Abstract
Periostin (POSTN) secreted by intrahepatic cholangiocarcinoma stem cells (ICSCs) serves important roles in promoting tumor progression. The present study aimed to investigate POSTN-recruited tumor-associated macrophages (TAMs) in intrahepatic cholangiocarcinoma (ICC). A total of 50 cases were used to investigate the distribution of ICSCs and TAMs in ICC. HCCC-9810 cells were sorted by cluster of differentiation (CD)44, the expression of POSTN of CD44+ (cancer stem cells) and CD44− cells (non-cancer stem cells), and medium were evaluated by western blot analysis. HCCC-9810 cells and THP-1 macrophages were used to detect the effects of POSTN on recruiting TAMs in vitro. The present study revealed that CD44+ cells in ICC tissues and the HCCC-9810 cell line were associated with high POSTN secretion levels. Furthermore, POSTN was associated with TAM density in primary ICC tissues. Additionally, POSTN increased the migration of TAMs derived from THP-1 cells. These findings suggested that POSTN secreted by ICSCs may serve important functions in TAM recruitment, and it may be a potential curative strategy to target the tumor microenvironment in ICC.
Keywords: intrahepatic cholangiocarcinoma, tumor-associated macrophages, periostin, migration, cancer stem cells
Introduction
Intrahepatic cholangiocarcinoma (ICC) is the second most common type of malignant primary hepatic tumor in numerous areas of the world, including North America, Europe, Australia, and Japan (1). ICC is a type of malignant tumor that originates from peripheral intrahepatic biliary epithelia (2,3). The incidence of ICC and the ICC-associated mortality rate has increased in several regions around the world since the 1970s (4–6). Cancer stem cells (CSCs) are defined as a small subgroup of cancer cells with the ability of self-renewal that may lead to tumor recurrence. A number of studies have suggested that CSCs lead to poor prognosis by promoting tumor recurrence and metastasis (7–9). It has previously been reported that the maintenance of CSC characteristics depends on the tumor microenvironment (TME) (10). The TME consists of tumor cells and stromal cells, including mesenchymal cells, endothelial cells and immune cells, and serves an important role in regulating tumorigenesis, cell invasion and metastasis (11).
Macrophages, a main component of tumor-infiltrating immunocytes, infiltrate a variety of cytokines, chemokines, growth factors and matrix metalloproteases, and contribute to tumor progression and recurrence (12,13). Macrophages are classified into M1 and M2 subtypes due to their polarization manners (14). The M1 subtype appears to be tumor suppressive, whereas the M2 subtype is tumor supportive in tumors (15). M2 subtype macrophages upregulate cluster of differentiation (CD)206, tumor growth factor-β and interleukin-10 (16). Macrophages that invade the TME are tumor-associated macrophages (TAMs), expressing similar molecular and functional characteristic of the M2 subtype (12). Abundant macrophage infiltration is a histological feature of ICC, and those macrophages in ICC express similar functional characteristics to the M2 subtype; furthermore, the increased density of macrophages in ICC was associated with a poor prognosis (17). Certain studies have demonstrated that a high density of TAMs was associated with poor prognosis in numerous other types of cancer (18,19). Therefore, researching the molecular mechanisms underlying TAM recruitment may promote the development of therapeutics to effectively improve ICC treatment.
Periostin (POSTN), also known as OSF-2, is a member of the fasciclin family and is a disulfide-linked cell adhesion protein (20). POSTN participates in the multifarious field of tumorigenic processes via signaling pathways, including protein kinase B/phosphoinositide-3 kinase, integrin and Wnt-1 (21,22). Zhou et al (23), revealed that POSTN secreted by stem cells may serve as a chemoattractant for recruiting M2 TAMs in clinical specimens and in an animal model of glioblastoma. In addition, POSTN acts as an important promoter in tumor progression, including growth, angiogenesis, metastasis and invasion, in certain types of malignant cancer (22,24,25). The present study demonstrated that CD44+ ICC stem cells secrete POSTN, and the density of CD206+ TAMs was associated with the expression level of POSTN in ICC.
