Abstract
A multidimensional exploratory statistical method, canonical correlation analysis (CCA), was applied to evaluate the impact of complexity parameters on the plan quality and deliverability of volumetric-modulated arc therapy (VMAT) and to determine parameters in the generation of an ideal VMAT plan. Canonical correlations among complexity, quality and deliverability parameters of VMAT, as well as the contribution weights of different parameters were investigated with 71 two-arc VMAT nasopharyngeal cancer (NPC) patients, and further verified with 28 one-arc VMAT prostate cancer patients. The average MU and MU per control point (MU/CP) for two-arc VMAT plans were 702.6 ± 55.7 and 3.9 ± 0.3 versus 504.6 ± 99.2 and 5.6 ± 1.1 for one-arc VMAT plans, respectively. The individual volume-based 3D gamma passing rates of clinical target volume (γCTV) and planning target volume (γPTV) for NPC and prostate cancer patients were 85.7% ± 9.0% vs 92.6% ± 7.8%, and 88.0% ± 7.6% vs 91.2% ± 7.7%, respectively. Plan complexity parameters of NPC patients were correlated with plan quality (P = 0.047) and individual volume-based 3D gamma indices γ(IV) (P = 0.01), in which, MU/CP and segment area (SA) per control point (SA/CP) were weighted highly in correlation with γ(IV) , and SA/CP, percentage of CPs with SA < 5 × 5 cm2 (%SA < 5 × 5 cm2) and PTV volume were weighted highly in correlation with plan quality with coefficients of 0.98, 0.68 and −0.99, respectively. Further verification with one-arc VMAT plans demonstrated similar results. In conclusion, MU, SA-related parameters and PTV volume were found to have strong effects on the plan quality and deliverability.
Keywords: volumetric-modulated arc therapy, canonical correlation analysis, plan complexity, plan quality, plan deliverability
INTRODUCTION
The practice of radiotherapy has been impacted in many ways with the evolution of radiotherapy technique from conventional 3D-confromal treatment (CRT) to intensity-modulated radiation therapy (IMRT) and volumetric-modulated arc therapy (VMAT). Due to the extra degrees of freedom obtained, IMRT can provide several advantages over CRT, such as improvement in dose distributions, target dose escalation, outcome and decrease in toxicities [1–3]. VMAT is a new IMRT delivery method with more degrees of freedom by means of one or more gantry rotations that combines a dynamic multileaf collimator (MLC) with varying dose rates and gantry speed [4, 5]. It has been demonstrated that compared with IMRT, VMAT decreases the delivery time and monitor units (MUs) with highly conformal dose distributions, which improves patient comfort and decreases the probability of intrafraction errors [6, 7]. However, these improvements are often associated with an increase in complexity that affects many steps of the treatment process, including treatment planning, quality assurance and treatment delivery [8].
It has been demonstrated that as the dose conformity increases, so the complexity of the technique increases for IMRT planning [9]. The compromise between plan complexity, quality and accuracy of delivery has long been a concern for IMRT and VMAT. McNiven et al. introduced a single metric of modulation complexity score (MCS) to assess the overall plan complexity and the relationship between complexity and delivery accuracy for IMRT [10]. Chen et al. studied the impact of leaf motion constraints on the plan quality, delivery accuracy and efficiency of intensity-modulated arc therapy (IMAT) and developed recommendations for optimizing the balance between plan quality and delivery efficiency [11]. Masi et al. evaluated the impact of average leaf travel (LT), MCS applied to VMAT (MCSv), MU, and a multiplicative combination of LT and MCSv (LCMCS) on VMAT dosimetric accuracy [12]. However, most of these correlations were based on two isolated parameters, and no single monotonic relationship was found and universally accepted.
The purpose of this study was to explore the multidimensional relationship between parameters representing different characteristics of VMAT plans: (i) complexity parameters, (ii) quality parameters and (iii) deliverability parameters with canonical correlation analysis (CCA) [13]. Thus, we explored not only the correlation between different sets of parameters representing specific characteristics of a VMAT plan, but also the contribution weight of each corresponding parameter.
MATERIALS AND METHODS
Study design
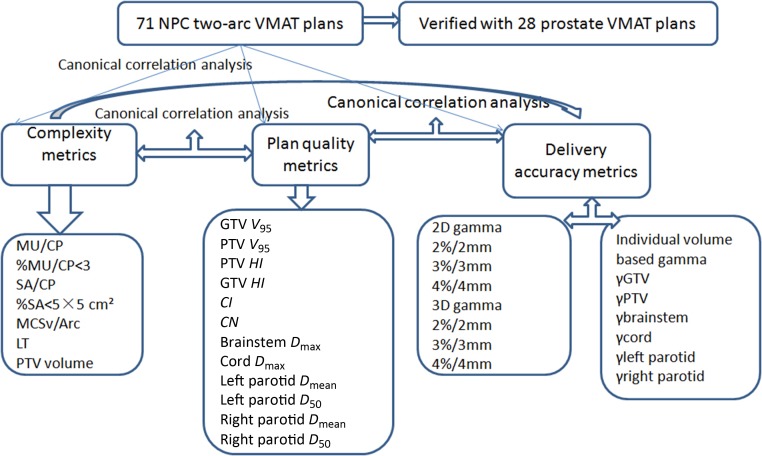
As shown in Fig. 1, the flowchart for the overall study design, CCA was conducted among complexity metrics, plan quality metrics, and delivery accuracy metrics for two-arc VMAT plans of 71 nasopharyngeal cancer (NPC) patients. Canonical correlation among metrics and the relative weight of each item in the metrics were obtained to evaluate the correlation between complexity, plan quality and deliverability, as well as the impact of each item in the correlation. The study was further verified with 28 one-arc VMAT plans of prostate cancer patients.
