Abstract
Objectives
We investigated differences in objectively measured sedentary behaviour (SB) and physical activity (PA) levels in subjects with cardiovascular disease (CVD) diagnosis or high CVD risk compared with healthy controls.
Methods
The present study includes a subsample (n=1398, Health 2011 Study) of participants, who attended health examinations and wore a triaxial accelerometer (≥4 days). Patients with CVD were identified and CVD risk was calculated for others using Framingham Risk Score (FRS). Participants were categorised into groups: FRS<10%; FRS=10%–30%; FRS>30%/CVD. Raw acceleration data were analysed with mean amplitude deviation (MAD) and angle for posture estimation (APE). MAD corresponding to intensity of PA was converted to metabolic equivalents (MET) and categorised to light (1.5–2.9 METs) and moderate to vigorous PA (MVPA≥3.0 METs). APE recognises SB and standing.
Results
Daily accumulated time of >30 s MVPA bouts was higher in FRS<10% group (46 min) than in FRS>30%/CVD group (29 min) (p<0.001). FRS>30%/CVD group were more sedentary, their mean daily number of >10 min SB bouts (13.2) was higher than in FRS <10% group (11.5) (p=0.002).
Conclusion
Number and accumulated times of SB and PA bouts differed between the CVD risk groups. Causative research is required to assess the importance of SB and PA in prevention and rehabilitation of CVDs.
Keywords: Accelerometer, Cardiology prevention, Physical activity, Sitting time.
Key messages.
There were no differences in sedentary behaviour (SB) and physical activity (PA) profiles among patients with cardiovascular disease (CVD) and their non-CVD peers with high CVD risk.
The participants with low CVD risk had 73% higher number of moderate-to-vigorous PA bouts lasting >3 min compared with the individuals with CVD diagnosis or high CVD risk.
The individuals with CVD diagnosis or high CVD risk had 14% higher total time of SB accumulating from bouts lasting >5 min than their peers with lower CVD risk.
Introduction
Cardiovascular diseases (CVDs), such as ischaemic heart disease, are the leading cause of death worldwide.1 The development of diagnostics, drug therapy and interventional procedures has decreased CVD mortality. However, the CVDs still cause 32% of deaths globally.1 Medical and invasive therapies also have side effects, and they induce great economical burden to society.2 Exposing factors behind CVDs are sex, old age, genetic vulnerability, impaired physical fitness, smoking, elevated low-density lipoprotein (LDL) cholesterol, hypertension and diabetes.3 4. These factors have been exploited to build models that predict individual’s risk of developing a CVD in the future, such as the well-established Framingham Risk Score (FRS).5
Sedentary behaviour (SB) was recently demonstrated to be a risk factor of CVDs and mortality.3 6 7 SB is defined as energy expenditure ≤1.5 metabolic equivalent (MET) (=3.5 mL/kg/min O2 consumption), which indicates energy consumed in seated, reclined or lying position. Low physical activity (PA) is another important risk factor of CVDs. PA is defined as energy expenditure >1.5 MET.8 9 Previous studies have confirmed an inverse association between PA and CVDs.10 In addition, the longitudinal effects of PA have been discovered to be beneficial in preventing CVDs.11
Assessment of PA and SB can be conducted by subjective or objective methods. Traditionally, subjective methods, such as questionnaires, have been used to determine the amount of SB and PA.12 13 One objective means is to use an accelerometer.9 Previous studies have shown that objective measurements are more accurate in investigating the associations of SB and PA with CVDs than self-report tools.14 15 Objective measurements might allow more precise dose–response relationship between CVDs and SB or PA than self-reported estimates.3 6 Accelerometer data have mostly been analysed with count-based units.6 15 However, the count-based data from various studies are largely incomparable because cut-points and algorithms are varying between studies.9 16
The specific differences in SB and PA profiles among patients with CVD and non-CVD peers should be determined to design lifestyle-based strategies for the primary and secondary prevention of CVDs. The purpose of the present study was to objectively investigate SB and PA parameters, for example, number and accumulated times of different bout lengths among subjects with high CVD risk or established CVD compared with their healthy peers with low CVD risk.
