Abstract
Background: Distal radius malunions lead to functional deficits. This study compares isolated ulnar shortening osteotomy (USO) to distal radius osteotomy (DRO) for the treatment of ulnar impaction syndrome following distal radius malunion. Methods: We retrospectively reviewed 11 patients with extra-articular distal radius malunions treated for ulnar impaction with isolated USO. This group was compared to a 1:1 age- and sex-matched cohort treated with isolated DRO for the same indication. Pain visual analog scale (VAS), wrist motion, grip strength, radiographic parameters, and perioperative complications were analyzed. Mean follow-up was 14.8 months. Results: VAS scores improved. Wrist range of motion improved in both cohorts with the exception of radial deviation, pronation, and supination in the USO cohort, which decreased from a mean of 17°-16°, 67°-57°, and 54°-52°, respectively. There was no significant difference between groups in regard to change in pain or range of motion, with the exception of pronation and ulnar deviation. The mean tourniquet time was shorter in the USO group. The final ulnar variance was 1.8 mm negative in the USO group and 1.1 mm positive in the DRO group. There was 1 reoperation following USO for painful nonunion, while there were 2 reoperations following DRO for persistent ulnar impaction. Conclusions: An improvement in range of motion, grip strength, and VAS with restoration of the radioulnar length relationship was observed in both cohorts. USO is a simpler procedure with a shorter tourniquet time that can be an attractive alternative to DRO for ulnar impaction syndrome after distal radius malunions.
Keywords: ulnar shortening osteotomy, distal radius corrective osteotomy, osteotomy, distal radius malunion, radius
Introduction
Distal radius fractures are the most common fractures of the upper extremity, representing up to 3% of all upper extremity injuries with an annual incidence of 640 000 cases per year in the United States alone.6 Mismanagement of these injuries often results in radial shortening as the main deformity leading to potential radioulnar variance disturbances, associated triangular fibrocartilage complex (TFCC), and distal radioulnar joint (DRUJ) derangements. This can lead to ulnar impaction syndrome secondary to malunion causing pain, loss of motion, decreased grip and pinch strength, and eventual varying degrees of osteoarthritis and debility.24 Various surgical interventions have been described for the management of extra-articular distal radius malunions causing ulnar impaction syndrome, including corrective distal radius osteotomy (DRO) and ulnar shortening osteotomy (USO).7 The goal of surgery in ulnar impaction syndrome after distal radius malunions without significant articular involvement or substantial derangements of volar tilt or radial inclination is to correct the length relationship between the radius and ulna.
DRO has been reported to have promising results in patients with painful malunions and angulations greater than 25°. However, it is a technically challenging surgery with a substantial operative time and often requires additional procedures such as bone grafting and concomitant ulnar osteotomies.1,13,22,23,27 Many of these patients are younger with active lifestyles that cannot afford the limitations associated with multiple procedures.29
Some reports have shown acceptable outcomes after USO for the treatment of ulnar impaction syndrome.2,3,8,11,12,15,18,25,26 Many studies, however, have noted high complication rates due to either plate failure or nonunions requiring further surgical interventions.4,5 In recent years, there have been numerous advances in the field of biomaterials and development of various cutting guides for corrective USO, which has led to a substantial decrease in the complication and reoperation rates previously seen.25 Recently, Srinivasan et al25 demonstrated a shorter operative time and fewer complications with the use of an isolated USO for the treatment of distal radius malunions with ulnar impaction syndrome compared with historical reports of DRO.
We sought to compare the clinical and radiographic outcomes of patients undergoing isolated USO versus isolated DRO in the management of symptomatic ulnar impaction syndrome after extra-articular distal radius malunions.
Materials and Methods
After institutional review board approval, we conducted a retrospective review of patients with ulnar impaction syndrome treated with USO after extra-articular distal radius malunion at our institution. Operative intervention was considered for ulnar-sided wrist pain after distal radius malunion in the presence of ulnar positive variance and absence of greater than 25° dorsal angulation or carpal malalignment. Porter and Stockley21 demonstrated worse outcomes of distal radius fractures when dorsal angulation exceeded 20°, while Srinivasan et al25 did not offer isolated USO to patients with greater than 25° of dorsal tilt.
