Abstract
Background
The phenotypes of heartburn patients are heterogeneous.
Objective
The objective of this study was to investigate the proportion of heartburn phenotypes in a Chinese population and to compare the Rome IV and III criteria for heartburn diagnosis.
Methods
A retrospective study was performed among heartburn patients referred for upper endoscopy and esophageal function tests in a tertiary hospital. Their symptoms fulfilled Rome IV and III criteria.
Results
A total of 233 patients were included. Fifty-nine patients (25%) were diagnosed with esophagitis, 96 (41%) with non-erosive reflux disease (NERD) and 78 (34%) with functional heartburn (FH) based on Rome III criteria. Approximately 70% of the Rome III NERD patients were changed based on Rome IV criteria, with 36 patients (15%) diagnosed with reflux hypersensitivity (RH) and 32 patients (14%) who didn’t fulfill the criteria considered unclassified. The FH and RH patients showed higher esophagogastric junction-contractile integral (EGJ-CI) and less hiatal hernia than did Rome IV NERD patients. The unclassified had more hiatal hernias than the FH and RH (p < 0.05). The EGJ-CI was similar between Rome III NERD and FH cases.
Conclusion
The Rome IV criteria were stricter for heartburn diagnosis and superior in distinguishing NERD from functional disorders on motility patterns than Rome III.
Keywords: Heartburn, gastroesophageal reflux disease, function esophageal disorders, Rome III criteria, Rome IV criteria, screening and diagnosis
Key summary
The phenotypes of patients with heartburn are heterogeneous and the proportions of each phenotype are unknown.
The utilization of Rome IV criteria changed the diagnosis of approximately 70% of Rome III-positive non-erosive reflux disease (NERD) cases, among whom approximately 34% had functional heartburn (FH) and 15% had reflux hypersensitivity (RH).
The Rome IV criteria were superior to the Rome III criteria in distinguishing NERD from FH and RH according to motility characteristics. Approximately 14% of the patients didn’t fit the updated criteria.
Introduction
Heartburn, defined as a retrosternal burning sensation rising up through the throat, is the primary symptom for gastroesophageal reflux disease (GERD).1 Given the moderate sensitivity and specificity of heartburn to GERD, clinical trials investigating heartburn patients have suggested that up to one-third of patients reported poor responses to the mainstay GERD therapy (proton pump inhibitors, PPIs),2 indicating that heartburn patients have heterogeneous causes. The diagnosis and management of heartburn therefore remains a major dilemma in clinical practice.
Up to now, the diagnostic criteria for different heartburn phenotypes have relied on the combination of several diagnostic tools including upper endoscopy, high-resolution manometry (HRM) and 24-hour multichannel intraluminal impedance-pH (MII-pH) monitoring. Along with further studies of heartburn, generalist physicians and gastroenterologists are beginning to understand that besides esophageal acid over-exposure, reflux hypersensitivity (RH) and functional heartburn (FH) are two major factors related to PPI refractoriness among heartburn patients.3,4 However, the knowledge regarding heartburn diagnostic criteria is still limited among most clinicians, and the proportions of different heartburn phenotypes remain unknown.
The reason why the proportions of different heartburn phenotypes remain unknown is partially due to their uncertain definitions. For the past 10 years, the Rome III criteria5 have been used as the guideline for heartburn diagnosis, based on which cases with RH and those with negative endoscopy and MII-pH results but an effective response to PPI treatment used to be included in the subgroup of non-erosive reflux disease (NERD). Currently, the definitions have changed according to the recently published Rome IV criteria.6 FH and RH are clearly defined in the updated criteria6 and the 24-hour MII-pH monitoring is used to distinguish these phenotypes among heartburn patients. The proportions of real GERD and functional esophageal disorders would vary according to the new criteria.
To the best of our knowledge, no studies have reported on the agreement or differences between the Rome III and IV criteria for heartburn diagnosis. The aims of the current study were to investigate the proportions of different phenotypes of heartburn patients in a Chinese population, to describe the esophageal function characteristics among these patients based on the Rome IV and III criteria, and to compare the Rome IV and III criteria for heartburn diagnosis. In addition, those patients who did not fit into the updated criteria were also investigated.
Materials and methods
Participants
Patients with uninvestigated heartburn who were referred to our hospital from 2013 to 2016 were enrolled. All patients underwent upper endoscopy, HRM and 24-hour MII-pH monitoring. Their symptom thresholds fulfilled the Rome III and IV criteria.5,6 Patient information including clinical features, upper endoscopy, HRM, 24-hour MII-pH monitoring and outcomes were retrospectively analyzed. Patients who had esophageal or gastric surgery, organic lesions on upper endoscopy including peptic ulcers, Barrett’s esophagus, eosinophilic esophagitis, upper gastrointestinal cancer, etc., or major motility disorders on HRM were excluded. Those who were on antacids, prokinetics, or PPIs seven days before or during the esophageal function test were also excluded. Only those who had undergone eight weeks of PPI treatment after the esophageal function test were included. The study was approved by the Ethical Review Board of Sun Yat-sen University (date: April 15, 2010, number: (2010) 31) and written informed consent was obtained from all participants. The study protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki.
