Abstract
Background: After the thread transecting technique was successfully applied for the thread carpal tunnel release, we researched using the same technique in the thread trigger finger release (TTFR). This study was designed to test the operational feasibility of the TTFR on cadavers and verify the limits of division on the first annular (A1) pulley to ensure a complete trigger finger release with minimal iatrogenic injuries. Methods: The procedure of TTFR was performed on 14 fingers and 4 thumbs of 4 unembalmed cadaveric hands. After the procedures, all fingers and thumbs were dissected and visually assessed. Results: All of the digits and thumbs demonstrated a complete A1 pulley release. There was no injury to the neurovascular bundle (radial digital nerve in case of thumb), flexor tendon, or A2 pulley for each case. Conclusions: The cadaveric study showed that the technique of TTFR was safe and effective, and the future clinical study is necessary to verify the findings of this study.
Keywords: trigger finger release, percutaneous procedure, thread dissecting procedure, ultrasound-guided procedure, ultra-minimally invasive procedure, Guo technique
Introduction
The surgery of trigger finger release, or the first annular (A1) pulley transection, is usually recommended by a doctor if corticosteroid injection and other conventional treatments have failed. The most acceptable surgeries for trigger finger release are open surgery or percutaneous procedure. Open trigger release is considered the standard surgery with a low morbidity and high success rate, and percutaneous trigger release is accepted as an alternative.5,6,8-19
Wang et al searched literatures for randomized controlled trials, comparing percutaneous release with open surgery or corticosteroid injections. The meta-analysis of 676 identified patients resulted that there were no differences in the failure rate and complication frequency between patients undergoing percutaneous release and open surgery.22
Izadpanah et al reviewed all published data of trigger finger treatments from 1965 to 2012. Ultrasound-guided percutaneous release was associated with the highest success rate of 98% followed by open surgical release 94.2%, percutaneous release 91.9%, and steroid injection 70.2%. The meta-analysis with the consideration of random effects demonstrated percutaneous release to have a 94% chance of success, compared with 92% in the open release group and only 65% in the corticosteroid administration group.13
Gilberts et al conducted a prospective randomized study comparing open and percutaneous techniques performed on 100 patients. The symptoms were relieved for 100% of patients treated percutaneously and for 98% of patients treated with an open surgical procedure, with no complications. For percutaneous and open techniques, the procedure time was 7 versus 11 minutes, duration of postoperative pain was 3.1 versus 5.7 days, recovery of full hand function was 7 versus 18 days, and return to work was 3.9 versus 7.5 days, respectively.6
Although percutaneous release, especially guided by ultrasound, has advantages of ease of the procedure, decreased pain, faster recovery, absence of a painful palmar scar, and the flexibility to perform the procedure in the office with reduced costs,1,3 the procedure has inherent weaknesses and sometimes results in digital nerve injury, incomplete division of the pulley, and superficial flexor tendon injuries even with the help of ultrasound.2,7,16,18,19 Although the studies have shown that the percutaneous procedure of A1 pulley transection is effective and safe for the treatment of trigger finger,15,17,19,20 we believe the technique could be improved by pursuing a new cutting element with a different mechanism.
Recently, an innovative technique of ultra-minimally invasive surgery, the thread transecting technique or Guo technique, was successfully applied to carpal tunnel release, namely, thread carpal tunnel release (TCTR),10 which was performed under local anesthesia in a clinic-based procedure room, and resulted in only 1 needle entry point at the wrist and 1 needle exit point in the palm. The flexibility of the thread enables it to be routed accurately along a designated path to form a loop with a routing accuracy of 0.15 to 0.2 mm around the target to precisely control the transection.8 The nature of thread transecting ensures that the division is controlled only inside the loop of the thread around the targeted tissue with a negligible influence on adjacent nontargeted tissue. The thread can be easily placed using an 18-gauge or smaller spinal needle with only 2 punctures as entry and exit points for the thread.8 The clinical outcomes of TCTR revealed a statistically significant improvement (P < .001) in the short-term results and a better improvement in long-term results when compared with the open or endoscopic release.9
Theoretically, the thread transecting technique might have many advantages for dividing the A1 pulley in the trigger finger release procedure, namely the thread trigger finger release (TTFR). The aim of this cadaveric study was to test the operational feasibility of the TTFR and verify the limits of division on the A1 pulley to ensure a complete trigger finger release with minimal iatrogenic injuries.