Materials and methods
Patients and specimens
A total of 50 patients (age, 43–75 years; median age, 59.8 years; 32 males and 18 females) with curative liver resection and pathology-proven ICC at the Hunan Provincial People's Hospital (Changsha, China) between May 2001 and February 2007 were included in the current study. Tumor stage was re-examined according to the 2009 International Union Against Cancer TNM Classification system (26). The present study was approved by the Hunan Provincial People's Hospital Research Ethics Committee. Written informed consent was obtained from all patients prior to enrollment in the present study.
Immunohistochemical examination
For immunohistochemical analysis of POSTN (TA804575; 1:100; OriGene Technologies, Inc., Beijing, China) and CD206 (SC-376232; 1:100; Santa Cruz Biotechnology, Inc., Dallas, TX, USA), tissue sections (thickness=4 mm) were deparaffinized in 100% xylene and rehydrated in graded concentrations (100, 95, 70 and 50%) of ethanol. Following incubation with 1% bovine serum albumin (BSA; Beijing Dingguo Changsheng Biotechnology Co., Ltd., Beijing, China) in PBS (pH 7.4) at 37°C for 30 min, the tissue sections were then incubated with primary antibody for 1 h at room temperature, followed by incubation with the secondary biotinylated mouse antibody (TA130008; 1:100; OriGene Technologies, Inc., Beijing, China) at 37°C for 30 min. Following PBS washing, tissue sections were subsequently treated with streptavidin-peroxidase (S5512; Sigma Aldrich; Merck KgaA, Darmstadt, Germany) at 37°C for 30 min. Finally, the results were visualized following a 15-min incubation with diaminobenzidine (DAB; Beyotime Institute of Biotechnology, Haimen, China) at room temperature for 5 min. Horseradish peroxidase was detected using 3,3′-diaminobenzidine (Phoenix Biotechnologies, San Antonio, TX, USA) substrate for 5 min, washed with distilled water, and counterstained with Gill's no. 3 hematoxylin (Sigma-Aldrich; Merck KGaA) at room temperature for 15 sec and mounted. The results were observed under a light microscope (IX51; Olympus Corporation, Tokyo, Japan; magnification, ×100).
Immunofluorescent staining
For immunohistochemical analysis of POSTN (TA500070; 1:100; OriGene Technologies, Inc.), CD44 (ab51037; 1:100; Abcam, Cambridge, UK) and CD206 (SC-34577; 1:100; Santa Cruz Biotechnology, Inc.), tissue sections were prepared as aforementioned. The sections were then incubated with primary antibody for 1 h at room temperature. The secondary biotinylated [goat anti-mouse IgG (ab150117; 1:100; Abcam), donkey anti-goat IgG (ab150079; 1:100; Abcam), donkey anti-mouse IgG (ab150131; 1:100; Abcam), Goat anti-mouse IgG (ab150129; 1:100; Abcam)] antibody was applied for identifying primary antibody and incubated at 37°C for 30 min. The nuclei were counterstained at room temperature for 10 min with 4′,6-diamidino-2-phenylindole (Sigma-Aldrich; Merck KGaA). The results were observed and representative images were captured using an inverted fluorescent microscope (BX41, Olympus Corporation, Tokyo, Japan) (magnification, ×100 and ×200).
Cell cultures and cell sorting
HCCC-9810 and THP-1 cells from the Cell Bank of Shanghai Institute of Biological Sciences (Shanghai, China) were cultured in RPMI-1640 medium (Gibco; Thermo Fisher Scientific, Inc., Waltham, MA, USA) supplemented with 10% fetal bovine serum (FBS; GE Healthcare, Chicago, IL, USA), 100 U/ml penicillin and 100 µg/ml streptomycin. Cells were incubated in stem cell medium with B27 (Gibco, Thermo Fisher Scientific, Inc.), 10 ng/ml epidermal growth factor (Prospec-Tany TechnoGene, Ltd., East Brunswick, NJ, USA) and basic fibroblast growth factor (Prospec-Tany TechnoGene, Ltd.) supplement at 37°C for 12 h to expose surface markers, and samples were sorted using a BD FACSVantage SE (BD Biosciences, Franklin Lakes, NJ, USA). Phycoerythrin (PE)-conjugated anti-human CD44 antibody (130-095-194; 1:10; Miltenyi Biotec, Cologne, Germany) was used to label HCCC-9810 cells according to the manufacturer's instructions. CD44+ and CD44− cell subpopulations were sorted by fluorescence-activated cell sorting with anti-REA (130-104-693; Miltenyi Biotec, Cologne, Germany). The purity of sorted cells was evaluated using a FACSCalibur™ flow cytometry system (BD Biosciences) and analyzed using flow cytometry on the MACSQuant Analyzer 10. CD44+ cells were enriched with stem cell medium and sorted as stem cells; similarly, CD44¯ cells were used as non-stem cells. All sorted cells were cultured in RPMI-1640 supplemented with 15% FBS at 37°C for a week. THP-1 cells were treated with phorbol-12-myristate-13-acetate at 100 ng/ml for 48 h to generate macrophages.