Patients’ symptoms were assessed using the validated Chinese version of GERDQ (GERD questionnaire)7 before and after therapy. PPI therapy was considered effective when patients had no heartburn symptoms at all during the final week of therapy.
The heartburn patients were categorized based on Rome IV and Rome III criteria. Patients were classified into the following five phenotypes based on the Rome IV criteria:6 reflux esophagitis (RE), NERD, RH, FH and unclassified (those with negative endoscopy and MII-pH results but an effective response to PPIs). The patients were also classified into three phenotypes based on the Rome III criteria,5 by which RH and the unclassified were defined as NERD: RE, NERD, and FH.
Upper gastrointestinal endoscopy
The patients underwent upper endoscopy examination before esophageal function tests. Upper endoscopy was performed according to international guidelines.8 The distal esophageal biopsy was taken to exclude the eosinophilic esophagitis. Organic lesions including peptic ulcers, Barrett’s esophagus and upper gastrointestinal cancer were excluded. RE was staged according to the Los Angeles classification. The included patients were then classified as (1) endoscopy negative or (2) RE.
High-resolution esophageal manometry
High-resolution esophageal manometry was performed using a 4.2 mm outer diameter solid-state manometric catheter with 36 circumferential sensors spaced at 1-cm intervals (Given Imaging, Los Angeles, CA, USA). After calibration from 0 to 300 mmHg, the catheter was fixed transnasally, and the measurement was obtained with the patient in a supine position. The manometric protocol included a baseline recording, 10 single liquid swallows and adequate multiple rapid swallows (MRS).
Pressure topography was analyzed manually by two independent investigators using Manoview analysis software (Given Imaging) and based on the Chicago classification criteria.9 The collected parameters included the following: (1) esophagogastric junction (EGJ) parameters: EGJ morphology, lower esophageal sphincter (LES) length, integrated relaxation pressure (IRP), EGJ inspiratory pressure, EGJ expiratory pressure, and EGJ contractile integral (EGJ-CI), which was calculated according to Nicodème et al.;10 (2) peristalsis parameters: distal latency (DL) and distal contractile integral (DCI). The MRS response was also evaluated according to Shaker et al.,11 and the MRS/liquid swallow ratios were calculated for the DCI. The classification of esophageal motility was also analyzed.
Twenty-four-hour MII-pH monitoring
Twenty-four-hour MII-pH monitoring was performed off-therapy using an ambulatory MII-pH monitoring system (Sandhill Scientific Inc, Highland Ranch, CO, USA). After calibration in buffer solutions of pH 4.0 and 7.0, the catheter (ZAI-BS-01, Sandhill Scientific Inc, Highland Ranch, CO, USA) was placed transnasally with the pH electrode 5 cm and impedance channels 3, 5, 7, 9,15, and 17 cm proximal to the LES. Patients were taught to use the digital data device to record symptoms, meals and postures during monitoring.
The data were analyzed manually by two investigators using the Bioview Analysis Software (Bioview Analysis; Sandhill Scientific Inc). Meal periods were excluded from the analysis. The collected parameters included the following: (1) acid exposure time (AET, abnormal value ≥4.0) and (2) symptom association probability (SAP, positive if ≥95%). Pathological reflux was defined as having an abnormal total AET.12
Statistical analysis
Data were presented as either the mean ± standard deviation (SD) or the median (25th, 75th). Grouped data were compared using analysis of variance (ANOVA) or Kruskal-Wallis test as appropriate. For multiple comparisons, Bonferroni’s correction was applied. Categorical data were compared using the χ-squared test. Differences were considered significant when p < 0.05. Statistical analysis was performed using SPSS 20.0 (SPSS Inc, Chicago, IL, USA).
Results
A total of 331 patients with heartburn who were referred for upper endoscopy, HRM and 24-hour MII-pH monitoring from 2013 to 2016 were screened. Eight patients with organic lesions and 75 patients with major motility disorders were excluded. Five patients did not undergo PPI therapy after the procedures and 10 patients were lost during follow-up. In total, 233 patients (122 males, age 43.35 ± 13.21 years) were finally included. Detailed demographic data are shown in Tables 1 and 2.
Table 1.
Demographic characteristics compared among groups based on Rome IV criteria (data presented as mean ± SD or N (%)).
| RE (N = 59) | NERD (N = 28) | RH (N = 36) | FH (N = 78) | Unclassified (N = 32) | p value | |
|---|---|---|---|---|---|---|
| Male gender | 38 (64.41%) | 19 (67.86%) | 14 (38.89%) | 33 (42.31%) | 18 (56.25%) | 0.017a |
| Age (years) | 44.80 ± 12.60 | 48.33 ± 12.49 | 41.39 ± 13.28 | 42.04 ± 12.23 | 41.33 ± 12.62 | 0.154 |
| Weight (kg) | 65.69 ± 10.06 | 62.57 ± 10.72 | 58.49 ± 11.15 | 57.02 ± 11.10 | 60.93 ± 9.83 | 0.000a |
| BMI (kg/m2) | 24.04 ± 2.96 | 23.22 ± 3.03 | 22.20 ± 3.62 | 21.90 ± 3.40 | 22.68 ± 3.21 | 0.004a |
p < 0.05. RE: reflux esophagitis; NERD: non-erosive gastroesophageal reflux disease; RH: reflux hypersensitivity; FH: functional heartburn; BMI: body mass index.