Fig. 1.
The flowchart for the overall study design.
Patients and data acquisition
Seventy-one NPC patients who underwent two-arc VMAT treatment were enrolled in this study, and 28 prostate cancer patients who underwent one-arc VMAT treatment were selected for further verification. VMAT plans were optimized with the SmartArc algorithm in the Pinnacle treatment planning system (TPS) (Philips Healthcare, Fitchburg, WI) for a 6-MV X-ray beam. Two-arc VMAT objective settings and optimization parameters for NPC patients have been reported in previous studies [14, 15]. Briefly, the gross tumor volume (GTV) was delineated as the mass shown in the enhanced computed tomography images or magnetic resonance images or both, including the nasopharyngeal tumor, retropharyngeal lymphadenopathy, and enlarged neck nodes. The clinical target volume (CTV) was defined as the GTV plus a margin of potential microscopic spread, encompassing the inferior sphenoid sinus, clivus, skull base, nasopharynx, ipsilateral parapharyngeal space, and posterior third of the nasal cavity and maxillary sinuses. High-risk nodal regions, such as the bilateral upper deep jugular nodes; submandibular nodes; jugulodigastric, mid-jugular, low jugular, and supraclavicular nodes; and the posterior cervical nodes, were included. The planning target volume (PTV) was created based on the target volume plus a 3 mm margin, allowing for set-up variability [14, 15]. Prescription doses were 70 Gy and 56 Gy for the GTV and PTV, respectively, in 28 fractions. Organs at risk (OARs), including the brainstem, spinal cord, and left and right parotids, were constrained for optimization. The first arc rotated clockwise from181° to 180°, and the second arc rotated counterclockwise from 180° to 181°.
For one-arc VMAT plans of prostate cancer patients, standardization contouring was done by one radiation oncologist according to the contouring guidelines of Radiation Therapy Oncology Group (RTOG) Trial 0126 [16]. The GTV encompassed the prostate gland, and the CTV encompassed the GTV plus the proximal bilateral seminal vesicles. The PTV was generated by adding a surrounding margin of 7 mm to the CTV. A total dose of 78 Gy was prescribed for the PTV, in 39 fractions. OARs were outlined according to the Male RTOG Normal Pelvis Atlas [17]. For one-arc VMAT optimization, at least 95% of the PTV must be covered by 95% of the prescription dose. OAR constraints included the rectum, bladder, peritoneal cavity or bowel, femurs, and unspecified tissue. A start angle of 181° and a stop angle of 180° were applied for one arc plans using a clockwise (CW) rotation direction. A leaf motion of 0.46 cm/deg and a final arc space degree of 4 were employed for both one-arc and two-arc VMAT. House-built software based on Matlab 2010a (Mathwork Inc., USA) was applied to read and process the information from exported DICOM-RT files, including plan information, structures, planned dose distribution, and CT images, etc.
Plan complexity parameters
The complexity information of VMAT plans is strongly related to control points (CPs) [4]. A low quota of MU/CP is believed to put a higher demand on MLC leaves to move faster between the two continuous CPs; therefore, it indicates a higher degree of plan complexity [4]. A small segment area per CP (SA/CP) causes more difficulties and uncertainties in dose measurement. Thus, the proportion of CPs with MU < 3 (%MU/CP < 3) and the percentage of CPs with segment area < 5 × 5 cm2 (%SA < 5 × 5 cm2) were adopted to give additional complexity information for the treatment plans. MCSv/Arc and the average LT distance reported in the study of Masi et al. were also included [12]. The PTV volume was another complexity parameter.
Plan quality parameters
Plan quality parameters provide information about target coverage, dose homogeneity, dose conformity and OAR sparing by the evaluation of dose–volume histograms (DVHs). Target parameters included the V95 of the GTV and the PTV; the homogeneity index (HI) for the GTV and the PTV, defined as the difference between the dose to 1% (D1) and 99% (D99) of the volume divided by the prescription dose (Dp) [18]:
| (1) |
The conformity index (CI) [19] and the conformation number (CN) [20] of the PTV were defined as:
| (2) |
| (3) |
where VT,Pi is the target volume covered by the prescription dose, VT is the target volume. VPi is the body volume covered by the prescription isodose line.
