Abstract
Rationale: The highest burden of liver cancer occurs in developing countries, where the use of herbal medicine (HM) is still widespread. Despite this trend, few studies have been conducted to report HM practices of patients with a hepatic tumor in the developing world. Hence, this study aimed to document the use of HM among patients with liver cancer in Peru. Study Design and Methods: A comparative behavioral epidemiological survey was conducted among liver cancer patients attending the National Cancer Institute of Peru. Information was obtained by direct interviews based on a semistructured questionnaire. The use of HM in Peruvian liver cancer patients was reported, first, regarding general consumption prior to the onset of disease, and second, after the appearance of symptoms that patients would relate to their tumor. In parallel, general consumption of HM in noncancerous people was assessed as a comparative figure. A correspondence analysis was performed to reveal potential associations between the symptoms of cancer and the specific use of HM. Results: Eighty-eight patients and 117 noncancerous individuals participated in the survey. Overall, 68.3% of the people interviewed claimed to use HM on a regular basis for general health preservation. Furthermore, 56.8% of the patients turned to plants first to treat the disorders for which they later came to the cancer care center. When compared with the number of plant species used routinely (n = 78), a selection of plants was made by patients in response to the symptoms of cancer (n = 46). At least 2 plant species, Aloe vera and Morinda citrifolia, were significantly associated with the treatment of liver cancer–related symptoms in the patient group. Conclusions: The present study is the first survey on the HM practices of patients with liver cancer in Latin America and, more broadly, in the developing world. Our findings confirm that HM remains one of the principal primary health care resources in Peru, even for a severe disease like liver cancer. These traditional, complementary and alternative medicine practices should be taken into consideration in Peruvian health programs aiming to educate the population in cancer prevention and treatment, as well as integrative cancer management.
Keywords: behavioral epidemiological survey, cancer, complementary and alternative medicine, developing world, ethnobotany, Indigenous people, integrative medicine, Latin America, liver disease, traditional medicine
Introduction
Liver cancer is one of the deadliest forms of malignancy. Its mortality rate makes it the second leading cause of tumor-related death worldwide, with 745 000 deaths a year.1 The global incidence of liver cancer has doubled over the past 2 decades, with nearly 83% of cases and 84% of related deaths occurring in the developing world.2,3 In Peru, liver cancer represents 6.5% of all cancer cases and 10% of the overall cancer mortality.4 We have recently described an unusually young subset of Peruvian patients with hepatocellular carcinoma who displayed peculiar pathophysiological characteristics.5,6 In this patient population, the rate of cirrhosis, the most common precancerous condition associated with hepatic carcinogenesis, was surprisingly low at only 5%. At the molecular genetic level, the mutation spectrum was unique with a major class of alterations epitomized by genomic deletions.7 The specific causes of this unusual molecular signature and the early age of clinical presentation have yet to be elucidated.
In Peru, conventional medicine coexists with traditional, complementary and alternative medicine (TCAM).8 TCAM has been institutionally recognized by the Peruvian authorities through the implementation in 1998 of the Complementary Medicine Service (CMS) in the EsSalud national health care system (CMS-EsSalud).9-11 CMS-EsSalud is responsible for conducting research programs on TCAM and integrative medicine, establishing safety guidelines, and disseminating information on TCAM practices. In 2014, there were 55 TCAM centers operating across the country, servicing more than 50 000 patients per year. However, cancer has not been included in the list of diseases under consideration by CMS-EsSalud.9
TCAM encompasses different health practices, ranging from biologically based therapies such as herbal medicine (HM), which is widely used in Peru, to mind-body interventions. Peruvian HM is based on the use of a rich pharmacopeia of plants,12 which has been partly compiled and analyzed through ethnobotanical and ethnopharmacological research programs.13-25 Still, much remains to be done to achieve the objective of accurately recording Peruvian traditional medication and assessing the relevance of HM, especially in cases of life-threatening diseases like cancer. To the best of our knowledge, only one research article deals specifically with HM and cancer in Peru.25 In this study, 51 plants encountered in Peruvian medicinal markets were selected from an ethnopharmacological point of view and evaluated in vitro for their antiproliferative activity on liver cancer cells. Additionally, sparse publications report the use of some plant taxa for cancer in Peru.13-15,20 Nevertheless, “cancer” was used therein as a generic term that was not precisely defined; thus, considerable uncertainty remains about the accuracy of this information.
The aim of the present study was thus to document the medicinal itinerary of Peruvian patients diagnosed with a liver cancer prior to their arrival at the cancer care center and to assess their genuine HM practices and their subsequent variation to a fiercely changing health condition due to the hepatic tumor. This cross-sectional study was supplemented by a comparison with a group of healthy, noncancerous individuals in order to gain insights into the health strategy adopted by people facing liver cancer in Peru.
The Peruvian authorities launched in 2012 the first national comprehensive cancer plan, Plan Esperanza, aiming to provide coverage for cancer care to the most vulnerable populations, and also to support cancer education and prevention.26 Hence, our work could contribute, by means of Plan Esperanza and CMS-EsSalud, to generate a holistic appraisal of cancer perception and treatment in Peru for better patient care in the frame of an integrative medical system, as recommended by the World Health Organization and other authorities.27-29
Materials and Methods
Rationale
In the present study, the term TCAM is utilized as defined previously by Bodeker and Burford,8 with the difference that only biologically based HM was considered, excluding de facto mind-body based practices, that is, those that are used to enhance the mind’s positive impact on the body such as meditation, prayer, yoga, massage, and so on.
Survey Site
Located in metropolitan Lima, the National Cancer Institute of Peru (INEN) is the Peruvian health care center in charge of the management of neoplastic diseases at the national level, under the auspices of the Peruvian Ministry of Health.30 As a public hospital, INEN accommodates individuals regardless of age, sex, ethnicity, residence, economic status, and health care coverage. The centralization of the Peruvian health care system means that INEN serves as a national hub for neoplastic diseases management, servicing cancer patients from across the country, and thus providing favorable conditions to assess their TCAM practices.
Groups Interviewed and Survey Period
The study was conducted between April 2013 and August 2014 among Peruvian patients with hepatic tumor consulting at the INEN Department of Abdominal Surgery (patient group) and noncancerous blood donors attending the INEN Blood Bank (comparative group). Blood donors were people without any a priori connection to the liver cancer patients included in the study.
Conduct of the Survey
Prior to their inclusion, people received information regarding the purpose and the conduct of the study. Survey participation was voluntary and at the discretion of the individuals involved. Interviewees were not remunerated. Both the patient and one of their relatives gave written consent for the storage of his or her information at INEN and for its use for research. In cases where the patient was a minor, the interview was conducted in the presence of his or her legal guardian, that is, one of the parents in most of the cases. The Human Subjects Committee of INEN approved the conduct of this survey (Protocol Number #113-2014-CIE-INEN).
Survey Questions
The study was conducted using a semistructured questionnaire provided in supplemental document S1. The ad hoc questionnaire included open- and closed-ended questions,31 and was divided into 6 sections categorized as follows:
Survey data. This section established the date, starting and ending times of the interview, the names of the interviewer and treating physician, and the INEN individual identification number.
Sociological data. This section included the age, gender, birthplace, marital status, and education level of the interviewee. Information on the native languages of the patients and their ethnic group was taken. Approximate monthly income of the interviewees and their family was estimated.
Living environment. This section provided information on the past and present work of the interviewees and their relatives (ie, parents, spouse, and children), the area of residence (eg, city, countryside, shanty town), the personal and familial history, and the migration pattern.
