Abstract
Background: Carpal tunnel syndrome (CTS) is a common occupational pathology, representing a high percentage of workers’ compensation (WC) claims. Methods: The literature was reviewed for all studies evaluating CTS outcomes including WC patients between 1993 and 2016. A total of 348 articles were identified; 25 of which met inclusion and exclusion criteria. A systematic review was generated; patient demographics, outcomes, and complications were recorded. Weighted averages were calculated for the demographic and outcome data. Categorical data such as complications were pooled from the studies and used to determine the overall complication rate. Statistical significance was determined between WC and non-WC cohorts when applicable with the chi-square statistic. Results: The WC cohort included 1586 wrists, and the non-WC cohort included 2781 wrists. The WC cohort was younger and more often involved the dominant extremity. The WC cohort was less likely to have appropriate physical exam findings confirming diagnosis and electrodiagnostic studies. WC patients took almost 5 weeks longer to return to work, were 16% less likely to return to preinjury vocation, and had lower Standard Form (SF)-36 scores. Finally, WC patients had nearly 3 times the number of complications and nearly twice the rate of persistent pain. Conclusions: WC patients undergoing carpal tunnel release (CTR) fare poorly as compared with non-WC patients in nearly every metric. Higher rates of postoperative pain with delayed return to work can be anticipated in a WC cohort. In addition, WC patients receive suboptimal preoperative workup, and it is possible that unnecessary surgery is being completed in these cases. These findings are important to consider when treating the WC patient with CTS.
Keywords: carpal tunnel syndrome, carpal tunnel release, workers’ compensation, disability
Introduction
Carpal tunnel syndrome (CTS) is the most common compressive neuropathy of the upper extremity and most common occupational injury to the hand, with a prevalence of 50 cases per 1000 patients per year.2,9 Up to 50% of the cases of CTS are work related, and as such, a substantial portion of CTS cases are treated under workers’ compensation (WC) coverage.6,10 Unfortunately, there are several factors that make WC patients less likely to benefit from treatment. WC patients are more poorly educated, are more likely to be in a union, are less likely to be married, are younger, have lower expectations from treatment, and have both lower preoperative and postoperative outcome scores following surgery as compared with non-WC patients.19,21,22
Specifically, those receiving WC for CTS do even worse than those receiving WC from other workplace injuries. In a study of patients receiving WC from Washington State, the CTS population had 3 times the amount of work loss as compared with the fracture cohort. In addition, the CTS cohort had earnings losses estimated as high as $382 million, or $89,000 per worker, over the study period.15
Small individual studies have determined that the WC CTS cohort is at a higher risk to do poorly with treatment and represents an enormous cost in lost work and wages and increased healthcare expenditures. Despite these factors, there is not a large analysis which directly compares the WC with non-WC patients in the treatment of CTS. We present a systematic review of CTS to compare demographics and outcomes to compare WC with non-WC patients.
Methods
Literature Search
A systematic review of the literature was performed. We used PubMed to search all years through April 2016 with combinations of search terms: “carpal tunnel syndrome” and “workers’ compensation.” Four independent reviewers assessed methodology and quality of each study. We extracted homogeneous data from studies which met the inclusion/exclusion criteria and generated frequency-weighted means.1,3-5,7,8,12,14,18,20,23,25-28,31,33,36-38,40-42,46 A systematic review was performed when data were sufficiently homogeneous according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines.
Inclusion/Exclusion Criteria
The studies were included if they: (1) were published in English, (2) involved CTS, (3) included greater than 10 patients in the cohort, (4) had all patients undergone surgical intervention in the analysis, and (5) included WC patients within the analysis. The studies were excluded if they: (1) were published in any language other than English, (2) had all patients not undergone surgical intervention, and (3) did not include WC patients.