Patients who underwent concomitant DRO, had preexisting DRUJ arthrosis, younger than 18 years old, or those with less than 6 months of follow-up were excluded. Eleven patients met the inclusion criteria, with an average follow-up of 14.8 months (range, 6-50 months).
Patients treated with an isolated DRO were matched 1:1 for age and gender. We compared the 2 cohorts for demographics including operative time, symptomatic improvement, pain visual analog scale (VAS), wrist range of motion, grip and pinch strength, complication rates, and preoperative and postoperative radiographic parameters. Using dedicated wrist views, preoperative and postoperative ulnar variance, radial height, radial inclination, and volar tilt were analyzed. Preoperative 3-dimensional imaging such as computed tomography (CT) was not uniformly available to assess for rotational deformity.
The initial injury was treated with immobilization with or without closed reduction in 8 patients in the USO cohort, and 9 patients in the DRO cohort. The remainder in each underwent open reduction internal fixation (ORIF) with a single volar distal radius plate.
Comparing the 2 cohorts, there was no significant difference in baseline demographics (Table 1). There were 9 females in the USO cohort and 8 females in the DRO cohort. The dominant extremity was involved in 4 patients in each cohort. Similarly, there was no significant difference between groups in regard to the baseline preoperative radiographic parameters (Table 1).
Table 1.
The Differences in the Observed Means Between Study Groups (DRO Minus USO) for Patient Demographics and Characteristics Along With the Corresponding 95% CIs as Calculated Using a Bootstrap Resampling Procedure With 5000 Replicates.
| Variable | USO cohort (n = 11) |
DRO cohort (n = 11) |
Difference in means | 95% CI | ||||
|---|---|---|---|---|---|---|---|---|
| Mean | Range | SD | Mean | Range | SD | |||
| Age at surgery | 52.3 | 22-72 | 15.3 | 53.6 | 40-63 | 7.8 | 1.36 | −7.5 to 11.3 |
| BMI | 28.2 | 22.2-36.2 | 3.9 | 26.3 | 19.7-32.8 | 4.3 | −1.93 | −5.2 to 1.3 |
| ASA | 1.9 | 1-3 | 0.8 | 2.4 | 1-3 | 0.7 | 0.45 | −0.2 to 1.1 |
| Charlson comorbidity index | 1.4 | 0-3 | 1.0 | 1.4 | 0-3 | 1.1 | 0.00 | −0.8 to 0.8 |
| Preoperative ulnar variance (mm) | +4.4 | +2.1-+6.2 | 1.5 | +5.5 | +2.2-+13.2 | 3.2 | 1.13 | −0.7 to 3.3 |
| Preoperative radial inclination (°) | 21.6 | 13.8-32.3 | 7.0 | 22.8 | 15.8-28.1 | 4.3 | 1.23 | −3.6 to 5.7 |
| Preoperative volar tilt (°) (− = dorsal tilt, + = volar tilt) |
11.5 | −13.9-19.6 | 13.5 | 12.3 | −8.0-20.1 | 10.9 | 0.77 | −10.8 to 12.6 |
| Preoperative radial height (mm) | 10.5 | 7.4-15.8 | 2.9 | 11.1 | 6.5-16.8 | 3.2 | 0.61 | −1.8 to 3.1 |
| Follow-up (months) | 12.7 | 6.2-50.3 | 13.2 | 17.0 | 6.0-43.7 | 12.2 | 4.31 | −6.4 to 13.9 |
Note. A 95% confidence with a lower limit below zero and an upper limit above zero represents a nonsignificant result. DRO = distal radius osteotomy; USO = ulnar shortening osteotomy; CI = confidence interval; ASA = American Society of Anesthesiologists; BMI = body mass index.
Continuous variables were reported with a mean, range, and standard deviation. Comparisons between the 2 cohorts for preoperative and postoperative range of motion, VAS pain scores, grip and pinch strength, and radiographic parameters were performed utilizing difference in means and corresponding bootstrapped 95% confidence intervals. Statistical analysis was performed with the assistance of a statistician. A significant difference was considered when the bootstrapped 95% confidence interval did not include zero.