Materials and Methods
General
The TTFR was performed on 14 fingers and 4 thumbs of 4 unembalmed cadaveric hands (2 of male and 2 of female) in the anatomy department of an academic institution in Minneapolis, Minnesota. The cadaveric specimens were obtained through the academic institution’s anatomy bequest program. All specimens were free from signs of trauma, deformity, or prior surgery. All fingers and thumbs were sonographically evaluated and found to have normal A1 pulleys.
Equipment
The ultrasound system used was a GE Logiq e or Logiq S8 ultrasound machine fitted with a GE L8-18i-D 18-MHz compact linear transducer (hockey stick probe) made by General Electric (Fairfield, Connecticut). Other materials included a commercial 18-gauge, 3.5-inch spinal needle; a piece of commercial surgical dissecting thread (Loop & Shear™, 0.009 inch in diameter and 18 inch in length; Ridge & Crest Company, Monterey Park, California); and a 5-mL syringe filled with 0.9% normal saline for hydrodissection of soft tissue.
Location of Division
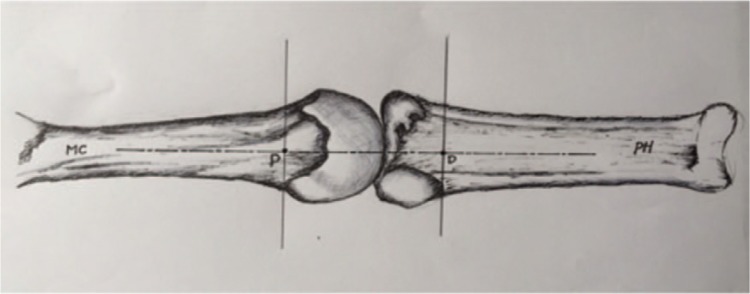
The division was designed along the midline of A1 pulley over the metacarpophalangeal joint. The proximal limit of division is determined by the most proximal position of the sonographic bone mark at the metacarpal head-neck junction at volar surface (note that it is not on the midline sagittal plane), and the distal position was determined by the most distal point at the phalangeal base-shaft junction. As illustrated in Figure 1, P is the proximal limit of division, the projection of the most proximal point on the midline, and D is the distal limit of division, the projection of the most distal point on the midline.
Figure 1.
Anterior view of the metacarpophalangeal joint.
Note. MC = metacarpal bone; P = the proximal limit of division on the midline; D = the distal limit of division on the midline; PH = phalanx (proximal).
Operating Technique
The hand and forearm were placed in the supine position. With the help of ultrasound, the midline of the A1 pulley was marked on the skin, and the point P of proximal limit of division and the point D of distal limit were also marked at the midline on the skin.
There are 2 similar approaches for looping the transecting thread around the A1 pulley, the distal to proximal approach and the proximal to distal approach. The distal to proximal approach is described below (Figure 2).
Figure 2.
