Innovations & Provocations are intended to start conversations. Share your reactions and discuss with other clinicians in the comments section online.
“A good solution applied with vigor now is better than a perfect solution applied ten minutes later.” –General George S. Patton (1)
For two decades, we have known that the growing number of older adults would place critical care medicine in a precarious position. In the early 2000s, epidemiologic studies demonstrated the association between age and critical illness (2–5). Workforce shortages, driven by that growth in the aging demographic, were forecasted (6). In response, high-income countries increased the number of intensive care unit (ICU) beds, developed telemedicine/electronic ICU programs to extend the reach of existing clinicians, and expanded the number of critical care providers by incorporating physician extenders into the ICU. Our approach thus far has been akin to preparation for a looming epidemic, building capacity to handle an increased volume of critical care. By these measures, we have been successful—it is now possible to provide more critical care today than ever. With the infrastructure and workforce in place, it is time to focus on an equally important (but thus-far neglected) problem: how to best care for older adults with critical illness.
Older adults bring with them complexity and vulnerability not present in many of their younger counterparts. Vulnerability factors, such as frailty, disability, and multimorbidity, are more prevalent with age (7), and increase the risk of adverse outcomes. In some cases, these factors overlap, conferring even greater risk (8). Although some intensivists may intuitively adapt their clinical practices to address this complexity, formal training at the nexus of geriatrics and critical care is lacking. There is a dearth of evidence to guide the management of critical illness in older adults. It is with our most vulnerable patients in the ICU that we are most in the dark.
Therefore, we propose that critical care medicine begin, in earnest, an effort devoted to addressing the needs of our older patients. This emerging field, known as “geriatric critical care medicine,” addresses the complexities and vulnerabilities of older adults with critical illness by incorporating the principles of geriatric medicine into critical care. The field also promotes an aging focus in basic, clinical, and translational critical care research.
Why Is It Necessary to Integrate the Principles of Geriatrics into Critical Care Medicine, Rather Than Just Consult Geriatrics?
By 2030, the number of Americans aged 65 years or older will double to 70 million (9). This includes nearly 18 million of the “oldest old” who will be aged 85 years or older (9). These demographic shifts are already evident in the ICU, where the oldest old account for more than 20% of admissions (10). For many years, the number of geriatricians has been well short of the number needed to care for all older adults (11). Because the population is aging faster than new geriatricians can be trained, this gap will widen in the coming years. Thus, geriatrician–intensivist comanagement models or widespread geriatric consultative models in the ICU are neither scalable nor sustainable. We, as ICU clinicians, must become adept at managing age-related complexity and vulnerability by integrating geriatrics into our field.
Is There a Precedent for Integrating Geriatrics into Other Subspecialties?
Over a decade ago, academic and philanthropic leaders engaged medical and surgical subspecialists to integrate geriatrics into their respective disciplines, with impressive results (12, 13). For example, among patients with hip fracture, a comanagement strategy between an orthopedic surgeon and a geriatrician (i.e., orthogeriatrics) reduced mortality, postoperative complications (such as delirium), and lengths of stay (14–16). More extensive integration has occurred with the development of the field of geriatric cardiology (12, 17–19). Geriatric cardiologists have created a fully integrated Cardiovascular and Geriatric Medicine fellowship program and developed other educational products, including an online curriculum. In research, an interventional trial of integrated geriatric strategies with acute congestive heart failure management reduced readmissions and improved quality of life for hospitalized older adults (20). The field continues to expand, with federal grant funding to support collaborative meetings and high-impact articles envisioning future growth.