Methods
Study population
This study is based on the ‘Physical activity and fitness’—subsample of the Health 2011 Study including 4916 men and women aged 18–85 years in Finland.17 In total, 2055 participants attended the health examinations and agreed to take the waist-worn accelerometer for 7 days. A total of 1398 participants fulfilled the criterion about the sufficient accelerometer use (≥4 days with ≥10 hours of data) and were used as a study population. The same criterion has been used in previous studies.15 The data were collected between August 2011 and March 2012.
Cardiovascular disease
Participants with established CVD (coronary artery disease, myocardial infarction, heart failure) were identified with questionnaires. Well-known CVD risk factors were assessed by trained research assistant (ie, blood pressure, plasma cholesterol) or asked in the questionnaires (smoking, diabetes diagnosis, antihypertensive medication) (table 1).5 These risk factors were used to build FRS to estimate individual’s 10-year risk to develop CVD. The obtained scores were then used to categorise participants into three groups: (1) subjects with low risk (<10%), n=884 (group 1); (2) subjects with medium risk (10%–30%), n=400 (group 2); and (3) subjects with high CVD risk (>30%) and/or CVD diagnosis (ischaemic heart disease, myocardial infarction), n=114 (group 3) (table 2).5
Table 1.
Clinical characteristics of the participants
| Male(n=596) | Female(n=802) | All(n=1398) | |
| Age (years) | 53.5 (13.2) | 53.3 (13.7) | 53.4 (13.5) |
| Weight (kg) | 84.7 (14.5) | 70.8 (13.4) | 76.8 (15.5) |
| Height (cm) | 177 (7) | 164 (7) | 170 (7) |
| BMI (kg/m2) | 26.9 (4.2) | 26.4 (4.8) | 26.7 (4.6) |
| Waist (cm) | 96.8 (12.3) | 86.8 (12.7) | 91.1 (13.4) |
| Total cholesterol (mmol/L) | 5.36 (0.99) | 5.45 (0.96) | 5.41 (0.98) |
| HDL cholesterol (mmol/L) | 1.40 (0.33) | 1.65 (0.37) | 1.54 (0.38) |
| LDL cholesterol (mmol/L) | 3.29 (0.87) | 3.28 (0.85) | 3.29 (0.86) |
| Triglycerides (mmol/L) | 1.45 (0.88) | 1.12 (0.59) | 1.26 (0.74) |
| Systolic BP (mm Hg) | 132 (16) | 130 (19) | 131 (18) |
| Diastolic BP (mm Hg) | 82 (10) | 79 (10) | 80 (10) |
| Smoking | 80 (13.4) | 95 (11.8) | 175 (12.5) |
| Diabetes | 41 (6.9) | 42 (5.2) | 83 (5.9) |
| Hypertension | 166 (27.9) | 213 (26.6) | 379 (27.1) |
| Antihypertensive medication | 142 (23.8) | 179 (22.3) | 321 (23.0) |
| Ischaemic heart disease | 36 (6.0) | 19 (2.4) | 55 (3.9) |
| Heart failure | 9 (1.5) | 7 (0.9) | 16 (1.1) |
The values denote mean (SD) or number (%).
BMI, body mass index; BP, blood pressure; HDL, high-density lipoprotein; LDL, low-density lipoprotein.
Table 2.