Western blot analysis
HCCC-9810 cells were lysed using lysis buffer containing 1 mM phenylmethanesulfonyl-fluoride (ST506; Beyotime, Shanghai, China) on ice for 5 min, then total protein of HCCC-9810 and supernatant content was evaluated using a bicinchoninic acid quantitative kit. Quantified protein lysates (5 µg per lane) were resolved using SDS-PAGE (7.5% gels), transferred onto a polyvinylidene difluoride membrane (EMD Millipore, Billerica, MA, USA). The membrane was blocked with 5% non-fat milk in TBS with Tween 20 for 30 min at 25°C and immunoblotted with primary antibodies against POSTN (TA500070; 1:500; OriGene Technologies, Inc., Beijing, China) at 4°C overnight. Following this, the membrane was incubated with horseradish peroxidase-conjugated secondary antibody (ab6789; 1:4,000; Abcam) at 4°C overnight. The blots were visualized using an enhanced chemiluminescence kit (Vazyme, Piscataway, NJ, USA). β-actin (ab13822; 1:1,000; Abcam) was used as a loading control at 4°C overnight. Protein was visualized using FluorChem FC3 (ProteinSimple, San Jose, CA, USA) and ImageJ software (version 1.51p; National Institutes of Health, Bethesda, MD, USA) quantified the band density.
Cell migration assays
Transwell chamber assays were used to compare the migratory ability of THP-1-derived macrophages using conditional medium (CM) [NSCCs CM, ICSCs CM, ICSCs CM with POSTN-neutralizing antibody (α-POSTN) and IgG, NSCCs CM with recombinant POSTN (rPOSTN)]. Briefly, phorbol-12-myristate-13-acetate (PMA) treated THP-1-derived macrophages were resuspended in serum-free RPMI-1640 (5×104 cells/200 µl). BSA (2%)-RPMI-1640 (500 µl) was added to the upper chambers as the control. Conditioned medium [CM; NSCCs CM, ICSCs CM, ICSCs CM with α-POSTN (10 µg/ml; cat no. TA600528; OriGene Technologies, Inc., Beijing, China) or IgG and NSCCs CM with rPOSTN (0.2 µg/ml)] with 10% FBS was added to the lower chambers. Following a 24-h incubation at 37°C, the migratory cells to the lower surface of the membrane were fixed with 4% paraformaldehyde at room temperature for 5 min, stained with Wright Giemsa for 20 min at room temperature, and counted and imaged using a microscope (BX41; Olympus Corporation, Tokyo, Japan; magnification, ×400).
Statistical analysis
Data were presented as the mean ± standard error of the mean from at least three samples or experiments per data point. Differences between the groups were analyzed by one-way analysis of variance with Fisher's Least Significant Difference test as a post-hoc using SPSS version 15.0 (SPSS, Inc., Chicago, IL, USA). P<0.05 was considered to indicate a statistically significant difference.