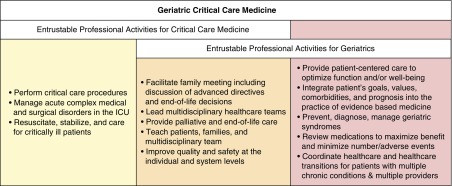
Despite demonstrable evidence of success in other subspecialties, critical care medicine has seen no such sustained effort. This absence is striking considering the overlap of discipline-specific expertise between geriatrics and critical care (Figure 1). This overlap might lead some to say that caring for complexity and vulnerability has always been the hallmark of critical care—that geriatric critical care is simply critical care. Nevertheless, recent data indicate that geriatric syndromes, such as delirium, sensory impairment, and frailty (i.e., age-related clinical conditions that do not fit into discrete disease categories) are: 1) common among patients with critical illness; and 2) associated with morbidity and mortality, independent of traditional critical illness–related risk factors (21–26). Thus, caring for older adults in the ICU does not automatically confer expertise in managing the complexity of these patients. Moreover, in the past, such older patients may have been triaged away from the ICU to a much greater extent than is acceptable today. A systematic approach for integrating geriatrics principles into critical care medicine is needed.
Figure 1.
Entrustable professional activities of geriatrics and critical care medicine. Entrustable professional activities define the skills that describe a discipline’s specific expertise. Geriatric critical care medicine represents the integration of entrustable professional activities from both geriatrics and critical care. The left-hand box (yellow) describes critical care–specific entrustable professional activities. The middle box (orange) describes entrustable professional activities that overlap between geriatrics and critical care. The right-hand box (red) describes the entrustable professional activities for geriatrics. Because these geriatric entrustable professional activities are not traditional components of critical care clinical training, they represent the skills that critical care clinicians should develop to provide optimal care for older adults with critical illness. ICU = intensive care unit.
What Geriatrics Principles Should We Learn and Incorporate into Critical Care Medicine?
A foundational principle of geriatrics is that of decreased reserve with aging. Aging-related physiologic changes, as well as the higher prevalence of geriatric syndromes with age, confer increased vulnerability to adverse outcomes. In practice, geriatricians manage the interaction of acute illness with aging-related decreases in reserve by identifying and managing predisposing, precipitating, and perpetuating factors. Predisposing factors (e.g., frailty) are pre-existing and increase vulnerability to adverse outcomes. Precipitating factors are acute illnesses or injuries (e.g., septic shock or a fall) that trigger an acute decline. Perpetuating factors are conditions (e.g., delirium, immobility, or polypharmacy) that prolong illness or hinder recovery. It is the interaction of predisposing, precipitating, and perpetuating factors that determines survival, development or worsening of impairments and disabilities, and recovery from critical illness. It should be noted that, although advanced age may confer increased vulnerability, patients of the same chronological age often have vastly different vulnerabilities. Consideration of a patient’s precritical illness trajectory provides context to a patient’s illness and their chances of recovery (27). Though not yet evaluated in critical illness, the importance of identifying and managing predisposing, precipitating, and perpetuating factors during acute illness has been shown to improve functional outcomes in multiple clinical trials (28–30).
What Steps Are Needed to Integrate the Principles of Geriatrics into Critical Care Medicine?
A first step toward integration can be achieved by adapting well-established models from non-ICU settings, such as the Acute Care for Elders (ACE) program. Through an interdisciplinary team approach, the ACE model emphasizes maintenance of physical, cognitive, and mental health function, prevention of hospital-acquired geriatric syndromes (such as delirium), and transition of care planning from admission (28). ACE models have been in use for over 20 years, with patients incurring less disability, lower healthcare costs, and fewer readmissions compared with usual care (28, 30, 31). In spite of the evidence supporting their use in non-ICU settings, these concepts have not been widely translated to the ICU. One cornerstone of the ACE model is interdisciplinary team rounding in which all members of the team (i.e., physicians, nurses, therapists, pharmacists, social workers, and nutritionists) coordinate care with an emphasis on rehabilitation and preservation of independence beginning at admission. Because many ICUs already incorporate interdisciplinary team rounding, with training, members of the ICU team could integrate these interventions into practice with minimal or no increases in personnel. Another cornerstone of the ACE model is the concept of the “prepared environment,” or physical environmental modifications to prevent cognitive and functional decline by fostering ambulation, functional independence, and orientation (32). These modifications include additions to the physical environment, such as large clocks and single-date calendars, to enhance orientation, and sensory aids (portable amplifying devices and reading glasses) for patients with hearing or vision impairment. Implementing the “prepared environment” in the ICU would also require significant subtractions from the existing environment, where sensory overload, sleep disruption, and frequent use of tethering devices (e.g., restraints and catheters) remain engrained in ICU culture. A final cornerstone of the ACE model is improving transitions of care. Recent studies highlight lack of communication between transferring and accepting providers about the complexity of patients, diagnoses and treatment plans, and goals of care (33, 34). Thus, early and thorough planning for the ICU-to-floor transition, which currently receives a fraction of the thought that goes into hospital discharge planning, is needed to enhance opportunities for and the quality of communication between multiple providers, patients, and their families, and to address vulnerability factors important to the patient’s recovery, including functional decline or sensory impairment.