For OAR sparing, the Dmax of the brainstem and spinal cord, and the Dmean and D50 of the left and right parotids were calculated for NPC patients. the Dmean of the rectum and bladder, V50 of the rectum, D40 of the bladder, and D3 of the left and right femoral heads were calculated as the quality parameters for prostate cancer.
Deliverability parameters
All plans were delivered on an Elekta Synergy linac (Elekta Ltd, Crawley, UK) with a MOSAIQ record and verify system (version 1.60Q3, IMPAC Medical Systems, Inc., Sunnyvale, CA). A 3D diode array ArcCHECK and 3DVH software (Sun Nuclear Corporation, Melbourne, FL,US) were applied to study the 2D and 3D dosimetric accuracies.Both 2D and 3D pre-treatment VMAT gamma passing rates (γ(2D/3D)) with relative gamma acceptance criteria of 4%/4 mm, 3%/3 mm, 2%/2 mm and 10% lower dose threshold (TH) were conducted [21]. Individual volume-based 3D gamma indices (γ(IV)) defined as relative percentage gamma passing rates (%GP) with 3%/3 mm criteria for individual target and OAR volumes, such as γGTV, γPTV, γbrainstem, γbladder, etc., were also calculated based on 3DVH QA analysis, and applied to further investigate the relationship between complexity and deliverability [22].
Canonical correlation analysis
Canonical correlation analysis for complexity, quality and deliverability parameters was conducted using SPSS (V.19, SPSS Inc., Chicago, IL, USA). CCA consists of analysing the correlation between two groups of variables, and it allows us to find linear combinations (canonical variates) of two sets of variables with the highest correlation. To do this, it selects an axis in each group that maximizes the variance in that group, while it tries to maximize the amount of covariation between the two variable groups. High correlation of CCA means that both groups share common information, and it is usually measured by the r coefficient and the assessment of statistical significance with Wilk’s lambda test. Usually, only the first correlation shows significant correlation (canonical variate 1), but sometimes more than one variate shows significant correlation (canonical variate 2).
The coefficients of each linear combination (canonical variate) give us information of what variables are correlated. The canonical coefficients are also called the canonical weights, and are used to assess the relative importance of individual variables’ contributions to a given canonical correlation. The canonical coefficients are the standardized weights in the linear equation of variables that creates the canonical variates. As such, they are analogous to beta weights in regression analysis [23]. A high coefficient on a variable marks that variable as correlated with the other group, while a low coefficient (in absolute value) on a variable means a lower correlation [13].
RESULTS
Descriptive statistics including Student’s t test of plan complexity, plan quality and deliverability parameters for two-arc VMAT and one-arc VMAT plans were summarized in Table 1. The average total MUs for two-arc VMAT plans were 702.6 ± 55.7 versus 504.6 ± 99.2 for one-arc VMAT plans. MUs/CP were 3.9 ± 0.3 and 5.6 ± 1.1 for NPC and prostate cancer patients, respectively. The γCTV and γPTV for NPC and prostate cancer patients were 85.7% ± 9.0% vs 92.6% ± 7.8%, and 88.0% ± 7.6% vs 91.2% ± 7.7%, respectively.
Table 1.
Descrtiptive statistics of plan complexity, plan quality and deliverability parameters for nasophageal cancer and prostate cancer patients
| NPC | Prostate | P | |
|---|---|---|---|
| Plan complexity | |||
| MU/CP | 3.9 ± 0.3 | 5.6 ± 1.1 | <0.001 |
| %MU/CP < 3 | 0.5 ± 0.05 | 0.3 ± 0.1 | <0.001 |
| SA(cm2)/CP | 70.1 ± 8.3 | 46.0 ± 21.8 | <0.001 |
| %SA < 5 × 5 cm2 | 66.3 ± 9.4 | 38.2 ± 20.0 | <0.001 |
| MCSv/Beam(Arc) | 0.6 ± 0.09 | 0.50 ± 0.09 | <0.001 |
| LT (mm/Arc) | 571.0 ± 27.1 | 0.5 ± 0.09 | <0.001 |
| PTV volume | 854.6 ± 168.2 | 325.5 ± 210.1 | <0.001 |
| MU | 702.6 ± 55.7 | 504.6 ± 99.2 | <0.001 |
| Plan quality | |||
| GTVV95% | 95.4 ± 12.4 | 99. 6 ± 0.6 | 0.06 |
| PTVV95% | 93.7 ± 3.5 | 95.5 ± 3.53 | 0.03 |
| GTVHI | 0.1 ± 0.03 | 0.07 ± 0.03 | <0.001 |
| PTVHI | 0.3 ± 0.08 | 0.1 ± 0.04 | <0.001 |
| CI | 0.9 ± 0.06 | 0.9 ± 0.06 | 0.64 |
| CN | 0.8 ± 0.05 | 0.8 ± 0.05 | 0.41 |
| Deliverability | |||
| 2D gamma passing rate (%) | |||
| 4%/4 mm | 99.2 ± 1.6 | 99.6 ± 0.4 | 0.04 |
| 3%/3 mm | 97.1 ± 1.3 | 97.9 ± 1.1 | 0.001 |
| 2%/2 mm | 87.6 ± 3.4 | 89.1 ± 3.6 | 0.05 |
| 3D gamma passing rate (%) | |||
| 4%/4 mm | 98.7 ± 0.9 | 99.6 ± 0.3 | <0.001 |
| 3%/3 mm | 96.0 ± 2.2 | 98.4 ± 0.9 | <0.001 |
| 2%/2 mm | 90.0 ± 4.3 | 93.7 ± 1.8 | <0.001 |
%MU/CP < 3 = the proportion of MU/CP less than 3, %SA < 5×5 cm2 = the proportion of SA less than 5 × 5 cm2, GTVV95% = the percent volume of the GTV covered by the 95% prescription isodose line, PTVV95% = the percent volume of the PTV covered by the 95% prescription isodose line, GTVHI = the HI of the GTV, PTVHI = the HI of the PTV.