SB and physical activity in the CVD risk groups*
| <10% risk (n=884) | 10%–30% risk(n=400) | >30% risk/CVD(n=114) | <10% risk vs10%–30% riskP values | <10% risk vs>30% risk/CVDP values | |
| MVPA | |||||
| Mean daily accumulated total times of MVPA bouts lasting | |||||
| >30 s† | 46 (0.8) | 40 (1.3) | 29 (2.3) | 0.001 | <0.001 |
| >5 min† | 16 (0.6) | 14 (0.8) | 10 (1.7) | <0.001 | <0.001 |
| >10 min† | 10 (0.5) | 9.3 (0.7) | 7.1 (1.4) | 0.002 | 0.002 |
| Mean daily number of MVPA bouts lasting | |||||
| >5 min‡ | 1.3 (0.04) | 1.1 (0.1) | 0.8 (0.1) | <0.001 | <0.001 |
| >10 min‡ | 0.48 (0.02) | 0.45 (0.03) | 0.36 (0.07) | 0.001 | 0.001 |
| >3 min‡ | 2.6 (0.1) | 2.2 (0.1) | 1.5 (0.2) | 0.003 | <0.001 |
| SB | |||||
| Mean daily accumulated total times of SB bouts lasting | |||||
| >3 min† | 350 (3.7) | 374 (5.5) | 398 (11.1) | 0.006 | 0.002 |
| >5 min† | 308 (3.6) | 335 (5.4) | 358 (11.0) | 0.005 | 0.004 |
| Mean daily number of SB bouts lasting | |||||
| >5 min‡ | 23.1 (0.2) | 23.2 (0.3) | 24.3 (0.6) | 0.028 | 0.001 |
| >10 min‡ | 11.5 (0.1) | 12.3 (0.2) | 13.2 (0.4) | 0.014 | 0.002 |
| Number of daily steps | |||||
| Maximum | 11 070 (160) | 9080 (220) | 6 670 (430) | <0.001 | <0.001 |
| Mean | 7 280 (100) | 5970 (150) | 4 400 (270) | <0.001 | <0.001 |
| METs | |||||
| Maximum peak MET-level of weekly physical activity bouts lasting | |||||
| 15 min | 5.8 (0.1) | 4.6 (0.1) | 3.8 (0.1) | <0.001 | <0.001 |
| 1 min | 8.5 (0.1) | 6.5 (0.1) | 5.5 (0.2) | <0.001 | <0.001 |
| Mean number of breaks in SB | |||||
| 43.4 (0.4) | 40.2 (0.6) | 40.3 (1.2) | 0.76 | 0.39 | |
Multinominal regression between the CVD groups. Standardised by age, sex and accelerometer wearing time.
*CVD risk groups: (1) participants with <10% risk of CVD; (2) participants with 10%–30% risk of CVD; (3) participants with >30% risk of CVD or CVD diagnosis (ischaemic heart disease, acute myocardial infarction or combination of these). CVD risk is based on Framingham Risk Score (includes age, systolic blood pressure, total cholesterol, high-density lipoprotein cholesterol, smoking, diabetes and antihypertensive medication as explanatory variables).
†The values denote: minutes (SEM).
‡The values denote: number of bouts (SEM).
CVD, cardiovascular disease; MET, metabolic equivalent; MVPA, moderate-to-vigorous physical activity; SB, sedentary behaviour.
Assessment of PA and SB
A waist-worn triaxial accelerometer (Hookie AM 20, Traxmeet Ltd, Espoo, Finland) was used to assess PA and SB. The accelerometer was attached to a flexible belt on the right side of the hip. The acceleration data were collected at 100 Hz sampling rate. Participants were given oral and written instructions to use the accelerometer for seven consecutive days during wake time. The accelerometer was not intended to be used in water. The raw accelerometer data were stored on a hard disk for analysis.
The mean amplitude deviation (MAD) values of the resultant acceleration of the three orthogonal acceleration components were determined in 6 s epochs. The MAD values have been found to be a valid indicator of incident energy consumption during locomotion.16 18 The MAD values were converted to METs for each epoch.
PA was divided into three intensity categories in terms of METs: light PA 1.5–2.9 MET; moderate PA 3.0–5.9 MET and vigorous PA >6.0 MET.9 The proportion of mean vigorous PA was generally <1% of daily wear time. Therefore, PA was reported as light (1.5–2.9 MET) and moderate-to-vigorous PA (MVPA ≥3.0 MET).4 8
SB was defined as the time spent in the seated/reclining/lying position without movement (<1.5 MET). Standing still was analysed separately. The accelerometer orientation in terms of the gravity vector was taken as the reference, with the posture being determined from the incident accelerometer orientation.19 The number of breaks in SB was calculated by measuring all of the lying and sitting periods, which ended in the vertical movement of standing up.
Total time, number and accumulated times of following bout lengths (eg, >30 s,>15 min) of SB, standing and PA were determined.4 Maximum and mean daily number of steps were also calculated. In addition, maximum peak MET levels of weekly PA bouts of different bout lengths (eg, 1 min, 15 min) were identified.4
The Coordinating ethics committee of the Hospital District of Helsinki and Uusimaa gave an ethical permission for the study (45113/03100/11). All the study participants signed a written informed consent before participation.