Results
POSTN is secreted by ICSCs in ICC tissues and HCCC-9810 cells
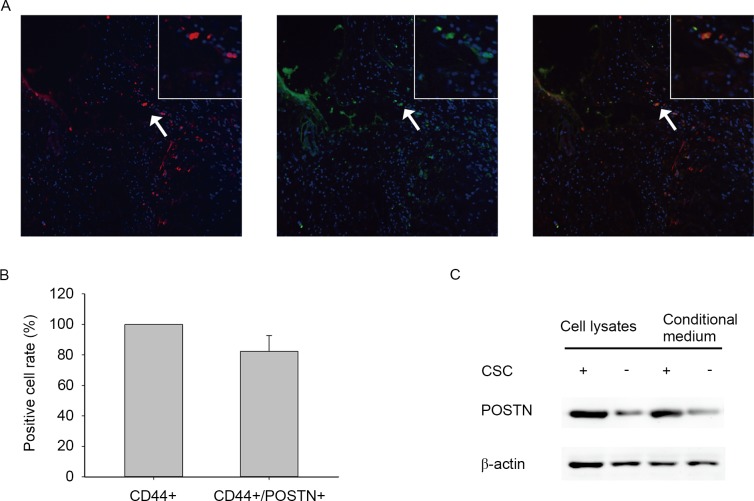
To investigate the latency association between POSTN expression and distribution of CSCs in cholangiocarcinoma, the present study determined the expression levels of POSTN and CSC marker CD44 in human primary ICC samples by evaluating immunofluorescence. The findings revealed that POSTN is preferentially expressed by CD44+ cancer cells and located in the area around ICSCs (Fig. 1A and B). To determine the differential expression of POSTN between ICSCs and non-stem cancer cells (NSCCs), the present study examined the expression levels of POSTN in ICSCs and NSCCs of the HCCC-9810 cell line by western blot analysis (Fig. 1C). The results demonstrated that ICSCs expressed higher levels of POSTN compared with NSCCs. Furthermore, ICSC conditioned medium also contained higher POSTN protein levels compared with matched NSCC conditioned medium (Fig. 1C). These results suggest that POSTN is preferentially secreted by ICSCs.
Figure 1.
POSTN is secreted by ICSCs in ICC tissues and HCCC-9810 cells. (A) Expression levels of ICSC marker CD44 (red), POSTN (green) and merged (yellow), were observed by immunofluorescent staining in human primary ICC tissues (magnification, ×100) and magnified area (arrow). (B) Graphical analysis of (A) identifying that >80% of cells were co-stained with CD44 and POSTN. (C) Western blot analysis of POSTN expression in cells and CM. Compared with non-stem cancer cells, CSC lysates and medium revealed POSTN overexpression. POSTN, periostin; ICSC, intrahepatic cholangiocarcinoma stem cells; ICC, intrahepatic cholangiocarcinoma; CD, cluster of differentiation; CSC, cancer stem cell.
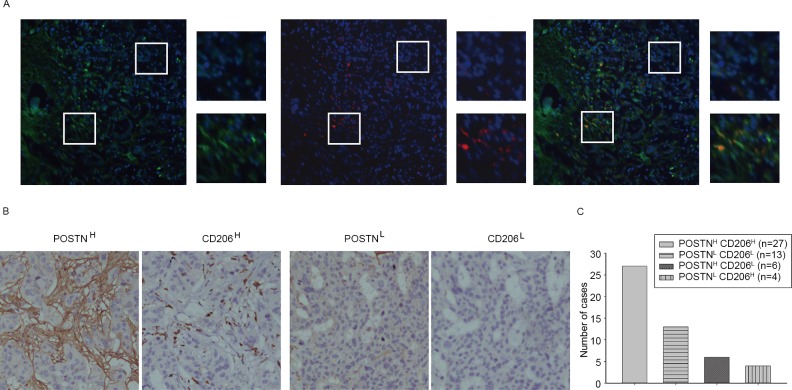
POSTN is associated with TAM density in primary ICC
The association between POSTN expression level and TAM density was first evaluated by immunofluorescence. The results demonstrated that TAM-labeled marker (CD206) was accumulated in a POSTN-abundant location (Fig. 2A). Immunohistochemistry demonstrated that high levels of POSTN and high levels of TAM markers were identified in ICC (Fig. 2B and C). These results suggest that POSTN expression levels had a positive association with the number of TAMs in ICC.
Figure 2.
POSTN is associated with TAM density in primary ICC. (A) Representative immunofluorescence images showing POSTN (green) and TAM marker CD206 (red) expression in ICC tissues (magnification, ×200) and selected areas (magnification, ×200). (B) Representative immunohistochemical images showing POSTN and CD206 staining (magnification, ×200). (C) A total of 54% of ICC cases presented POSTNH and CD206H staining, and 26% of ICC cases presented POSTNL and CD206L staining; however, 12% of ICC cases presented POSTNH and CD206L staining, and 8% of ICC cases presented POSTNL and CD206H staining. The majority (80%) of ICC cases revealed that POSTN expression was positively associated with TAM density. POSTN, periostin; TAM, tumor-associated macrophage; ICC, intrahepatic cholangiocarcinoma; CD, cluster of differentiation; H, high level; L, low level.