Adoption of geriatric care models into the ICU will require integration of geriatric concepts into critical care training programs and clinical practice. Critical care providers must be equipped with the skills to assess and manage geriatric syndromes, such as multimorbidity, frailty, delirium, sensory deficits, cognitive impairment, and disability (35). To achieve this, the current ICU workforce should be trained in foundational geriatric principles, including basic assessment tools and management strategies. This could be achieved with in-service training, quality improvement programs, interdisciplinary “geriatrics champions” to serve as peer resources, and educational programs developed by international critical care societies. Second, critical care medicine fellowship should teach geriatrics principles as part of training. Assessment and management of geriatric syndromes in the ICU should be tested on certification exams. Development of an educational curriculum should include aging physiology relevant to critical illness, assessment of cognitive and physical function, recognition and prevention of geriatric syndromes, evidence behind integrated geriatric models to improve patient outcomes, and thoughtful training in “when less is more” (e.g., minimizing polypharmacy, avoidance of tethering devices/restraints, and careful consideration of the risks and benefits of procedures). Trainees should also learn the limitations of current evidence and clinical practice guidelines as they apply to older adults. Fully integrated critical care and geriatrics fellowship programs should be developed to train true “geriatrics intensivists” who autonomously incorporate principles of geriatrics across the continuum from acute critical illness to ICU survivorship.
Finally, continued discovery in basic, translational, and clinical research is needed to enhance our understanding of how aging interfaces with critical illness and recovery. For example, although the incidence of critical illness increases with age, most basic science research examines critical illness pathology in younger animal models. Failure to consider age-related biological processes, such as cellular senescence, chronic inflammation, and mitochondrial dysfunction, which may not be present in younger animals, could be one reason that drugs effective in animal models of critical illness (e.g., sepsis) have not proven effective in clinical trials (36). In addition, the effects of critical illness on these age-related biological processes is unclear (37). Although incorporating aging into animal research will add time and cost to studies, the resulting findings may more readily translate to humans and provide mechanistic insights into the acute phases and long-term sequelae of critical illness (i.e., post–intensive care syndrome) (38).
Likewise, critical care clinical trials have not traditionally considered factors related to aging. For example, many studies exclude those with multiple comorbidities, disability, or cognitive impairment that results in de facto exclusion of older adults, particularly the oldest old. The importance of considering age-related vulnerability is highlighted by oncology clinical trials that have identified older age and frailty as risk factors for worse chemotherapy toxicity without additional survival benefit (39, 40). Thus, it is unclear whether interventions demonstrated to be effective in younger patients with critical illness are equally effective (or even harmful) in vulnerable older adults. To better align clinical trials with the population in which critical illness develops most frequently, funding agencies should encourage inclusion of older adults in all grant proposals, as is required with minorities and children. Future studies should ensure age-friendly strategies (e.g., allotting additional time to conduct assessments, provide visual and auditory assistive devices) are available. Validated measures of vulnerability factors should be incorporated to better inform outcomes and reduce bias in the reporting of results. The study of age-related vulnerability factors is already being used to facilitate a better understanding of the impairments and disabilities that comprise the post–intensive care syndrome (22, 25). Results from these studies could be used to develop prognostic tools focused on outcomes important to older adults, including function, independent living, and quality of life. In conjunction with interventional studies, benchmarks to gauge the quality of care provided to older adults should be developed. Finally, creation of an aging-focused critical care research consortium would be an ideal forum for multicenter trials, the development of best practices for critical care research, and mentoring the next generation of critical care researchers.