Four authors independently performed electronic searches. Abstracts with clearly or potentially relevant titles were browsed for relevance to CTS and WC and were included as appropriate. If an abstract met inclusion/exclusion criteria, the authors reviewed the entire text to verify qualification. There was no discrepancy between the findings of the 4 authors.
Data Extraction
We extracted and analyzed study design, demographic variables, presence of a WC claim, and outcomes. The 4 authors independently extracted the data, and then conferred and compiled the data.
Statistical Analysis
The weighted averages were calculated for the demographic and outcome data. Categorical data such as complications were pooled from the studies and used to determine the overall complication rate. For each variable, the calculations were performed out of the total number of patients or extremities which reported that variable. The authors assessed each aforementioned data set for homogeneity. Heterogeneous data were excluded from meta-analysis. If the data were homogeneous, we performed a chi-square statistic.
Results
Study Retrieval and Characteristics
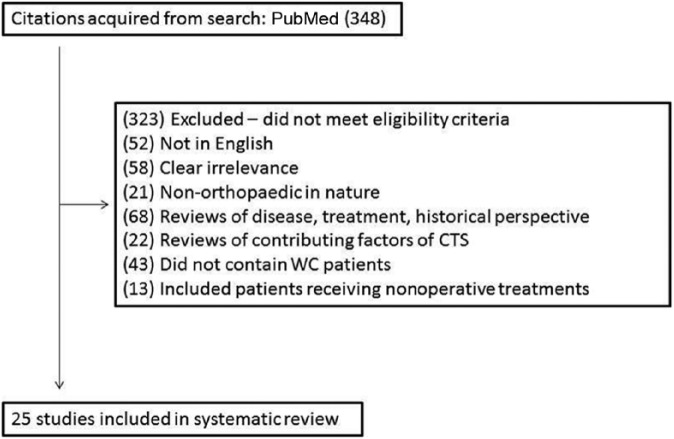
Our searches generated 348 different articles. After applying the exclusion criteria, 323 articles were excluded from the analysis. In all, 25 studies met the inclusion and exclusion criteria. Study characteristics are shown. There were 19 prospective and 6 retrospective studies (Figure 1). None of these studies involved the same author or patient cohorts. One study was level I, 9 were level III, and the remaining 14 were level IV evidence.
Figure 1.
Breakdown of PubMed database systematic review.
Note. CTS = carpal tunnel syndrome; WC = workers’ compensation.
Patient Demographics and Injury Characteristics
The 25 studies included in the systematic review comprised 1586 (36%) WC patients with 1856 wrists (38%) and 2781 (64%) non-WC patients with 3012 wrists (62%). The WC cohort was significantly younger (P < .0005), involved the dominant extremity (P = .0013), and underwent endoscopic over open release (P < .0001). The remaining demographic variables were otherwise not significantly different between the 2 groups (Table 1).
Table 1.
Demographic Information.
| Demographics | WC cohort | No. of studies | No. of patients | Non-WC cohort | No. of studies | No. of patients | P value |
|---|---|---|---|---|---|---|---|
| Age | 39 | 4 | 236 | 49.9 | 4 | 356 | <.0005 |
| Male | 26.6% | 6 | 440 | 30.5% | 6 | 492 | .649 |
| Open (vs endoscopic) | 65.0% | 17 | 857 | 77.3% | 17 | 1721 | <.0001 |
| Dominant extremity | 57.5% | 1 | 25 | 20.5% | 1 | 51 | .0013 |
| Preoperative symptom score | 3.3 | 1 | 94 | 3.1 | 1 | 856 | NC |
| Preoperative functional score | 2.6 | 1 | 94 | 2.4 | 1 | 856 | NC |
| Electrodiagnostic studies | 85.70% | 2 | 238 | 92.70% | 2 | 109 | .0656 |
| Tinel sign (positive) | 50.30% | 1 | 187 | 65.50% | 1 | 87 | .0181 |
| Phalen test (positive) | 49.70% | 1 | 187 | 80.50% | 1 | 87 | <.0001 |
Note. Boldface values indicate statistical significance (<.05). WC = workers’ compensation; NC = not calculated.
