Abstract
Background
Thoracic surgery is currently the optimal treatment for non-small cell lung cancer (NSCLC). However, it may be responsible for numerous postoperative complications and is often used in patients with multi co morbidities. In recent years, the optimization of a patient’s physical capacity before surgery has been the subject of several studies. The objective of this study was to determine whether participation in a prehabilitation program would improve outcomes after surgery and lower morbidity according to the Clavien-Dindo classification.
Methods
This retrospective cohort study was performed between 1st January 2014 and 31st January 2016 at Rouen University Hospital. All adult patients with NSCLC (IIIa or <) who had pulmonary lobectomy by minimally invasive surgery and cardiopulmonary exercise testing [CPET (VO2max ≤20 mL/min/kg)] were included.
Results
The cohort included 38 patients. Two groups were formed: one group with prehabilitation (n=19) and one group without prehabilitation (n=19). Four patients were not included leaving 34 patients for the final analysis. Most patients with a Clavien-Dindo grade of ≤2 had received prehabilitation compared to patients who had not received prehabilitation, respectively 17/19 vs. 8/15; P=0.0252. Patients who had received prehabilitation had fewer postoperative complications than patients who had not received prehabilitation, respectively 8/19 vs. 12/15; P=0.0382.
Conclusions
We have shown that prehabilitation has a positive impact on the occurrence and severity of postoperative complications after pulmonary lobectomy by minimally invasive surgery. Further studies conducted in larger populations are warranted to confirm these results.
Keywords: Rehabilitation, thoracic surgery, physiotherapy, postoperative complications
Introduction
While lung cancer is only 4th among tumors, it has the worst prognosis with nearly 1.69 million deaths each year (1). For patients with non-small cell lung cancer (NSCLC), surgery allows 40% survival at 5 years compared with 17% in its absence (2). However, in subjects with an operable lesion, the question of surgical tolerance is raised. Major lung resection is associated with an incidence of postoperative complications of 13% to 28% and mortality varying between 3% and 6% (3). The risk of complications increases 6-fold in those using tobacco (4). Moreover, operated patients often present numerous comorbidities, as respiratory, vascular and/or cardiac disorders. In this context, the prehabilitation of a patient before surgery including the optimization of a patient’s physical capacities has become meaningful. It is known that parameters such as VO2max or FEV1 are predictive of postoperative complications and are improved by aerobic training (5-7). In recent years, numerous studies have investigated the relevance of pulmonary rehabilitation, mostly in patients with Chronic Obstructive Pulmonary Disease (COPD), and subsequent improvement in quality of life, decreased dyspnea and lower risk of hospitalization (8). To a lesser extent, work is being carried out on the value of a prehabilitation program in preparation for pulmonary surgery with a view to improving physical fitness and limiting postoperative respiratory disability (9). The review published by Nagarajan et al. concluded that prehabilitation (PR) for pulmonary surgery improved exercise functional capacity and limited postoperative lung capacity reduction (10). However, conclusions concerning the impact on morbidity and mortality were uncertain, justifying the conduct of controlled studies. A recent meta-analysis reported a decrease in complications, especially respiratory (11). However, this decrease was diverse. Currently, there are no published data on the severity of postoperative complications after pulmonary lobectomy in patients with or without respiratory prehabilitation before surgery. The objective of this study was to determine whether participation in a prehabilitation program would improve outcomes after surgery and lead to lower morbidity according to the Clavien-Dindo classification. Secondary objectives were the impact of prehabilitation on the number of postoperative complications and whether it allowed a reduction in the length of hospital stay (LOS).
Methods
This was a retrospective cohort study carried out at Rouen University Hospital, France between January 1st, 2014 and January 31st, 2016. We analyzed the clinical and surgical data of all patients who had cardiopulmonary exercise testing (CPET), as part of their preoperative evaluation for pulmonary lobectomy.
We also collected the following information: presence of COPD, presence of peripheral arterial obstructive disease (PAOD), values of forced expiratory volume in one second (FEV1) using pulmonary function test, and Tiffeneau-Pinelli index. A follow-up visit was performed at day 30 after surgery. All procedures performed in this study were in accordance with the ethical standards of the institutional and national research committee (E2017-32).
