Abstract
The 2014 Ebola virus disease (EVD) outbreak affected several countries worldwide, including six West African countries. It was the largest Ebola epidemic in the history and the first to affect multiple countries simultaneously. Significant national and international delay in response to the epidemic resulted in 28,652 cases and 11,325 deaths. The aim of this study was to develop a risk analysis framework to prioritize rapid response for situations of high risk. Based on findings from the literature, sociodemographic features of the affected countries, and documented epidemic data, a risk scoring framework using 18 criteria was developed. The framework includes measures of socioeconomics, health systems, geographical factors, cultural beliefs, and traditional practices. The three worst affected West African countries (Guinea, Sierra Leone, and Liberia) had the highest risk scores. The scores were much lower in developed countries that experienced Ebola compared to West African countries. A more complex risk analysis framework using 18 measures was compared with a simpler one with 10 measures, and both predicted risk equally well. A simple risk scoring system can incorporate measures of hazard and impact that may otherwise be neglected in prioritizing outbreak response. This framework can be used by public health personnel as a tool to prioritize outbreak investigation and flag outbreaks with potentially catastrophic outcomes for urgent response. Such a tool could mitigate costly delays in epidemic response.
Keywords: Ebola virus disease, outbreak, risk analysis, risk framework, West Africa
1. BACKGROUND
The 2014 Ebola virus disease (EVD) outbreak that started in Guinea in December 2013 is the 25th known EVD outbreak since 1976.1 It is the largest outbreak in history in terms of morbidity and mortality, affecting over 10 countries worldwide in three continents (CDC, 2014). In terms of the duration, it is also the longest and largest Ebola epidemic and the first to affect the three entire countries in West Africa (Guinea, Sierra Leone, and Liberia) including state capitals simultaneously.1 Nigeria, Mali, and Senegal were other affected countries in West Africa.
Despite the scale of the epidemic, it was similar to previous EVD outbreaks in terms of incubation period, infectiousness, clinical course, the case fatality rate, and the reproductive number.2 This suggests that the failure to control the EVD outbreak in West Africa is not due to innate virological features, but may reflect the characteristics of the affected countries, health systems, and the response efforts.2 Travel, traditional practices, and transmission within health‐care systems have been implicated in the spread of EVD to some other West African countries and beyond.3
In areas of widespread transmission, several factors have been attributed to possible difficulties in controlling this outbreak. These include weak health services, scarcity of health workers, traditional beliefs in disease causation, high‐risk traditional burial practices, high population mobility across borders, low level of trust in authorities, and inadequate national and international response.1
While epidemiology is useful for disease‐based predictions and analysis, risk analysis can be used to prioritize epidemic response and improve systems outcomes.4 Risk analysis is a science that helps to understand important predictors of risks in various fields such as security, biochemistry, toxicology, modeling, climate change, information technology, and engineering.4 A few frameworks have been developed for programmatic risk assessment of polio and measles.5, 6, 7 One study also examined the impact of various strategies on the number of polio cases during an outbreak, and response delay was identified as the key factor determining the size of an outbreak.8 A risk analysis approach had also been used to examine the cross‐species transmission of pathogens in the past.5
The development of an EVD risk scoring framework would be useful to predict the risks and outcome of an outbreak. Its application would enable rapid, timely, and effective response to high‐risk outbreaks, so as to mitigate the impact of the outbreak. While there have been studies on the clinical risk stratification of EVD cases,9 no study has been done to risk‐stratify the region and countries with an EVD outbreak based on factors such as socioeconomic, environmental, and health system. The aim of this study was to develop a risk analysis framework to predict the risks and outcome of an outbreak. We used the EVD outbreak as a case study to identify countries that were successful in rapidly curtailing the outbreak and those that were unsuccessful. Findings from the newly developed risk score framework cannot be generalized but could be improved upon and adapted for other infectious diseases and public health emergencies.9
2. METHODS
An online search was conducted on Pubmed and Medline using key words to search peer‐reviewed journals from January 2014 to October 2015. The websites of Centers for Disease Control and Prevention, World Health Organisation (WHO), and Médecins Sans Frontières, media news, human interest articles, and reports around Ebola outbreaks from January 2014 to October 2015 were also reviewed to identify and collect data on EVD outbreak risk factors. Other sources from which data were also collected include gray literature and government websites of Ebola‐affected countries.
Data were collected on outbreak characteristics, socioeconomic factors, cultural and behavioral factors, traditional practices, health system, and economic indices of each country.
2.1. Criteria for Selecting Risk Factors
Based on literature review, comparison between countries’ outbreak situation, and reports from gray literature and theoretical relevance,10 some risk factors associated with the EVD outbreak, among several others, were identified and selected for the purpose of risk score framework development. The risk factors were categorized as socioeconomic, geographical, traditional/cultural, and health systems related. These consist of the followings:
-
(1)
Socioeconomic/political
-
(i)
Gross domestic product (GDP)
-
(ii)
Health expenditure, total (% of GDP)
-
(iii)
History of war/civil unrest/conflicts
-
(i)
-
(2)
Geographic
-
(i)
Nature (porosity) of country's land border
-
(ii)
Quarantine system and border screening
-
(iii)
Roadways/transport network
-
(i)
-
(3)
Health system
-
(i)
Physician density
-
(ii)
Nurses and midwife density
-
(iii)
Density of skilled health workers (nurses, midwives, and physicians)
-
(iv)
Hospital bed density
-
(v)
Availability of laboratory diagnostic capacities
-
(vi)
Timeliness of laboratory results
-
(vii)
Disease surveillance and response (DSR)
-
(i)
-
(4)
Cultural/traditional
-
(i)
High‐risk traditional practices
-
(ii)
Consumption of bush meat
-
(iii)
Unsafe animal handling practices
-
(iv)
Overcrowded living
-
(v)
Use of unregulated traditional medicine
-
(i)
Criteria for assigning risk scores (see Annex I in online supplementary file)
Risk scores were assigned to the selected risk factors based on criteria from WHO, the World Bank, U.N. Development Programmes, and other relevant studies. Values from 1 to 3 were used to denote the individual level of risk, where “1” was considered as low risk, “2” as moderate risk, and “3” as high risk.