Lifestyle. This section provided information on the interviewees’ diet, smoking and drinking habits, allopathic treatments, and HM practices. People were asked whether they usually consumed plants (regular HM) and what for (patient and comparative groups); and whether they took plant remedies especially against the symptoms (symptomatic HM) for which they came to INEN (patient group); see Table 1. When applicable, the vernacular name of the plants used and their mode of preparation and consumption were noted (Table 1). In cases where the patient was a minor, accompanying parents were solicited to identify the plants used, as well as the formulation and method of application.
General health status and symptoms experienced. This section referred specifically to the health status of the individual at the time of the interview. A checklist was previously established by the treating physician,32 and it was completed according to observations and individual statements. People were also invited to describe the symptoms they experienced prior to their arrival at INEN.
Itinerary of the patients. This last section collected information on the clinical itinerary and personal cancer history of the interviewee.
Table 1.
Questions Included in the Category 4 Questionnaire.
| Question | Questioning Type | Group(s) |
|---|---|---|
| In general, do you take plants on a regular basis to treat your health problems? (regular herbal medicine [HM]) | Closed-ended (yes vs no) | Patient, comparative |
| If so, what plants do you take? | Open-ended | Patient, comparative |
| Which disease(s) you take these plants to treat? | Open-ended | Patient, comparative |
| Could you describe the complete recipe? (plant parts, mode of preparation, and administration) | Open-ended | Patient, comparative |
| Who informed you about these plants? | Open-ended | Patient, comparative |
| What symptoms have you experienced before coming to the hospital? (to complete the checklist given by the physician) | Closed- and open-ended | Patient, comparative |
| Did you take plants to specifically treat the symptoms for which you are attending the hospital? (symptomatic HM) | Closed-ended (yes vs no) | Patient |
| If so, what plants did you take to treat these symptoms? | Open-ended | Patient |
| What did you take these plants for? | Open-ended | Patient |
| For how long did you take these plants? | Open-ended | Patient |
| Could you describe the complete recipe? (plant parts, mode of preparation, and administration) | Open-ended | Patient |
| Who informed you about these plants? | Open-ended | Patient |
In practice, people were interviewed at INEN shortly before or right after their medical consultation with a physician. The semistructured questionnaire was administered via face-to-face interviews conducted by an epidemiologist who was a native Spanish speaker. A photo catalog of 100 plant species was compiled prospectively by an ethnopharmacologist, using information and pictures obtained during previous studies in Peruvian plant markets and health food stores. This photo catalog reviewed species widely used in the Peruvian pharmacopeia and species with a local reputation for treating liver illness, and included pictures of both whole standing plants and packaged, as they can be seen on herbalist stalls in Peru. When the interviewee mentioned a plant or a packaged item, the catalog was shown to him or her in order to confirm the scientific name. Accepted Latin names of plant species were checked according to an established working list.33 When doubts remained, patients or relatives were asked to bring herbal samples to their second medical examination at INEN, in order to deposit specimens in the San Marcos Herbarium (USM) of the Museum of Natural History at the National University of San Marcos (UNMSM) and to allow accurate plant identification by specialists (see Acknowledgements). When it was not possible to assign a binomial name to a plant, for example, when people were not certain about the HM ingested, or they did not know the name of the plant used, or they mentioned vernacular plant names that it was not possible to identify due to a lack of material, HM were recorded as unidentified (UI).
Concurrently, a medical form encompassing patient’s clinical data (ie, personal medical history, tumor presentation, liver function, and physiological, biochemical, and immunological status) was filled out by the treating physician and added to the survey questionnaire to give further information on the clinical status of the patient.
Statistical Analysis
Data from the interviews were inputted by the patient’s interviewer using Microsoft Excel software version 14.4.7 (Microsoft Corporation) and later transferred to MySQL relational database management system (Oracle Corporation), using phpMyAdmin interface software version 4.3.10 (The phpMyAdmin Project). Statistical tests, such as Fisher’s exact test (for comparisons), were performed with a .05 significance level using R statistical software version 3.1.2.34 Chi-squared tests (for comparisons) and the correspondence analysis (for descriptive study) were performed using the R exploratory multivariate data analysis FactoMineR package.35 Holm-Bonferroni sequential correction method was used to adjust multiple comparison families of P values and control the family-wise error rate at the .05 level. Maps were created with QGIS geographic information system version 2.6.36
Results
Survey Data and Sociodemographics of the Population Sample
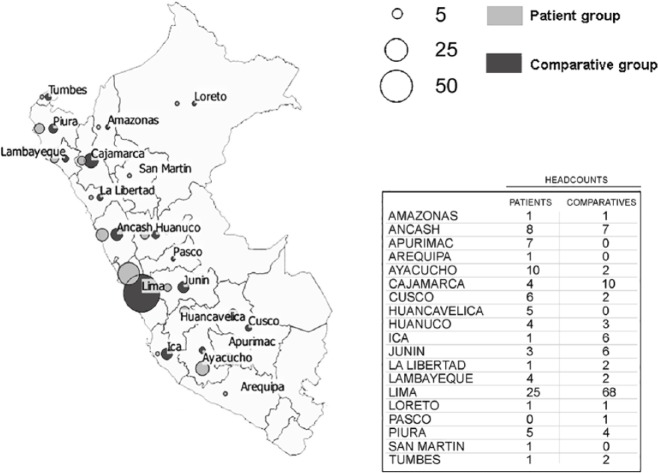
Between April 2013 and August 2014, 117 patients seeking treatment at INEN were diagnosed for hepatic neoplasm development. Eighty-eight patients (75.2%) participated in the survey (patient group). During the same period, 117 individuals visiting the INEN Blood Bank were also interviewed (comparative group). The average duration of the interviews was about 29 minutes, during which interviewees filled out the 6 sections of the questionnaire (Supplemental Document S1). Overall, people originating from 20 regions (out of 25) in Peru were interviewed: patients and comparative individuals were originating from 19 and 16 regions, respectively (Figure 1). A significant proportion of patients with primary liver cancer originated from the Southern-Central Andes, notably from the regions of Apurimac and Ayacucho, which are among the most disadvantaged Peruvian provinces.5,37 The sociodemographic structure of both patient and comparative groups is presented in Table 2. The sex ratio was 1.6, male to female, for both patient and comparative groups. The 2 groups displayed relatively young mean ages: 44.7 years for the patient group and 34.6 years for the comparative group (P < .001). The difference in age of both groups can be explained by both the criteria for blood donor selection in the comparative group and the pathophysiology of the disease in the patient group. However, age was not statistically correlated with the use of TCAM (P > .05). The individuals being treated at INEN were mostly low- and medium-income individuals. The comparative group consisted of persons displaying slightly higher monthly income than people from the patient group (P < .001). This observation is plausibly due to the fact that the ratio of blood donors originating from metropolitan Lima, where wealth is the highest in the country, was higher than in the patient group (Figure 1).37 However, no difference in ethnic composition between the patient group and the comparative group was noted (P > .05).
Figure 1.
Map of the regional headcounts for both patient and comparative groups.
Table 2.
