Abstract
Monitoring and audits are two distinct processes that ensure that the rights and safety of the participants are protected, and data integrity is maintained. The present narrative summates authors' experiences with monitoring and audits by sponsor along with challenges faced by the site. It also offers potential solutions for challenges faced during the process of monitoring and audits. It is important to remember that no monitoring or audit can ever substitute for a well-designed and articulated protocol. In addition, a determined approach by the investigator and his/her team to ensure that all aspects of the protocol are adhered to in totality will go a long way in assuring quality.
Keywords: Investigator's responsibilities, quality assurance, quality control, site preparedness
INTRODUCTION
Conducting clinical research is a highly complex and difficult endeavor. It mandates that the Principal Investigator (PI) constantly ensures oversight with regards to the study protocol, good clinical practice (GCP) guidelines, standard operating procedures (SOPs) of the site, institution and sponsor, requirements laid down by the Institutional Review Boards (IRB)/Institutional Ethics Committees (IECs), before, during and after conduct of the study. Monitoring and audits are two distinct processes that ensure that the rights and safety of the participants are protected, and data integrity is maintained. The latter is important so that the trial yields valid regulatory data in case of regulatory trials. Together, they have an additive impact on the data quality. A third process that can at times be associated with the two is an inspection. The present articles primarily focus on our experiences with monitoring and audits by a sponsor and/or a Contract Research Organization (CRO).
MONITORING AND AUDITS-DEFINITIONS
Monitoring
The International Council of Harmonization (ICH)-GCP defines monitoring as an act of overseeing the progress of a clinical trial, so as to ensure that the trial is conducted, recorded, and reported in accordance with the protocol, SOPs, GCP, and the applicable regulatory requirement(s).[1]
Audit
An audit, on the other hand, is a systematic and independent examination of trial-related activities and documents to determine whether the evaluated trial-related activities were conducted, and the data were recorded, analyzed, and accurately reported according to the protocol, sponsor's SOPs, GCP, and the applicable regulatory requirement(s).[1]
THE DISTINCTION BETWEEN MONITORING AND AUDIT
Monitoring and audits are similar in that they both protect the rights, safety, and well-being of study participants as well as data integrity. However, they are different with respect to responsibilities of the different stakeholders and the frequency with which these processes are carried out. For studies funded by the pharmaceutical industry, the responsibility for monitoring lies with them. For academic studies, it lies with the PI. Thus, for every study, the responsibility of ensuring monitoring rests with the “sponsor” and in the case of academic studies/Investigator Initiated Studies, the PI becomes the sponsor.
Monitoring is a regular activity done at predefined frequencies spelt out in a predefined monitoring plan. The process of monitoring ensures that study activities are being carried out as planned and deficiencies addressed and corrected promptly. It is thus a quality control tool. An audit, on the other hand, is not frequent. It can be done at any time during the conduct of the study (ad hoc) or “for cause” (for a specific purpose). An audit is essentially a quality assurance activity undertaken by personnel independent of the trial.
THE PROCESS OF MONITORING BY THE SPONSOR
Monitoring is necessary for all clinical trials regardless of whether they are academic studies or funded by the pharmaceutical industry. The monitoring plan for a particular research study should be made based on the study's complexity and envisaged risks. For Investigator-Initiated studies, the PI is responsible for having a written monitoring plan before study initiation. These studies should be monitored by someone independent of that particular study but may be part of the investigator's overall team. For industry-funded studies, the PI is responsible for ensuring that the sponsor or CRO, (when monitoring is outsourced), provides a monitoring plan for the study before its initiation. He/she must also ensure his team's familiarity with it.[2]
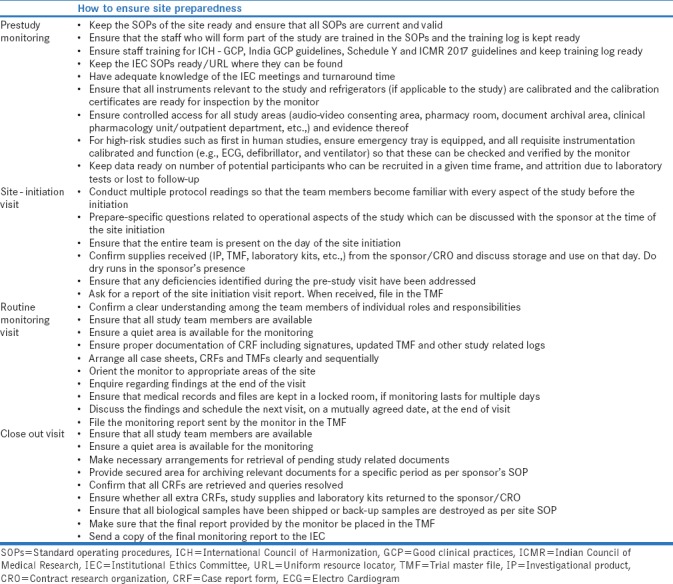
The monitoring process is usually undertaken in three phases – before, during, and after the study. Before the study, a prestudy qualification visit is done where the capability of the investigator is assessed, and facilities scrutinized. Post-IEC approval, a site initiation visit is done. Here, the protocol is discussed threadbare and key elements reiterated to minimize errors and the monitoring plan presented. Subsequently, monitoring is done at regular intervals as the study progresses. The last monitoring visit is a “close out” visit when a final check is done, and the data securely archived. Preparedness for all three stages of monitoring at the site is given in Table 1.
Table 1.