A risk score framework was then developed (Table I), which was used to compare Ebola‐affected West African countries (Guinea, Liberia, Sierra Leone, Nigeria, Senegal, and Mali) with two developed countries (the United Kingdom and the United States) that experienced Ebola outbreak. The values assigned were based on different criteria as explained under each of the risk factors and the total risk score ranged from 18 to 46. Risk scores were calculated for the different countries by summing scores for individual measures as shown in Table I.
Table I.
Risk Framework––Scoring Criteria
| Risk Factor | Risk Score | Comment | |||
|---|---|---|---|---|---|
| 1 | Gross domestic product (GDP) | Low‐income countries = 3 | Middle (lower and upper) income countries = 2 | High‐income countries = 1 | The World Bank classifies countries' GDP on the income level as high, middle (upper and lower), and low income. |
| 2 | Health expenditure, total (% of GDP) | Lower third (1.0–7.0%) = 3 | Middle third (7.1–14.0%) = 2 | Upper third (14.1–20.0%) = 1 | Country's health expenditure spread was divided into upper, middle, and lower third. |
| 3 | History of war/civil unrest within the last decade | > Five years = 3 | ≤Five years = 2 | No conflicts = 1 | Wars/civil unrest could destroy a nation's health system within two years. The longer the war, the more destructive impact it has on basic amenities and the health system. This reduces prompt response to disease outbreak. |
| 4 | Use of traditional healer and high‐risk traditional practicesa | High = 3 | Moderate = 2 | Low = 1 | Traditional healers are associated with high‐risk traditional practices such as the use and reuse of unsterilized needles/sharp objects/knives for blood‐letting procedures and unsafe burial practice. The higher the rate of use, the higher the risk of disease spread. |
| 5 | Consumption of bush meat | Routine = 3 | Occasional = 2 | Never = 1 | Consumption of bush meat has been associated with EVD outbreak in the past. The more frequently its consumption, the more the likelihood of exposure to infection. |
| 6 | Unsafe animal handling practices | Low = 3 | Occasional = 2 | Routine = 1 | Unsafe animal handling practices such as not using hand gloves and not performing hand‐washing after contacts with animals. |
| 7 | Physician density (per 1,000 population) | <0.1 = 2 | ≥ 0.1 = 1 | Sufficient number of physician as well as proportionate distribution across the country enhances adequate access to basic medical care. Insufficient physicians in the workforce is associated with increased travel distance and time for patient, thereby increasing the risk of disease spread. Other associated risks include increased contact with more patients due to increased workload for the physician. The World Bank recommended a minimum of 0.1 physician/1,000 population. | |
| 8 | Nurses and midwife density (per 1,000 population) | <0.2 = 3 | 0.2–0.4 = 2 | >0.4 = 1 | Nurses and midwives form a significant proportion of the health workforce. They play a major role in the hospital setting as well as other settings such as homecare and community. The World Bank recommends a minimum of 0.2–0.4 nurses and midwives/1,000 population. |
| 9 | Density of skilled health workers (nurses, midwives, and physicians) 22.8/10,000 | <22.8/10,000 = 2 | ≥22.8/10,000 | The World Health Organization recommends a minimum of 22.8 skilled health‐care workers per 10,000 population to provide basic health coverage. Countries that fail to achieve this target are at higher risk of disease spread than others. | |
| 10 | Hospital beds density (per 1,000 population) | Lower density (0.1–2/1,000) = 3 | Middle density (>2–4/1,000) = 2 | Upper density (>4/1,000) = 1 | Hospital beds are an indicator for available resources to deliver in‐patient services both in a normal hospital setting and during outbreaks when patient loads are likely to be increased. Insufficient hospital beds are likely to increase home/community stay, thereby increasing the risk of infectious disease spread. |
| 11 | Availability of diagnostic capacity of infectious agent(s) in available laboratory (including laboratory density and laboratory staff density) | Absent = 2 | Present = 1 | Availability of diagnostic capacity facilitates prompt detection/diagnosis of disease and confirmation of outbreak. This therefore enhances prompt public health intervention. The lack of such facility is associated with high risk of disease spread with major consequences. | |
| 12 | Timeliness of laboratory result | <80% of result available within minimum turnaround time for test = 2 | ≥80% of result available within minimum turnaround time for test = 1 | The presence of diagnostic capacity does not translate to performance. IDSR recommends that a minimum of 80% of test result should be available within the minimum turnaround time of the test. | |
| 13 | Disease surveillance response (DSR) indicators | <80% of target = 2 | ≥80% of target = 1 | Risk scores were assigned to DSR using the core capacity areas recommended in the technical guidelines for integrated disease surveillance and response. 80% is the recommended target. | |
| 14 | Nature of land border/border security | >3 or landlocked = 3 | 1 or 3 sided = 2 | Entirely surrounded by water = 1 | Topographic features of land borders correlate with the degree of pedestrian mobility and the time required to travel across the border. This also correlates with the likelihood of interborder disease spread. |
| 15 | Quarantine system/screening at the borders | Rarely = 3 | Occasional = 2 | Efficient /functional = 1 | Proper screening at the borders (air, land, and sea) can help to identify and prevent the spread of infection into a country. Identified cases can be promptly quarantined. |
| 16 | Roadways/transportation network | Poor = 2 | Good = 1 | Poor roadways/transportation networks affect patients’ evacuation to treatment center, specimen transportation to the laboratory, and contact tracing. | |
| 17 | Overcrowded living | High = 2 | Low = 1 | Overcrowded living is associated with infection of several people simultaneously as well as rapid spread. | |
| 18 | Use of unregulated traditional medicine | High = 2 | Low = 1 | Traditional medicine and cultural and spiritual belief in some countries serve as the main source of primary care. Countries with high use are associated with high risk (a score of 2) and those with low use have a low risk (a score of 1). | |
| Total | Highest = 46 | Lowest = 18 | |||
High‐risk traditional practices such as unsafe burial practices and scarification marks.