Sociodemographic Features of the Individuals Interviewed.
| Overall | Patient Group | Comparative Group | |
|---|---|---|---|
| Cohort | |||
| Headcount | 205 | 88 | 117 |
| Age (years) | |||
| Mean ± standard deviation | 38.9 ± 17.2 | 44.7 ± 22.5 | 34.6 ± 9.9 |
| Median | 36 | 41 | 34 |
| Interquartile range | 20 | 38.5 | 14.5 |
| Gender | |||
| Female | 77 | 33 | 44 |
| Male | 128 | 55 | 73 |
| Sex ratio (male to female) | 1.6 | 1.6 | 1.6 |
| Incomea (US$) | |||
| Less than 100 | 21 | 19 | 3 |
| Between 100 and 200 | 55 | 38 | 17 |
| Between 200 and 500 | 67 | 25 | 42 |
| Between 500 and 1500 | 48 | 6 | 42 |
| More than 1500 | 13 | 0 | 13 |
Incomes are indicated as household income per month and are estimates converted from Peruvian currency (Nuevo Sol).
Diagnosis and Symptoms
The development of an intrahepatic tumor was confirmed by noninvasive diagnostic imaging (computed axial tomography and abdominal ultrasounds) for the 88 patients included in the survey. Patients indicated they had experienced symptoms related to their hepatic disorder for an average of 4 months prior to their arrival at the hospital: about 7 months for the patients who used symptomatic HM and 3 months for the patients who did not use plant-based medicines (P < .05). There were no significant differences in clinical presentation between patients using or not using HM (all P > .05; Supplemental Figure S1). The symptoms listed by the people interviewed are presented in Table 3. According to physician observations and interviewee statements, symptoms most significantly present in the patient group (compared with the comparative group) were depression (61.4%), stress (anxiety; 61.4%), abdominal pain (dyspepsia; 60.3%), weight loss (59.1%), fatigue (54.5%), poor appetite (anorexia; 48.9%), digestive disorders (53.4%), insomnia (45.4%), nausea (34.1%), and jaundice (icterus; 22.7%); P < .001). Other symptoms, including aphonia, cramp, dehydration, diarrhea, fever (pyrexia), and weakness (asthenia), were also significantly listed by the patient group (P < .01) but came up less frequently (lower than 20%) than the first set of symptoms detailed above (Table 3).
Table 3.
Symptom Pattern in Both Patient and Comparative Groups.
| Symptom Namea | Patient group (%) [Confidence Interval] (n = 88) |
Comparative Group (%) [Confidence Interval] (n = 117) | P |
|---|---|---|---|
| Anorexia | 48.9 [38.5-59.3] | 2.6 [0-5.5] | <.001 |
| Anxiety | 61.4 [51.2-71.6] | 23.1 [15.5-30.7] | <.001 |
| Aphonia | 5.7 [0.9-10.5] | 0 | <.01 |
| Asthenia | 19.3 [11.1-27.5] | 0 | <.001 |
| Back pain | 20.5 [12.1-28.9] | 16.2 [9.5-22.9] | ns |
| Bloating | 12.5 [5.6-19.4] | 7.7 [2.9-12.5] | ns |
| Cephalgia | 14.8 [7.4-22.2] | 6.8 [2.2-11.4] | ns |
| Cramp | 10.2 [3.9-16.5] | 1.7 [0-4] | <.001 |
| Dehydration | 7.9 [2.3-13.5] | 0 | <.001 |
| Depression | 61.4 [51.2-71.6] | 4.3 [0.6-8] | <.001 |
| Diarrhea | 7.9 [2.3-13.5] | 0 | <.001 |
| Digestive disorders | 53.4 [43-63.8] | 5.1 [1.1-9.1] | <.001 |
| Dyspepsia | 60.3 [50.1-70.5] | 0.9 [0-2.6] | <.001 |
| Dyspnea | 5.7 [0.9-10.5] | 0.9 [0-2.6] | ns |
| Erythema | 6.8 [1.5-12.1] | 6 [1.7-10.3] | ns |
| Epistaxis | 3.4 [0-7.2] | 4.3 [0.6-8] | ns |
| Fatigue | 54.5 [44.1-64.9] | 5.1 [1.1-9.1] | <.001 |
| Hematuria | 1.1 [0-3.3] | 0 | ns |
| Hemoptysis | 3.4 [0-7.2] | 0 | ns |
| Icterus | 22.7 [13.9-31.5] | 0 | <.001 |
| Insomnia | 45.4 [35-55.8] | 10.3 [4.8-15.8] | <.001 |
| Irritation | 1.1 [0-3.3] | 2.3 [0-5] | ns |
| Nausea | 34.1 [24.2-44] | 4.3 [0.6-8] | <.001 |
| Paresthesia | 2.3 [0-5.4] | 0.9 [0-2.6] | ns |
| Pyrexia | 12.5 [5.6-19.4] | 0 | <.001 |
| Rash | 3.4 [0-7.2] | 0.9 [0-2.6] | ns |
| Sore throat | 11.4 [4.8-18] | 7.7 [2.9-12.5] | ns |
| Weight loss | 59.1 [48.8-69.4] | 0.9 [0-2.6] | <.001 |
| Other symptoms | 18.2 [10.1-26.3] | 9.4 [4.1-14.7] | ns |
Abbreviation: ns, nonsignificant.
Symptoms are presented in alphabetical order. Percentages are expressed as the proportion of the total patient (n = 88) and comparative (n = 117) population group for the considered symptom. P values are indicated for symptoms that are significantly, positively correlated with the patient group.
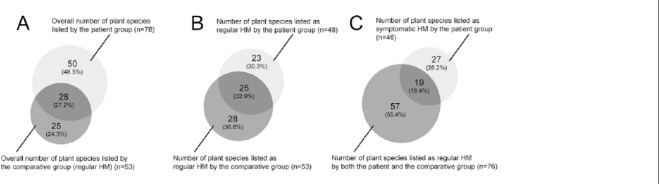
Herbal Medicine Consumption
Details of the survey are presented more extensively in Supplemental Table S1. Sixty-six patients (75%) and 74 individuals from the comparative group (63.2%) claimed to use HM routinely to achieve health promotion and disease prevention (P > .05). In addition, 50 patients (56.8%) had taken plants (symptomatic HM) especially to treat the symptoms associated with their liver disorder. During our survey, 76 plants (13 UI) were listed as routinely used HM, while 46 plants (11 UI) were listed in symptom-triggered HM treatment regimens, culminating in a total of 103 plant species (24 UI) (see Figure 2A-C, Table 4, and Supplemental Table S1). Interviewees using HM were taking an average of 1.7 plant species to achieve general health purposes, whereas the symptomatic HM treatment regimen used by liver cancer patients was based on an average of 1.2 plant species. As mentioned above, it must be noted that 22.2% of the patients and 9.3% of the comparative individuals were using unidentified plants at the time of their interview.
Figure 2.
Set diagrams of the plant species listed during the survey. (A) Overall number of plant species listed by the patient group (n = 78) and the comparative group (n = 53) [n∩ = 28]. (B) Number of plant species listed as regular herbal medicine (HM) by the patient group (n = 48) and the comparative group (n = 53) [n∩ = 25]. (C) Number of plant species listed in symptomatic HM treatments by the patient group (n = 46) and in regular HM by both the patient and comparative groups (n = 76) [n∩ = 19].
Table 4.