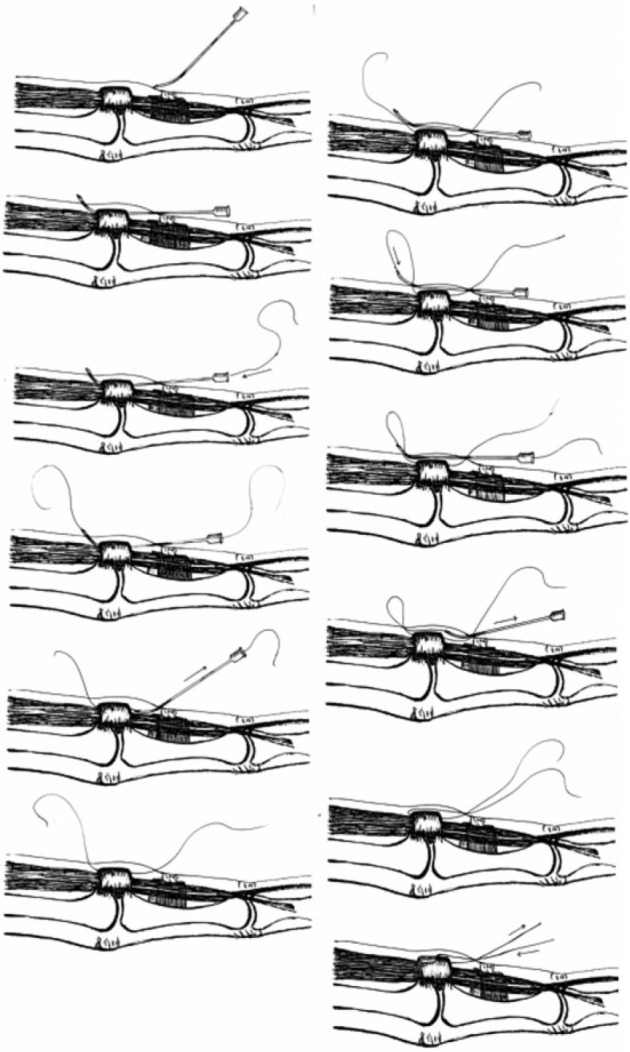
The steps of thread trigger finger release.
An 18-gauge, 3.5-inch spinal needle was bent at the distal shaft to a 15° angle with the bevel side concave and was connected with a 5-mL syringe filled with saline. Under the guidance of ultrasound, the needle was inserted into the subcutaneous tissue at the proximal finger crease and advanced to lever of the distal limit D of division. The needle penetrated into the tendon sheath; then, the advancing direction was adjusted to make the needle superficial to the tendon (Figure 3a and 3b). After checking the digital nerves and vessels on each side, the needle was advanced to the proximal limit, the point P of division on the midline, and the target digit was held in a hyperextension position to facilitate the needle to penetrate the subcutaneous tissue and exit the skin. The transecting thread was fed through the needle. The needle was then withdrawn, leaving the thread in the sheath deep to the pulley (Figure 4a and 4b). The same needle was inserted into the same entry, then advanced proximally over the A1 pulley subcutaneously (Figure 5a), and allowed to exit the skin at the same exit. The proximal end of the thread was fed through the needle. The needle was then withdrawn, leaving the thread looped around the A1 pulley (Figure 5b).
Figure 3.
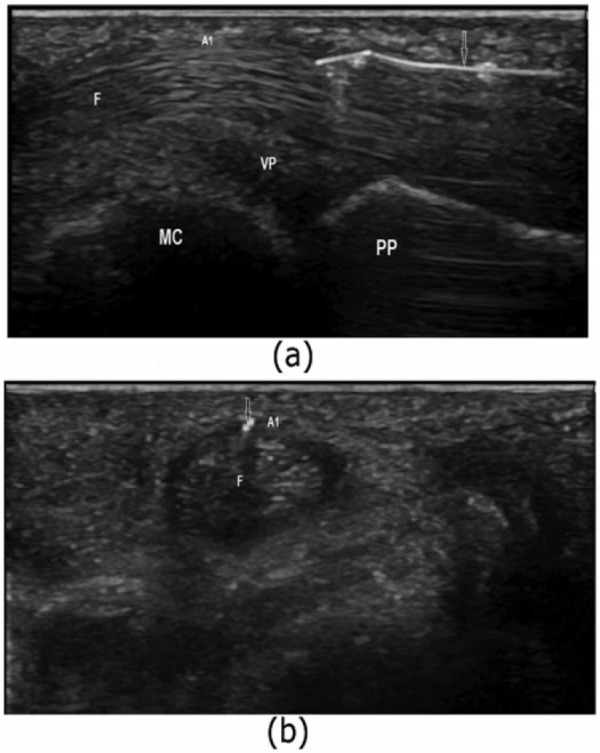
First needle pass at the A1 pulley. (a) The longitudinal view from the distal to proximal. (b) The short-axis view.