Eligibility
Inclusion criteria were patients aged ≥18 years old with NSCLC, which was operable, staged I to IIIa, and with VO2max ≤20 mL/min/kg on CPET, according to the recommendations of the ERS (12). Exclusion criteria were missing or incomplete medical records, preoperative death, non-surgical treatment, thoracotomy conversion or resection other than lobectomy.
Preoperative assessment
Preoperative assessment including CPET was performed to determine whether patients were operable (12). CPET was performed according to guidelines on an electromagnetic cycle ergometer with an incremental protocol (13). Following a 3-minute warm-up period, incremental ramp exercise (5–20 W/min) was maintained until exhaustion. A face mask, pneumotach, and gas analyzer were used to measure oxygen consumption (VO2) and carbon dioxide production (VCO2) breath by breath. Ventilatory threshold was manually determined.
After CPET, patients were either operated directly (non prehabilitation group or NPR) or were prehabilitated (PR group) and then operated. Respiratory prehabilitation was carried out by two physiotherapists specialized in this practice
Prehabilitation program
The prehabilitation program consisted of exercise re-training, muscular strengthening of the lower and upper limbs, therapeutic education and help with smoking cessation. It was organized in 3 to 5 sessions per week, until the operating date. Each session lasted about 90 minutes. Each session included a 45 minutes endurance activity, performed on a cycle ergometer and tailored to the ventilatory threshold (VT1) of each participant. It was performed in continuous training or interval training (14) with a possible gradual increment of workload. Prehabilitation also included muscular strengthening on the cycle ergometer at the rate of 3×12 movements at 70% of the 1RM (15), equivalent to the maximum load achievable once for the given movement. In addition, an incremental reinforcement of the inspiratory muscles by resistive valve (Threshold IMT, Respironics) was systematically performed at 30% maximum inspiratory pressure (MIP).
There is no evidence that any one component of the training schedule results in the benefits observed (16). The optimal preoperative exercise schedule remains unknown. A combination of strength exercises and endurance exercise seems more complete and allows a significant improvement in strength, dyspnoea and quality of life compared to these two parameters performed in isolation (17). A combination of these two techniques is also advised in international recommendations (14,16).
Surgery by video assisted thoracic surgery (VATS) or robotic assisted thoracic surgery (RATS)
Pulmonary lobectomy was performed by minimally invasive surgery using either VATS or RATS. Minimally invasive surgery limits the functional and painful impact of surgery and promotes early recovery (18).
Postoperative events
The primary endpoint was to investigate the severity of complications according to Clavien-Dindo classification (19). Potential complications included: acute respiratory failure, atelectasis, bronchospasm, pulmonary embolism, acute edema of the lung, rhythm disorder, myocardial infarction/angina, stroke, bronchopulmonary fistula, prolonged air leak, pneumonia, postoperative hemorrhage, pneumothorax, emphysema, infection of the thoracic lining (20). For each complication, we recorded the functional outcome as well as the treatment provided in order to grade morbidity. The same complication may have a different grade depending on the treatment used. Regarding secondary objectives, we recorded the LOS corresponding to the delay between hospital admission the day before surgery and hospital discharge after surgery. We also recorded postoperative complications occurring between the day of surgery and the follow-up visit at day 30.
Statistical analysis
Patient’s characteristics were described by frequencies and percentages for categorical parameters and as medians and 25th–75th percentiles for continuous parameters. Patient’s baseline characteristics were compared between groups (PR/NPR group) using the Wilcoxon-Mann-Whitney test for at least ordinal variables and Fisher’s exact test, as appropriate, for categorical variables.
No multivariable analysis was carried out because the univariable comparisons of both groups did not provide any evidence that they differed before the end of surgery.
As this study was exploratory, no correction for multiple testing was carried out, and a P value less than 0.05 was considered to be statistically significant.
Results
Demographics and clinical data
The cohort included 38 patients, 3 of whom received non-surgical treatment and one of whom had a thoracoscopy, which was converted to thoracotomy (Figure 1). Finally, 34 patients were completely followed up and analyzed. Two groups were formed: one group with prehabilitation (n=19) and one group without prehabilitation (n=15). Patients were followed from the date of the preoperative CPET to the postoperative visit at day 30.