Proportion of Use of Each Plant Species for Cancer-Related Symptoms (Symptomatic HM) and for Other Health Purposes (Regular HM).
| Plant Speciesa | Proportion (%) of Use for General Health (Regular HM) | Proportion (%) of Use for Liver Cancer–Related Symptoms (Symptomatic HM) | Overall Ranking [Citation Number] | Distributional Range in Peru38 |
|---|---|---|---|---|
| Allium cepa L. | 0.7 | 0 | 44 [1] | Introduced |
| Allium sativum L. | 0 | 2 | 44 [1] | Introduced |
| Aloe vera (L.) Burm. f. | 3.6 | 20 | 10 [15] | Introduced |
| Aloysia citrodora Palau | 10 | 0 | 11 [14] | Indigenous |
| Ambrosia peruviana Willd. | 0 | 2 | 44 [1] | Indigenous |
| Ananas comosus (L.) Merr. | 2.1 | 0 | 25 [3] | Indigenous |
| Annona muricata L. | 2.8 | 14 | 15 [11] | Introduced |
| Apium graveolens L. | 2.1 | 0 | 25 [3] | Introduced |
| Artemisia absinthium L. | 0.7 | 2 | 32 [2] | Introduced |
| Averrhoa carambola L. | 1.4 | 0 | 32 [2] | Introduced |
| Bidens pilosa L. | 0.7 | 0 | 44 [1] | Indigenous |
| Bixa orellana L. | 3.6 | 4 | 17 [7] | Indigenous |
| Caesalpinia spinosa (Molina) Kuntze | 0.7 | 0 | 44 [1] | Introduced |
| Camellia sinensis | 2.1 | 0 | 25 [3] | Introduced |
| Carica papaya L. | 1.4 | 0 | 32 [2] | Introduced |
| Carya illinoiensis (Wangenh.) K. Koch | 0.7 | 0 | 44 [1] | Introduced |
| Cestrum auriculatum L’Herit. | 0 | 2 | 44 [1] | Indigenous |
| Chamaemelum nobile (L.) All. | 30.7 | 4 | 1 [45] | Introduced |
| Cichorium intybus L. | 0.7 | 0 | 44 [1] | Introduced |
| Citrus aurantium L. | 0 | 2 | 44 [1] | Introduced |
| Citrus limon (L.) Burm. fil. | 0 | 2 | 44 [1] | Introduced |
| Citrus sinensis (L.) Osbeck | 0.7 | 0 | 44 [1] | Introduced |
| Clinopodium pulchellum (Kunth) Govaerts | 0.7 | 0 | 44 [1] | Indigenous |
| Clinopodium speciosum (Hook.) Govaerts | 1.4 | 0 | 32 [2] | Indigenous |
| Copaifera sp. | 0 | 2 | 44 [1] | Indigenous |
| Croton lechleri (Mull.) Arg. | 0 | 4 | 32 [2] | Indigenous |
| Cucurbita pepo L. | 0 | 2 | 44 [1] | Introduced |
| Cymbopogon citratus (DC.) Stapf. | 20.7 | 0 | 2 [29] | Indigenous |
| Cynara scolymus L. | 2.1 | 6 | 19 [6] | Introduced |
| Daucus carota L. | 0.7 | 0 | 44 [1] | Introduced |
| Dysphania ambrosioides (L.) Mosyakin & Clemants | 3.6 | 0 | 21 [5] | Introduced |
| Equisetum sp. | 13.6 | 2 | 6 [20] | Indigenous |
| Erythroxylum coca Lam. | 1.4 | 0 | 32 [2] | Indigenous |
| Eucalyptus sp. | 8.6 | 0 | 14 [12] | Introduced |
| Foeniculum vulgare L. | 0 | 2 | 44 [1] | Introduced |
| Furcraea andina Trel. | 0.7 | 0 | 44 [1] | Indigenous |
| Gentianella alborosea (Gilg) Fabris | 0.7 | 0 | 44 [1] | Indigenous |
| Hordeum vulgare L. | 10 | 8 | 9 [18] | Indigenous |
| Lepidium meyenii Walp. | 0.7 | 0 | 44 [1] | Indigenous |
| Linum usitatissimum L. | 12.8 | 8 | 5 [22] | Introduced |
| Malus pumila Mill. | 1.4 | 0 | 32 [2] | Introduced |
| Malva sp. | 3.6 | 0 | 21 [5] | Introduced |
| Medicago sativa L. | 1.4 | 0 | 32 [2] | Introduced |
| Melissa officinalis L. | 1.4 | 0 | 32 [2] | Introduced |
| Mentha sp. | 4.3 | 0 | 19 [6] | Introduced |
| Minthostachys mollis (Benth.) Griseb. | 12.8 | 4 | 6 [20] | Indigenous |
| Morinda citrifolia L. | 0 | 14 | 17 [7] | Introduced |
| Nasturtium officinale W.T. Aiton | 0 | 2 | 44 [1] | Introduced |
| Ocimum basilicum L. | 0.7 | 0 | 44 [1] | Introduced |
| Oenothera rosea L’Héritier ex. Aiton | 0.7 | 0 | 44 [1] | Indigenous |
| Opuntia ficus-indica (L.) Mill. | 0.7 | 0 | 44 [1] | Introduced |
| Origanum vulgare L. | 7.8 | 4 | 12 [13] | Introduced |
| Passiflora edulis Sims | 0.7 | 0 | 44 [1] | Introduced |
| Peperomia sp. | 0 | 2 | 44 [1] | Indigenous |
| Persea americana Mill. | 0.7 | 0 | 44 [1] | Indigenous |
| Petroselinum crispum | 0 | 4 | 32 [2] | Introduced |
| Peumus boldus Molina | 14.3 | 18 | 2 [29] | Introduced |
| Phalaris canariensis L. | 0.7 | 2 | 32 [2] | Indigenous |
| Phyllanthus sp. | 4.3 | 10 | 15 [11] | Indigenous |
| Pimpinella anisum L. | 16.4 | 4 | 4 [25] | Introduced |
| Piper sp. | 3.6 | 0 | 21 [5] | Indigenous |
| Plantago sp. | 9.3 | 14 | 6 [20] | Indigenous |
| Rosmarinus officinalis L. | 0.7 | 0 | 44 [1] | Introduced |
| Ruta chalepensis L. | 0.7 | 2 | 32 [2] | Introduced |
| Salvia officinalis L. | 0.7 | 0 | 44 [1] | Introduced |
| Sambucus peruviana Kunth | 0.7 | 0 | 44 [1] | Indigenous |
| Schinus molle L. | 0.7 | 0 | 44 [1] | Indigenous |
| Schkuhria pinnata (Lam.) Kuntze ex Thell. | 0.7 | 0 | 44 [1] | Indigenous |
| Senecio sp. | 0.7 | 2 | 32 [2] | Indigenous |
| Solanum peruvianum L. | 0 | 2 | 44 [1] | Indigenous |
| Solanum tuberosum L. | 2.8 | 0 | 24 [4] | Indigenous |
| Spartium junceum L. | 0.7 | 0 | 44 [1] | Introduced |
| Taraxacum campylodes G.E. Haglund | 0 | 6 | 25 [3] | Indigenous |
| Thymus vulgaris L. | 0 | 2 | 44 [1] | Introduced |
| Tilia sp. | 0.7 | 0 | 44 [1] | Introduced |
| UI | 9.3 | 22.2 | n/a | n/a |
| Uncaria tomentosa (Willd. ex Schult.) D.C. | 4.3 | 14 | 12 [13] | Indigenous |
| Urtica urens L. | 0.7 | 0 | 44 [1] | Introduced |
| Valeriana sp. | 2.1 | 0 | 25 [3] | Indigenous |
| Zea mays L. | 2.1 | 0 | 25 [3] | Indigenous |
Abbreviations: n/a, not applicable; UI, unidentified plant species.