The criteria are fully explained in Annex I (online supplementary file).
2.2. Sensitivity Analysis
The proposed risk framework could perform differently based on the number of selected measures. Sensitivity analysis was therefore done by selecting a subset of risk factors to check the performance of the risk framework. All criteria (18) were applied to the selected countries and compared with fewer (10) risk factors. The total risk scores for each country were calculated for the 18 criteria and compared with that of total risk score for the selected 10 criteria. The outcomes from the scores were then compared with the actual epidemic impact in each selected country.
3. RESULTS
Table II compares the outbreak magnitude and features in the six selected Ebola‐affected countries in West Africa.
Table II.
Outbreak Features in Selected Ebola‐Affected Countries, African Countries, November 2015
| Outbreak Characteristics | Nigeria | Guinea | Liberia | Sierra Leone | Senegal | Mali | United Kingdom | United States |
|---|---|---|---|---|---|---|---|---|
| Country population | 183,541,000 | 12,609,000 | 4,503,000 | 6,453,000 | 13,508, 715 | 17,600,000 | 64,559,135 | 318,857,056 |
| Source of outbreak | Liberia by air importation | Within Guinea ?? zoonosis | Guinea | Guinea | Guinea | Guinea | Sierra Leone | Liberia |
| Duration of outbreak | 13 weeks | One year, eight months (still ongoing) | 14 months (first outbreak) and 10 weeks (second outbreak | One year, seven months | Seven weeks | 11 weeks | 10 weeks | 12 weeks |
| Time from start to peak of outbreak | Three weeks | 12 months | Five months | Seven months | One week | Three weeks | One week | Five weeks |
| Involvement of country's capital city | No––but the most densely populated state was affected | Yes | Yes | Yes | No | No | No | No |
| Time taken for detection of index case/diagnosis of outbreak | Within three days | Three months | Several weeks | Several weeks | Within one week | Within three days | Within 24 hours | Five days |
| Number of confirmed, probable, or suspected cases | 20 | 3,792 | 10,672 | 13,683 | 1 | 8 | 1 | 4 |
| Number of confirmed, probable, or suspected deaths | 8 | 2,530 | 4,808 | 3,953 | 0 | 6 | 0 | 1 |
| No. of infected health workers | 11 | 196 | 378 | 307 | 0 | 2 | 1 | 3 |
| No. of health worker deaths | 5 | 100 | 100 | 221 | 0 | 2 | 0 | 0 |
| Infection control practices (ICPs) and preparedness practices | ICP was enhanced with available resources | Lack of resources limited ICP | Lack of resources limited ICP | Lack of resources limited ICP | Adequate resources enhanced ICP | Adequate resources enhanced ICP | Adequate resources enhanced ICP | Adequate resources enhanced ICP |
| Challenges with data collection and timely reporting | None | Present due to insufficient resources and Internet communication | Present due to insufficient resources and Internet communication | Present due to insufficient resources and Internet communication | None | None | None | None |
| Challenges with communication (phone and Internet) | Absent | Present | Present | Present | Absent | Absent | Absent | Absent |
| Basic infrastructural challengea | Moderately strong | Weak––affected transport of patients, laboratory samples, and health information | Weak––affected transport of patients, laboratory samples, and health information | Weak––affected transport of patients, laboratory samples, and health information | Moderately strong | Moderately strong | Strong | strong |
| Local health system responses | Good, intense contact tracing, early isolation of infected cases as polio program mobilized its resources | Difficulty with and inability to trace an isolate infected individual | Difficulty with and inability to trace an isolate infected individual | Difficulty with and inability to trace an isolate infected individual | Prompt, intense contact tracing, early isolation of infected cases | Prompt, intense contact tracing, early isolation of infected cases | Prompt, intense contact tracing, early isolation of infected cases | Prompt, intense contact tracing, early isolation of infected cases |
| International support and responses | Arrived early | Delayed, also met with resistance | Delayed, also met with resistance | Delayed, also met with resistance | Arrived early | Arrived early | Arrived early | Arrived early |
| Level of cooperation with international agencies | High level of cooperation and acceptance of support from WHO and others | History of uncooperativeness, local crises, and conflicts with international agencies and HCWs | History of uncooperativeness, local crises, and conflicts with international agencies and HCWs | History of uncooperativeness, local crises, and conflicts with international agencies and HCWs | High level of cooperation and acceptance of support from WHO and others | High level of cooperation and acceptance of support from WHO and others | High level of cooperation and acceptance of support from WHO and others | High level of cooperation and acceptance of support from WHO and others |
| Security challenges and noncompliance with health staff during outbreak | Absent | Present––due to traditional beliefs and practices, distrust in government and response efforts | Present––due to traditional beliefs and practices, distrust in government and response efforts | Present––due to traditional beliefs and practices, distrust in government and response efforts | Absent | Absent | Absent | Absent |
Basic infrastructural challenges include transportation, telecommunication, and road systems.