Figure 1.
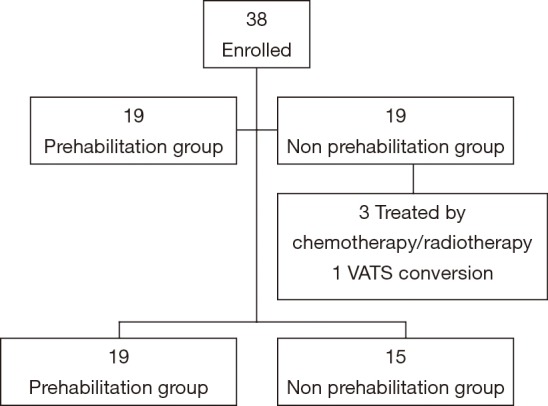
Flow chart. VATS, video assisted thoracic surgery.
The median age of patients at the time of surgery was 66 [58–72] years. Men accounted for 73% of the cohort (n=25). The presence of COPD-type comorbidities, hypertension, hypercholesterolemia, lower limb arterial disease and diabetes was observed in both groups. The median BMI was 25.9 [23.4–30]. The median VO2max was 15.4 [13.8–17.1] mL/min/kg. There was no baseline difference between the two groups (Table 1).
Table 1. Patients’ characteristics according to prehabilitation group.
| Variable | All | No | Yes | P value |
|---|---|---|---|---|
| Patients (n)a | 34 | 15 | 19 | |
| Age (years)b | 66 [58–72] | 69 [56–73] | 65 [59–71] | 0.6143 |
| Gender (n)a | 0.4620 | |||
| Male | 25 (73.5%) | 10 (66.6%) | 15 (78.9%) | |
| Female | 9 (26.4%) | 5 (33.4%) | 4 (21.1%) | |
| Tobacco (n)a | 33 (97%) | 15 (100%) | 18 (95%) | |
| Pack-years (n)b | 40 [30–52] | 40 [30–52] | 43 [30–56] | 0.7304 |
| BMI (kg/m2) b | 25.9 [23.4–30] | 25.0 [22.5–30] | 26.6 [23.7–30.4] | 0.8351 |
| COPD (n)a | 0.7379 | |||
| No | 15 | 6 (40%) | 9 (47.3%) | |
| Yes | 19 | 9 (60%) | 10 (52.7%) | |
| High blood pressure (n)a | 0.4888 | |||
| No | 15 | 8 (53.3%) | 7 (36.8%) | |
| Yes | 19 | 7 (46.7%) | 12 (63.2%) | |
| PAOD (n)a | 1 | |||
| No | 27 | 12 (80%) | 15 (78.9%) | |
| Yes | 7 | 3 (20%) | 4 (21.1%) | |
| Hypercholesterolemia (n)a | 1 | |||
| No | 29 | 13 (86.7%) | 16 (84.2%) | |
| Yes | 5 | 2 (13.3) | 3 (15.8%) | |
| Diabetes (n)a | 1 | |||
| No | 27 | 12 (80%) | 15 (78.9%) | |
| Yes | 7 | 3 (20%) | 4 (21.1%) | |
| VO2max (mL/min/kg)b | 15.4 [13.8–17.1] | 15.8 [14.6–18.4] | 14.8 [13.2–16.5] | 0.1313 |
| FEV1 (%)b | 61 [58–67] | 61 [58–71] | 61 [54–67] | 0.9307 |
| FEV1/FVC (%)b | 66 [59–70] | 66 [59–70] | 67 [59–71] | 0.9584 |
| Anesthesia score risk (n)a | 0.1319 | |||
| 2 | 7 (20.6%) | 3 (20%) | 4 (21.1%) | |
| 3 | 26 (76.5%) | 11 (73.3%) | 15 (78.9%) | |
| 4 | 1 (2.9%) | 1 (6.7%) | – |
a, data expressed as n or n (%); b, data expressed as median (Q1–Q3); BMI, body mass index; COPD, chronic obstructive pulmonary disease; PAOD, peripheral arterial obstructive disease; FEV1, forced expiratory volume in one second; FEV1/FVC, Tiffeneau-Pinelli index.