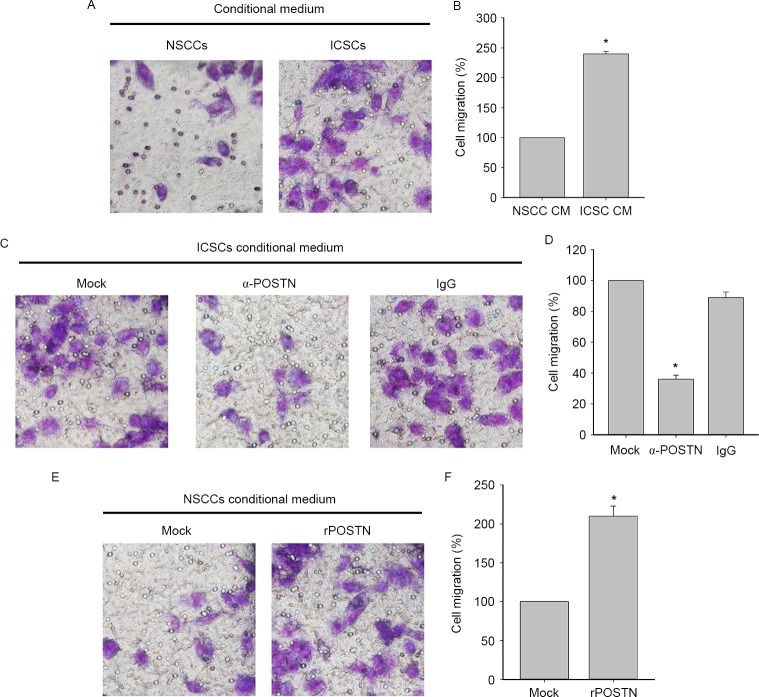
POSTN promotes migratory ability of TAMs derived from human macrophage-like THP-1 cells
To clarify the mechanism underlying POSTN action as an effective ICSC-secreted chemotaxin, migration of PMA-primed macrophage-like THP-1 cells were evaluated by Transwell assays. Conditioned medium from ICSCs attracted significantly more TAMs than the medium from matched NSCCs (Fig. 3A and B). Subsequently, the present study used α-POSTN to deplete POSTN expression. As presented in Fig. 3C and D, the depletion of POSTN in ICSC-CM suppressed the promoting effect of macrophage migration in vitro. The capacity of POSTN to increase invasiveness of human monocytes was also demonstrated in the present study (Fig. 3E and F). Collectively, these results demonstrate that POSTN preferentially secreted by ICSCs had an effective capacity to attract macrophages.
Figure 3.
POSTN promotes the migration of TAMs. (A) Transwell assay showing comparison of TAMs migration toward CM from NSCCs and ICSCs in HCCC-9810 cells (magnification, ×400) and (B) the graphical analysis. Data are presented as mean ± SD (n=3). *P<0.05, migrated TAMs towards ICSC CM vs. NSCC CM. The analysis identified that the increased TAMs cell migration toward ISCCs CM relative to NCSCs CM. (C) Comparison of TAMs migration toward ICSC CM or following treatment with anti-POSTN (10 µg/ml) antibody or IgG (magnification, ×400) and (D) its graphical analysis. Data are presented as mean ± SD (n=3). *P<0.05, migrated TAMs towards to α-POSTN ICSC CM vs. ICSC CM and IgG ICSC CM. (E) Comparison of invading TAMs toward NSCC CM or following treatment with rPOSTN (0.2 µg/ml) or IgG (magnification, ×400) and the (F) graphical analysis. Data are presented as mean ± SD (n=3). *P<0.05, migrated TAMs towards to rPOSTN NSCC CM vs. NSCC CM. POSTN, periostin; TAM, tumor-associated macrophage; NSCCs, non-stem cancer cells; ICSCs, intrahepatic cholangiocarcinoma stem cells; IgG, immunoglobulin G; r, recombinant; CM, conditional medium; SD, standard deviation; Ig, immunoglobulin.