Table 2.
Demographic characteristics compared among groups based on Rome III criteria (data presented as mean ± SD or N (%)).
| RE (N = 59) | NERD (N = 96) | FH (N = 78) | p value | |
|---|---|---|---|---|
| Male gender | 38 (64.41%) | 51 (53.13%) | 33 (42.31%) | 0.037a |
| Age (years) | 44.80 ± 12.60 | 43.53 ± 13.10 | 42.04 ± 13.23 | 0.446 |
| Weight (kg) | 65.69 ± 10.06 | 60.51 ± 10.64 | 57.02 ± 11.10 | 0.000a |
| BMI (kg/m2) | 24.04 ± 2.96 | 22.67 ± 3.31 | 21.90 ± 3.40 | 0.001a |
p < 0.05. RE: reflux esophagitis; NERD: non-erosive gastroesophageal reflux disease; FH: functional heartburn; BMI: body mass index.
Upper gastrointestinal endoscopy
All included patients underwent upper endoscopy examination before the esophageal function test. RE was demonstrated in 59 patients (25.32%), with grade A RE in 28 patients, grade B in 29 patients, and grades C and D in another two patients. A total of 174 patients were endoscopy negative.
High-resolution esophageal manometry
According to the updated Chicago classification of esophageal motility, 75 patients who had major motility disorders on HRM were excluded, with achalasia in eight patients, EGJ outflow obstruction in 58 patients, absent contractility in seven patients and distal esophageal spasm in two patients. Among the remaining 233 patients, 80 (34.33%) were found to have ineffective motility, two (0.86%) had fragmented contractions, and 151 (64.81%) were without motility disorders.
Twenty-four-hour MII-pH monitoring
Among the 59 RE patients, 22 (37.29%) had pathological reflux. Among the 174 endoscopy-negative patients, 28 (16.09%) had pathological reflux and were identified as NERD based on the Rome IV criteria. Among the remaining 146 patients (83.91%) with negative endoscopy and normal reflux, 36 (20.69%) had a positive SAP with 26 (14.94%) for acid reflux and 10 (5.75%) for non-acid reflux, while 110 patients (63.22%) had a negative SAP.
Phenotype diagnoses
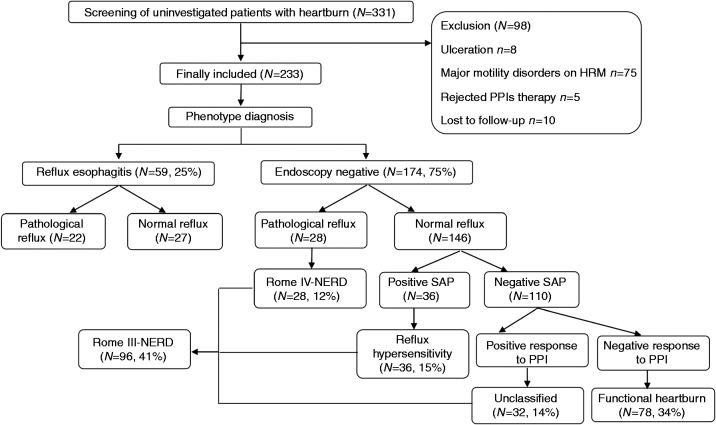
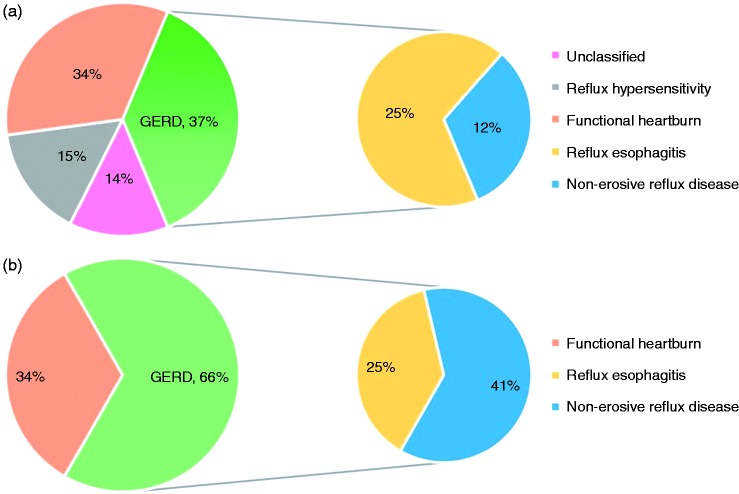
The study flow of clinical evaluation and the primary diagnosis of patients with heartburn based on the Rome IV and III criteria are shown in Figures 1 and 2. After clinical evaluation, 59 patients (25%) were diagnosed with RE, 96 patients (41%) with NERD, and 78 patients (34%) with FH based on the Rome III criteria. When the updated Rome IV criteria were applied, 68 patients (70.83%) out of 96 patients with Rome III-positive NRED were instead diagnosed with RH (N = 36, 15%) or were considered unclassified (N = 32, 14%). The proportion of real NERD dropped to 12%.