Statistical analysis
Table 2 shows the association between three CVD risk groups, and PA and SB variables, which was tested with multinominal logistic regression adjusted for age, sex and accelerometer wearing time. The CVD risk group of <10% was used as a reference group. Table 3 shows the difference between the subjects with >30% risk of CVDs and CVD diagnosis, which was tested with a general linear model (analysis of covariance). All analyses were conducted by IBM SPSS V.24.0.
Table 3.
Sedentary behaviour and physical activity levels in the subjects with >30% risk of CVDs* and CVD diagnosis†
| >30% risk(n=51) | CVD diagnosis(n=63) | Mean difference | 95% CI for the difference | |
| MVPA | ||||
| Mean daily accumulated total times of MVPA bouts lasting | ||||
| >30 s‡ | 31.2 (27.2) | 26.6 (23.0) | 2.9 | −6.2 to 12.1 |
| Mean daily number of MVPA bouts lasting | ||||
| >5 min§ | 0.89 (1.50) | 0.79 (1.12) | 0.04 | −0.46 to 0.54 |
| SB | ||||
| Mean daily accumulated total times of SB bouts lasting | ||||
| >3 min‡ | 380 (114) | 412 (120) | −39 | −75.4 to −2.6 |
| Mean daily number of SB bouts lasting | ||||
| >5 min§ | 23.5 (6.0) | 24.8 (6.6) | −1.6 | −3.6 to 0.3 |
| Number of daily steps | ||||
| Mean | 4740 (3160) | 4120 (2710) | 500 | −560 to 1550 |
General linear model (analysis of covariance) between the subjects with >30% risk and CVD diagnosis. Standardised by age, sex and accelerometer wearing time.
*CVD risk is based on Framingham Risk Score (includes age, systolic blood pressure, total cholesterol, high-density lipoprotein cholesterol, smoking, diabetes and antihypertensive medication as explanatory variables).
†CVD diagnosis: ischaemic heart disease, acute myocardial infarction or combination of these.
‡The values denote: minutes (SD).
§The values denote: number of bouts (SD).
CVD, cardiovascular disease; MVPA, moderate-to-vigorous physical activity; SB, sedentary behaviour.
Results
CVD risk factors
Clinical characteristics of the study sample are shown in table 1. Regarding the risk factors for CVDs, 43% (n=596) were men, 13% (n=175) were smokers, 5.9% (n=83) had diagnosed diabetes, 27% (n=379) had hypertension and 23% (n=321) were on antihypertensive medication. The mean total cholesterol was 5.4 mmol/L, LDL cholesterol 3.3 mmol/L and high-density lipoprotein (HDL) cholesterol 1.5 mmol/L.
Prevalence of CVDs
Ischaemic heart disease, being the leading CVD diagnosis, had been diagnosed in 3.9% (n=55) of the study population. On average, men had higher prevalence of ischaemic heart disease (6.0%, n=36) than women (2.4%, n=19) (table 1). Heart failure was another common CVD diagnosis with prevalence of 1.1% (n=16). As in the case of ischaemic heart disease, men had higher prevalence of heart failure (1.5%, n=9) compared with women (0.9%, n=7)(table 1).
Patients with CVD versus high CVD risk peers: SB and PA levels
Patients with CVD diagnosis and those with FRS >30% did not differ from each other with respect to SB and PA (table 3). Their daily accumulated total times of >30 s MVPA bouts differed by only 3.5 min (patients with CVD: 26.6 min vs FRS >30%: 31.2 min). Similarly, the mean daily number of steps differed between the patients with CVD (4120) and FRS >30% subjects (4740) with only 500 steps.