Note. Down arrow indicates the needle. A1 = A1 pulley; F = flexor tendons; VP = volar plate; MC = metacarpal bone; PP = proximal phalanx.
Figure 4.
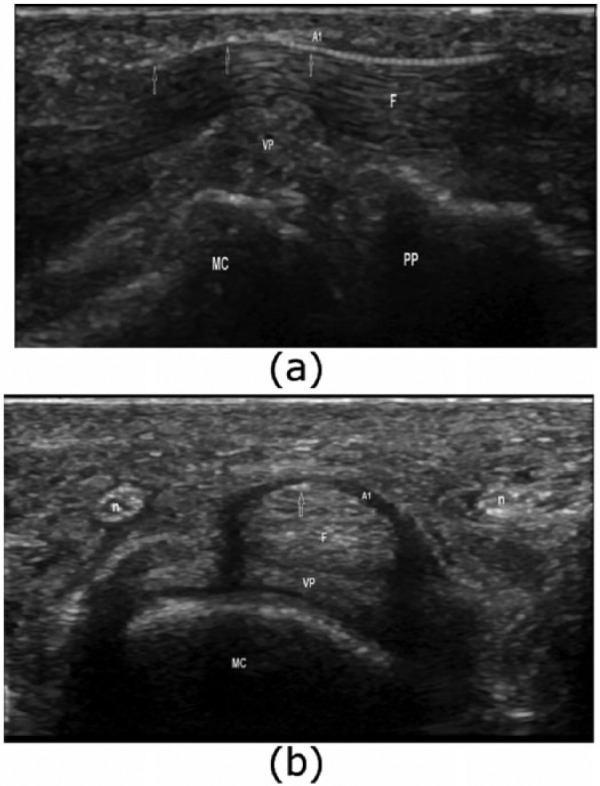
Transecting thread placed underneath the A1 pulley. (a) The longitudinal view. (b) The short-axis view.
Note. Up arrows indicate the transecting thread; n indicates common digital nerves. A1 = A1 pulley; F = flexor tendons; VP = volar plate; MC = metacarpal bone; PP = proximal phalanx.
Figure 5.
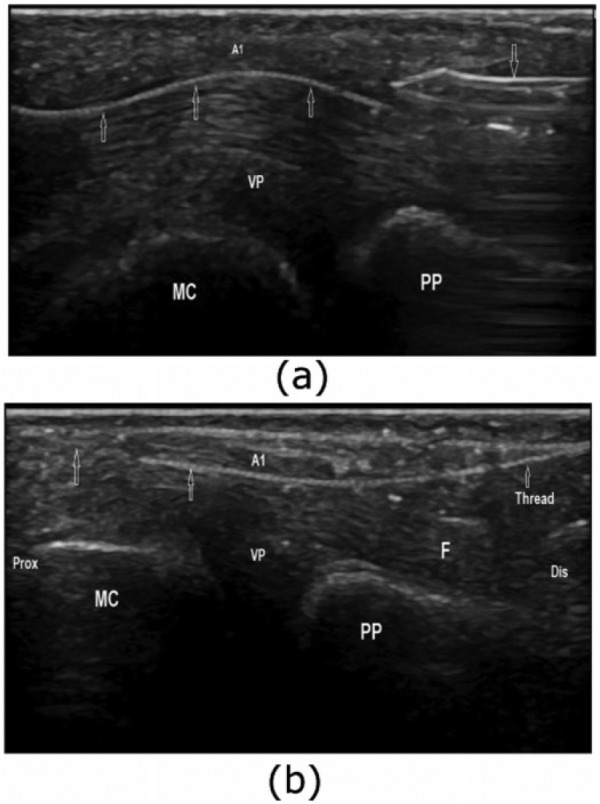
The second pass for completing the loop. (a) Second needle pass superficial to the A1 pulley. (b) A1 pulley was looped by a transecting thread.