The changes in behaviors and culture required to implement the proposed integration of geriatrics into critical care will require the skill and investment of leaders in critical care and geriatrics on the local, national, and international level, and training the next generation of leaders. In the United States, collaborations are already being forged by a growing number of critical care clinicians and researchers conducting work within existing aging-focused infrastructure, including the Department of Veterans Affairs Geriatric Research, Education, and Clinical Centers and the National Institutes of Health–funded Claude D. Pepper Older Americans Independence Centers and Nathan Shock Centers of Excellence. The next generation of leaders is emerging through the growing number of early career intensivists who are obtaining leadership training and mentorship in the aging-related aspects of critical care through career development programs, such as those sponsored by the National Institute on Aging (41, 42).
We Need to Begin Integrating the Principles of Geriatrics into Critical Care Now
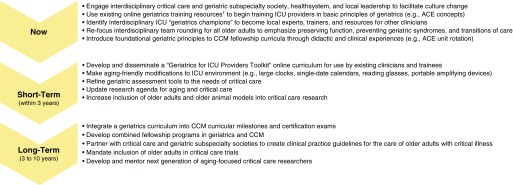
The time to begin this integration is now (Figure 2). If we begin only with future trainees, the number of clinicians who possess the skills to care for older adults will be insufficient and enter the workforce too late to meet the rising demand.
Figure 2.
Timeline and steps for integration of geriatrics principles in critical care medicine. ACE = Acute Care for Elders; CCM = critical care medicine; ICU = intensive care unit. 1https://geriatricscareonline.org/producttypestore/geriatrics-for-specialty-residents-toolkits/6/
Through the foresight of leaders in our field, we heeded the call to expand critical care capacity for the looming growth in the aging demographic—yet this solution leaves us underprepared to face the unique needs of older adults with critical illness. We lag behind our colleagues in other subspecialties who are already improving patient outcomes through the integration of geriatric principles in clinical practice and research. The demographic trends that seemed far off in the early 2000s are upon us, and will only continue. We must begin an immediate investment of time, talent, and resources. As General Patton reminds us, moving quickly will no doubt lead to early missteps, but these missteps will serve as important learning opportunities for how best to optimize care and change practice patterns to address the needs of our most complex and vulnerable patients. Critical care medicine in the 21st century is geriatric critical care; the time to realize this in practice is now.
Supplementary Material
Footnotes
Supported by the National Institute on Aging of the National Institutes of Health (NIH) under award K76AG054864 and by the Doris Duke Foundation (N.E.B.), and by the National Institute on Aging of the National Institutes of Health under award K76AG057023, the Francis Family Foundation, a Pepper Scholar award from the Yale Claude D. Pepper Older Americans Independence Center (NIH/NIA P30AG021342), and a T. Franklin Williams Scholar Award, with funding provided by: Atlantic Philanthropies, Inc., the John A. Hartford Foundation, the Alliance for Academic Internal Medicine-Association of Specialty Professors and the American Thoracic Society Foundation (L.E.F.).
The funding sources had no role in the preparation, review, approval of the manuscript, nor the decision to submit the manuscript for publication.
The views expressed in this paper are solely those of the authors and do not represent the views of the National Institutes of Health, the Doris Duke Foundation, Vanderbilt University Medical Center, or Yale University.