Characteristic physical exam findings including the Tinel sign and Phalen test were more often positive in non-WC patients (P = .0181 and P < .0001, respectively). Electrodiagnostic studies trended toward being more frequently positive in the non-WC cohort as well (P = .07).
Functional and Occupational Outcomes
At an average final follow-up of 14.4 months, 77% of WC patients were able to return to their preinjury vocation as compared with 93% of non-WC patients (P < .0005). WC patients furthermore required 4.9 weeks longer to return to work (Table 2).
Table 2.
Outcomes and Complications.
| Outcomes | WC cohort | No. of studies | No. of patients | Non-WC cohort | No. of studies | No. of patients | P value |
|---|---|---|---|---|---|---|---|
| Follow-up | 19.8 | 6 | 320 | 18.6 | 6 | 666 | .977 |
| Time to return to ADLs | 6.9 | 3 | 75 | 7.8 | 3 | 252 | NC |
| % Return to work | 76.9% | 8 | 728 | 93.0% | 8 | 729 | <.0005 |
| Time to return to work | 58.4 | 11 | 807 | 23.9 | 11 | 1029 | NC |
| Continued pain | 58.20% | 9 | 572 | 26.10% | 9 | 663 | <.0005 |
| SF-35 score | 44.2 | 1 | 25 | 56.3 | 1 | 51 | NC |
| Symptom score | 2 | 3 | 172 | 1.65 | 3 | 980 | NC |
| % Improvement | 39.39% | 3 | 172 | 46.77% | 172 | 980 | .1913 |
| Functional score | 1.93 | 3 | 172 | 1.54 | 3 | 980 | NC |
| % Improvement | 25.77% | 3 | 172 | 35.83% | 172 | 980 | .0356 |
| % Complications | 33.30% | 3 | 109 | 12.60% | 3 | 176 | .0001 |
| % Revision release | 3.10% | 1 | 50 | 2.60% | 1 | 63 | .8136 |
Note. Boldface values indicate statistical significance (<.05). WC = workers’ compensation; ADLs = activities of daily living; NC = not calculated.
Average SF-35 scores were lower among the WC population. Preoperative symptom and functional scores were not significantly different between the cohorts; however, the degree of symptomatic (39.4% vs 46.8%, P = .1913) and functional improvement (25.8% vs 35.8%, P = .0356) were greater for non-WC patients.
Complications and Reoperation
Overall, one-third (33.3%) of WC patients experienced complications. Complications in non-WC patients were significantly less common (12.6%, P < .0001). Complications in WC patients were almost exclusively drawn from the series by Hallock and Lutz who reported that 41 WC patients experienced complications (33.3%) versus 19 non-WC patients (57.6%). The authors however did not separate specific complications based on WC or non-WC populations but instead by type of procedure (open vs. endoscopic), reporting that scar hypersensitivity, pillar pain, incomplete symptom relief, and infection were overall the most common.18 Pomerance and Fine40 and Lewicky33 found no complications in the WC cohorts. Pomerance and Fine reported 3 cases of wound dehiscence in non-WC patients (2.7%).40 Similarly, Lewicky33 reported only 1 complication involving a reflex sympathetic dystrophy in 1 non-WC patients (2.5%).
Of those studies which reported postoperative pain, 58.2% of WC patients reported persistent pain following carpal tunnel release (CTR) versus 26.1% of non-WC patients (P < .0005). Incisional pain was more common in the non-WC cohort (19.4% vs 6.6%, P < .0001), whereas pillar pain was more common among WC patients (78.7% vs 62.0%, P = .0047; Table 2).
A comparable number of WC and non-WC patients underwent repeat CTR (3.1% vs 2.6%, respectively, P = .8136). Intraoperative findings and indication for reoperation were not discussed. Duncan et al12 reported that WC patients were more likely to undergo reoperation with an odds ratio greater than 5.0, although external median nerve neurolysis in repeat CTRs provided no improvement in residual symptoms in the WC cohort.