Parameters of prehabilitation and surgery
The median number of prehabilitation sessions was 17 [14–20]. The median number of days between CPET and surgery was 44 [29–46]. There was no significant difference between the two groups (Table 2). Patients were predominantly operated by VATS (n=28).
Table 2. Parameters of prehabilitation and surgery.
| Variables | All | No | Yes | P value |
|---|---|---|---|---|
| Patients | 19 | 0 | 19 | |
| Prehabilitation sessionsa | – | – | 17 [14–20] | |
| Days between end of prehabilitation and surgerya | – | – | 6 [4–21] | |
| Patients | 34 | 15 | 19 | 0.5098 |
| Days between CPET and surgerya | 44 [29–76] | 37 [23–76] | 52 [30–76] | |
| Lobectomy | 0.9597 | |||
| RLL | 7 | 3 | 4 | |
| LLL | 5 | 2 | 3 | |
| RUL | 11 | 6 | 5 | |
| LUL | 11 | 4 | 7 | |
| VATS or RATS resection | 0.6722 | |||
| VATS | 28 | 13 | 15 | |
| RATS | 6 | 2 | 4 |
Data expressed as n; a, data expressed as median (Q1–Q3). RUL, right upper lobectomy; RLL, right lower lobectomy; LUL, left upper lobectomy; LLL, left lower lobectomy; VATS, video assisted thoracic surgery; RATS, robotic assisted thoracic surgery; CPET, cardiopulmonary exercise testing.
Effect of prehabilitation on the severity of postoperative complications
The majority of patients with a Clavien-Dindo grade of 2 or less had received prehabilitation compared to patients who had not received prehabilitation, respectively 17/19 vs. 8/15; with a statistically significant difference in favor of the prehabilitation group (P=0.0252) (Table 3).
Table 3. Hospital stay and post-operative complications according to prehabilitation group.
| Variables | All | No | Yes | P value |
|---|---|---|---|---|
| Patients | 34 | 15 | 19 | |
| Length of stay (days)a | 6 [5–8] | 7 [5–8] | 5 [4–8] | 0.0838 |
| Occurrence of complications | 0.0382 | |||
| No | 14 | 3 | 11 | |
| Yes | 20 | 12 | 8 | |
| Among complications | ||||
| Atelectasis | 6 | 3 | 3 | |
| Empyema | 5 | 5 | – | |
| Pneumonia | 5 | 5 | – | |
| Acute respiratory disease | 4 | 2 | 2 | |
| Number of complications | 0.0030 | |||
| 0 | 14 | 3 | 11 | |
| 1 | 13 | 5 | 8 | |
| 2 | 6 | 6 | – | |
| 3 | 1 | 1 | – | |
| Clavien-Dindo classification | 0.0291 | |||
| 0 | 14 | 3 | 11 | |
| I | 7 | 3 | 4 | |
| II | 4 | 2 | 2 | |
| IIIa | 5 | 5 | – | |
| IIIb | 1 | – | 1 | |
| IV | 3 | 2 | 1 | |
| Clavien-Dindo classification ≤2 | 0.0252 | |||
| Yes | 25 | 8 | 17 | |
| No | 9 | 7 | 2 |
Data expressed as n; a data expressed as median (Q1–Q3).
Relationship between prehabilitation and number of postoperative complications
We also observed that the absence of postoperative complications was predominant in the prehabilitation group (11/19 vs. 3/15, P=0.0382).
Regarding the number of postoperative complications, patients who had received prehabilitation had fewer complications than patients who had not received prehabilitation, respectively 0-1 vs. 0-3 (Table 3).
Effect of prehabilitation on LOS
A median duration of hospitalization of 5 [4–8] days was observed in patients who had received prehabilitation compared with 7 [5–8] days in patients who had not received prehabilitation. The difference observed was not statistically significant (P=0.083).
Optimal number of prehabilitation sessions
Within the prehabilitation group, we compared two sub groups: patients who had more than 17 prehabilitation sessions (n=10) and patients who had fewer than 17 sessions (n=9).
There were no significant differences between these two sub groups in terms of length of stay (P=0.644), and severity of complications (P=0.4737) (Table 4).