Note. Up arrows indicate the transecting thread; down arrow indicates the needle approaching distal limit P in the second pass. A1 = A1 pulley; VP = volar plate; MC = metacarpal bone; PP = proximal phalanx; Prox = proximal; Dis = distal.
The A1 pulley was manually dissected by a reciprocating motion of the thread until the thread pulled out of the finger. It takes about 5 seconds.
The description for the proximal to distal approach is omitted for it is similar to the above description. For both approaches, the whole process was under the real-time visualization of ultrasound and was involved with hydrodissection all the time (injecting fluid to hydrostatically separate the tissues and create the space in between).
Assessment
Immediately after the procedures, all fingers and thumbs were carefully dissected and visually assessed. The degree of release of A1 pulley and possible injuries were all exposed and evaluated.
Results
All of the 14 digits and 4 thumbs demonstrated a complete A1 pulley release (Figures 6 and 7). There was no injury to the neurovascular bundle (radial digital nerve in case of thumb), flexor tendon, or A2 pulley for each case.
Figure 6.
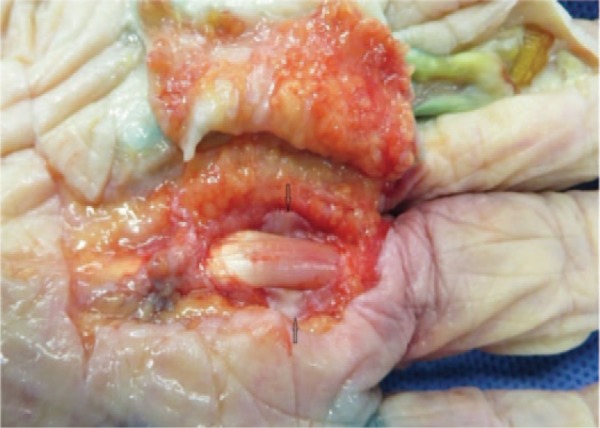
Complete release of first annular (A1) pulley of a finger.
Note. Up and down arrows indicate completely released A1 pulley.
Figure 7.
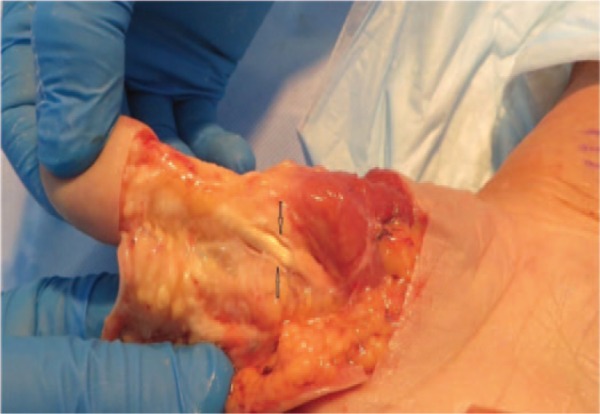
Complete release of first annular (A1) pulley of a thumb.
Note. Up and down arrows indicate completely released A1 pulley of a thumb.
Seven fingers underwent the proximal to distal approach, whereas other 7 fingers underwent the distal to proximal approach. Four thumbs underwent the proximal to distal approach (Figure 8). The distal to proximal approach was not operational for the thumbs due to difficulty in exiting the needle. Both approaches did not make any difference for fingers. Each procedure took about 5 to 10 minutes.
Figure 8.

First needle pass at the first annular (A1) pulley of a thumb.
Discussion
In this study, through the procedure of TTFR, all the cases resulted in the complete release of A1 pulley and no injury to the neurovascular bundle (radial digital nerve in case of thumb), flexor tendon, or A2 pulley. This near-perfect result is probably due to two main factors: the preciseness of the thread transecting technique and the correctness in determining the proximal and distal limits of division on the A1 pulley.
The control accuracy of the technique was shown in the previous study of carpal tunnel release to be 0.15 to 0.2 mm, which is precise enough in the procedure of TTFR to avoid all the unnecessary injuries and ensure a complete release of A1 pulley if the proximal and distal limits of division on the pulley are determined correctly.