Figure 1.
The study flowchart of clinical evaluation based on the Rome IV and III criteria. HRM: high-resolution manometry; PPIs: proton pump inhibitors; NERD: non-erosive reflux disease; SAP: symptom association probability.
Figure 2.
The phenotypes of patients with heartburn. (a) The phenotypes of patients with heartburn based on the Rome IV criteria. (b) The phenotypes of patients with heartburn based on the Rome III criteria. GERD: gastroesophageal reflux disease.
Outcome assessment
All patients who were recruited underwent PPI treatment. The PPI treatment protocol among patients included esomeprazole, rabeprazole, omeprazole, lansoprazole, pantoprazole and ilaprazole with standard or double doses once or twice daily, and the treatment protocols were similar among the phenotype groups (see Supplementary Table 1). The PPI response rates of patients with RE, NERD and RH were 61.36%, 65% and 36.67%, respectively. All patients with FH were PPI non-responders, whereas all of the unclassified patients were PPI responders.
Comparison among different heartburn phenotypes
According to the Rome IV criteria, the gender, weight, body mass index (BMI), EGJ-CI and EGJ morphology were different among groups (Tables 1 and 3). Rome IV GERD patients were predominantly male and had higher BMI (p < 0.05). Furthermore, the FH and RH patients showed higher EGJ-CI and less hiatal hernias than Rome IV NERD and RE patients (all p < 0.05). The unclassified patients were predominantly male and had more hiatal hernias than did FH and RH patients (p < 0.05) (Tables 1 and 3). No significant differences in HRM parameters were observed among the RE and NERD patients, or between the FH and RH patients. Additionally, the unclassified group was similar to all other groups considered regarding other HRM parameters. Similar results were found among groups based on the Rome III criteria (Tables 2 and 4). The Rome III GERD patients were also predominantly male with higher BMI (p < 0.05). The RE patients showed weaker EGJ-CI (p < 0.05). However, significant differences were not observed in either EGJ-CI or other parameters between the Rome III NERD and FH patients (Tables 2 and 4, Figure 3(a) and (b)).
Table 3.
HRM parameters compared among groups based on Rome IV criteria (data presented as median (25th, 75th) or N (%)).
| RE (N = 59) | NERD (N = 28) | RH (N = 36) | FH (N = 78) | Unclassified (N = 32) | p value | |
|---|---|---|---|---|---|---|
| EGJ parameters | ||||||
| EGJ inspiratoryp (mmHg) | 18.00(14.00-23.00) | 16.00 (11.00–20.00) | 19.00 (14.00–28.00) | 17.00 (14.00–24.00) | 17.00 (14.00–26.00) | 0.320 |
| EGJ expiratoryp (mmHg) | 11.00(7.00-14.00) | 10.00 (5.00–14.00) | 12.00 (8.00–20.00) | 10.00 (7.00–15.00) | 10.00 (7.00–13.00) | 0.246 |
| EGJ-CI (mmHg*s*cm) | 30.45(17.65-38.85) | 23.30 (17.42–44.86) | 44.00 (30.05–62.13) | 38.73 (31.00–51.18) | 28.06 (16.21–51.04) | 0.000a |
| LES length (cm) | 3.70(3.10-4.30) | 3.60 (3.00–4.00) | 3.70 (3.10–4.10) | 3.80 (3.50–4.40) | 3.70 (3.10–4.30) | 0.635 |
| IRP-4s (mmHg) | 8.55(6.65-11.30) | 8.65 (5.70–9.90) | 8.55 (5.45–10.10) | 8.65 (6.30–11.65) | 8.30 (5.80–11.10) | 0.469 |
| EGJ morphology | ||||||
| Type I | 44 (74.58%) | 16 (57.14%) | 31 (86.11%) | 67 (85.90%) | 21 (65.63%) | 0.038a |
| Type II | 13 (22.03%) | 11 (39.29%) | 5 (13.89%) | 10 (12.82%) | 11 (34.37%) | |
| Type III | 2 (3.39%) | 1 (3.57%) | 0 (0.00%) | 1 (1.28%) | 0 (0.00%) | |
| Peristalsis parameters | ||||||
| Mean DL (s) | 6.29 (5.56–6.84) | 6.11 (5.18–6.88) | 6.50 (5.76–7.79) | 6.23 (5.58–7.11) | 6.04 (5.50–6.72) | 0.619 |
| Mean DCI (mmHg*s*cm) | 710.66 (343.01–1210.28) | 644.99 (287.93–1111.80) | 777.13 (307.13–1159.40) | 919.01 (423.27–1450.89) | 1024.95 (379.36–1353.10) | 0.267 |
| MRS-DCI (mmHg*s*cm) | 713.70 (276.00–1385.40) | 640.50 (178.90–1189.20) | 570.00 (128.35–2138.00) | 853.90 (363.80–1653.70) | 959.80 (456.20–2172.60) | 0.152 |
| MRS-DCI/Mean DCI | 1.09 (0.49–1.40) | 0.92 (0.45–1.41) | 1.15 (0.58–1.99) | 1.20 (0.67–1.74) | 1.32 (0.66-1.80) | 0.446 |
p < 0.05. RE: reflux esophagitis; NERD: non-erosive gastroesophageal reflux disease; RH: reflux hypersensitivity; FH: functional heartburn; EGJ: esophagogastric junction; LES: lower esophageal sphincter; EGJ inspiratoryp: EGJ inspiratory pressure; EGJ expiratoryp; EGJ expiratory pressure; IRP-4s: integrated 4 seconds relaxation pressure; DL: distal latency; DCI: distal contractile integral; MRS: multiple rapid swallow; s: seconds.