Plants are presented in alphabetical order according to their scientific name.33 For further details on the vernacular name and collected data of the unidentified plant species, see Supplemental Table S1. Percentages are expressed as the proportion of interviewees that listed the considered plant species as part of their treatment allocation; that is, regular and/or symptomatic HM. Number of interviewees (patients + comparatives) using regular HM (n = 140); number of interviewees (patients) taking symptomatic HM (n = 50).
Chamaemelum nobile (P < .01) was significantly associated with the regular HM regimen, and A citrodora, C citratus, Equisetum sp, Eucalyptus sp, M mollis, P anisum, and Piper sp displayed a similar trend to be more consumed in this regimen (P > .05). Among the plants listed, A vera (P < .01) and M citrifolia (P < .001) were significantly associated with symptomatic HM treatment. While not statistically significant, A muricata, Phyllanthus sp, Plantago sp, and U tomentosa showed a trend to be used in symptomatic HM regimens as well (P > .05; Table 4). Additionally, A sativum, A peruviana, C auriculatum, C limon, Copaifera sp, C pepo, F vulgare, N officinale, Peperomia sp, S peruvianum, T vulgaris (all with 1 citation), C lechleri (2 citations), and T campylodes (3 citations) were listed only as symptomatic HM (Table 4). Reversely, C citratus (P < .001) was significantly excluded from the symptomatic HM regimens. The same observation could be made for A citriodora, Eucalyptus sp, and Piper sp, although not reaching the same level of significance (P > .05). Correspondence analysis did not bring out a clear-cut pattern of symptomatic plants usage in the HM anticancer treatment regimens: no plant was correlated with a specific symptom, but rather with an overall poor health status due to cancer (Supplemental Figures S2-S5).
The use of only 2 plants related significantly to the origin of the interviewees: A vera is consumed mainly in the rainforest regions (P < .01), whereas M mollis was taken preferentially by people from the Andes (P < .01). Patients were advised on these plants primarily by their nuclear family (parents) in 60.5% of cases, secondarily by relatives (extended family, friends, and neighbors) in 12.2% of cases, and finally by herbalists from local street markets, media, or health care professionals in 11.6%, 3.5%, and 1.7% of cases, respectively (Supplemental Table S1). These plants were consumed mostly in beverages (cold extractions, infusions, decoctions, macerations, and juices) or used as topical treatments, such as in poultices applied directly to the painful area (Supplemental Table S1).
Discussion
According to the World Health Organization, 65% of the world population, about 390 million people in Latin America, rely on traditional medicine for their primary health care.27,29 Meanwhile, along with vitamins, herbalism is among the biologically based TCAM most frequently used by cancer patients,39-41 notably in the developing world. Our study confirmed this figure in Peru with 56.8% of the patients interviewed using HM to treat their liver cancer-associated symptoms.
Most of the plant species listed as regular HM in our survey were commonplace, such as A citriodora, C citratus, C nobile, Eucalyptus spp, M mollis, P anisum, P boldus, and Plantago spp (Table 4), with a large fraction of them originating from Asia or Europe.38 These plants can be found easily in Peruvian markets or in home gardens, notably in the coastal and Andean regions of Peru. Beverages made from these plants are largely consumed in Peru for the purposes to stay in good health, to improve the functioning of the body, as digestive aids, or even for their soothing effect. Traditionally, there are different types of social beverages of this sort in Peru: (a) the emolientes are hot and sweet herbal drinks prepared with roasted grains of H vulgare and herb fragments (Equisetum spp and P boldus); (b) the refrescos are, in the Andean and coastal areas of Peru, hot mucilaginous beverages made from aromatic plants (A citriodora, C citratus, F vulgare, and P anisum) boiled together with seeds of L usitatissimum;24 and (c) the extractos are juices obtained from freshly pressed plants or from gel (A vera and M sativa). Moreover, people often drink vegetable and fruit juices (A carambola and C papaya) and infused herb teas called mates (A citriodora, C nobile, E coca, and Mentha spp). Thus, some plant species listed in regular HM during our survey appear to be part of the food-medicine continuum42 and reflect the habits and practices of the Peruvian population. Furthermore, the high number of plant species that are listed in our survey and that are introduced in Peru should be questioned, as no study has previously reported this trend (Table 4). It can be hypothesized that this feature ties with a preventive attitude, which has not been fairly documented hitherto in the Peruvian population. Indeed, a similar trend was observed in a study on traditional medicinal practices for malaria in French Guiana, where most of plant species used in prevention are introduced ones.43
In the patient group, the use of regular HM did not necessarily lead to the use of symptomatic HM treatments against liver disorder: while 75% of the patients initially used medicinal plants, the proportion of them taking symptom-focused HM lowered to 56.8%. Nonetheless, compared with the plant species used in regular HM, it can be observed in symptomatic HM treatments that there is a shift in the choice of plant species, as an attempt to provide an appropriate response to the health problem (Figure 2A and C). Indeed, for a significant proportion, plant species used in symptomatic HM treatments were different from those used as regular HM (Figure 2C). Plant species used in TCAM treatments for liver cancer included statistically significantly A vera and M citrifolia, as well as, to a lesser extent, A sativum, A peruviana, A muricata, C auriculatum, C limon, Copaifera sp, C lechleri, C pepo, F vulgare, N officinale, Peperomia sp, P boldus, Phyllanthus sp, Plantago sp, S peruvianum, T campylodes, T vulgaris, and U tomentosa (Table 4). By contrast, patients avoided in their symptomatic HM treatments some other plant species in their symptomatic HM treatments, including A citriodora, C citratus, Eucalyptus sp, and Piper sp.
Some plants listed in symptomatic HM treatments have a reputation of being beneficial to the liver. For example, N officinale and T campylodes are mainly used in Peru for their activity on the liver, and Phyllanthus niruri is frequently used in cases of hepatitis and icterus.25,44 Their traditional reputation is known in the regions where these species grow and they have been commercialized as medicinal plants.45 Interestingly, these 3 plants pooled are used at the most by merely 18% of the Peruvian patients with liver cancer (Table 4), suggesting that in the great majority of cases, tumors could appear without liver prodromes.5 Additionally, F vulgare is often used for bloating and digestive problems.44 Generally prepared in the form of a poultice, Peperomia and Plantago spp are prized for their general anti-inflammatory activity, with a special indication in case of gastritis for Peperomia spp.44,46
While it remains unsubstantiated by relevant clinical evidence, a significant fraction of the plant species used in symptomatic HM have a reputation of being effective for cancer. This is notably the case for A vera, A muricata, Copaifera spp, C lechleri, M citrifolia, and U tomentosa.44 U tomentosa, in particular, has received a lot of attention and several publications report its activity on the immune system, its anti-inflammatory properties, and its possible efficacy against cancer.47-51 The popularity of M citrifolia as a dietary supplement and natural health enhancer is increasing throughout the world. Its fruits, either unprocessed or in the form of extracts, can be found in every naturopathic store in Peru and are sold as a panacea, which has also presumed anticancer properties.52 Several scientific works have been recently undertaken on C lechleri, which displays cicatrizing and anti-inflammatory and anti-ulcerogenic properties. In addition, extracts of C lechleri have shown in vitro and in vivo anticancer activity.53 Copaifera spp is a popular medicinal plant due to its alleged anti-inflammatory and anti-infectious activities. In Peru, the resin of Copaifera spp has now gained the reputation of having anticancer properties and some studies have been conducted that support this claim.54,55 Likewise, anticancer activity of A muricata has been studied for many years and this plant is commercially produced as tablets in Peru under the generic name of Graviola.29,56-58 Finally, A vera gel has been partially investigated for its anticancer activity,59,60 but further studies are required to confirm its potential.61
Despite the lack of a formal diagnosis prior to their arrival at a cancer care center, these observations demonstrate that, in Peru, a high percentage of patients with liver cancer orient their TCAM practices toward the few HM that have the local reputation of treating “cancer”, regardless of the perception about the disease among these people without specific medical education.62 They also use plants to improve the symptomatic presentation of their illness (abdominal pain, digestive disorders with nausea, jaundice, and mood disorders) (Table 3). Unfortunately, it is unlikely that these plant species used alone have a beneficial impact on the hepatocarcinogenic process (Supplemental Figure S1).