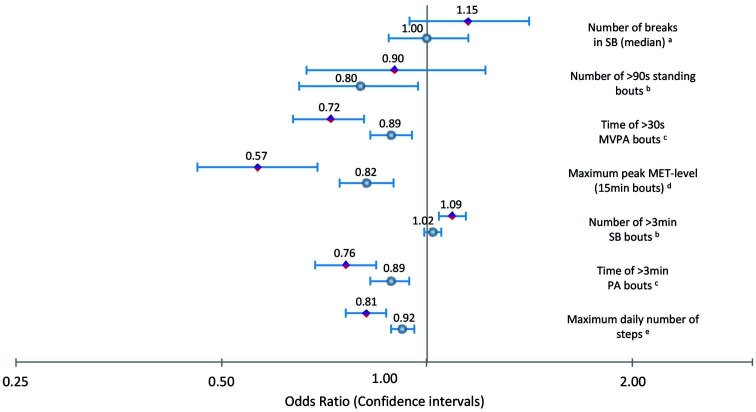
Subjects with CVD or high CVD risk versus non-CVD peers: PA
Table 2 illustrates the PA and SB levels in different CVD risk groups. Participants of the low-risk group had higher number of MVPA bouts compared with the medium-risk group, and especially, to the high-risk/CVD group. The number of MVPA bouts lasting for >3 or >5 min was 73% and 63% (p<0.001), respectively, greater in the low-risk group compared with the high-risk/CVD group. Participants of the low-risk group also had higher accumulated total times of different MVPA bouts than those in the medium-risk and high-risk/CVD group. The daily accumulated total times of MVPA bouts lasting for >30 s was 59% greater (p<0.001) in the low-risk group compared with the high-risk/CVD group (figure 1).
Figure 1.
The differences in sedentary behaviour and physical activity levels between the CVD groups*. CVD: Cardiovascular disease; number: mean daily number of bouts; time: mean daily accumulated total time of bouts; MVPA: moderate- to vigorous physical activity; MET: metabolic equivalent (3.5 mL/kg/min o2 consumption); level: level of weekly physical activity bout lengths; SB: sedentary behaviour; PA: physical activity. *CVD groups: 1. Participants with <10% risk of CVD; 2. Participants with 10-30% risk of CVD; 3. Participants with >30% risk of CVD or CVD diagnosis. CVD risk is based on Framingham risk score (includes age, systolic blood pressure, total cholesterol, HDL cholesterol, smoking, diabetes and antihypertensive medication as explanatory variables). Calculated against: a 10 breaks in SB; b one bout; c 10 minutes; d one MET; e 1000 steps. OR defines odds ratio versus subjects with <10% risk of CVD. The blue circle represents participants with 10-30% risk of CVD. The red square represents participants with >30% risk of CVD or CVD diagnosis.
Subjects with CVD or high CVD risk versus non-CVD peers: SB
SB levels also differed significantly between the three risk groups (table 2). The accumulated total times of SB bouts lasting for >3 or >5 min were 12% (p=0.002) and 14% (p=0.004), respectively, smaller in the low-risk group compared with the high-risk/CVD group. Also the mean daily number of SB bouts differed significantly between the CVD groups (figure 1). For example, the low-risk group had 13% (p=0.002) less SB bouts lasting >10 min compared with the high-risk/CVD group.
Subjects with CVD or high CVD risk versus non-CVD peers: steps and MET levels
Furthermore, the daily number of steps differed between the three risk groups. The maximum and mean daily number of steps were both 66% (p<0.001) greater in the low-risk group compared with the high-risk/CVD group (table 2, figure 1). Peak MET levels also differed between the groups, maximum weekly peak MET levels having the clearest difference. Especially, the maximum weekly peak MET level of bout lasting 15 min was 53% (p<0.001) greater in the low-risk group compared with the high-risk/CVD group (table 2, figure 1).