Table 4. Hospital stay and complications by number of prehabilitation sessions.
| Variable | Prehabilitation with more than 17 sessions | P value | |
|---|---|---|---|
| No | Yes | ||
| Number of patients | 9 | 10 | |
| Length of stay (days)a | 5 [5–6] | 5 [4–8] | 0.644 |
| Number of complications | 1 | ||
| 0 | – | – | |
| 1 | 5 | 6 | |
| 2 | 4 | 4 | |
| 3 | – | – | |
| Clavien Dindo scale | 0.7771 | ||
| 0 | 5 | 6 | |
| I | 3 | 1 | |
| II | 1 | 1 | |
| IIIa | – | – | |
| IIIb | – | 1 | |
| IV | – | 1 | |
| Clavien-Dindo >2 | 0.4737 | ||
| No | 9 | 8 | |
| Yes | – | 2 | |
Data expressed as n; a data expressed as median (Q1–Q3).
Discussion
In this study, we have shown that prehabilitation has an impact on the occurrence and severity of postoperative complications after pulmonary lobectomy by minimally invasive surgery. Furthermore, our results support the positive effect of prehabilitation on postoperative morbidity and mortality, in agreement with other works (11,21).
We found a median difference of two days in LOS between groups, but this was not statistically significant. Our results are not in line with those of previous studies which reported a correlation between prehabilitation and LOS (22,23). This may be related to the small size of our sample. Compared to other studies which included mostly invasive thoracotomy surgeries, the patients in our study benefited from minimally invasive surgery which may already be a contributing factor to reduced LOS and possibly reduced cost of hospitalization.
The originality of our study was its focus on the severity of postoperative complications and functional outcomes on patients. Indeed, a single severe complication requiring a stay in intensive care unit or surgical recovery will be more deleterious for the patient than the addition of two complications requiring analgesic, antiemetic or respiratory physiotherapy treatment. We are not aware of any other study associating prehabilitation and severity of complications, according to the Clavien-Dindo classification. Moreover, the vast majority of prehabilitation studies performed to date included populations with COPD preparing for pulmonary resection surgery (24-27), a context which is not relevant to all patients at operative risk (12). Only two studies included populations of all thoracic surgery patients without an underlying chronic disease criterion and authors concluded an increase in VO2max (28) and the distance traveled to 6 minutes walking test (29). This present work has the benefit of including and following up a larger population of patients at risk regardless of their medical history. The other point highlighted in our study was the feasibility of performing preoperative pulmonary rehabilitation. Some argue that prehabilitation takes time and may delay the date of surgery. However, we did not observe any significant difference in the time between CPET and surgery between prehabilitated patients and non-prehabilitated patients. It is noteworthy that preoperative assessment before lobectomy takes approximately the same time as prehabilitation. There are many studies in the literature on the value of prehabilitation and it is clearly recommended to facilitate postoperative recovery (30). After prehabilitation, an increase of VO2max was observed in all our patients. For one patient, VO2max rose from 9.2 to 12.8 mL/min/kg after 18 rehabilitation sessions and the patient went from inoperable to operable status.
Few studies have addressed the question of whether we should perform prehabilitation alone, prehabilitation combined with postoperative rehabilitation or just postoperative rehabilitation. Existing studies found a 12% to 20% decrease in preoperative VO2max after lung resection, depending on the type of surgery (lobectomy or pneumonectomy) (28,31). A study conducted in patients followed both before and after surgery, found an initial increase in VO2max after prehabilitation, then 50 days on average after the procedure a decrease to the pre-surgery level (28). The preoperative benefit was not preserved after surgery, thus necessitating further rehabilitation. Postoperative rehabilitation increase the exercise capacity of people following lung resection (32). In addition, this work was concerned only with minimally invasive surgery associated with prehabilitation with the objective of limiting outcomes generated by this surgery.
However, all major studies on this subject included patients who underwent thoracotomy and only one study included patients with prehabilitation associated with VATS (33).
VATS is a surgical technique which is increasingly used but studies on VATS and prehabilitation are lacking. Published studies were mainly conducted in patients who underwent thoracotomy, but the functional outcomes of thoracotomy are different to those of VATS (18).