Surgical Technique and Postoperative Management
USO was performed using a subcutaneous approach with a transverse or oblique ulnar osteotomy at the junction of distal and middle third of ulna. The distal extent of the incision was placed 4 cm proximal to ulnar styloid. USO was performed using a compression plate utilizing various cutting jig systems (Acumed, Hillsboro, Oregon; or Rayhack, Wright Medical, Arlington, Tennessee; or Trimed, Santa Clarita, California).
DRO was performed using a modified Henry approach utilizing locking compression plates (Synthes, Switzerland; or Trimed). The osteotomy was performed at the point of maximal deformity. Bone grafting was utilized in all 11 cases, 5 with autologous cancellous iliac crest and 6 with demineralized cancellous chips.
Postoperatively, patients were initially immobilized in a plaster splint and then switched to a Muenster cast for a total period of approximately 6 weeks. Patients were then transitioned to a removable splint and seen by trained hand therapists to work on range of motion exercises and strengthening. Interval radiographs were obtained to assess healing of osteotomy sites by the presence of bridging bony trabeculae. Patients were gradually allowed to return to full employment based on their job requirements.
Results
Clinical outcomes are summarized in Table 2.
Table 2.
The Differences in the Observed Means for Clinical Outcomes Following USO and DRO (Postoperative Minus Preoperative Values) Along With the Corresponding 95% CIs as Calculated Using a Bootstrap Resampling Procedure With 5000 Replicates.
| USO |
DRO |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Preoperative |
Postoperative |
Difference in means | 95% CI | Preoperative |
Postoperative |
Difference in means | 95% CI | |||||
| Mean | Range | Mean | Range | Mean | Range | Mean | Range | |||||
| Wrist flexion (°) | 46.6 | 15-80 | 50.5 | 25-80 | 3.82 | −10.7 to 18.1 | 37.2 | 20-65 | 51.9 | 30-80 | 14.68 | 3.6 to 25.6* |
| Wrist extension (°) | 44.6 | 15-70 | 53.2 | 30-70 | 8.55 | −3.7 to 20.9 | 37.5 | 25-50 | 53.6 | 37-70 | 16.06 | 8.9 to 23.4* |
| Radial deviation (°) | 17.0 | 4-45 | 15.7 | 10-25 | −1.30 | −11.6 to 6.9 | 13.4 | 0-40 | 21.2 | 10-30 | 7.77 | −1.1 to 15.5 |
| Ulnar deviation (°) | 25.0 | 15-40 | 28.0 | 15-40 | 3.00 | −5.6 to 11.5 | 17.6 | 10-30 | 29.0 | 20-50 | 11.33 | 4.2 to 19.3* |
| Pronation (°) | 67.1 | 60-80 | 57.0 | 40-80 | −10.14 | −24.3 to 5.3 | 56.4 | 30-80 | 70.6 | 50-80 | 14.18 | 2.2 to 25.2* |
| Supination (°) | 53.6 | 10-80 | 52.0 | 30-80 | −1.57 | −26.1 to 25.1 | 62.2 | 20-80 | 73.8 | 65-80 | 11.53 | −0.3 to 25.3 |
| Grip strength (kg) | 14.4 | 2-25 | 23.3 | 6-38 | 8.93 | −1.3 to 18.9 | 14.1 | 7-23 | 25.6 | 16-50 | 11.50 | 4.6 to 19.5* |
| Pinch strength (kg) | 4.9 | 1-8 | 11.4 | 3-35 | 6.55 | −0.9 to 18.6 | 12.3 | 3-36 | 9.6 | 5-14 | −2.69 | −18.9 to 7.3 |
| Pain VAS | 5.1 | 2-7 | 2.0 | 0-6 | −3.09 | −4.6 to −1.5* | 5.8 | 1-9 | 2.0 | 0-5 | −3.78 | −5.4 to −2.0* |
Note. A 95% confidence with a lower limit below zero and an upper limit above zero represents a nonsignificant result. USO = ulnar shortening osteotomy; DRO = distal radius osteotomy; CI = confidence interval; VAS = visual analog scale.
Denotes significant difference of the means.