Table 4.
HRM parameters compared among groups based on Rome III criteria (data presented as median (25th,75th) or N (%)).
| RE (N = 59) | NERD (N = 96) | FH (N = 78) | p value | |
|---|---|---|---|---|
| EGJ parameters | ||||
| EGJ inspiratoryp (mmHg) | 18.00 (14.00–23.00) | 17.00 (13.00–25.00) | 18.00 (14.00–24.00) | 0.805 |
| EGJ expiratoryp (mmHg) | 11.00 (7.00–14.00) | 11.00 (7.00–17.00) | 10.00 (7.00–15.00) | 0.912 |
| EGJ-CI (mmHg*s*cm) | 30.45 (17.65–38.85) | 34.00 (21.00–51.45) | 38.73 (31.00–51.18) | 0.001a |
| LES length (cm) | 3.70 (3.10–4.30) | 3.70 (3.10–4.10) | 3.80 (3.50–4.40) | 0.343 |
| IRP-4 s (mmHg) | 8.55 (6.65–11.30) | 8.55 (5.75–10.45) | 8.65 (6.30–11.65) | 0.179 |
| EGJ morphology | ||||
| Type I | 44 (74.58%) | 68 (70.83%) | 67 (85.90%) | 0.119 |
| Type II | 13 (22.03%) | 27 (28.13%) | 10 (12.82%) | |
| Type III | 2 (3.39%) | 1 (1.04%) | 1 (1.28%) | |
| Peristalsis parameters | ||||
| Mean DL (s) | 6.29 (5.56–6.84) | 6.15 (5.50–6.98) | 6.23 (5.58–7.11) | 0.956 |
| Mean DCI (mmHg*s*cm) | 710.66 (343.01–1210.28) | 723.91 (308.47–1172.46) | 919.01 (423.27–1450.89) | 0.234 |
| MRS-DCI (mmHg*s*cm) | 713.70 (276.00–1385.40) | 681.50 (200.30–1920.60) | 853.90 (363.80–1653.70) | 0.468 |
| MRS-DCI/Mean DCI | 1.09 (0.49–1.40) | 1.16 (0.56–1.71) | 1.20 (0.67–1.74) | 0.598 |
p < 0.05. RE: reflux esophagitis; NERD: non-erosive gastroesophageal reflux disease; FH: functional heartburn; EGJ: esophagogastric junction; LES: lower esophageal sphincter; EGJ inspiratoryp: EGJ inspiratory pressure; EGJ expiratoryp: EGJ expiratory pressure; IRP-4s: integrated 4 seconds relaxation pressure; DL: distal latency; DCI: distal contractile integral; MRS: multiple rapid swallow; s: seconds.
Figure 3.
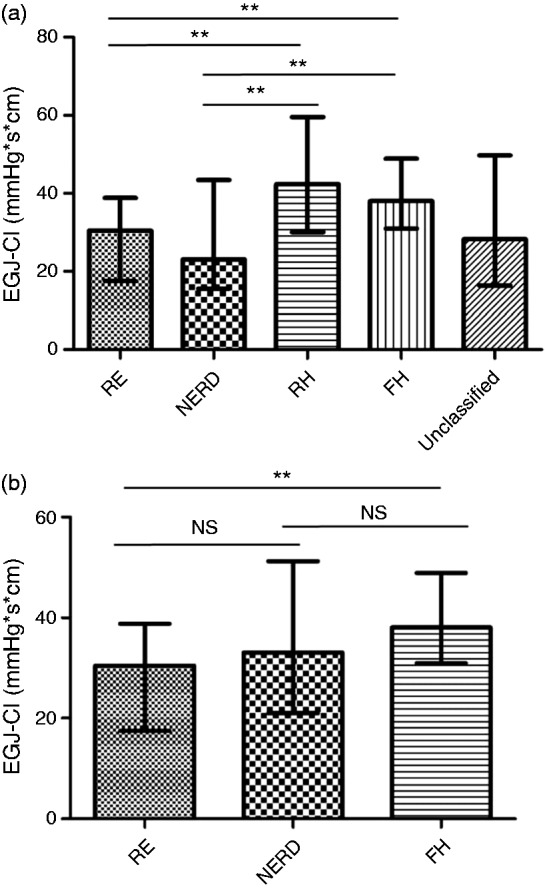
Comparison of esophagogastric junction-contractile integral (EGJ-CI) among patients with heartburn. (a) Comparison of EGJ-CI among patients with heartburn based on the Rome IV criteria. (b) Comparison of EGJ-CI among patients with heartburn based on the Rome III criteria. RE: reflux esophagitis; NERD: non-erosive reflux disease; RH: reflux hypersensitivity; FH: functional heartburn; NS: not significant; *p < 0.05; **, p < 0.01.