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Province CM. New York: Hippocrene Books; 1983. The Unknown Patton. [Google Scholar]
- 2.Martin GS, Mannino DM, Moss M. The effect of age on the development and outcome of adult sepsis. Crit Care Med. 2006;34:15–21. doi: 10.1097/01.ccm.0000194535.82812.ba. [DOI] [PubMed] [Google Scholar]
- 3.Needham DM, Bronskill SE, Sibbald WJ, Pronovost PJ, Laupacis A. Mechanical ventilation in Ontario, 1992–2000: incidence, survival, and hospital bed utilization of noncardiac surgery adult patients. Crit Care Med. 2004;32:1504–1509. doi: 10.1097/01.ccm.0000129972.31533.37. [DOI] [PubMed] [Google Scholar]
- 4.Angus DC, Linde-Zwirble WT, Lidicker J, Clermont G, Carcillo J, Pinsky MR. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001;29:1303–1310. doi: 10.1097/00003246-200107000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Carson SS, Cox CE, Holmes GM, Howard A, Carey TS. The changing epidemiology of mechanical ventilation: a population-based study. J Intensive Care Med. 2006;21:173–182. doi: 10.1177/0885066605282784. [DOI] [PubMed] [Google Scholar]
- 6.Angus DC, Kelley MA, Schmitz RJ, White A, Popovich J, Jr Committee on Manpower for Pulmonary and Critical Care Societies (COMPACCS) Caring for the critically ill patient. Current and projected workforce requirements for care of the critically ill and patients with pulmonary disease: can we meet the requirements of an aging population? JAMA. 2000;284:2762–2770. doi: 10.1001/jama.284.21.2762. [DOI] [PubMed] [Google Scholar]
- 7.Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Cardiovascular Health Study Collaborative Research Group. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56:M146–M156. doi: 10.1093/gerona/56.3.m146. [DOI] [PubMed] [Google Scholar]
- 8.Fried LP, Ferrucci L, Darer J, Williamson JD, Anderson G. Untangling the concepts of disability, frailty, and comorbidity: implications for improved targeting and care. J Gerontol A Biol Sci Med Sci. 2004;59:255–263. doi: 10.1093/gerona/59.3.m255. [DOI] [PubMed] [Google Scholar]
- 9.Ortman J, Velkoff V, Hogan H. An aging nation: the older population in the United States. Washington, DC: U.S. Census Bureau; 2014. [Google Scholar]
- 10.Sjoding MW, Prescott HC, Wunsch H, Iwashyna TJ, Cooke CR. Longitudinal changes in ICU admissions among elderly patients in the United States. Crit Care Med. 2016;44:1353–1360. doi: 10.1097/CCM.0000000000001664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Institute on Medicine, Committee on The Future Health Care Workforce for Older Americans, Board on Health Care Services. Retooling for an aging America: buliding the health care workforce. Washington, DC: National Academies Press; 2008. [PubMed] [Google Scholar]
- 12.Hurria A, High KP, Mody L, McFarland Horne F, Escobedo M, Halter J, et al. Aging, the medical subspecialties, and career development: where we were, where we are going. J Am Geriatr Soc. 2017;65:680–687. doi: 10.1111/jgs.14708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lee AG, Burton JA, Lundebjerg NE. Geriatrics-for-specialists initiative: an eleven-specialty collaboration to improve care of older adults. J Am Geriatr Soc. 2017;65:2140–2145. doi: 10.1111/jgs.14963. [DOI] [PubMed] [Google Scholar]
- 14.Friedman SM, Mendelson DA, Bingham KW, Kates SL. Impact of a comanaged Geriatric Fracture Center on short-term hip fracture outcomes. Arch Intern Med. 2009;169:1712–1717. doi: 10.1001/archinternmed.2009.321. [DOI] [PubMed] [Google Scholar]
- 15.Vidán M, Serra JA, Moreno C, Riquelme G, Ortiz J. Efficacy of a comprehensive geriatric intervention in older patients hospitalized for hip fracture: a randomized, controlled trial. J Am Geriatr Soc. 2005;53:1476–1482. doi: 10.1111/j.1532-5415.2005.53466.x. [DOI] [PubMed] [Google Scholar]