We were not able to determine the optimal number of prehabilitation sessions, due to the size of our sample. Nevertheless, the current recommendations agree on around 12 to 30 sessions (14).
Patients with NSCLC sometimes start chemotherapy or radiotherapy before surgery. According to a systematic review published by Pouwels et al., there is a heterogeneity of rehabilitation programs in the literature (34). We relied on a standardized program based on international recommendations, even for patients undergoing chemo-radiotherapy (16).
Authors reported that physical training improves the quality of life of cancer patients and decreases anxiety and disability related to sedentary lifestyles (35). Other authors found that rehabilitation is feasible, safe and can even prevent deterioration of the general condition in lung cancer patients (20). The intensity, repetitiveness and frequency of sessions must be adjusted to the fatigability of the patient and his/her many appointments.
Rehabilitation is often given in shorter and less intensive sessions over a longer period of time. Benzo et al. show that ten preoperative sessions using a customized protocol with non-standard components as exercise based on self-efficacy, inspiratory muscle training and slow breathing can reduce the length of stay (5).
Limitations
Our study has several limitations. First, we have no data on the prescription of preoperative respiratory rehabilitation. Indeed, numerous criteria are commonly used in the implementation of a rehabilitation program: initial delay, patient availability, geographic distance, associated therapeutics etc. As this type of program is not yet common practice, patients with similar characteristics may or may not have benefited from prehabilitation. Second, it would have been preferable to obtain a value of VO2max and FEV1 post-rehabilitation in order to confirm whether those patients improved by prehabilitation were those who best supported surgery. Third, the follow-up visit scheduled 30 days after surgery did not allow us to record postoperative complications occurring after day 30 and up to 6 months following surgery (36). It should also be noted that there are no unified protocols for analgesia, and that this may constitute a bias. Finally, this remains a retrospective cohort study conducted in a single center and with a small sample size. A larger scale study is needed to confirm the results.
Conclusions
The results of this study suggest that prehabilitation has an impact on the occurrence and severity of postoperative complications. Prehabilitation is easy to perform and easily adapted to each patient’s functional abilities. Prehabilitation should be considered systematically in patients with NSCLC to reduce operative risks and limit the functional impact of lung resection surgery.
Acknowledgements
The authors are grateful to Nikki Sabourin-Gibbs, Rouen University Hospital, for her help in editing the manuscript.
Ethical Statement: All procedures performed in this study were in accordance with the ethical standards of the institutional and national research committee: Cerni E2017-32.
Footnotes
Conflicts of Interest: Dr. Baste and Prof. Peillon are consultants for Medtronic and Intuitive surgery.
References
- 1.Collaborators GBDRF. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016;388:1659-724. 10.1016/S0140-6736(16)31679-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.de Leyn P, Decker G. Surgical treatment of non-small cell lung cancer. Rev Mal Respir 2004;21:971-82. 10.1016/S0761-8425(04)71479-5 [DOI] [PubMed] [Google Scholar]
- 3.Bach PB, Cramer LD, Schrag D, et al. The influence of hospital volume on survival after resection for lung cancer. N Engl J Med 2001;345:181-8. 10.1056/NEJM200107193450306 [DOI] [PubMed] [Google Scholar]