There are some limitations to recognize in the present study. Because patients self-reported information retrospectively, there is potential for recall bias that could be conducive to misclassifications of symptoms and HM allocation. However, the inclusion in the survey design of noncancerous individuals as a comparative group should have limited such effect, providing baseline information on the usage of plants in regular HM among the general Peruvian population (Figure 2B). Also, this study included a relatively small number of participants. Taking into account both the wealth of the Peruvian pharmacopeia and the complex clinical picture of cancer, this could have resulted in some dispersion that lowered the discriminating power of the statistical tests, notably in the correspondence analysis (Supplemental Figures S2-S5). Hierarchical clustering, as well as correction methods, has been applied in order to narrow this contingency. Finally, despite the best efforts, some plants species used by the interviewees remained unidentified (n = 24).
Conclusions
Our findings demonstrate that a significant proportion of Peruvian patients with liver cancer living in remote Peruvian provinces (but not exclusively) use HM as their first therapeutic resource prior to their decision to travel to the country’s capital to seek treatment from a cancer care center, on average, 4 months later. This behavior might be explained by the fact that access to health care is still very poor in some remote areas, notably concerning cancer diagnosis and treatment,63,64 and that traveling to the metropolis represents a significant expense for low-income people.65 The difficulties in traveling to the cancer care center in Lima might delay patients in seeking biomedical treatment and a proper management of their disease,66 and orient them toward HM before their relatives until the absolute need to travel arises. Thus, it is important to consider incorporating into the health intervention strategies of Plan Esperanza and CMS-EsSalud a wide-reaching educational campaign about TCAM in cancer care. This campaign would aim to promote awareness of this life-threatening disease among the at-risk Peruvian population and to summarize both the benefits and the limitations of TCAM practices. People should be encouraged to promptly consult a cancer care center, such as INEN, and should receive information aiming to change potential misperceptions about the deemed anticancer properties of plants, to deter their use as a primary treatment for cancer.
Supplemental Material
Supplemental material, ICT_681642-_Supplemental_Table_S1 for Herbal Medicine Practices of Patients With Liver Cancer in Peru: A Comprehensive Study Toward Integrative Cancer Management by Teresa Rojas Rojas, Geneviève Bourdy, Eloy Ruiz, Juan-Pablo Cerapio, Pascal Pineau, Jacques Gardon, Franco Doimi, Xavier Deparis, Eric Deharo and Stéphane Bertani in Integrative Cancer Therapies
Supplemental Material
Supplemental material, Supplemental_Document_S1 for Herbal Medicine Practices of Patients With Liver Cancer in Peru: A Comprehensive Study Toward Integrative Cancer Management by Teresa Rojas Rojas, Geneviève Bourdy, Eloy Ruiz, Juan-Pablo Cerapio, Pascal Pineau, Jacques Gardon, Franco Doimi, Xavier Deparis, Eric Deharo and Stéphane Bertani in Integrative Cancer Therapies
Acknowledgments
The authors express their gratitude to the interviewees whose participation was essential to the achievement of this study. The authors are grateful to Sandro Casavilca Zambrano from the INEN Department of Pathology, Enrique Argumanis Sánchez from the INEN Blood Bank, and Karina Cancino Maldonado, Dany Cordova Mamani, Macarena Farías Loza, Marlene Nuñez Salinas, and Maricarmen Valera Quiroz from the INEN Tumor Bank for their leadership in organizing the interviews with the patients; Joaquina Albán Castillo, Severo Baldeón Malpartida, and Hamilton Beltrán Santiago from USM at UNMSM for their support in determining plant specimens; Hervé Chaudet, Joffrey Marchi, and Rafael Vives from CESPA for their technical support; Agnès Marchio from the Institut Pasteur and Javier Herrera, Valérie Jullian, and Michel Sauvain from IRD for their critical discussions; and Elizabeth Elliott, Brian Gadd, and Alice Kan for their valuable editorial assistance.
Footnotes
Authors’ Note: The funding agencies did not participate in the design, analysis, interpretation of data, and writing of the article.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: TRR was a recipient of a doctoral fellowship from Innóvate Perú (069-FINCyT-BDE-2014); JPC was a recipient of a doctoral fellowship from the Peruvian National Council for Science and Technology (212-2015-FONDECYT); ER and FD were supported by the Young Research Teams Associated with IRD Program (JEAI-INCAncer); and GB, PP, JG, ED, and SB were supported by the Third Cancer Plan of the French National Alliance for Life Sciences and Health (ENV201408).
Supplemental Material:Supplementary material is available for this article online.
References
- 1. Ferlay J, Soerjomataram I, Dikshit R, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136:E359-E386. [DOI] [PubMed] [Google Scholar]
- 2. Bray F, Jemal A, Grey N, Ferlay J, Forman D. Global cancer transitions according to the Human Development Index (2008-2030): a population-based study. Lancet Oncol. 2012;13:790-801. [DOI] [PubMed] [Google Scholar]
- 3. Bray F, Piñeros M. Cancer patterns, trends and projections in Latin America and the Caribbean: a global context. Salud Publica Mex. 2018;58:104-117. [DOI] [PubMed] [Google Scholar]
- 4. Dirección General de Epidemiología. Análisis de la Situación del Cáncer en el Perú, 2013. Lima, Peru: Dirección General de Epidemiología; 2013. [Google Scholar]
- 5. Bertani S, Pineau P, Loli S, et al. An atypical age-specific pattern of hepatocellular carcinoma in Peru: a threat for Andean populations. PLoS One. 2013;8:e67756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ruiz E, Rojas Rojas T, Berrospi F, et al. Hepatocellular carcinoma surgery outcomes in the developing world: a 20-year retrospective cohort study at the National Cancer Institute of Peru. Heliyon. 2018;2:e00052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Marchio A, Bertani S, Rojas Rojas T, et al. A peculiar mutation spectrum emerging from young Peruvian patients with hepatocellular carcinoma. PLoS One. 2014;9:e114912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bodeker G, Burford G. Traditional, Complementary and Alternative Medicine: Policy and Public Health Perspectives. London, England: Imperial College Press; 2007. [Google Scholar]