- 16.Marcantonio ER, Flacker JM, Wright RJ, Resnick NM. Reducing delirium after hip fracture: a randomized trial. J Am Geriatr Soc. 2001;49:516–522. doi: 10.1046/j.1532-5415.2001.49108.x. [DOI] [PubMed] [Google Scholar]
- 17.Bell SP, Orr NM, Dodson JA, Rich MW, Wenger NK, Blum K, et al. What to expect from the evolving field of geriatric cardiology. J Am Coll Cardiol. 2015;66:1286–1299. doi: 10.1016/j.jacc.2015.07.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Forman DE, Rich MW, Alexander KP, Zieman S, Maurer MS, Najjar SS, et al. Cardiac care for older adults: time for a new paradigm. J Am Coll Cardiol. 2011;57:1801–1810. doi: 10.1016/j.jacc.2011.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dodson JA, Matlock DD, Forman DE. Geriatric cardiology: an emerging discipline. Can J Cardiol. 2016;32:1056–1064. doi: 10.1016/j.cjca.2016.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rich MW, Beckham V, Wittenberg C, Leven CL, Freedland KE, Carney RM. A multidisciplinary intervention to prevent the readmission of elderly patients with congestive heart failure. N Engl J Med. 1995;333:1190–1195. doi: 10.1056/NEJM199511023331806. [DOI] [PubMed] [Google Scholar]
- 21.Bagshaw SM, Stelfox HT, McDermid RC, Rolfson DB, Tsuyuki RT, Baig N, et al. Association between frailty and short- and long-term outcomes among critically ill patients: a multicentre prospective cohort study. CMAJ. 2014;186:E95–E102. doi: 10.1503/cmaj.130639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Brummel NE, Bell SP, Girard TD, Pandharipande PP, Jackson JC, Morandi A, et al. Frailty and subsequent disability and mortality among patients with critical illness. Am J Respir Crit Care Med. 2017;196:64–72. doi: 10.1164/rccm.201605-0939OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pisani MA, Kong SY, Kasl SV, Murphy TE, Araujo KL, Van Ness PH. Days of delirium are associated with 1-year mortality in an older intensive care unit population. Am J Respir Crit Care Med. 2009;180:1092–1097. doi: 10.1164/rccm.200904-0537OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pandharipande PP, Girard TD, Jackson JC, Morandi A, Thompson JL, Pun BT, et al. BRAIN-ICU Study Investigators. Long-term cognitive impairment after critical illness. N Engl J Med. 2013;369:1306–1316. doi: 10.1056/NEJMoa1301372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ferrante LE, Pisani MA, Murphy TE, Gahbauer EA, Leo-Summers LS, Gill TM. Factors associated with functional recovery among older intensive care unit survivors. Am J Respir Crit Care Med. 2016;194:299–307. doi: 10.1164/rccm.201506-1256OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Iwashyna TJ, Ely EW, Smith DM, Langa KM. Long-term cognitive impairment and functional disability among survivors of severe sepsis. JAMA. 2010;304:1787–1794. doi: 10.1001/jama.2010.1553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ferrante LE, Pisani MA, Murphy TE, Gahbauer EA, Leo-Summers LS, Gill TM. Functional trajectories among older persons before and after critical illness. JAMA Intern Med. 2015;175:523–529. doi: 10.1001/jamainternmed.2014.7889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Landefeld CS, Palmer RM, Kresevic DM, Fortinsky RH, Kowal J. A randomized trial of care in a hospital medical unit especially designed to improve the functional outcomes of acutely ill older patients. N Engl J Med. 1995;332:1338–1344. doi: 10.1056/NEJM199505183322006. [DOI] [PubMed] [Google Scholar]