The outbreak in Nigeria, Senegal, Mali, and the two developed countries (the United Kingdom and the United States) only lasted for weeks, while that of Guinea, Liberia, and Sierra Leone continued for over a year. The outbreaks lasted several months in these three most widely affected West African countries before reaching their peak, while they lasted only a few weeks for the other countries under study.
In terms of outbreak diagnosis, the Ebola virus was diagnosed within hours to a few days in the United Kingdom, the United States, Nigeria, Mali, and Senegal, whereas in Liberia, Guinea, and Sierra Leone, diagnosis was made after several weeks to several months from the onset of the outbreak. These three most widely affected countries also experienced a great morbidity and mortality among their health‐care workforce from the EVD outbreak when compared with other affected West African countries, the United Kingdom, and the United States.
The characteristic features of the EVD outbreak in the three most widely affected countries compared to others include: all their capital cities were affected, basic health system infrastructures were weak before the outbreak, local health system response was poor, and there was initial lack of cooperation with international agencies.
Tables III and IV, respectively, show the overall risk score for all the countries and their scores with some selected risk factors for sensitivity analysis. In the overall risk framework assessment (Table III), Guinea, Liberia, and Sierra Leone, the three most widely affected countries, had the highest ranking among the West Africa countries. Guinea has the highest risk score among all West African countries. The two developed countries had very low scores when compared with the West African countries generally. A higher risk score indicates a higher likelihood of outbreak occurrence and a higher outbreak magnitude.
Table III.
Combined Risk Scores for West African Countries and Two Developed Countries (United States and United Kingdom) Affected by EVD,a November, 2015
| Risk Criteria | Nigeria | Guinea | Liberia | Sierra Leone | Senegal | Mali | United States | United Kingdom | |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Gross domestic product (GDP) | 2 | 3 | 3 | 3 | 3 | 3 | 1 | 1 |
| 2 | Health expenditure (% of GDP) | 3 | 3 | 2 | 2 | 3 | 2 | 1 | 2 |
| 3 | History of war/civil unrest within the last decade | 1 | 3 | 3 | 3 | 2 | 1 | 1 | 1 |
| 4 | Use of traditional healer and high‐risk traditional practices | 1 | 3 | 3 | 3 | 2 | 2 | 1 | 1 |
| 5 | Consumption of bush meat | 2 | 3 | 3 | 3 | 3 | 3 | 1 | 1 |
| 6 | Unsafe animal handling practices | 2 | 3 | 3 | 3 | 3 | 3 | 1 | 1 |
| 7 | Physician density | 1 | 1 | 2 | 2 | 1 | 1 | 1 | 1 |
| 8 | Nurses and midwives density | 1 | 2 | 2 | 2 | 1 | 1 | 1 | 1 |
| 9 | Density of skilled HCW | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 1 |
| 10 | Hospital bed density | 3 | 3 | 3 | 3 | 3 | 3 | 2 | 2 |
| 11 | Availability of diagnostic capacity | 1 | 2 | 2 | 2 | 1 | 1 | 1 | 1 |
| 12 | Timeliness of laboratory result | 1 | 2 | 2 | 2 | 1 | 1 | 1 | 1 |
| 13 | Disease surveillance and response | 1 | 2 | 2 | 2 | 2 | 2 | 1 | 1 |
| 14 | Nature of land border | 3 | 3 | 2 | 2 | 3 | 3 | 2 | 2 |
| 15 | Quarantine system and border screening | 2 | 3 | 3 | 3 | 2 | 2 | 1 | 1 |
| 16 | Roadways/transportation network | 1 | 2 | 2 | 2 | 1 | 1 | 1 | 1 |
| 17 | Overcrowded living | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 1 |
| 18 | Use of unregulated traditional medicine | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 1 |
| TOTAL | 31 | 44 | 43 | 43 | 37 | 35 | 20 | 21 |
Rationale for assigning risk scores for each criterion to individual country (attached as Annex II in online supplementary file).
Table IV.
Simplified Risk Scores for West African Countries and Two Developed Countries (United States and United Kingdom) Affected by EVD
| Risk Criteria | Nigeria | Guinea | Liberia | Sierra Leone | Senegal | Mali | United States | United Kingdom | |
|---|---|---|---|---|---|---|---|---|---|
| 1 | GDP | 2 | 3 | 3 | 3 | 3 | 3 | 1 | 1 |
| 2 | Health expenditure (% of GDP | 3 | 3 | 2 | 2 | 3 | 2 | 1 | 2 |
| 3 | History of war/civil unrest within the last decade | 1 | 3 | 3 | 3 | 2 | 1 | 1 | 1 |
| 4 | Use of traditional healer and high‐risk traditional practices | 1 | 3 | 3 | 3 | 2 | 2 | 1 | 1 |
| 5 | Unsafe animal handling practices | 2 | 3 | 3 | 3 | 3 | 3 | 1 | 1 |
| 6 | Physician density | 1 | 1 | 2 | 2 | 1 | 1 | 1 | 1 |
| 7 | Nurses and midwives density | 1 | 2 | 2 | 2 | 1 | 1 | 1 | 1 |
| 8 | Density of skilled HCW | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 1 |
| 9 | Availability of diagnostic capacity | 1 | 2 | 2 | 2 | 1 | 1 | 1 | 1 |
| 10 | Quarantine system and border screening | 2 | 3 | 3 | 3 | 2 | 2 | 1 | 1 |
| TOTAL | 16 | 25 | 25 | 25 | 20 | 18 | 10 | 11 |
When risk criteria were reduced from 18 parameters to 10, the new risk scores for each of the countries followed the same pattern of the overall risk scores (Fig. 1).