Discussion
The present study observed a large level of CD206+ macrophage infiltration in parts of the ICC tumor niche. TAMs in cancerous tissues are regarded as immunosuppressive cells that have a tumor supportive role (27). Therefore, investigating the molecular mechanisms underlying TAM recruitment may contribute to improvement of ICC treatment.
It has been reported that tumors recruit TAMs by secreting the CC chemokine ligand 2 and soluble colony-stimulating factor 1 in tumors (28–30). The present study revealed that TAMs were concentrated in POSTN-abundant regions in ICCs. Similarly, immunohistochemistry analysis demonstrated the following: In ICC, tumor tissues with higher expression levels of POSTN contained higher densities of TAMs, revealing a positive association between POSTN levels and TAM density in human ICCs. The present study also revealed that POSTN was secreted by ICSCs. In order to determine the differential expression of POSTN in CD44+ ICSCs, the present study observed the expression of POSTN in matched ICSCs and NSCCs. These results demonstrated that ICSCs preferentially expressed markedly higher POSTN levels compared with NSCCs. Consistently, CM from ICSCs contained higher levels of POSTN protein compared with that from matched NSCCs. These results indicated that POSTN was preferentially produced by ICSCs rather than NSCCs.
To further elucidate whether ICSCs secreting POSTN had potent capacity to recruit TAMs, cell migration assays were performed in vitro. The Transwell assay identified that TAMs of the CM group had higher migratory ability compared with the NSCCs group. The present study also revealed the migratory ability of the CM group with anti-POSTN antibody exhibited a decreased migratory ability. Subsequently, the present study demonstrated that the migratory ability of NSCCs was increased by rPOSTN. These results revealed that POSTN preferentially secreted by ICSCs displays potent ability to attract TAMs.
Trabectedin has demonstrated antitumor activity by targeting TAMs (31). The present study revealed that the underlying mechanisms of TAM recruitment by ICSC-secreted POSTN may be responsible for the crosstalk of TAMs and ICSCs. In addition, therapeutic targeting of the immune TME may synergize with current immunotherapies to effectively increase survival of ICC patients.
Acknowledgements
The present study was supported by the Project of the National Natural Science Foundation of China (grant no. 81001107), the Project of the Scientific Research Fund of Hunan Provincial Education Department (grant no. 15A114) and the Project of Scientific Research Fund of Hunan Science and Technology Education Department (grant no. 2015SK2050).
References
- 1.Goodman ZD. Neoplasms of the liver. Mod Pathol. 2007;20:S49–S60. doi: 10.1038/modpathol.3800682. [DOI] [PubMed] [Google Scholar]
- 2.Nakanuma Y, Harada K, Ishikawa A, Zen Y, Sasaki M. Anatomic and molecular pathology of intrahepatic cholangiocarcinoma. J Hepatobiliary Pancreat Surg. 2003;10:265–281. doi: 10.1007/s00534-002-0729-3. [DOI] [PubMed] [Google Scholar]
- 3.Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics, 2002. CA Cancer J Clin. 2005;55:74–108. doi: 10.3322/canjclin.55.2.74. [DOI] [PubMed] [Google Scholar]
- 4.Okuno M, Ebata T, Yokoyama Y, Igami T, Sugawara G, Mizuno T, Yamaguchi J, Nagino M. Appraisal of inflammation-based prognostic scores in patients with unresectable perihilar cholangiocarcinoma. J Hepatobiliary Pancreat Sci. 2016;23:636–642. doi: 10.1002/jhbp.386. [DOI] [PubMed] [Google Scholar]