- 9. Pan American Health Organization, EsSalud. Estudio Costo-Efectividad: Programa Nacional de Medicina Complementaria. Lima, Peru: EsSALUD; 2000. [Google Scholar]
- 10. Luján-Carpio E, Lizarraga-Castañeda Z, Mayor-Vega A, Medrano-Canchari K, Medina-Salazar H, Goicochea-Lugo S. El Servicio de Medicina Complementaria de EsSalud, una alternativa en el sistema de salud peruano. Rev Medica Hered. 2014;25:105-106. [Google Scholar]
- 11. Torrejón MS. Medicina complementaria en EsSalud: 18 años cuidando la salud de los asegurados. Rev Peru Med Integrativa. 2018;1(2):3-4. [Google Scholar]
- 12. Swenson JJ, Young BE, Beck S, et al. Plant and animal endemism in the eastern Andean slope: challenges to conservation. BMC Ecol. 2012;12:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hammond GB, Fernández ID, Villegas LF, Vaisberg AJ. A survey of traditional medicinal plants from the Callejón de Huaylas, Department of Ancash, Peru. J Ethnopharmacol. 1998;61:17-30. [DOI] [PubMed] [Google Scholar]
- 14. Bussmann RW, Sharon D. Traditional medicinal plant use in Northern Peru: tracking two thousand years of healing culture. J Ethnobiol Ethnomed. 2006;2:47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Gonzales GF, Valerio LG. Medicinal plants from Peru: a review of plants as potential agents against cancer. Anticancer Agents Med Chem. 2006;6:429-444. [DOI] [PubMed] [Google Scholar]
- 16. Kvist LP, Christensen SB, Rasmussen HB, Mejia K, Gonzalez A. Identification and evaluation of Peruvian plants used to treat malaria and leishmaniosis. J Ethnopharmacol. 2006;106:390-402. [DOI] [PubMed] [Google Scholar]
- 17. Odonne G, Bourdy G, Castillo D, et al. Ta’ta’, Huayani: perception of leishmaniasis and evaluation of medicinal plants used by the Chayahuita in Peru. Part II. J Ethnopharmacol. 2009;126:149-158. [DOI] [PubMed] [Google Scholar]
- 18. Valadeau C, Pabon A, Deharo E, et al. Medicinal plants from the Yanesha (Peru): evaluation of the leishmanicidal and antimalarial activity of selected extracts. J Ethnopharmacol. 2009;123:413-422. [DOI] [PubMed] [Google Scholar]
- 19. Luziatelli G, Sørensen M, Theilade I, Mølgaard P. Asháninka medicinal plants: a case study from the native community of Bajo Quimiriki, Junín, Peru. J Ethnobiol Ethnomed. 2010;6:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Rehecho S, Uriarte-Pueyo I, Calvo J, Vivas LA, Calvo MI. Ethnopharmacological survey of medicinal plants in Nor-Yauyos, a part of the Landscape Reserve Nor-Yauyos-Cochas, Peru. J Ethnopharmacol. 2011;133:75-85. [DOI] [PubMed] [Google Scholar]
- 21. Polesna L, Polesny Z, Clavo MZ, Hansson A, Kokoska L. Ethnopharmacological inventory of plants used in Coronel Portillo Province of Ucayali Department, Peru. Pharm Biol. 2011;49:125-136. [DOI] [PubMed] [Google Scholar]
- 22. Ruiz L, Ruiz L, Maco M, Cobos M, Gutierrez-Choquevilca AL, Roumy V. Plants used by native Amazonian groups from the Nanay River (Peru) for the treatment of malaria. J Ethnopharmacol. 2011;133:917-921. [DOI] [PubMed] [Google Scholar]
- 23. Odonne G, Valadeau C, Alban-Castillo J, Stien D, Sauvain M, Bourdy G. Medical ethnobotany of the Chayahuita of the Paranapura basin (Peruvian Amazon). J Ethnopharmacol. 2013;146:127-153. [DOI] [PubMed] [Google Scholar]
- 24. de la Cruz MG, Malpartida SB, Santiago HB, Jullian V, Bourdy G. Hot and cold: medicinal plant uses in Quechua speaking communities in the high Andes (Callejón de Huaylas, Ancash, Peru). J Ethnopharmacol. 2014;155:1093-1117. [DOI] [PubMed] [Google Scholar]
- 25. Carraz M, Lavergne C, Jullian V, et al. Antiproliferative activity and phenotypic modification induced by selected Peruvian medicinal plants on Human hepatocellular carcinoma Hep3B cells. J Ethnopharmacol. 2015;166:185-199. [DOI] [PubMed] [Google Scholar]
- 26. Vidaurre T, Abugattas J, Santos C, et al, et al. Plan Esperanza: a model for cancer prevention and control in Peru. In: Magrath I. ed. Cancer Control 2015. 2nd ed. London, England: Global Health Dynamics; 2015:130-137. [Google Scholar]
- 27. World Health Organization. WHO Traditional Medicine Strategy: 2014-2023. Geneva, Switzerland: World Health Organization; 2013. [Google Scholar]
- 28. Goss PE, Lee BL, Badovinac-Crnjevic T, et al. Planning cancer control in Latin America and the Caribbean. Lancet Oncol. 2013;14:391-436. [DOI] [PubMed] [Google Scholar]
- 29. Salaverry O. Back to the roots: traditional medicine for cancer control in Latin America and the Caribbean. Lancet Oncol. 2013;14:384. [DOI] [PubMed] [Google Scholar]
- 30. Instituto Nacional de Enfermedades Neoplásicas. Plan Estratégico Institucional 2011-2015. Surquillo, Peru: Instituto Nacional de Enfermedades Neoplásicas; March 2011. [Google Scholar]
- 31. Nieuwenhuijsen MJ. Design of exposure questionnaires for epidemiological studies. Occup Environ Med. 2005;62:272-280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Younossi Z, Guyatt G, Kiwi M, Boparai N, King D. Development of a disease specific questionnaire to measure health related quality of life in patients with chronic liver disease. Gut. 1999;45:295-300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. The Plant List, version 1.1. http://www.theplantlist.org/. Accessed November 22, 2016.
- 34. R Core Team. R: a language and environment for statistical computing. https://www.r-project.org/. Accessed November 22, 2016.
- 35. Husson F, Josse J, Le S, Mazet J. FactoMineR: multivariate exploratory data analysis and data mining. R package version 1.24. http://www2.uaem.mx/r-mirror/web/packages/FactoMineR/FactoMineR.pdf. Accessed November 22, 2016.
- 36. QGIS Development Team. QGIS geographic information system. http://www.qgis.org/. Accessed November 22, 2016.
- 37. Instituto Nacional de Estadística e Informática. Perú: Perfil de la Pobreza por Dominios Geográficos, 2004-2015. Lima, Peru: Instituto Nacional de Estadística e Informática; 2018. [Google Scholar]
- 38. Roskov Y, Abucay L, Orrell T, et al. eds. Species 2000 & ITIS Catalogue of Life. www.catalogueoflife.org/col. Published September 2018. Accessed November 22, 2016.