USO Cohort Outcome
Wrist flexion, extension, and ulnar deviation all improved. Radial deviation worsened minimally from an average of 17.0° to 15.7° (95% CI, −11.6 to 6.9). Pronation and supination worsened from an average of 67.1° to 57.0°, and from 53.6° to 52.0° (95% CI, −24.3 to 5.3, −26.1 to 25.1, respectively). None of the changes in range of motion were considered to be significant. Grip strength improved from 14.4 kg to 23.3 kg (95% CI, −1.3 to 18.9), and pain scores improved significantly from 5.1 to 2.0 (95% CI, −4.6 to −1.5).
The final mean ulnar variance after surgery was 1.8 mm negative, and the mean total tourniquet time was 97 minutes (Figure 1).
Figure 1.
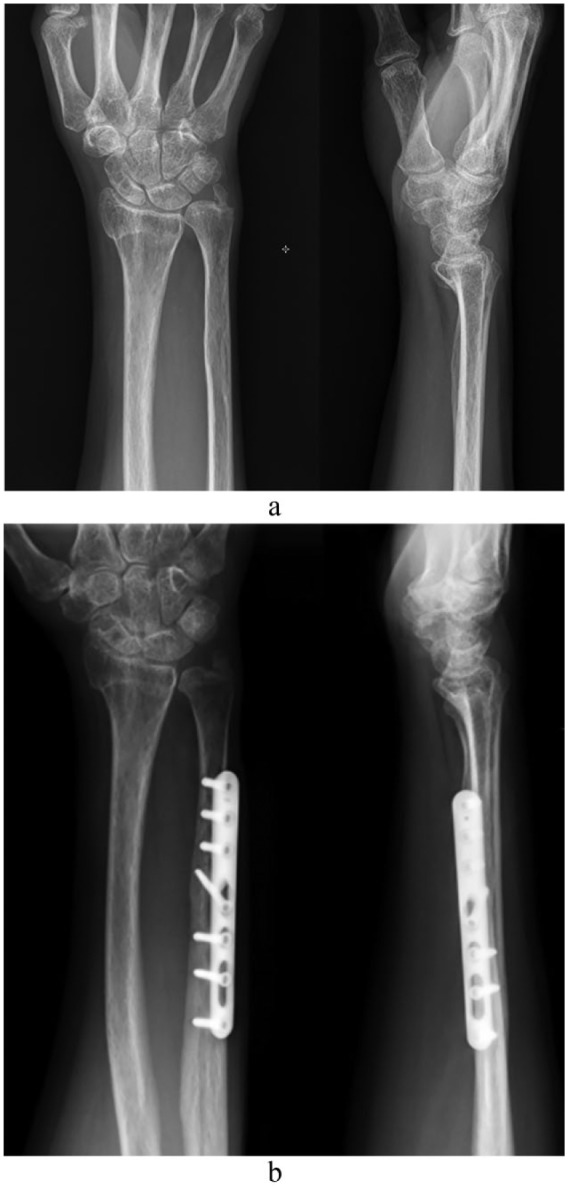
Preoperative (a) and 1-year postoperative (b) radiographs of a 56-year-old patient who underwent an ulnar shortening osteotomy after a distal radius malunion.
There was 1 nonunion in this group requiring reoperation with autologous cancellous iliac crest bone grafting. No other reoperations were noted. All remaining patients had evidence of bony union at 6 weeks follow-up with no need for plate removal. One patient had evidence of ulnocarpal degenerative changes at 30 months postoperatively.
DRO Cohort Outcome
Comparatively, patients undergoing DRO had a statistically significant increase in wrist flexion, extension, ulnar deviation and pronation (95% CI, 3.6 to 25.6, 8.9 to 23.4, 4.2 to 19.3, and 2.2 to 25.2, respectively). Radial deviation and supination were both improved (95% CI, −1.1 to 15.3, −0.3 to 25.3, respectively). There was an overall increase of 25.8° in the supination-pronation motion arc. Grip strength improved from 14.1 kg to 25.6 kg at final follow-up (95% CI, 4.6 to 19.5), and pain scores improved from 5.8 to 2.0 (95% CI, −5.4 to 2.0).