Discussion
We present the largest conglomeration of WC patients with CTS. The key findings were threefold. Our primary findings were as follows: First, WC patients had significantly higher rates of postoperative pain; second, WC patients had over twice as long before returning to work which trended toward significance; and last, the complication rate was 3 times as high in the WC group. We also had the following secondary findings. First, postoperative functional improvement was greater for the non-WC group. Second, WC patients were less likely to have appropriate physical exam and electrodiagnostic studies confirming CTS. These points are important to consider when counseling a WC patient with CTS regarding the risks and benefits of CTR.
WC patients undergoing CTR have demonstrably less preoperative workup as compared with non-WC patients. Surgeons may feel pressured by the patient to perform what may be unnecessary surgery. Patients may have a potential financial interest to prove their WC claim and therefore may request surgery for a condition that they do not have according to physical exam and objective studies. In addition, there is a potential for physicians to perform procedures outside the standard of care if financially incentivized to do so.21,34 It is estimated that unnecessary or inappropriate studies and procedures account for 20% of health care expenses.17 One study of 169 clavicle fractures in WC patients demonstrated that those receiving surgery did not have better outcomes as compared with those receiving conservative management. However, the surgical group consumed 3.5 times the amount of health care resources as the nonoperative group. Ongoing litigation was an independent predictor of delayed return to work and increased cost.43 Another analysis estimated that increasing a waiting period to 3 to 7 days before a WC claim could be made would decrease the number of claims by up to 25%. Perhaps these data could be extrapolated to the care of CTS: A reasonable workup without rushing to surgery could reduce the number of unnecessary CTRs.22 Surgeons would do well to refuse surgical management of any patient without appropriate physical exam and diagnostic studies confirming a diagnosis of CTS.
WC patients have exhibited worse postoperative functional results as compared with non-WC patients in the surgery of the hand, elbow, and shoulder.30 Specifically, in compressive neuropathies to include radial tunnel and cubital tunnel, the WC cohort has done poorly.11,16,24,29,32,35,39,44 These results parallel the poor postoperative outcomes found in this study. There are 2 primary factors which may precipitate the poor outcomes following CTR. First, as this analysis reported, WC patients have suboptimal preoperative workups and it is possible that patients without CTR are getting unnecessary surgery. Second, a WC patient may report poorer outcomes consciously, or believe they are doing poorly subconsciously, to continue receiving financial or social benefits. This may explain why states with more generous WC benefits tend to have higher WC claims.21,23
Similarly, WC patients may be financially incentivized to report complications. A complication may permit prolonged time on possibly lucrative disability, which in some states has historically represented 150% of a patient’s standard wage.47 In addition, the high complication rates noted in the WC cohort of this analysis may be related to a conscious decision to delay the return to work. The number of total WC claims is noted to be higher on Mondays as compared with other days of the week, and additionally, the ratio of hidden injuries (back pain and sprains) versus nonhidden injuries (lacerations) is also higher on Mondays.45 More specifically, in some states, a knee sprain can result in 40 weeks of benefits; this is calculated by a potential 20% impairment rating multiplied by the 200 weeks for loss of a leg. Other states award benefits for projected future loss of earnings. Some WC patients may choose to exacerbate complications to retain such benefits.13
The limitations to this analysis are threefold. First, as a systematic review, the quality of detail contained within is limited to the studies which we included. The lack of specific demographic, social, and psychiatric factors limits our ability to stratify risk. Second, potential biases contained within the included literature affect our results. Finally, the patients contained within the cohorts of a systematic review are not homogeneous, as in a meta-analysis limiting its external validity.