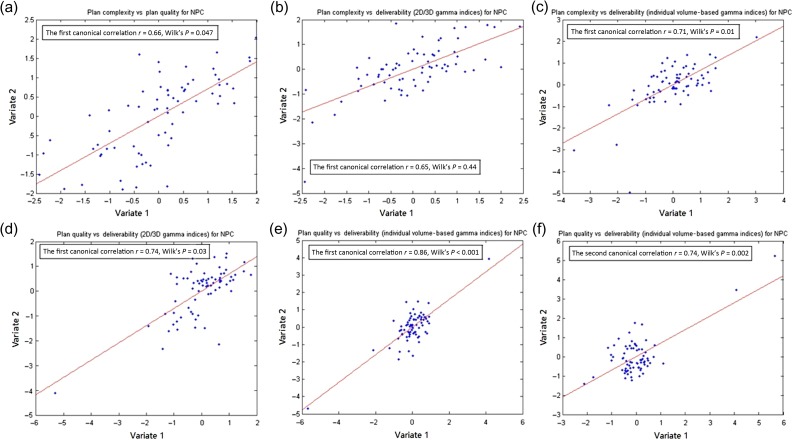
The CCA results for NPC are shown in Fig. 2. The first canonical correlation was significant between plan complexity and quality, with a canonical correlation of 0.66 (P = 0.047 according to Wilk’s test). The correlation between plan complexity and 2D/3D gamma passing rate (γ(2D/3D)) was not statistically significant, with a canonical correlation of 0.65 (P = 0.44). Individual volume-based 3D gamma indices (γ(IV)) were calculated and their correlations with complexity were investigated. The first canonical correlation between complexity and γ(IV) was significant, with the canonical correlation of 0.71 (P = 0.01). The plan qualities were correlated with both γ(2D/3D) and γ(IV), as shown in Fig. 2.
Fig. 2.
Canonical correlation analysis results for nasopharyngeal cancer patients, the x and y axes were canonical variates for (a) plan complexity vs quality; (b) plan complexity vs deliverability (2D/3D gamma indices); (c) plan complexity vs deliverability (individual volume-based gamma indices); (d) plan quality vs deliverability (2D/3D gamma indices); (e, f) plan quality vs deliverability (individual volume-based gamma indices).
The standard canonical coefficients for the canonical variates of NPC CCA analysis are presented in Table 2. According to the canonical coefficients, the complexity parameters of SA/CP, % SA < 5 × 5 cm2 and PTV volume were weighted highly in correlation with plan quality, with a coefficient of 0.98, 0.68 and −0.99, respectively. The plan quality parameters of HIs, CI, CN, and Dmean of the left parotid were weighted highly in the correlation. The γ(2D/3D) with 3D 4%/4 mm and 3%/3 mm criteria were weighted heavily among deliverability parameters in their correlation with plan quality. The complexity parameters of MU/CP and SA/CP were weighted highly in correlation with γ(IV). γ(IV) parameters of γCTV and γPTV were weighted heavily in their correlation with plan complexity parameters, as well with plan quality.
Table 2.
