-deflation line image determining the intersegmental plane (Table 2), which enabled intersegmental dissection by applying electrocautery, an energy device, or a staple along this demarcated line. Reasons for poor visualized cases were as follows: emphysematous change and airway obstruction in two cases, or severe pleural adhesion and difficulty for one-lung ventilation in one case.
Table 2. Visualization of the intersegmental plane using the slip-knot method.
| Variables | Number |
|---|---|
| Visualization of the intersegmental plane, n [%] | |
| Good | 141 [96] |
| Poor | 6 [4] |
| Reasons for poor cases* | |
| Emphysematous change | 2 |
| Airway obstruction for sputum | 2 |
| Severe pleural adhesion | 1 |
| Difficulty for one-lung ventilation | 1 |
| Time for the slip knot method** (min), median (range) | |
| Time for bilateral ventilation | 2.7 (1.0–5.0) |
| Time for visualizing inflation-deflation line | 10.6 (7.5–17.7) |
| Total | 13.0 (9.0–20.8) |
*, cases for poor visualization (n=6); **, cases available for time (n=17).
The time required to perform the slip-knot method was divided into two phases (i.e., the time required for bilateral ventilation and the time spent until the inflation-deflation line could be visualized). We performed a pilot study for 17 cases. The median time for bilateral ventilation and visualization of the inflation-deflation line was 2.7 and 10.6 minutes, respectively. During the latter phase, we were able to dissect the hilar parenchyma along the intersegmental vein and divide the intrasegmental vein without difficulty.
Surgical results are shown in Table 3. In cases using the slip-knot method, the mean operative time was 171 min and the mean duration of chest tube insertion was 1.5 days. Three cases (2.0%) had prolonged air-leakage and one (0.7%) had readmission for late air-leakage. A comparison of the cases with or without the slip-knot method showed that the chest tube duration and hospital stay were shorter in cases using this method than in non-used cases (0.027 and 0.004, respectively).
Table 3. Surgical results.
| Characteristics | All cases (n=221) | Case using the slip-knot method | P value | |
|---|---|---|---|---|
| Yes (n=147) | No (n=74) | |||
| Operative time (min) | 173±54 [30–370] | 171±51 [71–367] | 175±60 [30–370] | 0.592 |
| Chest tube duration (day) | 1.7±1.6 [1–15] | 1.5±1.2 [1–7] | 2.0±2.1 [1–15] | 0.027 |
| Hospital stay (day) | 6.5±2.7 [2–18] | 6.1±2.4 [3–16] | 7.3±3.1 [2–18] | 0.004 |
| Complication | 0.152 | |||
| Prolonged air leakage | 5 (2.3) | 3 (2.0) | 2 (2.7) | |
| Pneumothorax after discharge | 1 (0.5) | 1 (0.7) | 0 | |
| Pneumonia | 1 (0.5) | 0 | 1 (1.4) | |
| Hemothorax | 1 (0.5) | 0 | 1 (1.4) | |
| Morbidity | 0 | 0 | 0 | |
| Mortality | 0 | 0 | 0 | |
Data are shown as mean ± SD [range] or number (percentage).
The conversion to an open approach caused by surgical technique was not observed in this group and all lesions were detected in the resected pulmonary segment. The success rate of thoracoscopic anatomic segmentectomy using the slip-knot method was 100%.
Discussion
Anatomical thoracoscopic pulmonary segmentectomy is an abstruse procedure because the intersegmental demarcated line on the lung cannot be found on thoracoscopy. Furthermore, in cases involving pulmonary malignancies, a sufficient surgical margin from the tumor is essential (23-25). The resected segment inflation method is reported to yield a sufficient surgical margin from the tumor by inflation of the affected segment (15). Several methods for resected segment inflation have been introduced, including the selective inflating segment method using high-frequency jet ventilation (9) and the air insufflation method using a butterfly needle (16). The butterfly needle method can cause an air embolism in the vessels adjacent the bronchus (17,26). Therefore, we devised the slip-knot method to visualize the intersegmental demarcation line during thoracoscopic segmentectomy in 2010 (18). The slip-knot bronchial ligation method shortened the mean operative time from 210 to 164 min between 2004 and 2012 (18). However, the rate of visualization of the parenchymal intersegmental demarcation line was not mentioned. In this study, 141 (96%) of 147 patients had good visualization of the inflation-deflation line on the lung, which enabled intersegmental dissection using various devices along the parenchymal demarcated border. Regarding the median time required for the slip-knot method, the method requires 2.7 min for bilateral ventilation plus approximately 10.6 min to visualize the intersegmental plane. During bilateral ventilation, we again checked the CT images to confirm the running of the intersegmental and intrasegmental veins. On resumption of unilateral ventilation, we began the hilar dissection in the bronchial division, parenchymal dissection along the intersegmental veins, etc. Subsequently, we proceeded to dissect along the inflation-deflation line. Bilateral ventilation using pure oxygen might facilitate rapid deflation of the preserving segments (27).