Despite these limitations, we present the largest comparison of WC and non-WC patients after CTR. We determined that WC patients are likely to take longer time to return to work with higher rates of postoperative pain and complications. Secondarily, they are also less likely to have a physical exam and diagnostic studies that correspond to the operative diagnosis, and WC patients have significantly worse postoperative functional outcomes. These findings are important for the surgeon to keep in mind when counseling patients undergoing CTR. WC patients should undergo the same preoperative workup, and should expect to have poorer results with a high complication rate following surgery.
Footnotes
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: This study was a retrospective chart review with institutional review board approval ensuring no human rights violations. No animals were involved.
Statement of Informed Consent: The retrospective nature of this review makes informed consent not relevant as the patients have already received their treatment.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Al-Qattan M, Bowen V, Manktelow RT. Factors associated with poor outcome following primary carpal tunnel release in non-diabetic patients. J Hand Surg Br. 1994;19:622-625. [DOI] [PubMed] [Google Scholar]
- 2. American Academy of Orthopaedic Surgeons Work Group Panel. Clinical guidelines on diagnosis of carpal tunnel syndrome. http://www.aaos.org/Research/guidelines/CTS_guideline.pdf. Accessed April 16, 2016.
- 3. Amick B, Habeck R, Ossmann J, et al. Predictors of successful work role functioning after carpal tunnel release surgery. J Occup Environ Med. 2004;46:490-500. [DOI] [PubMed] [Google Scholar]
- 4. Atroshi I, Johnsson R, Nouhan R, et al. Use of outcome instruments to compare workers’ compensation and non-workers’ compensation carpal tunnel syndrome. J Hand Surg Am. 1997;22:882-888. [DOI] [PubMed] [Google Scholar]
- 5. Bessette L, Keller R, Lew R, et al. Prognostic value of a hand symptom diagram in surgery for carpal tunnel syndrome. J Rheumatol. 1997;24:726-734. [PubMed] [Google Scholar]
- 6. Bickel KD. Carpal tunnel syndrome. J Hand Surg Am. 2010;35:147-152. [DOI] [PubMed] [Google Scholar]
- 7. Cagle P, Reams M, Agel J, et al. An outcomes protocol for carpal tunnel release: a comparison of outcomes in patients with and without medical comorbidities. J Hand Surg Am. 2014;39:2175-2180. [DOI] [PubMed] [Google Scholar]
- 8. Chaise F, Hellemere P, Fril JP, et al. Return-to-work interval and surgery for carpal tunnel syndrome. Results of a prospective series of 233 patients. J Hand Surg Br. 2004;29:568-570. [DOI] [PubMed] [Google Scholar]
- 9. Concannon MJ, Brownfield ML, Puckett CL. The incidence of recurrence after endoscopic carpal tunnel release. Plast Reconstr Surg. 2000;105:1662-1665. [DOI] [PubMed] [Google Scholar]
- 10. Davis L, Wellman H, Punnett L. Surveillance of work-related carpal tunnel syndrome in Massachusetts, 1992–1997: a report from the Massachusetts Sentinel Event Notification System for Occupational Risks (SENSOR). Am J Ind Med. 2001;39:58-71. [DOI] [PubMed] [Google Scholar]
- 11. Dellon AL, Coert JH. Results of the musculofascial lengthening technique for submuscular transposition of the ulnar nerve at the elbow. J Bone Joint Surg Am. 2004;86:169-179. [DOI] [PubMed] [Google Scholar]
- 12. Duncan S, Calandruccio J, Merritt M, et al. A comparison of workers’ compensation patients and nonworkers’ compensation patients undergoing endoscopic carpal tunnel release. Hand Surg. 2010;15:75-80. [DOI] [PubMed] [Google Scholar]
- 13. Durbin D. Workplace injuries and the role of insurance: claims costs, outcomes, and incentives. Clin Orthop Relat Res. 1997;336:18-32. [DOI] [PubMed] [Google Scholar]