The final ulnar variance following DRO was 1.1 mm positive, and the mean total tourniquet time was longer than USO at a mean of 124 minutes (Figure 2).
Figure 2.

Preoperative (a) and 1-year postoperative (b) radiographs of a 49-year-old patient who underwent a distal radius osteotomy after a distal radius malunion.
Two patients failed to achieve symptomatic relief and functional improvement after DRO. These patients did not have restoration of their radioulnar length relationship with ulnar variances of 6.1 mm positive and 2.6 mm positive. Each underwent subsequent USO for persistent impaction symptoms at 8 months postoperatively, with good final clinical and functional results.
Comparison Between USO and DRO
There was no statistically significant difference between treatment groups in regard to change in range of motion, grip or pinch strength, pain scores, or radiographic outcomes, with the exception of a change in ulnar deviation and pronation (Table 3). In the USO group, pronation worsened by 9°, while this increased by 16° in the DRO group (95% CI, 9.8 to 40.3). The difference in tourniquet time was not statistically significant (95% CI, −6.5 to 56.0). However, there was 1 outlier in the USO group with a tourniquet time of 208 minutes. This was related to additional upper extremity procedures not related to the wrist. When excluding this patient, the average tourniquet time in the USO group was 86 minutes and the difference in means between study groups is statistically significant (95% CI, 13.3 to 60.6) (Figure 3).
Table 3.
The Differences in the Observed Means for the Difference in Clinical Outcomes Between Study Groups (DRO Minus USO) Along With the Corresponding 95% CIs as Calculated Using a Bootstrap Resampling Procedure With 5000 Replicates.
| USO |
DRO |
Difference in means | 95% CI | |||||
|---|---|---|---|---|---|---|---|---|
| Mean | Range | SD | Mean | Range | SD | |||
| Tourniquet time (minutes) | 97.3 | 46-208 | 46.0 | 124.0 | 60-181 | 31.0 | 26.73 | −6.5 to 56.0 |
| Δ Pain | −3.1 | −6-0 | 1.9 | −3.7 | −9-−1 | 2.5 | −0.58 | −2.5 to 1.3 |
| Δ Wrist flexion (°) | 3.8 | −50-55 | 24.2 | 14.7 | −10-30 | 13.8 | 10.86 | −4.7 to 26.8 |
| Δ Wrist extension (°) | 8.5 | −25-40 | 16.9 | 16.1 | 0-42 | 12.8 | 7.52 | −4.3 to 19.4 |
| Δ Radial deviation (°) | −1.7 | −20-10 | 10.4 | 6.8 | −10-25 | 11.2 | 8.53 | −1.7 to 18.6 |
| Δ Ulnar deviation (°) | 5.0 | 0-20 | 7.6 | 12.7 | 0-20 | 7.4 | 7.68 | 0.5 to 14.5* |
| Δ Pronation (°) | −9.0 | −25-10 | 14.3 | 15.9 | −5-35 | 16.3 | 24.88 | 9.8 to 40.3* |
| Δ Supination (°) | 7.0 | −30-50 | 29.9 | 13.8 | −5-60 | 20.5 | 6.75 | −20.9 to 33.6 |
| Δ Grip strength (kg) | 10.3 | 0-25 | 8.7 | 8.8 | −2-20 | 7.8 | −1.54 | −9.7 to 6.0 |
| Δ Pinch strength (kg) | 6.2 | −2-33 | 15.0 | −9.8 | −28-9 | 25.8 | −15.95 | −41.2 to 9.3 |
Note. A 95% confidence with a lower limit below zero and an upper limit above zero represents a nonsignificant result. Δ = Change. If the patient with a tourniquet time of 208 minutes in the USO group is excluded, the difference in means for tourniquet time and corresponding bootstrapped 95% confidence interval are 37.8 minutes and 13.3 to 60.6, respectively. DRO = distal radius osteotomy; USO = ulnar shortening osteotomy; CI = confidence interval.
Denotes significant difference of the means.
Figure 3.