The standard conanical coefficients for canonical variates among these three variable sets for NPC patients
| Complexity vs. quality | Complexity vs γ(2D/3D) | Plan quality vs.γ(2D/3D) | Complexity vs γ(IV) | Plan quality vs γ(IV) | |||
|---|---|---|---|---|---|---|---|
| Canonical variate 1 | Canonical variate 1 | Canonical variate 1 | Canonical variate 1 (γ(IV)) | Canonical variate 1 (γ(IV)) | Canonical variate 2 (γ(IV)) | ||
| Complexity parameter | |||||||
| MU/CP | −0.16 | −0.81 | −0.63 | ||||
| %MU/CP < 3 | −0.48 | −0.53 | −0.43 | ||||
| SA(cm2)/CP | 0.98 | 0.62 | −0.72 | ||||
| %SA < 5 × 5 cm2 | 0.68 | 0.47 | 0.03 | ||||
| MCSv/Beam(Arc) | −0.14 | −0.77 | 0.21 | ||||
| LT (mm/Arc) | 0.16 | 0.21 | −0.37 | ||||
| PTV volume | −0.99 | 0.34 | 0.04 | ||||
| Plan quality | |||||||
| GTVV95% | 0.24 | −0.57 | −0.20 | 0.28 | |||
| PTVV95% | 0.40 | −0.65 | −0.40 | 0.82 | |||
| GTVHI | 1.36 | −2.91 | 5.67 | 2.34 | |||
| PTVHI | −1.18 | −0.091 | 0.05 | −0.09 | |||
| CI | 2.98 | −5.73 | 9.93 | 4.27 | |||
| CN | −3.01 | 5.32 | −9.6 | −4.01 | |||
| Brainstem Dmax | 0.16 | −0.02 | 0.14 | −0.21 | |||
| Cord Dmax | −0.05 | −0.10 | −0.09 | −0.19 | |||
| Right parotid Dmean | −0.46 | −0.02 | −0.27 | −0.06 | |||
| Right parotid D50 | 0.37 | 0.27 | 0.24 | 0.01 | |||
| Left parotid Dmean | 0.73 | 0.12 | −0.15 | 0.04 | |||
| Left parotid D50 | −0.30 | −0.14 | 0.47 | −0.01 | |||
| Deliverability (2D/3D gamma indices) | Individual volume-based 3D gamma indices | ||||||
| 2D 4%/4 mm | −0.15 | −0.18 | −0.07 | 0.06 | 0.32 | γcord | |
| 2D 3%/3 mm | 1.04 | 0.093 | 0.13 | 0.80 | 0.70 | γbrainstem | |
| 2D 2%/2 mm | −0.61 | 0.097 | −0.42 | 0.12 | −0.30 | γleft parotid | |
| 3D 4%/4 mm | 3.32 | −2.51 | −0.24 | −0.47 | 0.09 | γright parotid | |
| 3D 3%/3 mm | −5.92 | 1.65 | 0.37 | −0.63 | 0.73 | γGTV | |
| 3D 2%/2 mm | 3.36 | 0.32 | −5.89 | −1.84 | 0.98 | γCTV | |
| 5.70 | 1.91 | −1.45 | γPTV | ||||
%MU/CP < 3 = the proportion of MU/CP less than 3, %SA < 5 × 5 cm2 = the proportion of SA less than 5 × 5 cm2, GTVV95% = the percentage volume of the GTV covered by the 95% prescription isodose line, PTVV95% = the percentage volume of the PTV covered by the 95% prescription isodose line, GTVHI = the HI of the GTV, PTVHI = the HI of the PTV.
The correlations between plan complexity, quality and deliverability parameters were further verified with CCA analysis on one-arc VMAT prostate cancer patients. The first canonical correlation was significant between complexity and quality, with a canonical correlation of 0.92 (P = 0.02). The first two canonical correlations were significant between complexity and both (γ(2D/3D)) and γ(IV), with correlations of 0.88 (P = 0.001), 0.79 (P = 0.02) and 0.93 (P < 0.001), 0.84 (P = 0.006), respectively. Plan qualities were correlated with both (γ(2D/3D)) (r = 0.92, P = 0.01) and γ(IV) (r = 0.96, P = 0.02). The first canonical correlation for plan quality vs deliverability γ(IV) was significant, with a correlation of 0.96 (P = 0.02).
Table 3 presents the standard canonical coefficients of canonical variates of prostate cancer CCA. According to the canonical coefficients, the complexity parameters of MU/CP and SA/CP were weighted highly in correlation with plan quality for prostate cancer patients. The HI and CI of the PTV of plan quality had a higher weight during correlation. The parameters of MU/CP, SA/CP, LT, as well as PTV volume were weighted highly for the correlation between complexity and deliverability for both γ(2D/3D) and γ(IV). For γ(2D/3D), the gamma passing rates with 2D 4%/4mm and 3%/3mm were weighted highly during their correlation with complexity.
Table 3.