- 14. Elmaraghy M, Hurst L. Single-portal endoscopic carpal tunnel release: Agee carpal tunnel release system. Ann Plast Surg. 1996;36:286-291. [DOI] [PubMed] [Google Scholar]
- 15. Foley M, Silverstein B, Pollisar N. The economic burden of carpal tunnel syndrome: long-term earnings of CTS claimants in Washington State. Am J Ind Med. 2007;50:155-172. [DOI] [PubMed] [Google Scholar]
- 16. Glowacki KA, Weiss AP. Anterior intramuscular transposition of the ulnar nerve for cubital tunnel syndrome. J Shoulder Elbow Surg. 1997;6:89-96. [DOI] [PubMed] [Google Scholar]
- 17. Griner PF. Payment reform and the mission of academic medical centers. N Engl J Med. 2010;363:1784-1786. [DOI] [PubMed] [Google Scholar]
- 18. Hallock G, Lutz D. Prospective comparison of minimal incision “open” and two-portal endoscopic carpal tunnel release. Plast Reconstr Surg. 1995;96:941-947. [DOI] [PubMed] [Google Scholar]
- 19. Henn RF, Kang L, Tashijan RZ, et al. Patients with workers’ compensation claims have worse outcomes after rotator cuff repair. J Bone Joint Surg Am. 2008;90:2105-2113. [DOI] [PubMed] [Google Scholar]
- 20. Higgs PE, Edwards D, Martin DS, et al. Carpal tunnel surgery outcomes in workers: effect of workers’ compensation status. J Hand Surg Am. 1995;20:354-360. [DOI] [PubMed] [Google Scholar]
- 21. Hirsch BT. Incentive effects of workers’ compensation. Clin Orthop Relat Res. 1997;336:33-41. [DOI] [PubMed] [Google Scholar]
- 22. Hirsch BT, Macpherson DA, DuMond JM. Workers’ compensation recipiency in union and nonunion workplaces. Ind Labor Relat Rev. 1997;50:213-236. [Google Scholar]
- 23. Hulsizer D, Staebler M, Weiss AP, et al. The results of revision carpal tunnel release following previous open versus endoscopic surgery. J Hand Surg Am. 1998;23:865-869. [DOI] [PubMed] [Google Scholar]
- 24. Jebson PJ, Engber WD. Radial tunnel syndrome: long-term results of surgical decompression. J Hand Surg Am. 1997;22:889-896. [DOI] [PubMed] [Google Scholar]
- 25. Katz J, Amick B, Keller R, et al. Determinants of work absence following surgery for carpal tunnel syndrome. Am J Ind Med. 2005;47:120-130. [DOI] [PubMed] [Google Scholar]
- 26. Katz J, Keller R, Fossel A, et al. Predictors of return to work following carpal tunnel release. Am J Ind Med. 1997;31:85-91. [DOI] [PubMed] [Google Scholar]
- 27. Katz J, Lew R, Bessette L, et al. Prevalence and predictors of long-term work disability due to carpal tunnel syndrome. Am J Ind Med. 1998;33:543-550. [DOI] [PubMed] [Google Scholar]
- 28. Katz J, Losina E, Amick B, et al. Predictors of outcomes of carpal tunnel release. Arthritis Rheum. 2001;44:1184-1193. [DOI] [PubMed] [Google Scholar]
- 29. Kleinman WB, Bishop AT. Anterior intramuscular transposition of the ulnar nerve. J Hand Surg Am. 1989;14:972-979. [DOI] [PubMed] [Google Scholar]
- 30. Konrad G, Huang K, Wanich T, et al. Workers’ compensation and outcomes of upper extremity surgery. J Am Acad Orthop Surg. 2013;21:67-77. [DOI] [PubMed] [Google Scholar]
- 31. Lee H, Jackson T. Carpal tunnel release through a limited skin incision under direct visualization using a new instrument, the carposcope. Plast Reconstr Surg. 1996;98:313-319. [DOI] [PubMed] [Google Scholar]
- 32. Lee JT, Azari K, Jone NF. Long term results of radial tunnel release—the effect of co-existing tennis elbow, multiple compression syndromes and worker’ compensation. J Plast Reconstr Aesthet Surg. 2008;61:1095-1099. [DOI] [PubMed] [Google Scholar]
- 33. Lewicky R. Endoscopic carpal tunnel release: the guide tube technique. Arthroscopy. 1994;10:39-49. [DOI] [PubMed] [Google Scholar]
- 34. Medicare: higher use of advanced imaging services by providers who self-refer costing Medicare Millions. US Government Accountability Office. GAO-12-966. http://www.gao.gov/assets/650/648988.pdf. Published September 2012. Accessed March 10, 2017.