Figure 1.
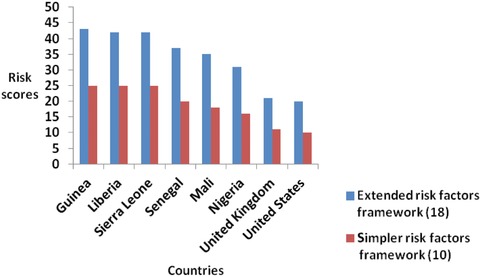
Sensitivity analysis: a comparison of countries’ extended (18) risk score with a simpler set (10).
4. DISCUSSION
A risk scoring framework is a useful tool for predicting the impact of infectious disease outbreaks as well as those of public health emergencies. This would inform the decision to initiate prompt response to mitigate the impact of such outbreaks. A higher risk score indicates the need for a more proactive, aggressive, and prompt response compare to a lower risk score. Risk scores and health preparedness indices could also help to improve disease surveillance and strengthen planning and engagement at the community level.11
This risk scoring framework is a tool that can be used by local and state governments, health organizations, and other stakeholders to rapidly assess and predict the outbreak characteristic and plan control measures.
In this study, we developed a risk scoring framework (Table I) that could be used to prioritize epidemic response, predict the impact and extent of an outbreak, and therefore enhance rapid and effective response in outbreaks of high risk. We showed that the overall risk score for Ebola‐affected countries correlated well with the magnitude and impact of the epidemic in each country, with the worst affected countries, Guinea (score = 44), Liberia (score = 43), and Sierra Leone (score = 43) scoring highest, and the United States (20) and the United Kingdom (21) scoring lowest. Nigeria had the lowest risk score (31) in all the West African countries. We further demonstrated that a simplified framework with fewer measures performs equally well in predicting risk. This indicates that a complex scoring system with multiple parameters is not necessary, and that for utility in the field, a shorter scoring system can be used.
Such a risk scoring system, if in use prior to the 2014 EVD epidemic, might have flagged the need for urgent intervention by WHO and improved the response time. In the case of the West African Ebola outbreak, there have been criticisms of the severely delayed international response, with the outbreak documented in March 2014 but sustained control efforts not undertaken until August/September 2014, close to the peak of the epidemic.12 Epidemics rise exponentially, so every day of delay averted saves lives.
Such a risk scoring system could have correctly predicted that the risk of the outbreak in Guinea, Liberia, or Sierra Leone would be extremely high.13 The predictive parameters of the risk scoring framework can further be demonstrated by comparing the outcome of the EVD outbreak in the less affected West African countries with the three most widely affected countries.
In Nigeria, it was observed that early detection of the virus through accessible diagnostic facilities, as well as swift quarantine and contact tracing procedures, was central to the success of curtailing the outbreak swiftly in Nigeria.13 The same diagnostic capability also aided containment of the outbreak in Senegal and Mali.14 These all correspond with a lower risk score in the health system. In Guinea, in contrast, it took several weeks to months before the initial cases were detected,15 a factor associated with a higher risk score. This prolonged period of exposure to Ebola virus before detection generated many cases and several chains of transmission, including into the capital, Conakry, which made the outbreak difficult to control.16 When diagnostic facilities became available in the course of the outbreak, the local capacity was quickly overwhelmed, which is another factor associated with higher risk.16 This same factor also expedited the transmission of the virus into Liberia and Sierra Leone.
Other factors associated with lower risk scores such as effective and prompt contact tracing in addition to adequate infection control practices correlated with reduction in the geographic range and size of EVD outbreaks.17 Nigeria replicated the structure and system of its well‐established Polio Emergency Operation Centre to combat the EVD outbreak.6, 18 The country promptly deployed about 200 health‐care staff for contact tracing19 and within a month, over 26,000 homes were visited and over 18,000 people with EVD contacts were interviewed.6, 9, 18 The contact tracing teams were able to trace every generation of contact and those who escaped quarantine were tracked down and brought under supervision.9, 20, 21 Contact tracing was also very prompt and effective in Senegal and Mali. The staff strength in Mali was particularly increased by training and engaging medical students.14
In contrast, in Guinea, Liberia, and Sierra Leone, insufficient health‐care staff, difficulty and lack of ability to trace contacts, and failure to isolate infected individuals complicated the outbreak.17 In places where contact tracing occurred, isolation and monitoring were deficient.22
The existing structure of the health system before the outbreak has also been found to be central to the outcome of the EVD outbreak. The health‐care systems in Liberia, Guinea, and Sierra Leone are associated with high‐risk scores as they were weak before the outbreak, with a severe shortage of health‐care workers.18 The impact of decades of wars and civil unrest (high‐risk factors) in those countries increased the risk and impacted health systems. Those years were marked with fleeing health‐care workers, infrastructure destruction, and interruption of supplies of drugs and medical equipment.23 Nigeria has a robust health system compared to Liberia, Guinea, and Sierra Leone, and has higher health professional density and more advanced surveillance experience in other disease conditions, which was leveraged in responding to the EVD outbreak.18 The polio program experience in Nigeria played a critical role in stopping Ebola transmission.6 Senegal and Mali also have relatively well‐funded health systems.14
While there was a high level of coordination among, and cooperation with, local and international response agencies during the outbreak in Nigeria,24 fear and distrust in the government and the health system characterized the outbreak in Liberia, Guinea, and Sierra Leone.25 This has resulted in hiding of infected patients, escape of contacts from the surveillance system and patients from the treatment centers, high patronage of traditional healers, and hostility to both international and national response team.22 The impact of traditions and culture on epidemics cannot be underestimated.