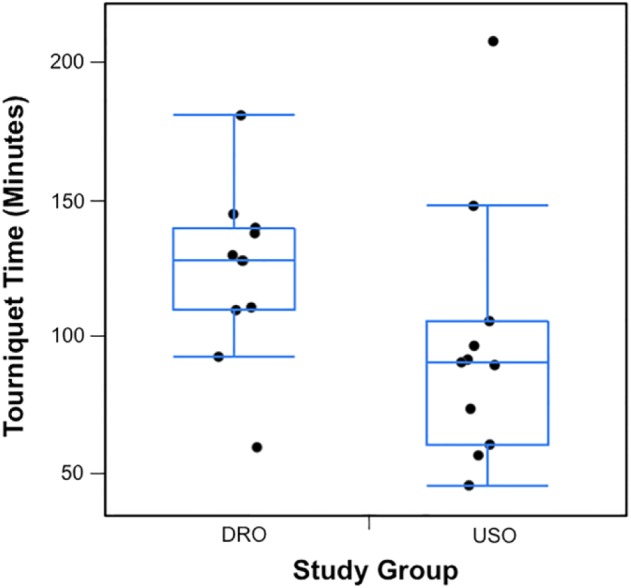
Tourniquet time (minutes) comparing distal radius osteotomy (DRO) to ulnar shortening osteotomy (USO.)
Discussion
Positive ulnar variance secondary to distal radius malunion can lead to major disabilities and chronic wrist pain. Loss of radial height can cause ulnar impaction syndrome with associated ulnar-sided wrist pain, loss of grip strength, and impingement of the DRUJ.9,10,16
Numerous studies have demonstrated a benefit in correcting the relative radioulnar length relationship to resolve symptoms associated with ulnar impaction and DRUJ derangement. USO for the management of ulnar impaction syndrome was originally described by Milch in 1941.17 Since then, there have been numerous techniques and implant designs described. The rationale for an ulnar-based procedure is to offload the ulnocarpal joint. In 1984, Palmer and Werner demonstrated that the DRUJ bore 18% of the total load in an ulnar neutral wrist. An increase in the ulnar variance by 2.5 mm increases the load on the ulnocarpal joint to 42%, whereas a decrease in length of the ulna by 2.5 mm decreases the load to only 4.3%.20
In the setting of a distal radius malunions, a radial-based osteotomy can be an effective treatment modality for management of deformity.19,22,23 However, this procedure is associated with considerable complications and an extended operative time. Simultaneous correction of the height and angulation is challenging and frequently incomplete.19,22,23 These patients may continue to suffer from wrist pain, ulnar abutment, loss of function and motion, and eventual osteoarthritis of the wrist. In our series, 2 of 11 patients failed to attain restoration of their radioulnar length relationship and required further surgery. Therefore, USO has the potential to be an attractive alternative to DRO, with a shorter tourniquet time and safer complication profile, which could address the same pathology after distal radius malunions.
Kamal and Leversedge12 reported on 10 patients who underwent USO for distal radius malunions and noted 4 nonunions which were attributed to increased volar radiocarpal deformity. This also occurred prior to the introduction of novel cutting guides. Tatebe et al26 later reviewed 16 patients with isolated USO and noted only 1 patient with a poor result based on the Mayo wrist score. Still, the use of isolated USO for distal radius malunions remains controversial.
Srinivasan et al25 described the use of an isolated USO for extra-articular distal radius malunions treated for ulnar impaction. They noted improved pain, range of motion, and strength with fewer complications. The range of motion in their series demonstrated more significant improvements than this current study, which may be related to our smaller sample size. Furthermore, both studies lack 3-dimensional assessment of the DRUJ. Any potential incongruence may result in decreased range of motion, particularly in forearm rotation. This may contribute to the less profound improvements in range of motion noted in our subjects.
The average tourniquet time in our study was longer than that reported by Srinivasan et al25 (86 minutes vs 57 minutes). However, this is still shorter than the mean tourniquet time of 130 minutes reported by Wada et al28 for opening wedge DRO and shorter than the 124-minute tourniquet time in our series.
Srinivasan et al25 also attempted to establish parameters that are appropriate for isolated USO in the setting of a distal radius malunion. The extremes in that study included 22° of dorsal tilt, 19° of volar tilt, and between 2° to 34° of radial inclination. Our study cohort was within these criteria and thus reaffirms the parameters. Due to the limited follow-up and smaller sample size, this study is unable to further define indications and contraindications for isolated USO based on radiographic measurements.