- 35. Naam NH, Nemani S. Radial tunnel syndrome. Orthop Clin North Am. 2012;43:529-536. [DOI] [PubMed] [Google Scholar]
- 36. Nagle D, Harris G, Foley M. Prospective review of 278 endoscopic carpal tunnel releases using the modified chow technique. Arthroscopy. 1994;10:259-265. [DOI] [PubMed] [Google Scholar]
- 37. Olney J, Quenzer D, Makowsky M. Contested claims in carpal tunnel surgery: outcome study of workers’ compensation factors. Iowa Orthop J. 1999;19:111-121. [PMC free article] [PubMed] [Google Scholar]
- 38. Palmer D, Paulson C, Lane-Larsen C, et al. Endoscopic carpal tunnel release: a comparison of two techniques with open release. Arthroscopy. 1993;9:498-508. [DOI] [PubMed] [Google Scholar]
- 39. Pasque CB, Rayan GM. Anterior submuscular transposition of the ulnar nerve for cubital tunnel syndrome. J Hand Surg Br. 1995;20:447-453. [DOI] [PubMed] [Google Scholar]
- 40. Pomerance J, Fine I. Outcomes of carpal tunnel surgery with and without supervised postoperative therapy. J Hand Surg Am. 2007;32:1159-1163. [DOI] [PubMed] [Google Scholar]
- 41. Roth J, Richards R, MacLeod M. Endoscopic carpal tunnel release. Can J Surg. 1994;37:189-193. [PubMed] [Google Scholar]
- 42. Shapiro S. Microsurgical carpal tunnel release. Neurosurg Focus. 1997;3:e3. [DOI] [PubMed] [Google Scholar]
- 43. Shields E, Thirukumaran C, Thorsness R, et al. Patient factors influencing return to work and cumulative financial claims after clavicle fractures in workers’ compensation cases. J Shoulder Elbow Surg. 2016;25:1115-1121. [DOI] [PubMed] [Google Scholar]
- 44. Smith RS. Mostly on Monday: is workers’ compensation covering off-the-job injuries? In: Borba PS, Appel D, eds. Benefits, Costs, and Cycles in Workers’ Compensation Insurance. Norwell, MA: Kluwer Academic Publishers; 1990:115-127. [Google Scholar]
- 45. Sotereanos DG, Vartimidis SE, Giannakopoulos PN, et al. Results of surgical treatment for radial tunnel syndrome. J Hand Surg Am. 1999;24:566-570. [DOI] [PubMed] [Google Scholar]
- 46. Straub T. Endoscopic carpal tunnel release: a prospective analysis of factors associated with unsatisfactory results. Arthroscopy. 1999;15:269-274. [DOI] [PubMed] [Google Scholar]
- 47. US Chamber of Commerce. Analysis of Workers’ Compensation Laws. 1995 ed. Washington, DC: US Chamber of Commerce; 1995. [Google Scholar]
- 48. Wolfe SW, Pederson WC, Hotchkiss RN, et al. Green’s Operative Hand Surgery. 6th ed. Philadelphia, PA: Elsevier Churchill Livingstone; 2010. [Google Scholar]