Discussion
Heartburn is a primary symptom of a cluster of functional diseases that derive from esophagus-brain interactions.13 Along with the launch of the Rome IV criteria, it became possible to classify heartburn patients into detailed categories, although the proportions of these phenotypes have remained unclear. The current study was not only the first study to test the utility of the Rome IV criteria among outpatients with heartburn but also the first study to compare the Rome III and Rome IV criteria for heartburn diagnosis in clinical practice. Our results demonstrated patients with heartburn had heterogeneous causes with less than 40% of patients with real GERD, among whom approximately 34% were FH and 15% were RH based on the Rome IV criteria. Additionally, application of the Rome IV criteria changed the diagnosis of nearly 71% of the Rome III-positive NERD patients to be RH or unclassified. The FH and RH patients showed better anti-reflux barrier competence than did the Rome IV NERD patients. However, approximately 14% of patients did not fit into the updated criteria.
Up to now, the epidemiology of different subgroups of heartburn patients has remained unclear. It has been revealed that 37%–60% of NERD patients have normal acid reflux, and the proportion of FH and RH can vary from less than 10% to 75% and to 36%, respectively.14–25 One factor that has contributed to the variation is the changing definitions of heartburn phenotypes. For example, the Rome III committee used to define those with normal reflux but positive symptom-reflux association as NERD, but these patients were then isolated as a single group named RH in the updated criteria. It has been revealed that RH is more likely to present with esophageal mucosal changes than FH.26 Furthermore, RH may respond less well than real NERD, so separating RH from real NERD and FH is of clinical significance.
The current study also focused on the motility characteristics of heartburn patients. We found that FH and RH patients showed higher EGJ-CI and fewer hiatal hernias than did the Rome IV NERD patients, which was more accordant with the pathophysiological features of NERD.24,27 However, no significant differences in EGJ-CI could be observed between the Rome III NERD and FH patients. Since the differences are present only in minor motor dysfunction with uncertain clinical relevance, these types of motor dysfunction cannot preclude a functional diagnosis. Even so, a weakened anti-reflux barrier was still the prominent characteristic of well-defined NERD when compared with functional disorders in the Rome IV criteria, which may further support the superiority of the Rome IV criteria over Rome III criteria.
It was worth noting that a group of heartburn patients with negative endoscopy and MII-pH results but an effective response to PPI who used to be defined as NERD in the Rome III criteria could not fit into the updated Rome criteria. The diagnosis of these patients is controversial since the role of the PPI response is now emphasized. Why such patients respond to acid suppression remains uncertain. The explanation could be partly due to the false-negative results of MII-pH testing with a reported sensitivity of 66.4%28 and the unreliability of symptom reports.29 Therefore, negative MII-pH testing results cannot rule out pathological reflux or positive symptom-reflux association, and some responders could have NERD or RH that was missed during diagnosis. To avoid false-negative MII-pH results and to reduce the diagnosis of unclassified patients, we could prolong recording periods beyond 48 and even 96 hours to increase the sensitivity of reflux detection, and Bravo would be a very good tool to accomplish this target. However, some experts doubt that the PPI response may result from the placebo effect, since some placebo-controlled clinical trials of functional gastrointestinal diseases have demonstrated that the placebo effect does exist.30 The current study put these patients into the unclassified category and found that they were predominantly male and had more hiatal hernias than did the FH and RH patients, which partly indicated a similar pathophysiological mode compared with NERD. However, further investigation of the weight of the PPI response still needs to be studied based on a larger population.
The current study also demonstrated that the PPI response rates of patients with RE, NERD and RH were 61.36%, 65% and 36.67%, respectively. Since NERD is well defined in the Rome IV criteria, PPI therapy was almost equally effective among patients with real NERD and RE in the current study, which was consistent with other previous studies.31 Excessive esophageal acid exposure is the main pathophysiological mechanism of real GERD, whereas visceral hypersensitivity is more prominent for RH and FH.32 This can explain, to some extent, the lower responsiveness of routine PPI treatment among RH and FH patients. Therefore, different treatment strategies using pain modulators after failure of first-step PPI therapy would be much more reasonable for patients with RH and FH due to the similar pathogenesis. Additionally, patients with RH and FH have different responses to PPIs, and RH patients may respond to PPIs, whereas FH patients do not.