- 39. Girgis A, Adams J, Sibbritt D. The use of complementary and alternative therapies by patients with cancer. Oncol Res. 2005;15:281-289. [DOI] [PubMed] [Google Scholar]
- 40. Adams J, Valery PC, Sibbritt D, Bernardes CM, Broom A, Garvey G. Use of traditional Indigenous medicine and complementary medicine among Indigenous cancer patients in Queensland, Australia. Integr Cancer Ther. 2015;14:359-365. [DOI] [PubMed] [Google Scholar]
- 41. Arslan C, Guler M. Alternative medicine usage among solid tumour patients receiving chemotherapy. Eur J Cancer Care (Engl). 2017;26(Themed section: Cancer and work):e12530. [DOI] [PubMed] [Google Scholar]
- 42. Pieroni A, Quave CL. Functional foods or food-medicines? On the consumption of wild plants among Albanians and Southern Italians in Lucania. In: Pieroni A, Price LL. eds. Eating and Healing: Traditional Food as Medicine. Binghamton, NY: Haworth Press, Inc; 2006:101-129. [Google Scholar]
- 43. Vigneron M, Deparis X, Deharo E, Bourdy G. Antimalarial remedies in French Guiana: a knowledge attitudes and practices study. J Ethnopharmacol. 2005;98:351-360. [DOI] [PubMed] [Google Scholar]
- 44. Brack Egg A. Diccionario Enciclopedico de Plantas Utiles del Perú. Cuzco, Peru: Programa de las Naciones Unidas para el Desarrollo; Centro de Estudios Regionales Andinos Bartolomé de Las Casas; 1999. [Google Scholar]
- 45. Robineau L, Edna-Caribe. Farmacopea Vegetal Caribeña. Fort-de-France, Martinique, FWI; Santo Domingo, Républica Dominicana: Ediciones Emile Désormeaux; Edna-Caribe; 1997. [Google Scholar]
- 46. Villegas LF, Fernández ID, Maldonado H, et al. Evaluation of the wound-healing activity of selected traditional medicinal plants from Peru. J Ethnopharmacol. 1997;55:193-200. [DOI] [PubMed] [Google Scholar]
- 47. Rojas-Duran R, González-Aspajo G, Ruiz-Martel C, et al. Anti-inflammatory activity of mitraphylline isolated from Uncaria tomentosa bark. J Ethnopharmacol. 2012;143:801-804. [DOI] [PubMed] [Google Scholar]
- 48. Caon T, Kaiser S, Feltrin C, et al. Antimutagenic and antiherpetic activities of different preparations from Uncaria tomentosa (cat’s claw). Food Chem Toxicol. 2014;66:30-35. [DOI] [PubMed] [Google Scholar]
- 49. Dietrich F, Kaiser S, Rockenbach L, et al. Quinovic acid glycosides purified fraction from Uncaria tomentosa induces cell death by apoptosis in the T24 Human bladder cancer cell line. Food Chem Toxicol. 2014;67:222-229. [DOI] [PubMed] [Google Scholar]
- 50. Montserrat-de la Paz S, de la Puerta R, Fernandez-Arche A, et al. Pharmacological effects of mitraphylline from Uncaria tomentosa in primary Human monocytes: skew toward M2 macrophages. J Ethnopharmacol. 2015;170:128-135. [DOI] [PubMed] [Google Scholar]
- 51. Zhang Q, Zhao JJ, Xu J, Feng F, Qu W. Medicinal uses, phytochemistry and pharmacology of the genus Uncaria. J Ethnopharmacol. 2015;173:48-80. [DOI] [PubMed] [Google Scholar]
- 52. Abou Assi R, Darwis Y, Abdulbaqi IM, Khan AA, Vuanghao L, Laghari MH. Morinda citrifolia (Noni): a comprehensive review on its industrial uses, pharmacological activities, and clinical trials. Arab J Chem. 2017;10:691-707. [Google Scholar]
- 53. Alonso-Castro AJ, Ortiz-Sánchez E, Domínguez F, et al. Antitumor effect of Croton lechleri Mull. Arg. (Euphorbiaceae). J Ethnopharmacol. 2012;140:438-442. [DOI] [PubMed] [Google Scholar]
- 54. Ohsaki A, Yan LT, Ito S, Edatsugi H, Iwata D, Komoda Y. The isolation and in vivo potent antitumor activity of clerodane diterpenoid from the oleoresin of the Brazilian medicinal plant, Copaifera langsdorfi desfon. Bioorg Med Chem Lett. 1994;4:2889-2892. [Google Scholar]
- 55. Gomes N, de M, Rezende C, de M, Fontes SP, et al. Antineoplasic activity of Copaifera multijuga oil and fractions against ascitic and solid Ehrlich tumor. J Ethnopharmacol. 2008;119:179-184. [DOI] [PubMed] [Google Scholar]
- 56. Minari JB, Okeke U. Chemopreventive effect of Annona muricata on DMBA-induced cell proliferation in the breast tissues of female albino mice. Egypt J Med Hum Genet. 2014;15:327-334. [Google Scholar]
- 57. Zorofchian Moghadamtousi S, Karimian H, Rouhollahi E, Paydar M, Fadaeinasab M, Abdul Kadir H. Annona muricata leaves induce G1 cell cycle arrest and apoptosis through mitochondria-mediated pathway in human HCT-116 and HT-29 colon cancer cells. J Ethnopharmacol. 2014;156:277-289. [DOI] [PubMed] [Google Scholar]
- 58. Sun S, Liu J, Zhou N, Zhu W, Ping Dou Q, Zhou K. Isolation of three new annonacous acetogenins from graviola fruit (Annona muricata) and their anti-proliferation on Human prostate cancer cell PC-3. Bioorg Med Chem Lett. 2018;26:4382-4385. [DOI] [PubMed] [Google Scholar]
- 59. Radha MH, Laxmipriya NP. Evaluation of biological properties and clinical effectiveness of Aloe vera: a systematic review. J Tradit Complement Med. 2015;5:21-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Shalabi M, Khilo K, Zakaria MM, Elsebaei MG, Abdo W, Awadin W. Anticancer activity of Aloe vera and Calligonum comosum extracts separately on hepatocellular carcinoma cells. Asian Pac J Trop Biomed. 2015;5:375-381. [Google Scholar]
- 61. Cathcart P, Stebbing J. Aloe vera, a natural cancer soother? Lancet Oncol. 2018;17:421. [DOI] [PubMed] [Google Scholar]
- 62. McGrath P, Holewa H, Ogilvie K, Rayner R, Patton MA. Insights on Aboriginal peoples’ views of cancer in Australia. Contemp Nurse. 2006;22:240-254. [DOI] [PubMed] [Google Scholar]
- 63. Moore SP, Forman D, Piñeros M, Fernández SM, Oliveira Santos M, Bray F. Cancer in Indigenous people in Latin America and the Caribbean: a review. Cancer Med. 2014;3:70-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Cazap E, Magrath I, Kingham TP, Elzawawy A. Structural barriers to diagnosis and treatment of cancer in low- and middle-income countries: the urgent need for scaling up. J Clin Oncol. 2018;34:14-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Knaul F, Horton S, Yerramilli P, Gelband H, Atun R. Financing cancer care in low-resource settings. In: Gelband H, Jha P, Sankaranarayanan R, Horton S. eds. Cancer: Disease Control Priorities. Vol. 3 3rd ed. Washington, DC: World Bank; 2015:281-294. [PubMed] [Google Scholar]
- 66. Shahid S, Finn L, Bessarab D, Thompson SC. Understanding, beliefs and perspectives of Aboriginal people in Western Australia about cancer and its impact on access to cancer services. BMC Health Serv Res. 2009;9:132. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, ICT_681642-_Supplemental_Table_S1 for Herbal Medicine Practices of Patients With Liver Cancer in Peru: A Comprehensive Study Toward Integrative Cancer Management by Teresa Rojas Rojas, Geneviève Bourdy, Eloy Ruiz, Juan-Pablo Cerapio, Pascal Pineau, Jacques Gardon, Franco Doimi, Xavier Deparis, Eric Deharo and Stéphane Bertani in Integrative Cancer Therapies
Supplemental material, Supplemental_Document_S1 for Herbal Medicine Practices of Patients With Liver Cancer in Peru: A Comprehensive Study Toward Integrative Cancer Management by Teresa Rojas Rojas, Geneviève Bourdy, Eloy Ruiz, Juan-Pablo Cerapio, Pascal Pineau, Jacques Gardon, Franco Doimi, Xavier Deparis, Eric Deharo and Stéphane Bertani in Integrative Cancer Therapies