- 4.Smetana GW, Lawrence VA, Cornell JE, et al. Preoperative pulmonary risk stratification for noncardiothoracic surgery: systematic review for the American College of Physicians. Ann Intern Med 2006;144:581-95. 10.7326/0003-4819-144-8-200604180-00009 [DOI] [PubMed] [Google Scholar]
- 5.Benzo R, Wigle D, Novotny P, et al. Preoperative pulmonary rehabilitation before lung cancer resection: results from two randomized studies. Lung Cancer 2011;74:441-5. 10.1016/j.lungcan.2011.05.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Benattia A, Debeaumont D, Guyader V, et al. Physiologic assessment before video thoracoscopic resection for lung cancer in patients with abnormal pulmonary function. J Thorac Dis 2016;8:1170-8. 10.21037/jtd.2016.04.38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pehlivan E, Turna A, Gurses A, et al. The effects of preoperative short-term intense physical therapy in lung cancer patients: a randomized controlled trial. Ann Thorac Cardiovasc Surg 2011;17:461-8. 10.5761/atcs.oa.11.01663 [DOI] [PubMed] [Google Scholar]
- 8.Bolton CE, Bevan-Smith EF, Blakey JD, et al. British Thoracic Society guideline on pulmonary rehabilitation in adults. Thorax 2013;68:ii1-30. 10.1136/thoraxjnl-2013-203808 [DOI] [PubMed] [Google Scholar]
- 9.Divisi D, Di Francesco C, Di Leonardo G, et al. Preoperative pulmonary rehabilitation in patients with lung cancer and chronic obstructive pulmonary disease. Eur J Cardiothorac Surg 2013;43:293-6. 10.1093/ejcts/ezs257 [DOI] [PubMed] [Google Scholar]
- 10.Nagarajan K, Bennett A, Agostini P, et al. Is preoperative physiotherapy/pulmonary rehabilitation beneficial in lung resection patients? Interact Cardiovasc Thorac Surg 2011;13:300-2. 10.1510/icvts.2010.264507 [DOI] [PubMed] [Google Scholar]
- 11.Sebio Garcia R, Yanez Brage MI, Gimenez Moolhuyzen E, et al. Functional and postoperative outcomes after preoperative exercise training in patients with lung cancer: a systematic review and meta-analysis. Interact Cardiovasc Thorac Surg 2016;23:486-97. 10.1093/icvts/ivw152 [DOI] [PubMed] [Google Scholar]
- 12.Brunelli A, Charloux A, Bolliger CT, et al. ERS/ESTS clinical guidelines on fitness for radical therapy in lung cancer patients (surgery and chemo-radiotherapy). Eur Respir J 2009;34:17-41. 10.1183/09031936.00184308 [DOI] [PubMed] [Google Scholar]
- 13.ATS/ACCP Statement on cardiopulmonary exercise testing. Am J Respir Crit Care Med 2003;167:211-77. 10.1164/rccm.167.2.211 [DOI] [PubMed] [Google Scholar]
- 14.Societe de Pneumologie de Langue F. Recommendations of the French Language Society of Pneumology on the management of COPD (update 2009). Presse Med 2010;39:895-8. [DOI] [PubMed] [Google Scholar]
- 15.Marino DM, Marrara KT, Ike D, et al. Study of peripheral muscle strength and severity indexes in individuals with chronic obstructive pulmonary disease. Physiother Res Int 2010;15:135-43. 10.1002/pri.454 [DOI] [PubMed] [Google Scholar]
- 16.Cavalheri V, Granger C. Preoperative exercise training for patients with non-small cell lung cancer. Cochrane Database Syst Rev 2017;6:CD012020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ortega F, Toral J, Cejudo P, et al. Comparison of effects of strength and endurance training in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2002;166:669-74. 10.1164/rccm.2107081 [DOI] [PubMed] [Google Scholar]
- 18.Agostini P, Lugg ST, Adams K, et al. Postoperative pulmonary complications and rehabilitation requirements following lobectomy: a propensity score matched study of patients undergoing video-assisted thoracoscopic surgery versus thoracotomydagger. Interact Cardiovasc Thorac Surg 2017;24:931-7. 10.1093/icvts/ivx002 [DOI] [PubMed] [Google Scholar]
- 19.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004;240:205-13. 10.1097/01.sla.0000133083.54934.ae [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stephan F. Complications postopératoires de la chirurgie pulmonaire. Reanimation 2002:40-8. 10.1016/S1624-0693(01)00202-X [DOI] [Google Scholar]