A country's resources are also in correlation with the extent and outcome of the outbreak. Nigeria has the highest GDP in Africa and ranks 23rd in the world.18 The government, some private organizations, and individuals were able to quickly mobilize funds and all needed resources to contain the outbreak.26 In contrast, the three most affected countries are in the group of the world's poorest countries.22 This is due to the impact of wars and civil unrest on the economy. Another consequence of this poverty from civil unrest is a high rate of unemployment, leading to high mobility across the porous borders of the three countries.22 This high interborder mobility has resulted in transnational importation and reinfection of the EVD, thereby making containment difficult.
Other factors that helped Nigeria in containing the EVD outbreak were: ensuring safe and dignified burial practices with a ban on national and international corpse transfer,27 establishment of diagnostic centers, treatment centers, and research groups across the six geopolitical zones of the country, effective audio‐visual and social media communication, especially on infection control practices and destigmatization,26 as well as strengthened Port Health surveillance.20, 28
In contrast, behavioral, cultural, and traditional practices fueled the EVD outbreak in Liberia, Guinea, and Sierra Leone.25 About 60% of cases of EVD have been linked with unsafe burial practices such as washing, kissing, and touching of corpses.22 The use of traditional healers in these countries is very high25 and spread of Ebola virus in a significant chain of transmission in the Sierra Leone outbreak was associated with attending the funeral ceremony of a traditional healer who died after treating EVD patients.29
Nigeria and Senegal may not be directly comparable with the three worst affected countries because the former countries had ample time to prepare and prevent the outbreak.18 Further, the outbreak in both countries started with a single case, which made contact tracing easier. However, the fact remains that they were well positioned and resourced for containment of the outbreak, while the three worst affected countries had several common risk factors that propagated the outbreak and its impacts. These would have been flagged as needing urgent intervention with availability of a risk score framework.
The United States had a score of 21, while the United Kingdom scored 22, far lower than the lowest score of 32 (Nigeria) in West African countries. The risk score, if applied before the outbreak, would have predicted a low likelihood of outbreak, less significant impact, and easier containment in developed countries when compared with the developing countries such as the West African countries.25
One of the limitations of this study includes the fact that some of the criteria for assigning risk scores were based on gray literature sources, which may not have a proven statistical basis. Another limitation is based on the fact that some of the risk factors may not be suitable for all infectious diseases (e.g., mosquito‐borne infections). Further, this tool was made for Ebola and has not been validated for other diseases.
Finally, our aim was to develop a risk framework that has multiple components that can be used to rapidly assess and predict the outbreak risks for a country in terms of likelihood of spread, epidemic preparedness, magnitude, and impact. It is flexible and can be improved upon.30 This can aid prioritization of epidemic response and timely intervention.
5. CONCLUSION
In conclusion, we have developed and demonstrated the utility of a risk score framework for epidemic response. Criteria that reflect socioeconomic, geographical, traditional/cultural, and health systems related parameters can be used to identify countries at high risk of catastrophic outcomes in terms of morbidity and mortality. This framework can be modified and used by epidemiologists and public health personnel as a tool for identifying and prioritizing the need for urgent intervention in global epidemics and may reduce costly delays in response.
Supporting information
Table 1. Gross domestic product
Table 2. Country's health expenditure, total (% of GDP)
Table 3. History of war/civil unrest in Ebola‐affected areas within the last decade
Table 4. Use of traditional healer and high‐risk traditional practices
Table 5. Consumption of bush meat
Table 6. Unsafe animal handling practices
Table 7. Physician density (per 1,000 population)
Table 8. Nurses and midwives density (per 1,000 population)
Table 9. Skilled health workers (doctors, nurses, and midwives) (per 10,000 population)
Table 10. Hospital bed density (per 1,000 population)
Table 11. Availability of diagnostic capacity for EVD at the initial stage of outbreak
Table 12. Timeliness of laboratory result
Table 13. Disease surveillance and response
Table 14. Nature of land borders
Table 15. Quarantine system and border screening before outbreak
Table 16. Roadways/transportation network
Table 17. Overcrowded living
Table 18. Use of unregulated traditional medicine
ACKNOWLEDGMENTS
This research was supported by NHMRC Centre for Research Excellence Grant APP1107393 (Integrated Systems for Epidemic Response [ISER]).