The standard conanical coefficients for canonical variates among these three variable sets for prostate cancer patients
| Complexity vs quality | Complexity vs γ(2D/3D) | Plan quality vs γ(2D/3D) | Complexity vs γ(IV) | Plan quality vs γ(IV) | ||||
|---|---|---|---|---|---|---|---|---|
| Canonical variate 1 | Canonical variate 1 | Canonical variate 2 | Canonical variate1 | Canonical variate1 | Canonical variate 2 | Canonical variate 1 | ||
| Complexity parameter | ||||||||
| MU/CP | −0.49 | −0.15 | −1.57 | −1.69 | 0.53 | |||
| %MU/CP < 3 | −0.02 | 0.28 | −0.68 | −0.46 | 0.23 | |||
| SA(cm2)/CP | 0.34 | −1.14 | −2.85 | 1.63 | 2.04 | |||
| %SA < 5 × 5 cm2 | 0.18 | 0.19 | −0.85 | 0.87 | 0.66 | |||
| MCSv/Beam(Arc) | 0.26 | 0.66 | 0.17 | −0.44 | −0.13 | |||
| LT (mm/Arc) | −0.28 | 0.68 | −0.79 | 0.98 | 1.30 | |||
| PTV volume | −0.006 | 0.39 | 1.38 | −0.99 | −1.39 | |||
| Plan quality | ||||||||
| GTVV95% | −0.51 | −0.77 | −0.26 | |||||
| PTVV95% | 0.42 | −0.1 | −0.44 | |||||
| GTVHI | 3.70 | −4.33 | −8.08 | |||||
| PTVHI | 0.42 | −0.54 | −0.59 | |||||
| CI | 6.28 | −6.05 | −12.86 | |||||
| CN | −5.81 | 5.54 | 11.96 | |||||
| Rectum Dmean | 0.31 | 0.09 | −0.64 | |||||
| Rectum V50 | −0.50 | 0.1 | 0.86 | |||||
| Bladder Dmean | −0.44 | 0.07 | 0.48 | |||||
| Bladder D40 | 0.42 | 0.03 | −0.66 | |||||
| Rfemoral D3 | 0.83 | −0.61 | −0.38 | |||||
| Lfemoral D3 | −3.20 | −0.04 | 0.81 | |||||
| Deliverability (2D/3D gamma indices) | Individual volume-based 3D gamma indices γ(IV) | |||||||
| 2D 4%/4 mm | 0.86 | 0.81 | 0.69 | 0.009 | −0.95 | −0.49 | γGTV | |
| 2D 3%/3 mm | −0.80 | −0.86 | −0.07 | 0.37 | −0.56 | −1.16 | γCTV | |
| 2D 2%/2 mm | −0.24 | −0.11 | −1.14 | 0.35 | 0.58 | 0.84 | γPTV | |
| 3D 4%/4 mm | −0.48 | −0.30 | 0.03 | 0.55 | 0.18 | −0.52 | γRectum | |
| 3D 3%/3 mm | 0.11 | 1.51 | 0.26 | 0.69 | 0.11 | −0.10 | γlfemoral | |
| 3D 2%/2 mm | −0.25 | −0.47 | 0.56 | 0.19 | 0.11 | 0.32 | γr femoral | |
| −0.82 | 0.18 | 0.39 | γbladder | |||||
%MU/CP < 3 = the proportion of MU/CP less than 3, %SA < 5 × 5 cm2 = the proportion of SA less than 5 × 5 cm2, GTVV95% = the percentage volume of the GTV covered by the the 95% prescription isodose line, PTVV95% = the percentage volume of the PTV covered by the 95% prescription isodose line, GTVHI = the HI of the GTV, PTVHI = the HI of the PTV, lfemoral = left femoral head, rfemoral = right femoral head.
DISCUSSION
In this study, CCA was adopted to investigate the multidimensional correlations among parameters of VMAT plans: (i) plan complexity vs quality, (ii) plan complexity vs deliverability, and (iii) plan quality vs deliverability. Compared with previous studies presenting only correlations between two single parameters, the current study provided not only the relationship between two different collections, with each containing multiple parameters, but also the contribution weight of each specific parameter.
Generally, a high degree of complexity of fixed-beam IMRT was associated with multiple parameters, such as a large number of MUs, small segment apertures, large number of segments, etc. [10, 24, 25]. As shown in Table 1, two-arc VMAT plans were much more complex than one-arc VMAT plans, as indicated by the complexity parameters. The plan quality comparison in Table 1 implied that the complexity of the two-arc VMAT plan decreased the target coverage HI, compared with the one-arc VMAT plan.
CCA results for NPC in this study demonstrated that the complexity parameters of SA/CP, % SA < 5 × 5 cm2, PTV volume, and the complexity parameters of MU/CP and SA/CP were weighted highly in correlation with plan quality and deliverability. This was consistent with previous findings that a low quota of MU/CP is believed to put a higher demand on MLC leaves to move faster between the two continuous CPs, and therefore it indicates a higher degree of plan complexity [5, 25]. As small segment fields cause more difficulties and uncertainties in the accuracy of dose measurement, a plan with more small fields exerts strong demands on and challenge to the delivery accuracy.