- 5.Shaib Y, El-Serag HB. The epidemiology of cholangiocarcinoma. Semin Liver Dis. 2004;24:115–125. doi: 10.1055/s-2004-828889. [DOI] [PubMed] [Google Scholar]
- 6.Patel T. Worldwide trends in mortality from biliary tract malignancies. BMC Cancer. 2002;2:10. doi: 10.1186/1471-2407-2-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sun YF, Xu Y, Yang XR, Guo W, Zhang X, Qiu SJ, Shi RY, Hu B, Zhou J, Fan J. Circulating stem cell-like epithelial cell adhesion molecule-positive tumor cells indicate poor prognosis of hepatocellular carcinoma after curative resection. Hepatology. 2013;57:1458–1468. doi: 10.1002/hep.26151. [DOI] [PubMed] [Google Scholar]
- 8.Chiba T, Zheng YW, Kita K, Yokosuka O, Saisho H, Onodera M, Miyoshi H, Nakano M, Zen Y, Nakanuma Y, et al. Enhanced self-renewal capability in hepatic stem/progenitor cells drives cancer initiation. Gastroenterology. 2007;133:937–950. doi: 10.1053/j.gastro.2007.06.016. [DOI] [PubMed] [Google Scholar]
- 9.Wu XZ, Yu XH. Bone marrow cells: The source of hepatocellular carcinoma? Med Hypotheses. 2007;69:36–42. doi: 10.1016/j.mehy.2006.10.064. [DOI] [PubMed] [Google Scholar]
- 10.Borovski T, De Sousa E, Melo F, Vermeulen L, Medema JP. Cancer stem cell niche: The place to be. Cancer Res. 2011;71:634–639. doi: 10.1158/0008-5472.CAN-10-3220. [DOI] [PubMed] [Google Scholar]
- 11.Schiavoni G, Gabriele L, Mattei F. The tumor microenvironment: A pitch for multiple players. Front Oncol. 2013;3:90. doi: 10.3389/fonc.2013.00090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Biswas SK, Allavena P, Mantovani A. Tumor-associated macrophages: Functional diversity, clinical significance, and open questions. Semin Immunopathol. 2013;35:585–600. doi: 10.1007/s00281-013-0367-7. [DOI] [PubMed] [Google Scholar]
- 13.Cook J, Hagemann T. Tumour-associated macrophages and cancer. Curr Opin Pharmacol. 2013;13:595–601. doi: 10.1016/j.coph.2013.05.017. [DOI] [PubMed] [Google Scholar]
- 14.Sielska M, Przanowski P, Wylot B, Gabrusiewicz K, Maleszewska M, Kijewska M, Zawadzka M, Kucharska J, Vinnakota K, Kettenmann H, et al. Distinct roles of CSF family cytokines in macrophage infiltration and activation in glioma progression and injury response. J Pathol. 2013;230:310–321. doi: 10.1002/path.4192. [DOI] [PubMed] [Google Scholar]
- 15.Staudt ND, Jo M, Hu J, Bristow JM, Pizzo DP, Gaultier A, VandenBerg SR, Gonias SL. Myeloid cell receptor LRP1/CD91 regulates monocyte recruitment and angiogenesis in tumors. Cancer Res. 2013;73:3902–3912. doi: 10.1158/0008-5472.CAN-12-4233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhang G, Guo L, Yang C, Liu Y, He Y, Du Y, Wang W, Gao F. A novel role of breast cancer-derived hyaluronan on inducement of M2-like tumor-associated macrophages formation. Oncoimmunology. 2016;5:e1172154. doi: 10.1080/2162402X.2016.1172154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Oishi K, Sakaguchi T, Baba S, Suzuki S, Konno H. Macrophage density and macrophage colony-stimulating factor expression predict the postoperative prognosis in patients with intrahepatic cholangiocarcinoma. Surg Today. 2015;45:715–722. doi: 10.1007/s00595-014-0989-y. [DOI] [PubMed] [Google Scholar]
- 18.Mantovani A, Sica A. Macrophages, innate immunity and cancer: Balance, tolerance, and diversity. Curr Opin Immunol. 2010;22:231–237. doi: 10.1016/j.coi.2010.01.009. [DOI] [PubMed] [Google Scholar]
- 19.Liu JY, Yang XJ, Geng XF, Huang CQ, Yu Y, Li Y. Prognostic significance of tumor-associated macrophages density in gastric cancer: A systemic review and meta-analysis. Minerva Med. 2016;107:314–321. [PubMed] [Google Scholar]