Hardware removal following DRO has been reported as high as 55%.22 Srinivasan et al25 reported only 1 plate removal, while none were required in our series.
Some studies have shown that radial inclination and sagittal angulation may lead to the development of arthritic changes over time.14 Srinivasan et al25 did not recommend performing isolated USO in patients younger than 50 years of age, particularly if a multiplanar deformity was present. Overall, there were 5 (2 USO, 3 DRO) patients who were younger than 50 years of age in this study, yet none of these required reoperation, had decreased range of motion, or persistent pain. With longer term follow-up, eventual development of wrist arthrosis may be a concern for young patients undergoing isolated USO.
This study has several limitations, including the retrospective design, small cohort, and limited follow-up. The combination of these factors limits the ability to make conclusions regarding long-term radiographic and clinical outcomes. The ideal inclusion criteria for isolated USO, such as age and baseline radiographic parameters, cannot be further elucidated by this series. Functional outcome scores were not universally available for the subjects and thus not reported. The strength of this study is the comparison between ulnar- and radial-based corrective osteotomies for patients with similar radiographic deformities, which was lacking in prior studies.
With improvements in pain, range of motion, a shorter tourniquet time, and decreased risk for revision surgery, isolated USO seems to be a reasonable and safe alternative to the use of DRO in the management of extra-articular distal radius malunions. We recommend considering an isolated USO in patients with sagittal angulation less than 20°, older than 50 years of age, and ulnar positive variance with impaction symptoms. A CT scan should be performed to evaluate the 3-dimensional alignment of the wrist deformity and assess whether a multiplanar DRO would be better indicated.
Footnotes
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5).
Statement of Informed Consent: Informed consent was obtained from all patients for being included in the study.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Arslan H, Subasi M, Kesemenli C, et al. Distraction osteotomy for malunion of the distal end of the radius with radial shortening. Acta Orthop Belg. 2003;69:23-28. [PubMed] [Google Scholar]
- 2. Baek GH, Lee HJ, Gong HS, et al. Long-term outcomes of ulnar shortening osteotomy for idiopathic ulnar impaction syndrome: at least 5-years follow-up. Clin Orthop Surg. 2011;3:295-301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Barbaric K, Rujevcan G, Labas M, et al. Ulnar shortening osteotomy after distal radius fracture malunion: review of literature. Open Orthop J. 2015;9:98-106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Chan SK, Singh T, Pinder R, et al. Ulnar shortening osteotomy: are complications under reported? J Hand Microsurg. 2015;7:276-282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Chun S, Palmer AK. The ulnar impaction syndrome: follow-up of ulnar shortening osteotomy. J Hand Surg Am. 1993;18:46-53. [DOI] [PubMed] [Google Scholar]
- 6. Chung KC, Spilson SV. The frequency and epidemiology of hand and forearm fractures in the United States. J Hand Surg Am. 2001;26:908-915. [DOI] [PubMed] [Google Scholar]
- 7. Cooney WP, III, Dobyns JH, Linscheid RL. Complications of Colles’ fractures. J Bone Joint Surg Am. 1980;62:613-619. [PubMed] [Google Scholar]
- 8. Fricker R, Pfeiffer KM, Troeger H. Ulnar shortening osteotomy in posttraumatic ulnar impaction syndrome. Arch Orthop Trauma Surg. 1996;115:158-161. [DOI] [PubMed] [Google Scholar]
- 9. Harness NG, Jupiter JB, Orbay JL, et al. Loss of fixation of the volar lunate facet fragment in fractures of the distal part of the radius. J Bone Joint Surg Am. 2004;86-A:1900-1908. [DOI] [PubMed] [Google Scholar]