- 21.Morano MT, Araujo AS, Nascimento FB, et al. Preoperative pulmonary rehabilitation versus chest physical therapy in patients undergoing lung cancer resection: a pilot randomized controlled trial. Arch Phys Med Rehabil 2013;94:53-8. 10.1016/j.apmr.2012.08.206 [DOI] [PubMed] [Google Scholar]
- 22.Bradley A, Marshall A, Stonehewer L, et al. Pulmonary rehabilitation programme for patients undergoing curative lung cancer surgery. Eur J Cardiothorac Surg 2013;44:e266-71. 10.1093/ejcts/ezt381 [DOI] [PubMed] [Google Scholar]
- 23.Gao K, Yu PM, Su JH, et al. Cardiopulmonary exercise testing screening and pre-operative pulmonary rehabilitation reduce postoperative complications and improve fast-track recovery after lung cancer surgery: A study for 342 cases. Thorac Cancer 2015;6:443-9. 10.1111/1759-7714.12199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bagan P, Oltean V, Ben Abdesselam A, et al. Pulmonary rehabilitation and non-invasive ventilation before lung surgery in very high-risk patients. Rev Mal Respir 2013;30:414-9. 10.1016/j.rmr.2012.12.004 [DOI] [PubMed] [Google Scholar]
- 25.Stefanelli F, Meoli I, Cobuccio R, et al. High-intensity training and cardiopulmonary exercise testing in patients with chronic obstructive pulmonary disease and non-small-cell lung cancer undergoing lobectomy. Eur J Cardiothorac Surg 2013;44:e260-5. 10.1093/ejcts/ezt375 [DOI] [PubMed] [Google Scholar]
- 26.Sekine Y, Chiyo M, Iwata T, et al. Perioperative rehabilitation and physiotherapy for lung cancer patients with chronic obstructive pulmonary disease. Jpn J Thorac Cardiovasc Surg 2005;53:237-43. 10.1007/s11748-005-0032-8 [DOI] [PubMed] [Google Scholar]
- 27.Mujovic N, Mujovic N, Subotic D, et al. Preoperative pulmonary rehabilitation in patients with non-small cell lung cancer and chronic obstructive pulmonary disease. Arch Med Sci 2014;10:68-75. 10.5114/aoms.2013.32806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jones LW, Peddle CJ, Eves ND, et al. Effects of presurgical exercise training on cardiorespiratory fitness among patients undergoing thoracic surgery for malignant lung lesions. Cancer 2007;110:590-8. 10.1002/cncr.22830 [DOI] [PubMed] [Google Scholar]
- 29.Cesario A, Ferri L, Galetta D, et al. Pre-operative pulmonary rehabilitation and surgery for lung cancer. Lung Cancer 2007;57:118-9. 10.1016/j.lungcan.2007.03.022 [DOI] [PubMed] [Google Scholar]
- 30.Granger CL, McDonald CF, Berney S, et al. Exercise intervention to improve exercise capacity and health related quality of life for patients with Non-small cell lung cancer: a systematic review. Lung Cancer 2011;72:139-53. 10.1016/j.lungcan.2011.01.006 [DOI] [PubMed] [Google Scholar]
- 31.Wang JS, Abboud RT, Wang LM. Effect of lung resection on exercise capacity and on carbon monoxide diffusing capacity during exercise. Chest 2006;129:863-72. 10.1378/chest.129.4.863 [DOI] [PubMed] [Google Scholar]
- 32.Cavalheri V, Tahirah F, Nonoyama M, et al. Exercise training undertaken by people within 12 months of lung resection for non-small cell lung cancer. Cochrane Database Syst Rev 2013:CD009955. [DOI] [PubMed] [Google Scholar]
- 33.Sebio R, Yanez-Brage MI, Gimenez-Moolhuyzen E, et al. Impact of a pre-operative pulmonary rehabilitation program on functional performance in patients undergoing video-assisted thoracic surgery for lung cancer. Arch Bronconeumol 2016;52:231-2. [DOI] [PubMed] [Google Scholar]
- 34.Pouwels S, Fiddelaers J, Teijink JA, et al. Preoperative exercise therapy in lung surgery patients: A systematic review. Respir Med 2015;109:1495-504. 10.1016/j.rmed.2015.08.009 [DOI] [PubMed] [Google Scholar]
- 35.Bade BC, Thomas DD, Scott JB, et al. Increasing physical activity and exercise in lung cancer: reviewing safety, benefits, and application. J Thorac Oncol 2015;10:861-71. 10.1097/JTO.0000000000000536 [DOI] [PubMed] [Google Scholar]
- 36.Jayle C, Corbi P. Complications of pulmonary resection. Rev Mal Respir 2007;24:967-82. 10.1016/S0761-8425(07)92762-X [DOI] [PubMed] [Google Scholar]