REFERENCES
- 1. Piot P, Muyembe J‐J, Edmunds WJ. Ebola in West Africa: From disease outbreak to humanitarian crisis. Lancet Infectious Diseases, 2014; 14(11):1034–1035. Available at: http://www.sciencedirect.com/science/article/pii/S1473309914709569, Accessed on April 4, 2015. [DOI] [PubMed] [Google Scholar]
- 2. WHO Ebola Response Team . Ebola virus disease in West Africa—The first 9 months of the epidemic and forward projections. New England Journal of Medicine, 2014; 371(16):1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Tseng C‐P, Chan Y‐J. Overview of Ebola virus disease in 2014. Journal of the Chinese Medical Association, 2014; 78(1):51–55. Available at: http://www.sciencedirect.com/science/article/pii/S1726490114003219, Accessed on January 2, 2015. [DOI] [PubMed] [Google Scholar]
- 4. Jones‐Engel L, Engel GA. Disease risk analysis: A paradigm for using health‐based data to inform primate conservation and public health. American Journal of Primatology, 2006; 68(9):851–854. Available at: http://www.ncbi.nlm.nih.gov/pubmed/16900505, Accessed on October 16, 2015. [DOI] [PubMed] [Google Scholar]
- 5. Bruce Aylward R, Sutter RW, Cochi SL, Thompson KM, Jafari H, Heymann D. Risk management in a polio‐free world. Risk Analysis, 2006; 26(6):1441–1448. Available at: http://doi.wiley.com/10.1111/j.1539-6924.2006.00840.x, Accessed on April 6, 2017. [DOI] [PubMed] [Google Scholar]
- 6. Vaz RG, Mkanda P, Banda R, Komkech W, Ekundare‐Famiyesin OO, Onyibe R, Abidoye S, Nsubuga P, Maleghemi S, Hannah‐Murele B, Tegegne SG. The role of the polio program infrastructure in response to Ebola virus disease outbreak in Nigeria 2014. Journal of Infectious Disease, 2016; 213(Suppl. 3):S140–S146. Available at: https://academic.oup.com/jid/article-lookup/doi/10.1093/infdis/jiv581, Accessed on March 30, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kriss JL, Stanescu A, Pistol A, Butu C, Goodson JL. The World Health Organization Measles Programmatic Risk Assessment Tool—Romania, 2015. Risk Analysis, 2016. Available at: http://doi.wiley.com/10.1111/risa.12669, Accessed on April 6, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Thompson KM, Duintjer Tebbens RJ, Pallansch MA. Evaluation of response scenarios to potential polio outbreaks using mathematical models. Risk Analysis, 2006; 26(6):1541–1556. Available at: http://doi.wiley.com/10.1111/j.1539-6924.2006.00843.x, Accessed on May 31, 2017. [DOI] [PubMed] [Google Scholar]
- 9. Shuaib F, Gunnala R, Musa EO, Mahoney FJ, Oguntimehin O, Nguku PM, Nyanti SB, Knight N, Gwarzo NS, Idigbe O, Nasidi A, Vertefeuille JF. Ebola virus disease outbreak—Nigeria, July–September 2014. Morbidity and Mortality Weekly Report, 2014; 63(39):867–872. Available at: https://www.cdc.gov/Mmwr/preview/mmwrhtml/mm6339a5.htm, Accessed on April 6, 2017. [PMC free article] [PubMed] [Google Scholar]
- 10. Nikolopoulos GK, Fotiou A, Kanavou E, Richardson C, Detsis M, Pharris A, Suk JE, Semenza JC, Costa‐Storti C, Paraskevis D, Sypsa V, Malliori M‐M, Friedman SR, Hatzakis A. National income inequality and declining GDP growth rates are associated with increases in HIV diagnoses among people who inject drugs in Europe: A panel data analysis. PLoS One [Internet], 2015; 10(4):e0122367 Available at: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=4398461&tool=pmcentrez&rendertype=abstract, Accessed on September 27, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Schnirring L. Public health index finds US fairly well prepared. CIDRAP News, 2016. Available at: http://www.cidrap.umn.edu/news-perspective/2016/04/public-health-index-finds-us-fairly-well-prepared. Accessed on April 30, 2016. [Google Scholar]
- 12. World Health Organization . Report of the Ebola Interim Assessment Panel. 2015. Available at: http://www.who.int/csr/resources/publications/ebola/report-by-panel.pdf. Accessed on October 31, 2015.
- 13. Shuaib F, Gunnala R, Musa EO, Mahoney FJ, Oguntimehin O, Nguku PM, Nyanti SB, Knight N, Gwarzo NS, Idigbe O, Nasidi A, Vertefeuille JF. Ebola virus disease outbreak—Nigeria, July–September 2014. Morbidity and Mortality Weekly Report, 2014; 63(39):867–872. Available at: http://www.ncbi.nlm.nih.gov/pubmed/25275332, Accessed on September 28, 2015. [PMC free article] [PubMed] [Google Scholar]
- 14. World Health Organization . Successful Ebola responses in Nigeria, Senegal and Mali In One Year into the Ebola Epidemic. World Health Organization, 2015.. Available at: http://www.who.int/csr/disease/ebola/one-year-report/nigeria/en/, Accessed on September 29, 2015. [Google Scholar]
- 15. Baize S, Pannetier D, Oestereich L, Rieger T, Koivogui L, Magassouba N, Soropogui B, Sow MS, Keïta S, De Clerck H, Tiffany A, Dominguez G, Loua M, Traoré A, Kolié M, Malano ER, Heleze E, Bocquin A, Mély S, Raoul H, Caro V, Cadar D, Gabriel M, Pahlmann M, Tappe D, Schmidt‐Chanasit J, Impouma B, Diallo AK, Formenty P, Van Herp M, Günther S. Emergence of Zaire Ebola virus disease in Guinea. New England Journal of Medicine, 2014; 371:1418–1425. Available at: http://www.nejm.org/doi/full/10.1056/NEJMoa1404505#t=article, Accessed on August 4, 2015. [DOI] [PubMed] [Google Scholar]
- 16. Frieden TR, Damon I, Bell BP, Kenyon T, Nichol S. Ebola 2014—New challenges, new global response and responsibility. New England Journal of Medicine, 2014; 371:1177–1180. [DOI] [PubMed] [Google Scholar]
- 17. Fasina FO, Shittu A, Lazarus D, Tomori O, Simonsen L, Viboud C, Chowell G. Transmission dynamics and control of Ebola virus disease outbreak in Nigeria, July to September 2014. Eurosurveillance, 2014; 19(40):1–8. Available at: http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=20920. [DOI] [PubMed] [Google Scholar]