The seeking of complexity metrics and their correlations with the dosimetric accuracy of IMRT and VMAT plans had been studied aggressively with the hope of providing a valuable tool for improving plan optimization and verification. For VMAT plans, leaf motion constraints, average LT, MCS applied to VMAT (MCSv), MU value, and a multiplicative combination of LT and MCSv (LCMCS) had been found to be significantly correlated with VMAT dosimetric accuracy [11, 12]. The CCA results of this study consistently demonstrated that MU/CP, %MU/CP < 3 and MCSv/Arc affected the plan deliverability parameter of 3D γ for NPC, although no significant correlation was observed. Recently, the correlation between γ and the magnitude of dose discrepancy between the planned dose and the actual delivered dose for IMRT had been questioned [26, 27]. In our previous study, we found the 3D pre-treatment VMAT γ evaluation was more sensitive than the 2D γ index [21]. This study confirmed that 3D γ was weighted higher than 2D γ for NPC deliverability. Further analysis with γ(IV) confirmed that deliverability was highly correlated with plan quality, in which γGTV, γCTV, γPTV and γbrainstem were weighted heavily.
Plans included in this study were for the treatment of NPC and prostate cancer patients, and included both highly complex and simple VMAT plans. As indicated in this study, PTV volume was a very important complexity parameter that affected the plan quality and deliverability of VMAT. However, PTV volume is an intrinsic parameter related to an individual patient, rather than a user decidable parameter. For patients with a large PTV volume, IMRT may be an option instead of VMAT. It has been reported that as the complexity of the target volume increases, VMAT may have difficulty in achieving reasonable target coverage and OAR sparing, compared with IMRT [15, 28].
CCA results for prostate cancer further verified the correlations among VMAT parameters. The complexity parameters of MU/CP, SA/CP, and the complexity parameters of MU/CP, SA/CP, LT, PTV volume were weighted heavily in correlation with plan quality and deliverability for one-arc VMAT. Potentially, the methodology proposed in this study can be extended to other tumor sites and treatment techniques to create a large database that would be useful in determining optimal clinical radiotherapy treatment plans.
The outcome of CCA reports a significant canonical correlation and its associated coefficients, which maximizes the correlation between corresponding variates. However, the objective of CCA is not only to identify the relationships between two datasets, but to further predict the dependence of one set of variables on the other. Thus, based on the model of correlation, increasing SA/CP would be of help in improving conformity and homogeneity for the target, while increasing MU/CP would increase the delivery accuracy for NPC VMAT plans. Our future work will focus on the prediction of plan quality or deliverability of a treatment plan according to the complexity parameters. One could accordingly adjust the parameters of plan complexity to improve the plan quality and deliverability, thereby aiding in the process of treatment planning through patient QA.
CONCLUSION
MU, SA-related parameters and PTV volume were found to have strong effects on the plan quality and deliverability. The presented correlations identified between various quantified parameters could be used to improve the efficiency of the radiotherapy process from VMAT treatment planning to patient QA.
ACKNOWLEDGEMENTS
An abstract of partial results of this study was accepted as an oral presentation in the 2015 Asian–Ocean Congress of Medical Physics.
CONFLICT OF INTEREST
The authors declare that they have no competing interests.
FUNDING
This study was partially supported by grants from the National Natural Science Foundation of China (11675122), the Natural Science Foundation of Zhejiang Province (LY16H160046, LQ17C100002), and the Health Science and Technology Funding of Zhejiang Provincial Health Department (2015KYB241).
REFERENCES
- 1. Lee N, Xia P, Quivey JM et al. . Intensity-modulated radiotherapy in the treatment of nasopharyngeal carcinoma: an update of the UCSF experience. Int J Radiat Oncol Biol Phys 2002;53:12–22. [DOI] [PubMed] [Google Scholar]
- 2. Kuban DA, Tucker SL, Dong L et al. . Long-term results of the MD Anderson randomized dose-escalation trial for prostate cancer. Int J Radiat Oncol Biol Phys 2008;70:67–74. [DOI] [PubMed] [Google Scholar]
- 3. Pignol JP, Olivotto I, Rkovitch E et al. . A multicenter randomized trial of breast intensity-modulated radiation therapy to reduce acute radiation dermatitis. J Clin Oncol 2008;26:2085–92. [DOI] [PubMed] [Google Scholar]
- 4. Otto K. Volumetric modulated arc therapy: IMRT in a single gantry arc. Med Phys 2008;35:210–317. [DOI] [PubMed] [Google Scholar]