The determination of the limits of division on A1 pulley is critical for the successful A1 pulley release. It is difficult to sonographically determine the boundary of the A1 pulley only by means of the hyperechoic or hypoechoic image of the A1 pulley, especially at the proximal boundary.15,17,20
Many researchers accepted the topographic bone marks of the metacarpal head-neck junction and the phalangeal base-shaft junction as the reference for the proximal and distal boundaries of the pulley, because the A1 pulley is functionally a joint pulley of the metacarpophalangeal joint, originating from the regions of the metacarpal head-neck junction and the phalangeal base-shaft junction.11,21 But there are many possible selections when using the bone marks as the references for the limits of division on A1 pulley. The location of the metacarpal head-neck junction or the phalangeal base-shaft junction at the different sagittal plane is not on the same transverse plane, and its projection on the midline is variable (Figure 1). Specifically on the midline sagittal plane, if the mark of head-neck junction is used for the proximal boundary of A1 pulley, it is less proximal to the actual boundary of the A1 pulley, and if the mark of base-shaft junction is used for the distal boundary, it is less distal to the actual boundary.2,18
Clinically, when using the bone marks on the midline plane as the references, Rojo-Manaute et al determined the proximal limit of division at 5 mm proximal to the head-neck junction, and the distal limit at 3 mm distal to the base-shaft junction.17 Jou and Chern selected 5 mm in proximal end and 3 mm in distal end.15 In a cadaveric study, Smith et al used 1 to 2 mm for both ends.20
In general, the length of each pulley varies in direct proportion to the length of the digit.11,12 The people from the West have the average length of A1 pulley about 10 mm, but for Asian people, it is about 6 mm.4,14 Therefore, the security margin should not be a constant and has to be adjusted each time according to the length of the digit or thumb of the specific patient. There was no such adjustment in the present determination for the limits of division via the most proximal and the most distal marks during the procedure of TTFR, and the correctness was verified in the cadaveric study.
The cadaveric study showed that the technique of TTFR was safe and effective, and we will verify the present findings in future clinical studies.
Footnotes
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: All procedures in the study were in accordance with the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Statement of Informed Consent: No informed consent was obtained for this cadaveric study.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Joseph Guo owns the US patent of the technique used in the study. The rest of the authors have no conflict of interest.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: General Electric Corp and Ridge & Crest Company provided the devices used in this study. Joseph Guo has financial interest in the devices for thread trigger finger release. Danqing Guo and Danzhu Guo have received a research grant from BayCare Clinic, Green Bay, Wisconsin.
References
- 1. Calleja H, Tanchuling A, Alagar D, et al. Anatomic outcome of percutaneous release among patients with trigger finger. J Hand Surg Am. 2010;35(10):1671-1674. [DOI] [PubMed] [Google Scholar]
- 2. Chern TC, Jou IM, Yen SH, et al. Cadaveric study of sonographically assisted percutaneous release of the A1 pulley. Plast Reconstr Surg. 2005;115(3):811-822. [DOI] [PubMed] [Google Scholar]
- 3. Eastwood DM, Gupta KJ, Johnson DP. Percutaneous release of the trigger finger: an office procedure. J Hand Surg Am. 1992;17(1):114-117. [DOI] [PubMed] [Google Scholar]