- 20.Bao S, Ouyang G, Bai X, Huang Z, Ma C, Liu M, Shao R, Anderson RM, Rich JN, Wang XF. Periostin potently promotes metastatic growth of colon cancer by augmenting cell survival via the Akt/PKB pathway. Cancer Cell. 2004;5:329–339. doi: 10.1016/S1535-6108(04)00081-9. [DOI] [PubMed] [Google Scholar]
- 21.Baril P, Gangeswaran R, Mahon PC, Caulee K, Kocher HM, Harada T, Zhu M, Kalthoff H, Crnogorac-Jurcevic T, Lemoine NR. Periostin promotes invasiveness and resistance of pancreatic cancer cells to hypoxia-induced cell death: Role of the beta4 integrin and the PI3k pathway. Oncogene. 2007;26:2082–2094. doi: 10.1038/sj.onc.1210009. [DOI] [PubMed] [Google Scholar]
- 22.Malanchi I, Santamaria-Martínez A, Susanto E, Peng H, Lehr HA, Delaloye JF, Huelsken J. Interactions between cancer stem cells and their niche govern metastatic colonization. Nature. 2011;481:85–89. doi: 10.1038/nature10694. [DOI] [PubMed] [Google Scholar]
- 23.Zhou W, Ke SQ, Huang Z, Flavahan W, Fang X, Paul J, Wu L, Sloan AE, McLendon RE, Li X, et al. Periostin secreted by glioblastoma stem cells recruits M2 tumour-associated macrophages and promotes malignant growth. Nat Cell Biol. 2015;17:170–182. doi: 10.1038/ncb3090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Michaylira CZ, Wong GS, Miller CG, Gutierrez CM, Nakagawa H, Hammond R, Klein-Szanto AJ, Lee JS, Kim SB, Herlyn M, et al. Periostin, a cell adhesion molecule, facilitates invasion in the tumor microenvironment and annotates a novel tumor-invasive signature in esophageal cancer. Cancer Res. 2010;70:5281–5292. doi: 10.1158/0008-5472.CAN-10-0704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Liu Y, Li F, Gao F, Xing L, Qin P, Liang X, Zhang J, Qiao X, Lin L, Zhao Q, Du L. Periostin promotes tumor angiogenesis in pancreatic cancer via Erk/VEGF signaling. Oncotarget. 2016;7:40148–40159. doi: 10.18632/oncotarget.9512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nathan H, Aloia TA, Vauthey JN, Abdalla EK, Zhu AX, Schulick RD, Choti MA, Pawlik TM. A proposed staging system for intrahepatic cholangiocarcinoma. Ann Surg Oncol. 2009;16:14–22. doi: 10.1245/s10434-008-0180-z. [DOI] [PubMed] [Google Scholar]
- 27.Mantovani A, Sica A, Sozzani S, Allavena P, Vecchi A, Locati M. The chemokine system in diverse forms of macrophage activation and polarization. Trends Immunol. 2004;25:677–686. doi: 10.1016/j.it.2004.09.015. [DOI] [PubMed] [Google Scholar]
- 28.Popivanova BK, Kostadinova FI, Furuichi K, Shamekh MM, Kondo T, Wada T, Egashira K, Mukaida N. Blockade of a chemokine, CCL2, reduces chronic colitis-associated carcinogenesis in mice. Cancer Res. 2009;69:7884–7892. doi: 10.1158/0008-5472.CAN-09-1451. [DOI] [PubMed] [Google Scholar]
- 29.Qian BZ, Li J, Zhang H, Kitamura T, Zhang J, Campion LR, Kaiser EA, Snyder LA, Pollard JW. CCL2 recruits inflammatory monocytes to facilitate breast-tumour metastasis. Nature. 2011;475:222–225. doi: 10.1038/nature10138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pyonteck SM, Gadea BB, Wang HW, Gocheva V, Hunter KE, Tang LH, Joyce JA. Deficiency of the macrophage growth factor CSF-1 disrupts pancreatic neuroendocrine tumor development. Oncogene. 2012;31:1459–1467. doi: 10.1038/onc.2011.337. [DOI] [PubMed] [Google Scholar]
- 31.Germano G, Frapolli R, Belgiovine C, Anselmo A, Pesce S, Liguori M, Erba E, Uboldi S, Zucchetti M, Pasqualini F, et al. Role of macrophage targeting in the antitumor activity of trabectedin. Cancer Cell. 2013;23:249–262. doi: 10.1016/j.ccr.2013.01.008. [DOI] [PubMed] [Google Scholar]