Discussion
CVD risk groups: PA
As far as we are aware, the present study is the first one evaluating habitual PA and SB between the subjects with high CVD risk or CVD diagnosis and their lower risk peers in an inclusive population-based sample using diverse accelerometer parameters. We found that there were significant differences in the PA habits between the subjects with low and high risk or established CVD. Especially, MVPA levels differed markedly between the three groups in favour of low-risk participants. The mean daily number and accumulated total times of MVPA bouts (eg, lasting >30 s) showed most significant differences in PA levels between the groups. Associations between MVPA and CVD risk have been investigated in previous studies and most of them have reported negative associations between MVPA/PA and CVD risk.6 20 However, objective measurements of MVPA have not been used to compare subjects with high CVD risk or established CVD and those with lower risk. Furthermore, instead of using only the common total times of PA and SB, the present study used a novel set of diverse PA and SB parameters only exploited in a few earlier studies.4 8
CVD risk groups: SB
We found that both mean daily number and accumulated times of objectively measured SB bouts differed between the participants with low, medium and high CVD risk or CVD diagnosis. Accumulated total times of SB bouts differed significantly between the risk groups, the participants with high CVD risk or CVD diagnosis having the highest accumulated times. Also the numbers of SB bouts of different lengths (eg, >5 min) showed clear differences between the groups; patients with CVD or high-risk participants had the higher number of SB bouts compared with other groups. Our results are in line with the previous studies reporting that objectively measured SB is related to CVD markers/risks.3 6 However, objectively measured SB data are rare when it comes to patients with CVD and their non-CVD peers. Creating of specific parameters requires dedicated analysis algorithms, such as MAD and APE, to recognise different postures and breaks in SB.16 18 19 Previous studies have used count-based thresholds to separate SB from PA, whereas specific posture-based information of SB does not exist in the previous CVD studies.3 6 15 However, those investigations have discovered deleterious associations between SB and CVD risk factors, which is in line with the present study.
CVD risk groups: steps and METs
We also found that the daily number of steps differed significantly between the risk groups. The low-risk subjects had the highest daily step counts compared with other subjects, especially to those with high risk or CVD. The previous studies including data on steps have reported associations with CVD risk.4 21 In the present study, maximum peak MET levels differed between participants in favour of the low-risk subjects. MET levels have rarely been used as outcome parameters of PA in the previous studies. Instead, they have usually been used to categorise activity.
Objective measurements
To assess the relevance of daily SB and PA levels in progression and management of CVDs, objective measurements conducted to the patients with CVD and their non-CVD controls with different CVD risk profiles are required. Results from this kind of measurements are relevant in making recommendations for CVD prevention.
Patients with CVD vs high CVD risk peers
In this study, we separated diagnosed patients with CVD and high CVD risk subjects from their non-CVD peers and compared their habitual PA and SB. The participants without diagnosed CVD were furthermore categorised by their CVD risk in order to divide the whole study sample in three specific groups. Categorisation was based on established FRS, which is one of the most accurate risk models for estimating individual’s overall CVD risk (accuracy: 79% for women and 76% for men).5 The subjects with CVD (coronary artery disease, myocardial infarction) and/or high CVD risk (FRS >30%) were categorised into the same group because they did not differ from each other with respect to PA levels. For example, mean daily step count differed between these groups with only 500 steps and daily total time of >30 s MVPA bouts with 3.5 min. These differences are minimal compared with the ones detected between the three CVD groups.
CVD risk
Separate CVD risk parameters (ie, cholesterol levels) are most often used for estimating CVD risk in the previous accelerometer studies.3 6However, these parameters do not give information about comprehensive CVD risk. Few CVD risk studies with accelerometer measurements have included FRS or other CVD risk models, and found SB as positive and PA as negative factors associating with CVD risk.20 22
Strengths of the present study
A large population-based sample is one of the most important strengths of the present study, giving an opportunity to compare the relationship of SB and PA levels in subjects with different CVD risk profiles in Finnish adult population.17 In addition, we exploited specific and novel algorithms, such as MAD and APE, for assessing the duration and intensity of SB and PA.16 18 19 We also employed multiple SB and PA parameters. Because of the universal nature of the algorithms used in the present study (not depending on the device brand), the MAD and the APE have the potential to be exploited as tools of clinical practice. With these novel algorithms researchers can provide clinically relevant variables (ie, number of breaks in SB, number of steps, number and accumulated times of different bout lengths of SB, standing and PA). These new variables could be used as a target of PA counselling when creating, for instance, future systems with interactive accelerometer and smartphone application.