The inflation-deflation line is not easily visualized in patients with impaired lung function, such as those with chronic emphysema or chronic bronchitis with narrow airway retaining sputum. In patients with chronic bronchitis, making inflation-deflation lines is burdensome because sending airflow is hard to pass through the bronchus of the pulmonary segment. Severe emphysematous lung includes problems with air trapping, inducing failure to collapse of the lung, and an unclear demarcation line owing to peripheral pulmonary disruption. Therefore, patients in the poorly visualized group often underwent the use of staplers to divide the intersegmental plane to preventing air leakage.
In our series of surgeries, the resected bronchi were often ligated at the level of the subsegmental region. Thus, the slip-knot bronchial ligation method is adaptable to bronchus of small caliber to perform anatomical subsegmentectomies. In our experience, visualizing the boundary between subsegments was easier and required less time for visualization after inducing the slip-knot method. The frequency of subsegmentectomies therefore became higher than it was before using the slip-knot method (28,29).
Other methods for recognizing the intersegmental plane are reported, including a method of transbronchial infusion of indocyanine green (ICG) into the pulmonary segment for dissection (30,31) and intravenous injection of ICG after segmental artery cutting to identify the difference of blood flow between the intersegmental plane using an infrared imaging thoracoscopic device (32). ICG infused transbronchially might not spread uniformly in the segmental parenchyma. Although this method using ICG injected via a vein might be promising, the cost of the procedure may be high and an invisible demarcation line made by the dye quickly vanishes.
Segmentectomy using the slip-knot method is possible if the segmental bronchi to resect can be exposed. Once the inflation-deflation lines become visible, its demarcation line does not disappear. Additionally, the advantage of this method is that it does not necessitate costly equipment such as the jet ventilation or infrared thoracoscopic system. This method also does not require anesthesiologists with bronchoscopic skills. Therefore, the surgeon can make the intersegmental plane in the surgical field at that time. The application of this method is expected to allow segmentectomy to be performed with minimal cost, comparable to the cost of a single monofilament thread.
One limitation of our study is that it is a single-center, retrospective study. These results can be difficult to apply to more complicated perioperative condition. There are also biases related to learning curves and newly developed devices and instruments.
In conclusion, our study shows that determination of the intersegmental plane using the slip-knot method enables anatomical precision to dissect the pulmonary segment for thoracoscopic segmentectomy. This method is simple and easily to employ that allows oncologically safe resection, especially for small lung tumors that are not visible or palpable.
Acknowledgements
None.