Preparedness for monitoring by the sponsor
AUDIT
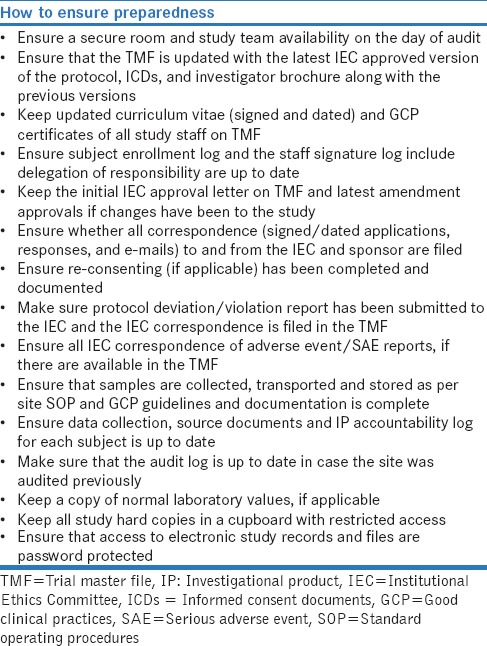
The purpose of an audit as mentioned earlier is to evaluate that the trial is conducted in compliance with the protocol, SOPs, GCP, and the applicable regulatory requirements and it is a quality assurance tool. Audits are usually conducted by the sponsor and/or the regulatory authorities. The PI is usually notified about an audit in advance. Measures to ensure site preparedness (there is some overlap of preparedness for an audit with monitoring) for an audit is depicted in Table 2.
Table 2.
Site preparedness for a sponsor or a regulatory audit
INSPECTION
An inspection is a regulatory audit. It is conducted by the regulatory authority and assesses whether the investigator and sponsor are conducting the study as per applicable statutory and regulatory requirements. Rule 122 DAC of Drugs and Cosmetic act 1940 states that the regulator is authorized to conduct trial site inspection at any time.[3] In the event that noncompliance is found, the regulator can suspend/cancel the trial and even debar the sponsor and/or investigator from conducting future studies. Thus, preparedness of the study site at all times must be ensured, as unlike audits and monitoring; an inspection can be sudden or with very little warning. The preparedness for inspection is in no way different from that of an audit or monitoring.
CHALLENGES FACED BY INVESTIGATOR FOR THE MONITORING AND AUDITS AND PROPOSED SOLUTIONS-A PERSONAL PERSPECTIVE
Table 3 lists all the challenges that were faced by the authors with regards to monitoring and audits. Most or all of these challenges can be addressed through mutual understanding, appropriate communication, and adequate training of all stakeholders involved.
Table 3.
Challenges faced by investigator for the monitoring and audits
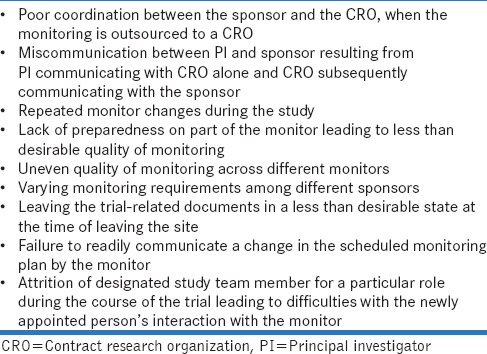
Potential solutions to address challenges faced during monitoring and audits
The solutions for ensuring effective monitoring and audits lie with all stakeholders involved. The relationship between the stakeholders should be one of mutual respect. At the level of the sponsor, following measures can be initiated:
Establish effective communication between all the stakeholders involved
Avoid frequent change of monitors
Have an SOP to ensure uniform quality of monitoring in case of repeated monitor changes
Every monitor should be knowledgeable about the site-specific protocol and related documents and establish clear and coherent communication channels with the PI and his/her team
At the level of the investigator,
Appoint an internal monitor, even for regulatory studies, to oversee the trial-related activities on a periodic basis
Maintain a site-specific SOP to ensure continuity of trial in case of study staff attrition
Conduct assessment test at specified intervals for the study team to ensure better compliance with the protocol and amendments.
CONCLUSION
Effective monitoring is crucial to data integrity and human rights protection. It is, however, important to remember that the most effective tool for this is a well-designed and articulated protocol. Subsequent to this is a determined approach by the investigator and his/her team to ensure that all aspects of the protocol are adhered to in totality. A study by the authors that analyzed warning letters issued to investigators by the US Food and Drug Administration showed that the most common reasons for these letters were failure to adhere to the investigational plan (81%), failure to maintain adequate and accurate case histories (58.1%) followed by informed consent issues (48%).[4] Thus, while monitoring and audits are quality tools, true quality comes from adherence to the protocol and attention to detail.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.ICH-GCP E6 (R2) Guidelines. [Last accessed on 2017 Dec 20]. Available from: http://www.ich.org/fileadmin/Public_Web_Site/ICH_Products/Guidelines/Efficacy/E6/E6_R2__Step_4_2016_1109.pdf .
- 2. [Last accessed on 2018 Mar 21]. Available from: https://www.fda.gov/downloads/Drugs/Guidances/UCM269919.pdf.
- 3.Drugs and Cosmetics Act 1940 and Rules. 1945. [Last accessed on 2017 Dec 20]. Available from: http://www.cdsco.nic.in/writereaddata/2016Drugs%20and%20Cosmetics%20Act%201940%20 and %20Rules%201945.pdf .
- 4.Gogtay NJ, Doshi BM, Kannan S, Thatte U. A study of warning letters issued to clinical investigators and institutional review boards by the United States food and drug administration. Indian J Med Ethics. 2011;8:211–4. doi: 10.20529/IJME.2011.082. [DOI] [PubMed] [Google Scholar]