Limitations of the present study
Some limitations in our study need to be addressed. The lack of objective measurements in water-based activities is one. Accelerometers were instructed to be used during the wake-up time, which is why some of the SB data may have been lost. In addition, the present study had cross-sectional design. Due to the lack of causative results, we cannot prove whether high SB and low PA levels resulted in high CVD risk and CVD development, or whether the patients with CVD and high-risk subjects were just more likely to spend time as sedentary. It is possible that the subjects with CVD diagnosis or high risk might have limited ability to reach high PA levels, which could explain some of the differences in MVPA. Finally, the subjects with CVD diagnosis were recognised with questionnaires, which might have led to few incorrect classifications in the categorisation of participants. However, the proportion of the incorrect classification is obviously minor in the study population.
Conclusions
The present study found that both mean daily number and accumulated times of SB differed significantly between the subjects with high risk of CVD or CVD diagnosis and their non-CVD peers with lower risk, which supports the findings previously discovered in the field of CVD risk factors. The subjects with high CVD risk as well as patients with CVD had the highest mean daily number of SB bouts, especially bouts lasting for >10 min. In conclusion to results of PA, the daily total time of MVPA bouts lasting for >30 s was the most significant predictor of CVD risk. Mean and maximal daily number of steps, and weekly peak MET levels also were predictors of CVD risk in favour of the participants with lowest CVD risk. There were no significant differences in accumulated SB and PA levels between patients with CVD and high CVD risk subjects. Due to the cross-sectional design of the present study, further research with causative design is required for determining the importance of SB and PA in primary and secondary prevention of CVDs.
Acknowledgments
The authors acknowledge the contribution of the National Institute for Health and Welfare for collecting and preparing the Health 2011 data.
Footnotes
Contributors: All authors contributed to the design of the study. VV, PH, HV-Y, JHS, KT, HS and TV contributed to the statistical analysis of the work. VV drafted the manuscript. All authors have read and revised the manuscript, and approved the submission to BMJ Open Sport & Exercise Medicine.
Funding: The present study was supported by the Finnish Ministry of Education and Culture.
Competing interests: None declared.
Ethical approval: The coordinating ethics committee of the Hospital District of Helsinki and Uusimaa gave an ethical permission for the study (45113/03100/11).
Provenance and peer review: Not commissioned; internally peer reviewed.
Data sharing statement: The Health 2011 Study data are maintained by the National Institute for Health and Welfare (THL). The data are available for research purposes from http://www.terveys2011.info/aineisto after the research protocol has been accepted by the executive scientific committee of THL.
Patient consent: Not required.
References
- 1. Naghavi M, Wang H, Lozano R, et al. . Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015;385:117–71. 10.1016/S0140-6736(14)61682-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Hambrecht R, Walther C, Möbius-Winkler S, et al. . Percutaneous coronary angioplasty compared with exercise training in patients with stable coronary artery disease: a randomized trial. Circulation 2004;109:March:1371–8. 10.1161/01.CIR.0000121360.31954.1F [DOI] [PubMed] [Google Scholar]
- 3. Healy GN, Winkler EA, Owen N, et al. . Replacing sitting time with standing or stepping: associations with cardio-metabolic risk biomarkers. Eur Heart J 2015;36:2643–9. 10.1093/eurheartj/ehv308 [DOI] [PubMed] [Google Scholar]
- 4. Vasankari V, Husu P, Vähä-Ypyä H, et al. . Association of objectively measured sedentary behaviour and physical activity with cardiovascular disease risk. Eur J Prev Cardiol 2017;24:1311–8. 10.1177/2047487317711048 [DOI] [PubMed] [Google Scholar]
- 5. D'Agostino RB, Vasan RS, Pencina MJ, et al. . General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation 2008;117:743–53. 10.1161/CIRCULATIONAHA.107.699579 [DOI] [PubMed] [Google Scholar]