- 5. Cao D, Afghan MKN, Ye J et al. . A generalized inverse planning tool for volumetric-modulated arc therapy. Phys Med Biol 2009;54:6725–30. [DOI] [PubMed] [Google Scholar]
- 6. Palma D, Vollans E, James K et al. . Volumetric modulated arc therapy for delivery of prostate radiotherapy: comparison with intensity-modulated radiotherapy and three dimensional conformal radiotherapy. Int J Radiat Oncol Biol Phys 2008;72:996–1001. [DOI] [PubMed] [Google Scholar]
- 7. Rao M, Yang W, Chen F et al. . Comparison of Elekta VMAT with helical tomotherapy and fixed field IMRT: plan quality, delivery efficiency and accuracy. Med Phys 2010;37:1350–59. [DOI] [PubMed] [Google Scholar]
- 8. Bedford JL, Warrington AP. Commissioning of volumetric modulated arc therapy (VMAT). Int J Radiat Oncol Biol Phys 2009;73:537–45. [DOI] [PubMed] [Google Scholar]
- 9. Webb S. Use of a quantitative index of beam modulation to characterize dose conformality: illustration by a comparison of full beamlet IMRT, few-segment IMRT (fsIMRT) and conformal unmodulated radiotherapy. Phys Med Biol 2003;48:2051–62. [DOI] [PubMed] [Google Scholar]
- 10. McNiven AL, Sharpe MB, Purdie TG. A new metric for assessing IMRT modulation complexity and plan deliverability. Med Phys 2010;37:505–15. [DOI] [PubMed] [Google Scholar]
- 11. Chen F, Rao M, Ye J et al. . Impact of leaf motion constraints on IMAT plan quality, deliver accuracy, and efficiency. Med Phys 2011;38:6106–18. [DOI] [PubMed] [Google Scholar]
- 12. Masi L, Doro R, Favuzza V et al. . Impact of plan parameters on the dosimetric accuracy of volumetric modulated arc therapy. Med Phys 2013;40:071718-1–11. [DOI] [PubMed] [Google Scholar]
- 13. Hotelling H. Relations between two sets of variates. Biometrika 1936;28:312–77. [Google Scholar]
- 14. Wu S, Xie C, Jin X et al. . Simultaneous modulated accelerated radiation therapy in the treatment of nasopharyngeal cacner: a local center’s experience. Int J Radiat Oncol Biol Phys 2006;66:S40–S46. [Google Scholar]
- 15. Jin X, Yi J, Zhou Y et al. . Comparison of whole field simultaneous integrated boost VMAT and IMRT in the treatment of nasopharyngeal cancer. Med Dosim 2013;38:418–23. [DOI] [PubMed] [Google Scholar]
- 16. Michalski J, Purdy J, Watkins-Bruner D. RTOG P-0126: A Phase III Randomized Study of High-Dose 3D-CRT/IMRT Versus Standard Dose 3D-CRT/IMRT in Patients Treated for localized Prostate Cancer. http://www.rtog.org/ClinicalTrials/ProtocolTable/StudyDetails.aspx?study=0126 (30 July 2016, date last accessed).
- 17. Gay HA, Barthold HJ, O’Meara E et al. . Pelvic normal tissue contouring guidelines for radiation therapy: a radiation therapy Oncology Group Consensus Panel Atlas. Int J Radiat Oncol Biol Phys 2012;83:e353–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Iori M, Cattaneo GM, Cagni E et al. . Dose–volume and biological-model based comparison between helical tomotherapy and (inverse-planned) IMAT for prostate tumours. Radiother Oncol 2008,88:34–45. [DOI] [PubMed] [Google Scholar]
- 19. Lomax NJ, Scheib SG. Quantifying the degree of conformity in radiosurgery treatment planning. Int J Radiat Oncol Biol Phys 2003;55:1409–19. [DOI] [PubMed] [Google Scholar]
- 20. Nelms BE, Simon JA. A survey on IMRT QA analysis. J Appl Clin Med Phys 2007;8, 76–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Jin X, Yan H, Han C et al. . Correlation between gamma index passing rate and clinical dosimetric difference for pre-treatment 2D and 3D volumetric modulated arc therapy dosimetric verification. Br J Radiol 2015;88:20140577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Wu C, Hosier KE, Beck KE et al. . On using 3D γ-analysis for IMRT and VMAT pretreatment plan QA. Med Phys 2012;39:3051–9. [DOI] [PubMed] [Google Scholar]
- 23. Thompson B, Borrello GM. The importance of structure coefficients in regression research. Educ Psychol Meas 1985;45:203–9. [Google Scholar]
- 24. Mohan R, Amfield M, Tong S et al. . The impact of fluctuations in intensity patterns on the number of monitor units and the quality and accuracy of intensity modulated radiotherapy. Med Phys 2000;27:1226–37. [DOI] [PubMed] [Google Scholar]
- 25. Valdes G, Scheuermann R, Hung CY et al. . A mathematical framework for virtual IMRT QA using machine learning. Med Phys 2016;43:4323. [DOI] [PubMed] [Google Scholar]
- 26. Zhen H, Nelms BE, Tome WA. Moving from gamma passing rates to patient DVH-based QA metrics in pretreatment dose QA. Med Phys 2011;38:5477–89. [DOI] [PubMed] [Google Scholar]
- 27. Stasi M, Bresciani S, Miranti A et al. . Pretreatment patient-specific IMRT quality assurance: a correlation study between gamma index and patient clinical dose volume histogram. Med Phys 2012;39:7626–34. [DOI] [PubMed] [Google Scholar]
- 28. Verbakel WF, Cuijpers JP, Hoffmans D et al. . Volumetric intensitymodulated arc therapy vs. conventional IMRT in head-and-neck cancer: a comparative planning and dosimetric study. Int J Radiat Oncol Biol Phys 2009;74:252–9. [DOI] [PubMed] [Google Scholar]