- 29.Ellis G, Whitehead MA, Robinson D, O’Neill D, Langhorne P. Comprehensive geriatric assessment for older adults admitted to hospital: meta-analysis of randomised controlled trials. BMJ. 2011;343:d6553. doi: 10.1136/bmj.d6553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fox MT, Persaud M, Maimets I, O’Brien K, Brooks D, Tregunno D, et al. Effectiveness of acute geriatric unit care using acute care for elders components: a systematic review and meta-analysis. J Am Geriatr Soc. 2012;60:2237–2245. doi: 10.1111/jgs.12028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Flood KL, Maclennan PA, McGrew D, Green D, Dodd C, Brown CJ. Effects of an acute care for elders unit on costs and 30-day readmissions. JAMA Intern Med. 2013;173:981–987. doi: 10.1001/jamainternmed.2013.524. [DOI] [PubMed] [Google Scholar]
- 32.Fox MT, Sidani S, Persaud M, Tregunno D, Maimets I, Brooks D, et al. Acute care for elders components of acute geriatric unit care: systematic descriptive review. J Am Geriatr Soc. 2013;61:939–946. doi: 10.1111/jgs.12282. [DOI] [PubMed] [Google Scholar]
- 33.Stelfox HT, Leigh JP, Dodek PM, Turgeon AF, Forster AJ, Lamontagne F, et al. A multi-center prospective cohort study of patient transfers from the intensive care unit to the hospital ward. Intensive Care Med. 2017;43:1485–1494. doi: 10.1007/s00134-017-4910-1. [DOI] [PubMed] [Google Scholar]
- 34.Britton MC, Ouellet GM, Minges KE, Gawel M, Hodshon B, Chaudhry SI. Care transitions between hospitals and skilled nursing facilities: perspectives of sending and receiving providers. Jt Comm J Qual Patient Saf. 2017;43:565–572. doi: 10.1016/j.jcjq.2017.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Brummel NE, Balas MC, Morandi A, Ferrante LE, Gill TM, Ely EW. Understanding and reducing disability in older adults following critical illness. Crit Care Med. 2015;43:1265–1275. doi: 10.1097/CCM.0000000000000924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.López-Otín C, Blasco MA, Partridge L, Serrano M, Kroemer G. The hallmarks of aging. Cell. 2013;153:1194–1217. doi: 10.1016/j.cell.2013.05.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rubenfeld GD. Does the hospital make you older faster? Am J Respir Crit Care Med. 2012;185:796–798. doi: 10.1164/rccm.201202-0267ED. [DOI] [PubMed] [Google Scholar]
- 38.Kennedy BK, Berger SL, Brunet A, Campisi J, Cuervo AM, Epel ES, et al. Geroscience: linking aging to chronic disease. Cell. 2014;159:709–713. doi: 10.1016/j.cell.2014.10.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dale W, Mohile SG, Eldadah BA, Trimble EL, Schilsky RL, Cohen HJ, et al. Cancer and Aging Research Group. Biological, clinical, and psychosocial correlates at the interface of cancer and aging research. J Natl Cancer Inst. 2012;104:581–589. doi: 10.1093/jnci/djs145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Corre R, Greillier L, Le Caër H, Audigier-Valette C, Baize N, Bérard H, et al. Use of a comprehensive geriatric assessment for the management of elderly patients with advanced non–small-cell lung cancer: the phase III randomized ESOGIA-GFPC-GECP 08-02 study. J Clin Oncol. 2016;34:1476–1483. doi: 10.1200/JCO.2015.63.5839. [DOI] [PubMed] [Google Scholar]
- 41.National Institute on Aging. Grants for Early Medical/Surgical Specialists’ Transition to Aging Research (GEMSSTAR)—overview. 2017 [accessed 2017 Dec 5]. Available from: https://www.nia.nih.gov/research/dgcg/grants-early-medical-surgical-specialists-transition-aging-research-gemsstar.
- 42.National Institute on Aging. Paul B. Beeson Emerging Leaders Career Development Award in Aging (K76). 2017 [accessed 2017 Dec 5]. Available from: https://grants.nih.gov/grants/guide/rfa-files/rfa-ag-18-006.html.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.