- 6. Qi Q, Strizich G, Merchant G, et al. . Objectively measured sedentary time and cardiometabolic biomarkers in US hispanic/latino adults: The Hispanic Community Health Study/Study of Latinos (HCHS/SOL). Circulation 2015;132:1560–9. 10.1161/CIRCULATIONAHA.115.016938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Chau JY, Grunseit A, Midthjell K, et al. . Sedentary behaviour and risk of mortality from all-causes and cardiometabolic diseases in adults: evidence from the HUNT3 population cohort. Br J Sports Med 2015;49:737–42. 10.1136/bjsports-2012-091974 [DOI] [PubMed] [Google Scholar]
- 8. Husu P, Suni J, Vähä-Ypyä H, et al. . Objectively measured sedentary behavior and physical activity in a sample of Finnish adults: a cross-sectional study. BMC Public Health 2016;16:920 10.1186/s12889-016-3591-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Strath SJ, Kaminsky LA, Ainsworth BE, et al. . Guide to the assessment of physical activity: clinical and research applications: a scientific statement from the American Heart Association. Circulation 2013;128:2259–79. 10.1161/01.cir.0000435708.67487.da [DOI] [PubMed] [Google Scholar]
- 10. Ekblom-Bak E, Ekblom B, Vikström M, et al. . The importance of non-exercise physical activity for cardiovascular health and longevity. Br J Sports Med 2014;48:233–8. 10.1136/bjsports-2012-092038 [DOI] [PubMed] [Google Scholar]
- 11. Mann S, Jimenez A, Domone S, et al. . Comparative effects of three 48-week community-based physical activity and exercise interventions on aerobic capacity, total cholesterol and mean arterial blood pressure. BMJ Open Sport Exerc Med 2016;2:e000105 10.1136/bmjsem-2015-000105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Wanner M, Hartmann C, Pestoni G, et al. . Validation of the global physical activity questionnaire for self-administration in a european context. BMJ Open Sport Exerc Med 2017;3:e000206 10.1136/bmjsem-2016-000206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Grøntved A, Hu FB. Television viewing and risk of type 2 diabetes, cardiovascular disease, and all-cause mortality: a meta-analysis. JAMA 2011;305:2448–55. 10.1001/jama.2011.812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Celis-Morales CA, Perez-Bravo F, Ibañez L, et al. . Objective vs. self-reported physical activity and sedentary time: effects of measurement method on relationships with risk biomarkers. PLoS One 2012;7:e36345 10.1371/journal.pone.0036345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kozàkovà M, Palombo C, Morizzo C, et al. . Effect of sedentary behaviour and vigorous physical activity on segment-specific carotid wall thickness and its progression in a healthy population. Eur Heart J 2010;31:1511–9. 10.1093/eurheartj/ehq092 [DOI] [PubMed] [Google Scholar]
- 16. Vähä-Ypyä H, Vasankari T, Husu P, et al. . Validation of cut-points for evaluating the intensity of physical activity with accelerometry-based Mean Amplitude Deviation (MAD). PLoS One 2015;10:e0134813 10.1371/journal.pone.0134813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Koskinen S, Lundqvist A, Ristiluoma N. Health, functional capacity and welfare in Finland in 2011. Helsinki: National Institute for Health and Welfare (THL), 2012. [Google Scholar]
- 18. Vähä-Ypyä H, Vasankari T, Husu P, et al. . A universal, accurate intensity-based classification of different physical activities using raw data of accelerometer. Clin Physiol Funct Imaging 2015;35:64–70. 10.1111/cpf.12127 [DOI] [PubMed] [Google Scholar]
- 19. Vähä-Ypyä H, Husu P, Suni J, et al. . Reliable recognition of lying, sitting, and standing with a hip-worn accelerometer. Scand J Med Sci Sports 2018;28:1092-1102 10.1111/sms.13017 [DOI] [PubMed] [Google Scholar]
- 20. Maddison R, Jiang Y, Foley L, et al. . The association between the activity profile and cardiovascular risk. J Sci Med Sport 2016;19:605–10. 10.1016/j.jsams.2015.08.001 [DOI] [PubMed] [Google Scholar]
- 21. Parsons TJ, Sartini C, Ellins EA, et al. . Objectively measured physical activity, sedentary time and subclinical vascular disease: Cross-sectional study in older British men. Prev Med 2016;89:194–9. 10.1016/j.ypmed.2016.05.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Wijndaele K, Orrow G, Ekelund U, et al. . Increasing objectively measured sedentary time increases clustered cardiometabolic risk: a 6 year analysis of the ProActive study. Diabetologia 2014;57:305–12. 10.1007/s00125-013-3102-y [DOI] [PMC free article] [PubMed] [Google Scholar]