Ethical Statement: The study was approved by the ethics committee of Yamagata University Faculty of Medicine (No. 483) and the need for written informed consent from each patient was waived.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Okada M, Nishio W, Sakamoto T, et al. Correlation between computed tomographic findings, bronchioloalveolar carcinoma component, and biologic behavior of small-sized lung adenocarcinomas. J Thorac Cardiovasc Surg 2004;127:857-61. 10.1016/j.jtcvs.2003.08.048 [DOI] [PubMed] [Google Scholar]
- 2.Nakata M, Sawada S, Yamashita M, et al. Objective radiologic analysis of ground-glass opacity aimed at curative limited resection for small peripheral non-small cell lung cancer. J Thorac Cardiovasc Surg 2005;129:1226-31. 10.1016/j.jtcvs.2004.10.032 [DOI] [PubMed] [Google Scholar]
- 3.Kodama K, Higashiyama M, Okami J, et al. Oncologic outcomes of segmentectomy versus lobectomy for clinical T1a N0 M0 non-small cell lung cancer. Ann Thorac Surg 2016;101:504-11. 10.1016/j.athoracsur.2015.08.063 [DOI] [PubMed] [Google Scholar]
- 4.Sagawa M, Oizumi H, Suzuki H, et al. A prospective 5-year follow-up study after limited resection for lung cancer with ground-glass opacity. Eur J Cardiothorac Surg 2018;53:849-56. 10.1093/ejcts/ezx418 [DOI] [PubMed] [Google Scholar]
- 5.Shiraishi T, Shirakusa T, Iwasaki A, et al. Video-assisted thoracoscopic surgery (VATS) segmentectomy for small peripheral lung cancer tumors: intermediate results. Surg Endosc 2004;18:1657-62. [DOI] [PubMed] [Google Scholar]
- 6.Atkins BZ, Harpole DH, Jr, Mangum JH, et al. Pulmonary segmentectomy by thoracotomy or thoracoscopy: reduced hospital length of stay with a minimally-invasive approach. Ann Thorac Surg. 2007;84:1107-12. 10.1016/j.athoracsur.2007.05.013 [DOI] [PubMed] [Google Scholar]
- 7.Oizumi H, Kanauchi N, Kato H, et al. Total thoracoscopic pulmonary segmentectomy. Eur J Cardiothorac Surg 2009;36:374-7. 10.1016/j.ejcts.2009.03.038 [DOI] [PubMed] [Google Scholar]
- 8.Ghaly G, Kamel M, Nasar A, et al. Video-assisted thoracoscopic surgery is a safe and effective alternative to thoracotomy for anatomic segmentectomy in patients with clinical stage I non-small cell lung cancer. Ann Thorac Surg 2016;101:465-72. 10.1016/j.athoracsur.2015.06.112 [DOI] [PubMed] [Google Scholar]
- 9.Okada M, Mimura T, Ikegaki J, et al. A novel video-assisted anatomic segmentectomy technique: selective segmental inflation via bronchofiberoptic jet followed by cautery cutting. J Thorac Cardiovasc Surg 2007;133:753-8. 10.1016/j.jtcvs.2006.11.005 [DOI] [PubMed] [Google Scholar]
- 10.Oizumi H, Endoh M, Takeda S, et al. Anatomic lung segmentectomy simulated by computed tomographic angiography. Ann Thorac Surg. 2010;90:1382-3. 10.1016/j.athoracsur.2009.11.062 [DOI] [PubMed] [Google Scholar]
- 11.Oizumi H, Kanauchi N, Kato H, et al. Anatomic thoracoscopic pulmonary segmentectomy under 3-dimensional multidetector computed tomography simulation: a report of 52 consecutive cases. J Thorac Cardiovasc Surg 2011;141:678-82. 10.1016/j.jtcvs.2010.08.027 [DOI] [PubMed] [Google Scholar]
- 12.Blades B. Conservation of lung tissue by partial lobectomy. Ann Surg 1943;118:353-65. 10.1097/00000658-194309000-00003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Overholt RH, Woods FM, Betts RH. An improved method of resection of pulmonary segments: report of a technique applied in 70 operations. J Thorac Surg 1948;17:464-79. [PubMed] [Google Scholar]
- 14.Rubenstein LH, O'Neill TJ, Glover RP. A technique for pulmonary segmental delineation. J Thorac Surg 1949;18:75-81. [PubMed] [Google Scholar]
- 15.Tsubota N, Ayabe K, Doi O, et al. Ongoing prospective study of segmentectomy for small lung tumors. Ann Thorac Surg 1998;66:1787-90. 10.1016/S0003-4975(98)00819-4 [DOI] [PubMed] [Google Scholar]
- 16.Kamiyoshihara M, Kakegawa S, Morishita Y. Convenient and improved method to distinguish the intersegmental plane in pulmonary segmentectomy using a butterfly needle. Ann Thorac Surg 2007;83:1913-4. 10.1016/j.athoracsur.2006.06.052 [DOI] [PubMed] [Google Scholar]