There were some limitations in our study. First, the current study was a retrospective study, and therefore, the symptom evaluation and therapy efficacy evaluation have some bias. Thus, a prospective design would further clarify the phenotypes of heartburn patients. Second, the types of PPI therapy used varied, which made the therapy efficacy incomparable to some extent. However, the dosage and duration of the therapy was in line with the current recommended therapy for GERD. Third, some patients referred to our clinic had already been on PPI therapy during their first visit and were then not referred to esophageal function tests, therefore the current study could not include these patients. Furthermore, biopsies should be performed both in the distal and proximal esophagus to exclude eosinophilic esophagitis according to the guidelines. However, this was a retrospective study, and no more than one doctor performed the upper endoscopy for these included patients in our center. Lastly, since the symptom association analysis was generated by machine and was actually a secondary analysis, it could have been influenced by multiple factors, so the results should be analyzed with caution.
In conclusion, the Rome IV criteria were stricter in defining heartburn phenotypes, and superior in distinguishing NERD from FH and RH by HRM compared with the Rome III criteria. Recognition of the heterogeneous phenotypes of patients with heartburn will lead to more successful treatment and optimized medical resource utilization.
Supplemental Material
Supplemental Material for The Rome IV versus Rome III criteria for heartburn diagnosis: A comparative study by Mengyu Zhang, Minhu Chen, Sui Peng and Yinglian Xiao in United European Gastroenterology Journal
Acknowledgments
Author contributions are as follows: MZ: data acquisition and analysis, manuscript drafting; SP: data acquisition and analysis; MC and YX: study design, data analysis, finalizing and approving the manuscript.
Funding
This work was supported by grants from the National Natural Science Foundation of China (81400582) and the National Natural Science Foundation of China (81470817).
Declaration of conflicting interests
None declared.
Ethics approval
This study was approved by the Ethical Review Board of Sun Yat-sen University (date: April 15, 2010, number: (2010) 31). The study protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki.
Informed consent
Written informed consent was obtained from all participants.
References
- 1.Vakil N, van Zanten SV, Kahrilas P, et al. The Montreal definition and classification of gastroesophageal reflux disease: A global evidence-based consensus. Am J Gastroenterol 2006; 101: 1900–1920. quiz 1943. [DOI] [PubMed] [Google Scholar]
- 2.Cicala M, Emerenziani S, Guarino MP, et al. Proton pump inhibitor resistance, the real challenge in gastro-esophageal reflux disease. World J Gastroenterol 2013; 19: 6529–6535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sifrim D, Zerbib F. Diagnosis and management of patients with reflux symptoms refractory to proton pump inhibitors. Gut 2012; 61: 1340–1354. [DOI] [PubMed] [Google Scholar]
- 4.Fass R, Sifrim D. Management of heartburn not responding to proton pump inhibitors. Gut 2009; 58: 295–309. [DOI] [PubMed] [Google Scholar]
- 5.Galmiche JP, Clouse RE, Balint A, et al. Functional esophageal disorders. Gastroenterology 2006; 130: 1459–1465. [DOI] [PubMed] [Google Scholar]
- 6.Aziz Q, Fass R, Gyawali CP, et al. Functional esophageal disorders. Gastroenterology 2016; 150: 1368–1379. [DOI] [PubMed] [Google Scholar]
- 7.Suzuki H, Matsuzaki J, Okada S, et al. Validation of the GerdQ questionnaire for the management of gastro-oesophageal reflux disease in Japan. United European Gastroenterol J 2013; 1: 175–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lundell LR, Dent J, Bennett JR, et al. Endoscopic assessment of oesophagitis: Clinical and functional correlates and further validation of the Los Angeles classification. Gut 1999; 45: 172–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kahrilas PJ, Bredenoord AJ, Fox M, et al. The Chicago Classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil 2015; 27: 160–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nicodème F, Pipa-Muniz M, Khanna K, et al. Quantifying esophagogastric junction contractility with a novel HRM topographic metric, the EGJ-Contractile Integral: Normative values and preliminary evaluation in PPI non-responders. Neurogastroenterol Motil 2014; 26: 353–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shaker A, Stoikes N, Drapekin J, et al. Multiple rapid swallow responses during esophageal high-resolution manometry reflect esophageal body peristaltic reserve. Am J Gastroenterol 2013; 108: 1706–1712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shay S, Tutuian R, Sifrim D, et al. Twenty-four hour ambulatory simultaneous impedance and pH monitoring: A multicenter report of normal values from 60 healthy volunteers. Am J Gastroenterol 2004; 99: 1037–1043. [DOI] [PubMed] [Google Scholar]