- 10. Hollevoet N, Verdonk R. The functional importance of malunion in distal radius fractures. Acta Orthop Belg. 2003;69:239-245. [PubMed] [Google Scholar]
- 11. Iwasaki N, Ishikawa J, Kato H, et al. Factors affecting results of ulnar shortening for ulnar impaction syndrome. Clin Orthop Relat Res. 2007;465:215-219. [DOI] [PubMed] [Google Scholar]
- 12. Kamal RN, Leversedge FJ. Ulnar shortening osteotomy for distal radius malunion. J Wrist Surg. 2014;3:181-186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kiliç A, Kabukçuoğlu YS, Gül M, et al. Fixed-angle volar plates in corrective osteotomies of malunions of dorsally angulated distal radius fractures. Acta Orthop Traumatol Turc. 2011;45:297-303. [DOI] [PubMed] [Google Scholar]
- 14. Kopylv P, Johnell O, Redlund-Johnell I, et al. Fractures of the distal end of the radius in young adults: a 30-year follow-up. J Hand Surg Br. 1993;18:45-49. [DOI] [PubMed] [Google Scholar]
- 15. Loh YC, Van Den Abbeele K, Stanley JK, et al. The results of ulnar shortening for ulnar impaction syndrome. J Hand Surg Br. 1999;24:316-320. [DOI] [PubMed] [Google Scholar]
- 16. McQueen M, Caspers J. Colles fracture: does the anatomical result affect the final function? J Bone Joint Surg Br. 1988;70:649-651. [DOI] [PubMed] [Google Scholar]
- 17. Milch H. So-called dislocation of the lower end of the ulna. Ann Surg. 1942;116:282-292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Moermans A, Degreef I, De Smet L. Ulnar shortening osteotomy for ulnar ideopathic impaction syndrome. Scand J Plast Reconstr Surg Hand Surg. 2007;41:310-314. [DOI] [PubMed] [Google Scholar]
- 19. Oskam J, Bongers KM, Karthaus AJ, et al. Corrective osteotomy for malunion of the distal radius: the effect of concomitant ulnar shortening osteotomy. Arch Orthop Trauma Surg. 1996;115:219-222. [DOI] [PubMed] [Google Scholar]
- 20. Palmer AK, Werner FW. Biomechanics of the distal radioulnar joint. Clin Orthop Relat Res. 1984;(187);26-35. [PubMed] [Google Scholar]
- 21. Porter M, Stockley I. Fractures of the distal radius. Intermediate and end results in relation to radiologic parameters. Clin Orthop Relat Res. 1987;220:241-252. [PubMed] [Google Scholar]
- 22. Prommersberger KJ, Van Schoonhoven J, Lanz UB. Outcome after corrective osteotomy for malunited fractures of the distal end of the radius. J Hand Surg Br. 2002;27:55-60. [DOI] [PubMed] [Google Scholar]
- 23. Ring D. Treatment of the neglected distal radius fracture. Clin Orthop Relat Res. 2005;(431):85-92. [DOI] [PubMed] [Google Scholar]
- 24. Sammer DM, Rizzo M. Ulnar impaction. Hand Clin. 2010;26:549-557. [DOI] [PubMed] [Google Scholar]
- 25. Srinivasan RC, Jain D, Richard MJ, et al. Isolated ulnar shortening osteotomy for the treatment of extra-articular distal radius malunion. J Hand Surg Am. 2013;38:1106-1110. [DOI] [PubMed] [Google Scholar]
- 26. Tatebe M, Nakamura R, Horii E, et al. Results of ulnar shortening osteotomy for ulnocarpal impaction syndrome in wrists with neutral or negative ulnar variance. J Hand Surg Br. 2005;30:129-132. [DOI] [PubMed] [Google Scholar]
- 27. von Campe A, Nagy L, Arbab D, et al. Corrective osteotomies in malunions of the distal radius: do we get what we planned? Clin Orthop Relat Res. 2006;450:179-185. [DOI] [PubMed] [Google Scholar]
- 28. Wada T, Tatebe M, Ozasa Y, et al. Clinical outcomes of corrective osteotomy for distal radial malunion: a review of opening and closing-wedge techniques. J Bone Joint Surg Am. 2011;93:1619-1626. [DOI] [PubMed] [Google Scholar]
- 29. Young BT, Rayan GM. Outcome following nonoperative treatment of displaced distal radius fractures in low-demand patients older than 60 years. J Hand Surg Am. 2000;25:19-28. [DOI] [PubMed] [Google Scholar]