- 17.Otsuka T, Nakamura Y, Harada A, et al. Extremely rare but potential complication of diffuse brain edema due to air embolism during lung segmentectomy with selected segmental inflation technique by syringe needle during video-assisted thoracoscopic surgery. J Thorac Cardiovasc Surg 2011;142:e151-2. 10.1016/j.jtcvs.2011.07.061 [DOI] [PubMed] [Google Scholar]
- 18.Oizumi H, Kato H, Endoh M, et al. Slip knot bronchial ligation method for thoracoscopic lung segmentectomy. Ann Thorac Surg 2014;97:1456-8. 10.1016/j.athoracsur.2013.07.125 [DOI] [PubMed] [Google Scholar]
- 19.Endoh M, Oizumi H, Kato H, et al. How to demarcate intersegmental plane with resected- segments inflation method using the slip knot technique in thoracoscopic anatomic segmentectomy. J Vis Surg 2017;3:100. 10.21037/jovs.2017.06.11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kodama K, Doi O, Higashiyama M, et al. Intentional limited resection for selected patients with T1 N0 M0 non-small-cell lung cancer: a single institution study. J Thorac Cardiovasc Surg 1997;114:347-53. 10.1016/S0022-5223(97)70179-X [DOI] [PubMed] [Google Scholar]
- 21.Travis WD, Brambilla E, Muller-Hermelink HK, et al. Pathology and Genetics. Tumours of the Lung, Pleura, Thymus and Heart. Lyon, France: IARC Press, 2004. [Google Scholar]
- 22.Chan EG, Landreneau JR, Schuchert MJ, et al. Preoperative (3-dimensional) computed tomography lung reconstruction before anatomic segmentectomy or lobectomy for stage I non–small cell lung cancer. J Thorac Cardiovasc Surg 2015;150:523-8. 10.1016/j.jtcvs.2015.06.051 [DOI] [PubMed] [Google Scholar]
- 23.Sawabata N, Ohta M, Matsumura A, et al. Optimal distance of malignant negative margin in excision of nonsmall cell lung cancer: a multicenter prospective study. Ann Thorac Surg 2004;77:415-20. 10.1016/S0003-4975(03)01511-X [DOI] [PubMed] [Google Scholar]
- 24.Nishio W, Yoshimura M, Maniwa Y, et al. Re-Assessment of Intentional Extended Segmentectomy for Clinical T1aN0 Non-Small Cell Lung Cancer. Ann Thorac Surg 2016;102:1702-10. 10.1016/j.athoracsur.2016.05.071 [DOI] [PubMed] [Google Scholar]
- 25.Shiono S, Okumura T, Boku N, et al. Outcomes of segmentectomy and wedge resection for pulmonary metastases from colorectal cancer. Eur J Cardiothorac Surg 2017;51:504-10. [DOI] [PubMed] [Google Scholar]
- 26.Li NL, Lin CS, Shih CH, et al. Intraoperative cardiac arrest caused by air embolism during video-assisted thoracoscopic segmentectomy. J Thorac Cardiovasc Surg 2018;155:e111-3. 10.1016/j.jtcvs.2017.11.015 [DOI] [PubMed] [Google Scholar]
- 27.Iwata H, Shirahashi K, Mizuno Y, et al. Surgical technique of lung segmental resection with two intersegmental planes. Interact Cardiovasc Thorac Surg 2013;16:423-5. 10.1093/icvts/ivs560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kato H, Oizumi H, Inoue T, et al. Port-access thoracoscopic anatomical lung subsegmentectomy. Interact Cardiovasc Thorac Surg 2013;16:824-9. 10.1093/icvts/ivt037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Endoh M, Oizumi H, Kato H, et al. Posterior approach to thoracoscopic pulmonary segmentectomy of the dorsal basal segment: A single-institute retrospective review. J Thorac Cardiovasc Surg 2017;154:1432-9. 10.1016/j.jtcvs.2017.03.120 [DOI] [PubMed] [Google Scholar]
- 30.Sekine Y, Ko E, Oishi H, et al. A simple and effective technique for identification of intersegmental planes by infrared thoracoscopy after transbronchial injection of indocyanine green. J Thorac Cardiovasc Surg 2012;143:1330-5. 10.1016/j.jtcvs.2012.01.079 [DOI] [PubMed] [Google Scholar]
- 31.Oh S, Suzuki K, Miyasaka Y, et al. New technique for lung segmentectomy using indocyanine green injection Ann Thorac Surg 2013;95:2188-90. 10.1016/j.athoracsur.2012.12.068 [DOI] [PubMed] [Google Scholar]
- 32.Misaki N, Chang SS, Igai H, et al. New clinically applicable method for visualizing adjacent lung segments using an infrared thoracoscopy system. J Thorac Cardiovasc Surg 2010;140:752-6. 10.1016/j.jtcvs.2010.07.020 [DOI] [PubMed] [Google Scholar]