- 13.Savarino E, Zentilin P, Savarino V. NERD: An umbrella term including heterogeneous subpopulations. Nat Rev Gastroenterol Hepatol 2013; 10: 371–380. [DOI] [PubMed] [Google Scholar]
- 14.Martinez SD, Malagon IB, Garewal HS, et al. Non-erosive reflux disease (NERD)—acid reflux and symptom patterns. Aliment Pharmacol Ther 2003; 17: 537–545. [DOI] [PubMed] [Google Scholar]
- 15.Kushnir VM, Sayuk GS, Gyawali CP. The effect of antisecretory therapy and study duration on ambulatory esophageal pH monitoring. Dig Dis Sci 2011; 56: 1412–1419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Savarino E, Tutuian R, Zentilin P, et al. Characteristics of reflux episodes and symptom association in patients with erosive esophagitis and nonerosive reflux disease: Study using combined impedance-pH off therapy. Am J Gastroenterol 2010; 105: 1053–1061. [DOI] [PubMed] [Google Scholar]
- 17.Savarino E, Zentilin P, Tutuian R, et al. Impedance-pH reflux patterns can differentiate non-erosive reflux disease from functional heartburn patients. J Gastroenterol 2012; 47: 159–168. [DOI] [PubMed] [Google Scholar]
- 18.Savarino E, Zentilin P, Tutuian R, et al. The role of nonacid reflux in NERD: Lessons learned from impedance-pH monitoring in 150 patients off therapy. Am J Gastroenterol 2008; 103: 2685–2693. [DOI] [PubMed] [Google Scholar]
- 19.Park EY, Choi MG, Baeg M, et al. The value of early wireless esophageal pH monitoring in diagnosing functional heartburn in refractory gastroesophageal reflux disease. Dig Dis Sci 2013; 58: 2933–2939. [DOI] [PubMed] [Google Scholar]
- 20.Zerbib F, Roman S, Ropert A, et al. Esophageal pH-impedance monitoring and symptom analysis in GERD: A study in patients off and on therapy. Am J Gastroenterol 2006; 101: 1956–1963. [DOI] [PubMed] [Google Scholar]
- 21.Savarino E, Marabotto E, Zentilin P, et al. The added value of impedance-pH monitoring to Rome III criteria in distinguishing functional heartburn from non-erosive reflux disease. Dig Liver Dis 2011; 43: 542–547. [DOI] [PubMed] [Google Scholar]
- 22.Zerbib F, Belhocine K, Simon M, et al. Clinical, but not oesophageal pH-impedance, profiles predict response to proton pump inhibitors in gastro-oesophageal reflux disease. Gut 2012; 61: 501–506. [DOI] [PubMed] [Google Scholar]
- 23.Frazzoni M, Conigliaro R, Mirante VG, et al. The added value of quantitative analysis of on-therapy impedance-pH parameters in distinguishing refractory non-erosive reflux disease from functional heartburn. Neurogastroenterol Motil 2012; 24: 141–146, e87. [DOI] [PubMed] [Google Scholar]
- 24.Frazzoni M, De Micheli E, Zentilin P, et al. Pathophysiological characteristics of patients with non-erosive reflux disease differ from those of patients with functional heartburn. Aliment Pharmacol Ther 2004; 20: 81–88. [DOI] [PubMed] [Google Scholar]
- 25.Mainie I, Tutuian R, Shay S, et al. Acid and non-acid reflux in patients with persistent symptoms despite acid suppressive therapy: A multicentre study using combined ambulatory impedance-pH monitoring. Gut 2006; 55: 1398–1402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Savarino E, Zentilin P, Mastracci L, et al. Microscopic esophagitis distinguishes patients with non-erosive reflux disease from those with functional heartburn. J Gastroenterol 2013; 48: 473–482. [DOI] [PubMed] [Google Scholar]
- 27.Savarino E, Gemignani L, Pohl D, et al. Oesophageal motility and bolus transit abnormalities increase in parallel with the severity of gastro-oesophageal reflux disease. Aliment Pharmacol Ther 2011; 34: 476–486. [DOI] [PubMed] [Google Scholar]
- 28.Zhou LY, Wang Y, Lu JJ, et al. Accuracy of diagnosing gastroesophageal reflux disease by GerdQ, esophageal impedance monitoring and histology. J Dig Dis 2014; 15: 230–238. [DOI] [PubMed] [Google Scholar]
- 29.Kavitt RT, Higginbotham T, Slaughter JC, et al. Symptom reports are not reliable during ambulatory reflux monitoring. Am J Gastroenterol 2012; 107: 1826–1832. [DOI] [PubMed] [Google Scholar]
- 30.Enck P, Horing B, Weimer K, et al. Placebo responses and placebo effects in functional bowel disorders. Eur J Gastroenterol Hepatol 2012; 24: 1–8. [DOI] [PubMed] [Google Scholar]
- 31.Weijenborg PW, Cremonini F, Smout AJ, et al. PPI therapy is equally effective in well-defined non-erosive reflux disease and in reflux esophagitis: A meta-analysis. Neurogastroenterol Motil 2012; 24: 747–757, e350. [DOI] [PubMed] [Google Scholar]
- 32.Knowles CH, Aziz Q. Basic and clinical aspects of gastrointestinal pain. Pain 2009; 141: 191–209. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material for The Rome IV versus Rome III criteria for heartburn diagnosis: A comparative study by Mengyu Zhang, Minhu Chen, Sui Peng and Yinglian Xiao in United European Gastroenterology Journal