- 4. Fiorini HJ, Santos JB, Hirakawa CK, et al. Anatomical study of the A1 pulley: length and location by means of cutaneous landmarks on the palmar surface. J Hand Surg Am. 2011;36(3):464-468. doi: 10.1016/j.jhsa.2010.11.045. [DOI] [PubMed] [Google Scholar]
- 5. Fowler JR, Baratz ME. Percutaneous trigger finger release. J Hand Surg Am. 2013;38(10):2005-2008. doi: 10.1016/j.jhsa.2013.03.001. [DOI] [PubMed] [Google Scholar]
- 6. Gilberts EC, Beekman WH, Stevens HJ, et al. Prospective randomized trial of open versus percutaneous surgery for trigger digits. J Hand Surg Am. 2001;26:497-500. [DOI] [PubMed] [Google Scholar]
- 7. Guler F, Kose O, Ercan EC, et al. Open versus percutaneous release for the treatment of trigger thumb. Orthopedics. 2013;36(10):e1290-e1294. [DOI] [PubMed] [Google Scholar]
- 8. Guo D, Guo D, Guo J, et al. A cadaveric study for the improvement of thread carpal tunnel release. J Hand Surg Am. 2016;41(10):e351-e357. http://dx.doi.org/10.1016/j.jhsa.2016.07.098. [DOI] [PubMed] [Google Scholar]
- 9. Guo D, Guo D, Guo J, et al. A clinical study of the modified thread carpal tunnel release (TCTR). Hand 2016. doi: 10.1177/1558944716668831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Guo D, Yu T, Ji Y, et al. A non-scalpel technique for minimally invasive surgery: percutaneously looped thread transection of the transverse carpal ligament. Hand. 2015;10(1):40-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hauger O, Chung CB, Lektrakul N, et al. Pulley system in the fingers: normal anatomy and simulated lesions in cadavers at MR imaging, CT, and US with and without contrast material distention of the tendon sheath. Radiology. 2000;217(1):201-212. [DOI] [PubMed] [Google Scholar]
- 12. Idler RS. Anatomy and biomechanics of the digital flexor tendons. Hand Clin. 1985;1(1):3-11. [PubMed] [Google Scholar]
- 13. Izadpanah A, Zein M, Kanevsky J, et al. Comparison of percutaneous release, open release, endoscopic and corticosteroid injection in the treatment of trigger digits: a systematic review and meta-analysis. Plast Reconstr Surg. 2013;131(suppl 5):85. [Google Scholar]
- 14. Jongjirasiri Y. Length and landmark of A1 pulley in hand: an anatomical study. J Med Assoc Thai. 2009;92(1):41-46. [PubMed] [Google Scholar]
- 15. Jou IM, Chern TC. Sonographically assisted percutaneous release of the A1 pulley: a new surgical technique for treating trigger digit. J Hand Surg Br. 2006;31(2):191-199. [DOI] [PubMed] [Google Scholar]
- 16. Paulius KL, Maguina P. Ultrasound-assisted percutaneous trigger finger release: is it safe? Hand. 2009;4:35-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Rojo-Manaute JM, Rodríguez-Maruri G, Capa-Grasa A, et al. Sonographically guided intrasheath percutaneous release of the first annular pulley for trigger digits, part 1: clinical efficacy and safety. J Ultrasound Med. 2012;31(3):417-424. [DOI] [PubMed] [Google Scholar]
- 18. Rojo-Manaute JM, Soto VL, De las Heras Sánchez-Heredero J, et al. Percutaneous intrasheath ultrasonographically guided first annular pulley release: anatomic study of a new technique. J Ultrasound Med. 2010;29(11):1517-1529. [DOI] [PubMed] [Google Scholar]
- 19. Ryzewicz M, Wolf JM. Trigger digits: principles, management, and complications. J Hand Surg Am. 2006;31:135-146. [DOI] [PubMed] [Google Scholar]
- 20. Smith J, Rizzo M, Lai JK. Sonographically guided percutaneous first annular pulley release cadaveric safety study of needle and knife techniques. J Ultrasound Med. 2010;29(11):1531-1542. [DOI] [PubMed] [Google Scholar]
- 21. Strickland JW. Flexor tendon injuries: I. Foundations of treatment. J Am Acad Orthop Surg. 1995;3(1):44-54. [DOI] [PubMed] [Google Scholar]
- 22. Wang J, Zhao JG, Liang CC. Percutaneous release, open surgery, or corticosteroid injection, which is the best treatment method for trigger digits? Clin Orthop Relat Res. 2013;471(6):1879-1886. [DOI] [PMC free article] [PubMed] [Google Scholar]