- 18. Pizzi M. Soon to be Ebola‐free, Nigeria and Senegal show merits of early response. Al Jazeera America, 2014. Available at: http://america.aljazeera.com/articles/2014/10/14/nigeria-senegal-ebola.html, Accessed on September 29, 2015. [Google Scholar]
- 19. Thottam J. The year in Ebola: How to stop the next outbreak. Al Jazeera America, 2014. Available at: http://america.aljazeera.com/articles/2014/12/28/the-year-in-ebolahowtostopthenextoutbreak.html, Accessed on September 29, 2015. [Google Scholar]
- 20. Asuzu MC, Onajole AT, Disu Y. Public health at all levels in the recent Nigerian Ebola viral infection epidemic: Lessons for community, public and international health action and policy. Journal of Public Health Policy, 2015; 36(2):251–258. Available at: http://link.springer.com/10.1057/jphp.2015.2, Accessed on April 6, 2017. [DOI] [PubMed] [Google Scholar]
- 21. Boseley S. Nigeria's Ebola crackdown is an example to the world. Guardian, 2014. Available at: http://www.theguardian.com/world/2014/oct/20/nigeria-ebola-crackdown-example-to-world, Accessed on September 29, 2015. [Google Scholar]
- 22. Chan M. Ebola virus disease in West Africa—No early end to the outbreak. New England Journal of Medicine, 2014; 371:1183–1185. Available at: http://www.nejm.org/doi/full/10.1056/NEJMp1409859, Accessed on September 29, 2015. [DOI] [PubMed] [Google Scholar]
- 23. Kruk ME, Freedman LP, Anglin GA, Waldman RJ. Rebuilding health systems to improve health and promote state building in post‐conflict countries: A theoretical framework and research agenda. Social Science & Medicine, 2010; 70(1):89–97. Available at: http://www.ncbi.nlm.nih.gov/pubmed/19850390, Accessed on September 19, 2015. [DOI] [PubMed] [Google Scholar]
- 24. Tozzi J. How to avert an Ebola nightmare: Lessons from Nigeria's victory. Businessweek, 2014.. Available at: http://www.bloomberg.com/bw/articles/2014-10-20/ebola-how-nigeria-averted-a-nightmare-in-densely-populated-lagos, Accessed on September 29, 2015. [Google Scholar]
- 25. Alexander KA, Sanderson CE, Marathe M, Lewis BL, Rivers CM, Shaman J, Drake JM, Lofgren E, Dato VM, Eisenberg MC, Eubank S. What factors might have led to the emergence of Ebola in West Africa? PLoS Neglected Tropical Diseases, 2015; 9(6):e0003652 Available at: http://journals.plos.org/plosntds/article?id_https://doi.org/10.1371/journal.pntd.0003652, Accessed on June 5, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Ikhuoria E. Case study: How Nigeria contained the Ebola outbreak. [Internet]. Available at: http://www.one.org/us/2014/10/29/case-study-how-nigeria-contained-the-ebola-outbreak/, Accessed on September 29, 2015.
- 27. Federal Ministry of Health . Minister of Health Releases Updated EVD Status of Nigeria, Gives Details of FG's Containment Efforts, 2015.. Available at: http://www.health.gov.ng/index.php/news-media/press-releases/9-uncategorised/193-minister-of-health-releases-updated-evd-status-of-nigeria-gives-details-of-fg-s-containment-efforts, Accessed on September 29, 2015.
- 28. News Medical . Rapid and coordinated response helps control Ebola outbreak in Nigeria. News Medical, 2014. Available at: http://www.news-medical.net/news/20141001/Rapid-and-coordinated-response-helps-control-Ebola-outbreak-in-Nigeria.aspx, Accessed on September 29, 2015. [Google Scholar]
- 29. Gire SK, Goba A, Andersen KG, Sealfon RSG, Park DJ, Kanneh L, Jalloh S, Momoh M, Fullah M, Dudas G, Wohl S, Moses LM, Yozwiak NL, Winnicki S, Matranga CB, Malboeuf CM, Qu J, Gladden AD, Schaffner SF, Yang X, Jiang P‐P, Nekoui M, Colubri A, Coomber MR, Fonnie M, Moigboi A, Gbakie M, Kamara FK, Tucker V, Konuwa E, Saffa S, Sellu J, Jalloh AA, Kovoma A, Koninga J, Mustapha I, Kargbo K, Foday M, Yillah M, Kanneh F, Robert W, Massally JLB, Chapman SB, Bochicchio J, Murphy C, Nusbaum C, Young S, Birren BW, Grant DS, Scheiffelin JS, Lander ES, Happi C, Gevao SM, Gnirke A, Rambaut A, Garry RF, Khan SH, Sabeti PC. Genomic surveillance elucidates Ebola virus origin and transmission during the 2014 outbreak. Science, 2014; 345(6202):1369–1372. Available at: http://www.sciencemag.org/content/345/6202/1369.abstract, Accessed on August 29, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. MacIntyre CR, Seccull A, Lane JM, Plant A. Development of a risk‐priority score for category A bioterrorism agents as an aid for public health policy. Military Medicine, 2006; 171:589–594. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table 1. Gross domestic product
Table 2. Country's health expenditure, total (% of GDP)
Table 3. History of war/civil unrest in Ebola‐affected areas within the last decade
Table 4. Use of traditional healer and high‐risk traditional practices
Table 5. Consumption of bush meat
Table 6. Unsafe animal handling practices
Table 7. Physician density (per 1,000 population)
Table 8. Nurses and midwives density (per 1,000 population)
Table 9. Skilled health workers (doctors, nurses, and midwives) (per 10,000 population)
Table 10. Hospital bed density (per 1,000 population)
Table 11. Availability of diagnostic capacity for EVD at the initial stage of outbreak
Table 12. Timeliness of laboratory result
Table 13. Disease surveillance and response
Table 14. Nature of land borders
Table 15. Quarantine system and border screening before outbreak
Table 16. Roadways/transportation network
Table 17. Overcrowded living
Table 18. Use of unregulated traditional medicine


